Abstract
Fasting plasma glucose (FPG) and hemoglobin A1c (HbA1c) are both used to diagnose diabetes, but these measurements can identify different people as having diabetes. We used data from 117 population-based studies and quantified, in different world regions, the prevalence of diagnosed diabetes, and whether those who were previously undiagnosed and detected as having diabetes in survey screening, had elevated FPG, HbA1c or both. We developed prediction equations for estimating the probability that a person without previously diagnosed diabetes, and at a specific level of FPG, had elevated HbA1c, and vice versa. The age-standardized proportion of diabetes that was previously undiagnosed and detected in survey screening ranged from 30% in the high-income western region to 66% in south Asia. Among those with screen-detected diabetes with either test, the age-standardized proportion who had elevated levels of both FPG and HbA1c was 29–39% across regions; the remainder had discordant elevation of FPG or HbA1c. In most low- and middle-income regions, isolated elevated HbA1c was more common than isolated elevated FPG. In these regions, the use of FPG alone may delay diabetes diagnosis and underestimate diabetes prevalence. Our prediction equations help allocate finite resources for measuring HbA1c to reduce the global shortfall in diabetes diagnosis and surveillance.
Similar content being viewed by others
Main
Diabetes is associated with debilitating complications such as amputation, vision loss and renal failure, and with increased risk of cardiovascular events, dementia, some cancers and infectious diseases such as severe COVID-19 and tuberculosis1,2,3,4,5,6. The diagnostic criteria for diabetes have evolved over time to incorporate hemoglobin A1c (HbA1c), which is a measure of long-term glycemic status and more convenient to measure for patients than fasting glucose or the 2-h oral glucose tolerance test (OGTT)7,8,9,10. In contemporary guidelines, any one or the combination of fasting plasma glucose (FPG), OGTT and HbA1c may be used to diagnose diabetes10,11,12,13,14. With the exception of diagnosis of gestational diabetes, OGTT is now rarely used in clinical practice or population surveillance because of the inconvenience related to the glucose load, 2-h time frame and the two blood draws required for the test15,16. FPG and HbA1c, which are both used in clinical practice and epidemiological research and surveillance, measure different glycemic features, namely basal glucose level (FPG) and average glucose level in the previous 2–3 months (HbA1c)17. Therefore, individuals may have elevated levels of one or both biomarkers, and FPG and HbA1c may classify different people as having diabetes9,10. Diabetes also has a long subclinical period defined by hyperglycemia and can remain undiagnosed without screening or other mechanisms for early identification18.
Some studies have assessed sensitivity and specificity of diabetes diagnosis using either FPG or HbA1c relative to the OGTT or have compared diabetes prevalence based on these different glycemic biomarkers, but most did not provide a direct comparison of HbA1c and FPG19,20,21. Most population-based studies on the concordance and discordance of diabetes diagnosis using FPG versus HbA1c have been conducted in a single country or region14,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42 and the only multi-country study43 used data largely from high-income western countries. Therefore, there are scant data on how the concordance and discordance of FPG and HbA1c in classifying diabetes vary across regions in the world, and on the factors associated with this variation. The lack of data on the regional variation in diabetes identified based on FPG versus HbA1c means that we cannot quantify the full extent of the global diabetes epidemic and its regional variation, because diabetes prevalence is measured and reported using a single glycemic biomarker in most population-based surveys and analyses44,45,46. For example, in the latest global analysis44, only ~15% of surveys had measured both FPG and HbA1c.
We assembled a global database of population-based studies that had measured both FPG and HbA1c. Using these data, we quantified the regional variation in the extent of diabetes diagnosis, with diabetes defined as in the Methods. We also quantified, among those who were previously undiagnosed and were detected as having diabetes through screening in the survey, the concordance and discordance of having FPG and HbA1c above common diagnostic thresholds (7.0 mmol l−1 for FPG and 6.5% for HbA1c). We refer to this group as screen-detected diabetes, which is an epidemiological definition, because many clinical guidelines recommend two measurements for diabetes diagnosis10,11,12,13. We then used regression analysis to examine what individual and study-level factors were associated with whether participants with screen-detected diabetes were identified by elevated FPG, elevated HbA1c or elevated levels of both. It has been shown that having elevated levels of both biomarkers has high positive predictive value for subsequent clinical diagnosis and risk of complications14,47, and hence this group is similar to clinically diagnosed diabetes.
Finally, we leveraged the global coverage of the dataset and its large sample size to develop prediction equations that estimate, for any given FPG level, the probability that a person without previously diagnosed diabetes would have HbA1c above the clinical threshold for diabetes had it been measured, and vice versa. We aimed to develop and validate global and generalizable prediction equations that account for both personal characteristics and regional differences. These equations serve three purposes. First, they allow more efficient use of finite diagnostic resources, by identifying some people with below- or near-threshold level for one biomarker (for example, FPG) for measurement of another (for example, HbA1c). Second, they allow the estimation of the probability that a person with a screen-detected elevated level of one biomarker would also have an elevated level of the other, as a confirmation of diabetes status14,47. Finally, the prediction equations could improve diabetes surveillance by allowing estimation of prevalence of diabetes based on both FPG and HbA1c in health surveys that have measured only one of these biomarkers.
Results
Data sources
We used data collated by the NCD Risk Factor Collaboration (NCD-RisC), a global consortium of population-based health examination surveys and studies with measurement of both FPG and HbA1c, and with data on previous diagnosis of diabetes, as described in the Methods. The criteria for including and excluding studies are stated in Methods. Within each study, we excluded participants who had missing data or were pregnant, under 18 years of age or from follow-up rounds of studies that had multiple measurements of the same cohort over time (Fig. 1). After exclusions, we used data on 601,307 participants aged 18 years and older with information on whether they had been previously diagnosed with diabetes, of whom 364,825 participants also had measured FPG and HbA1c. The difference between the number of participants with data on previous diagnosis and with biomarker data is mostly because many studies do blood tests on a subsample of those with questionnaire data. These participants were from 117 studies whose mid-year was from 2000 to 2021 in 45 countries from seven of eight world regions (Extended Data Table 1). We had no study that measured both FPG and HbA1c from the region of Oceania, which consists of Pacific island nations. The number of studies in other regions ranged from seven in sub-Saharan Africa to 48 in the high-income western region (Table 1). The mean age of study participants was 50 years and 56% of participants were women. Of the 117 studies with data on glycemic variables, 113 (97%) with 351,270 participants (96% of all participants) also had data on body-mass index (BMI); the remaining four studies either did not collect anthropometric information or only had self-reported height and weight data.
aExcluded because glucose metabolism changes during pregnancy. bData from the first available measurement were used for these participants. cSome surveys only measured glycemic biomarker on a subset of participants for logistic or budget reasons. dExcluded because glycemic measurements in these participants were systematically different from the rest from the same study, possibly because the specific area had high prevalence of thalassemia94. eExcluded because such values are more likely to be due to data recording error than values within the range. fWe removed participants for implausible pairs of FPG and HbA1c using the method of local outlier factor (LOF)95. This approach detects data combinations that are extremes in the joint density of the variable pairs (for example, a participant with FPG of 5 mmol l−1 and HbA1c of 17%, or with FPG of 28 mmol l−1 and HbA1c of 5%). We identified extremes as those measurements whose measure of local density by LOF method is less than half of the average of their 100 nearest neighbors. gIncluding all 2,436 participants from four studies that did not measure BMI. hIncluding all 3,455 participants from four studies in which all individuals without previously diagnosed diabetes had FPG < 7.0 mmol l−1 and HbA1c < 6.5%.
Screen-detected diabetes by FPG and HbA1c
Across all studies, 16% of participants had diagnosed or previously undiagnosed screen-detected diabetes. Diagnosed diabetes was calculated based on reporting a previous diagnosis and screen-detected diabetes as having FPG and/or HbA1c levels at or above the thresholds of 7.0 mmol l−1 and 6.5% (refs. 10,11,12,13) (Fig. 2). After age-standardization, the total prevalence of diabetes became 12%. The age-standardized prevalence of diagnosed and screen-detected diabetes were 7% and 5%, respectively. Those without a previous diabetes diagnosis had a lower BMI than those with a previous diagnosis in every region, by an average of 2.9 kg m−2 across all studies (Table 1). Among those without a previous diagnosis, participants with screen-detected diabetes (FPG ≥7.0 mmol l−1 and/or HbA1c ≥ 6.5%) had a mean BMI that was higher than those who did not have diabetes (FPG < 7.0 mmol l−1 and HbA1c < 6.5%) by an average of 2.4 kg m−2.
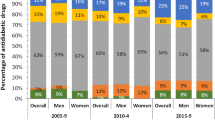
a, Crude and age-standardized proportion of participants with diagnosed or screen-detected diabetes and, for those without previous diagnosis, whether they had isolated elevated FPG (FPG ≥ 7.0 mmol l−1 and HbA1c < 6.5%), isolated elevated HbA1c (HbA1c ≥ 6.5% and FPG < 7.0 mmol l−1) or elevated levels of both. b, Crude and age-standardized proportion of participants with screen-detected diabetes who had isolated elevated FPG, isolated elevated HbA1c or elevated levels of both, by region. The contents in b are the same as the segment of a that is below the zero line, scaled to 100% so that the composition of screen-detected diabetes can be compared across regions, regardless of its total prevalence. Having elevated levels of both biomarkers has high positive predictive value for subsequent clinical diagnosis and risk of complications14,47 and hence this group is similar to clinically diagnosed diabetes. In a, regions are ordered by the total proportion of participants who had diagnosed and screen-detected diabetes. In b, regions are ordered by the crude proportion of participants with screen-detected diabetes who had elevated levels of both FPG and HbA1c. Extended Data Fig. 1 provides sex-specific results.
In most regions, age-standardized diabetes prevalence was slightly lower than crude prevalence, except south Asia where the participants were on average younger than in other regions (Table 1). Regionally, the age-standardized total diabetes prevalence (the combination of diagnosed and screen-detected diabetes) ranged from ~9% in the high-income western region to ~21% in south Asia and sub-Saharan Africa. The age-standardized proportion of diabetes that was previously undiagnosed, and was detected in the screening via the survey, was highest (66%) in studies from south Asia, and lowest (<35%) in studies from the high-income western region, central and eastern Europe, and the region of central Asia, Middle East and north Africa. Two studies in sub-Saharan Africa were from Mauritius, a country that is different demographically and economically from most other countries in the region. When these studies were removed, total age-standardized diabetes prevalence in sub-Saharan Africa declined from 21% to 13% and the proportion who were previously undiagnosed increased from 46% to 53% (Extended Data Fig. 2).
Across all studies together, 29% of participants with screen-detected diabetes had isolated elevated FPG, 37% had isolated elevated HbA1c and 34% had elevated levels of both. These global proportions were the same before and after age-standardization. There was substantial variation across regions in the composition of screen-detected diabetes across these three groups, both in terms of whether both biomarkers were elevated or only one, and in the case of the latter, whether the elevated biomarker was FPG or HbA1c (Fig. 2). Regionally, the shares of participants in these three groups changed little after age-standardization, and we report the age-standardized results here. The age-standardized proportion of those with screen-detected diabetes who had elevated levels of both FPG and HbA1c ranged from 29–39% across regions. The remaining 61–71% of participants with screen-detected diabetes had discordant FPG and HbA1c elevations. Isolated elevated HbA1c made up 54% of participants with screen-detected diabetes in sub-Saharan Africa, and 47% in the region of central Asia, Middle East and north Africa. In these regions, isolated elevated FPG accounted for <17% of all screen-detected diabetes. In contrast, 55% of participants with screen-detected diabetes in central and eastern Europe, and 46% in high-income western region, had isolated elevated FPG. The correlation coefficient between FPG and HbA1c among participants without previous diagnosis of diabetes ranged from 0.51 in central and eastern Europe to 0.76 in sub-Saharan Africa (Extended Data Fig. 3).
Association with individual and study characteristics
Some participant and study-level characteristics were associated with whether screen-detected diabetes was manifested as elevated levels of FPG, HbA1c or both (Table 2). Among those with screen-detected diabetes, male sex was associated with a higher probability of having elevated FPG, either alone (prevalence ratio (PR) = 1.10; 95% credible interval (CrI) 1.07–1.14) or together with elevated HbA1c (1.07; 1.03–1.11), and with a lower probability of having isolated elevated HbA1c (0.86; 0.83–0.89). Older age was associated with a lower probability of having elevated FPG, alone (PR = 0.97 per decade of age; 0.96–0.98) or together with elevated HbA1c (PR = 0.97; 0.96–0.99) and a higher probability of having isolated elevated HbA1c (1.05; 1.04–1.06). Higher BMI was associated with a higher probability of having concordant elevation of FPG and HbA1c (PR = 1.07 per 5 units; 1.06–1.08) and a lower probability of having isolated elevated FPG (PR = 0.92; 0.90–0.93).
At the study level, in studies that used a portable device to measure HbA1c, the composition of screen-detected diabetes was shifted toward more isolated elevated HbA1c, but the estimates for this association had wide confidence intervals because the great majority of studies in our analysis had measured glucose and HbA1c in a laboratory. Neither the year of study nor the percentage of participants with diabetes who had reported previous diagnosis were associated with the composition of screen-detected diabetes.
After adjustment for participant and study characteristics, regional differences remained in the composition of screen-detected diabetes (Table 2). After adjustment for these factors, the composition of screen-detected diabetes, in terms of having elevated FPG and HbA1c in isolation or together, was statistically indistinguishable between the high-income western region and central and eastern Europe. In other regions, elevated HbA1c was a more common form of screen-detected diabetes than in the high-income western region, in isolation (PR ranging 1.42–2.20 across these regions) or together with elevated FPG (PR ranging 1.31–1.52 in east and southeast Asia and the Pacific; south Asia; sub-Saharan Africa). In all regions, isolated elevated FPG was less common than in the high-income western region (PR ranging 0.24–0.51).
Prediction equations
We developed nine prediction equations (Extended Data Table 2) that estimate, for any given FPG level, the probability that a person without previously diagnosed diabetes would have HbA1c above the clinical threshold for diabetes had it been measured, and vice versa. The variables in the prediction equations included FPG as well as sex, age, BMI, whether FPG was measured in a laboratory or using a portable device, and region. We assessed the performance of the models in predicting (1) individual participants’ status of having HbA1c ≥ 6.5% based on their FPG and (2) the prevalence of HbA1c ≥ 6.5% for an entire study. We used the same method for predicting the probability of having FPG ≥ 7.0 mmol l−1 based on HbA1c. The performance at the individual level reflects how well the prediction equation works for triaging patients for further measurement for diabetes, and the performance at study (or population) level assesses how well the prediction equation works for diabetes surveillance. Most of the prediction equations had acceptable performance for estimating the probability that a person without diagnosed diabetes at a specific level of one glycemic biomarker (FPG or HbA1c) was above the clinical threshold for the other (Extended Data Tables 3 and 4). Specifically, the C-statistic ranged 0.85–0.90 for prediction equations that used either biomarker to predict the elevated level of the other. The mean errors were between −0.18 and −0.65 percentage points and the mean absolute errors were between 2.32 and 3.30 percentage points. The best-performing models for predicting whether participants had HbA1c ≥ 6.5% using FPG measurement included BMI and region-specific terms for FPG, referred to as models 5 and 8 in Extended Data Tables 2 and 3. These two models had similar C-statistic. Model 5 had the smallest deviation and model 8 had the smallest bias. The addition of sex interaction terms did not improve model performance. The best models for predicting whether participants had FPG ≥ 7.0 mmol l−1 using HbA1c measurement were also models 5 and 8 (Extended Data Tables 2 and 4). The coefficients of these models are shown in Extended Data Tables 5 and 6.
In Fig. 3, the coefficients from model 8 were used to calculate the probability that a person without a history of diabetes diagnosis, based on measurement of a single glycemic biomarker that is below the clinical threshold, would have elevated level of the other (elevated HbA1c at a specific FPG and BMI level (Fig. 3a) or elevated FPG at a specific HbA1c and BMI level (Fig. 3b)). For example, in south Asia, people aged 55 years and older, without a previous diabetes diagnosis, with obesity (BMI ≥ 30 kg m−2), whose FPG is 6.5–6.9 mmol l−1 have a 29–63% probability of having elevated HbA1c. In contrast, the probability of having elevated HbA1c remained no higher than 17% for men and women of the same age and FPG level in the high-income western region and central and eastern Europe, which means that screen-detected diabetes that is manifested as isolated elevated HbA1c is relatively rare in these two regions. For those whose HbA1c was measured, the probability of having elevated FPG was below 30% in every region except central and eastern Europe; the probability surpassed 20% only in those with high BMI and HbA1c levels.
a,b, The probability, by sex, age and region, of participants who did not have previous diagnosis of diabetes of having elevated HbA1c (≥6.5%) at different FPG and BMI levels (a) and elevated FPG (≥7.0 mmol l−1) at different HbA1c and BMI levels (b). The probabilities were calculated using coefficients of prediction equation model 8, with measurement method set to laboratory for prediction. These results show the probability of having screen-detected diabetes if the second biomarker had been measured, for a person whose first biomarker was below the clinical threshold for diabetes diagnosis.
In Fig. 4, the coefficients from model 8 were used to calculate the probability that a person without a history of diabetes diagnosis, based on measurement of a single glycemic biomarker that is above the clinical threshold, would have elevated level of the other (elevated HbA1c at a specific FPG and BMI level (Fig. 4a) or elevated FPG at a specific HbA1c and BMI level (Fig. 4b)). These results show that people without a previous diagnosis who had an elevated level of one diabetes biomarker had varying probabilities of also being elevated for the other depending on region, age, sex and BMI. In particular, for those with screen-detected elevated HbA1c, the probability of also having FPG ≥ 7.0 mmol l−1 surpassed 90% in some region-age-BMI combinations. The exceptions were south Asia and Latin America and the Caribbean, where isolated elevated HbA1c and isolated elevated FPG were both common and hence only partially predicted one another.
a,b, The probability by sex, age and region of participants who did not have a previous diagnosis of diabetes of having elevated HbA1c (≥6.5%) at different FPG and BMI levels (a) and elevated FPG (≥7.0 mmol l−1) at different HbA1c and BMI levels (b). The probabilities were calculated using coefficients of prediction equation model 8, with measurement method set to laboratory for prediction. These results show the probability that the second biomarker, had it been measured, would be above the clinical threshold for diabetes diagnosis, for a person whose first biomarker was above the clinical threshold for diabetes diagnosis. Having elevated levels of both biomarkers has high positive predictive value for subsequent clinical diagnosis and risk of complications14,47.
Discussion
Our analysis of pooled global data showed that the use of either FPG or HbA1c alone might substantially underestimate the burden of diabetes relative to the number of people who would have elevated levels of either glycemic measure, especially in low- and middle-income countries where diagnosis rates are currently low. We also presented prediction equations to help allocate finite resources for measurement of HbA1c in settings where FPG (but not HbA1c) is routinely measured due to logistic or cost constraints. The prediction equations can also be used to enhance diabetes surveillance, to adjust the estimated prevalence in the majority of population-based health surveys which measure only one biomarker.
Our results, based on a large number of studies from different regions of the world, are consistent with a previous smaller study with data from mostly high-income western countries43 and with the collective results from studies done in individual countries22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42 in identifying substantial variation in diabetes classified by FPG versus HbA1c across regions. None of the previous studies had sufficient geographical coverage or participants to robustly quantify regional differences in how those with previously undiagnosed diabetes that were identified based on elevation of FPG and HbA1c, in isolation or together, as we did. A study using baseline data from the ORIGIN trial48, which covered people with diabetes or prediabetes from 40 countries, did not quantify the concordance and discordance of diabetes based on different biomarkers but its graphical results indicated smaller differences in FPG-HbA1c relationship between Europe and north America than between these regions and Asia or south America. We found that sex, age and BMI were predictors of having concordant versus discordant elevated FPG and elevated HbA1c, which is consistent with results from studies in individual countries22,32,34,40,49. Finally, to our knowledge, our prediction equations are the only global and generalizable tool for predicting the probability of being classified as having diabetes based on one glycemic biomarker based on measurement of another. A previous regression related HbA1c to average glucose50 (but not fasting glucose). This relationship is currently used by the American Diabetes Association for assessing glycemic control51 and not for inferring new diagnosis of diabetes. It used data from only 507 individuals, 422 of whom were non-Hispanic White. The data came from ten centers, of which nine were in the United States and Europe. Over half (268) had type 1 diabetes, which is the less common form of diabetes in adults. The conversions did not account for other traits such as BMI and age, nor was the performance of the prediction equation validated in data that were not used in its derivation.
The strengths of our study include the amount, quality and geographical diversity of data, with studies from seven of eight major world regions. We carefully checked that data on biomarkers of diabetes and previous diagnosis were of high quality and consistent across studies as stated in detail in the Methods. The scale, quality and consistency of data allowed the characterization of the relationship between these glycemic biomarkers and the development of prediction equations that can inform the allocation of resources toward closing the global diagnosis and monitoring gaps.
Our study is also affected by limitations that apply to data pooling analyses, especially those that use data collected in different countries and time periods. Despite our extensive efforts to identify and access data, we had limited data in some regions and none from Pacific island nations in the Oceania region. We did not analyze concordance and discordance with OGTT because few studies, mostly from high-income countries, had data on all three glycemic biomarkers and because the use of OGTT in clinical settings is largely for diagnosis of gestational diabetes and not for population surveillance. The use of OGTT would identify additional people as having diabetes above and beyond those identified with FPG and HbA1c25,28. We did not analyze time trends of diagnosed and screen-detected diabetes, which should be the subject of future work, as conducted for hypertension52. Although we checked all data sources and their characteristics thoroughly, and accounted for whether a study had measured FPG and HbA1c in a laboratory or using a portable device, other unobserved differences might remain due to differing methods. Examples include differences in assays used for measuring FPG and HbA1c. We attempted to mitigate these differences by limiting our data to studies with mid-year of 2000 and later, a period over which HbA1c assays were more likely to be standardized, and by including the study-level random effects in our models, which remove the influence of unobserved differences across studies. Beyond our finding that the results were not sensitive to exclusion of studies that used a portable device (Extended Data Table 7), studies that have tested different devices on the same set of samples have found high correlations (>0.97) among their measurements and between these devices and reference laboratory methods53,54. We did not have consistent data from all studies on other potential determinants of concordant versus discordant elevated levels of FPG and HbA1c, such as genetics, fasting duration, time between puncture and centrifuge, measures of insulin resistance and pre-existing disease status and comorbidities (for example, liver disease, hemoglobinopathies and anemia) that might have differential influence on FPG and HbA1c. These variables should ideally be the subject of coordinated multicenter studies with consistent data collection methods in different regions and populations; however, such studies would be very costly especially as the number of outcomes and variables increases. There is intraindividual variation in FPG, and to a lesser extent HbA1c55, which could reduce the concordance between FPG and HbA1c, and repeated measurements of FPG may improve its concordance with HbA1c39. Finally, while the studies that were used to define the diagnostic cutoff points were all based on single measurements of glycemia8,56, as are epidemiological and surveillance studies44,57,58,59, many clinical guidelines recommend using a second confirmatory test for diabetes diagnosis and initiating treatment10,11,12,13 (we note that there is variation in this guidance, for example while the American Diabetes Association requires two above-threshold tests for diagnosing diabetes in most cases10, the European Association for the Study of Diabetes only advises doing so11, the World Health Organization only recommends repeated testing for asymptomatic patients13, and the International Diabetes Federation further limits repeated testing to when the first measurement is close to the threshold for diagnosis12). A key reason for clinical guidelines recommending a confirmatory test is to minimize risks of erroneous results, for example, due to mis-recording of laboratory results or large intraindividual variability (which is more relevant for FPG than HbA1c), potentially leading to a lifelong (mis-)diagnosis for an individual patient. This is not a relevant issue in prevalence studies in a population, as random measurement error and fluctuations in one direction are approximately balanced by those in the opposite direction. Reflecting the difference between the clinical and epidemiological approaches to diabetes definition, we referred to those without a previous diagnosis who had biomarker levels above the clinical thresholds as screen-detected diagnosis, and our prediction equations should be considered a tool for triaging some people at specific levels of FPG for measurement of HbA1c, and possibly vice versa, rather than a tool for conferring a diagnosis.
The observed variation in the composition of screen-detected diabetes across regions may be due to a number of factors. Some genetic and phenotypic factors that affect fasting glucose and glucose metabolism through their effects on β-cell function and insulin sensitivity may be more common in some regions or ethnic groups60,61,62,63,64. Other non-glycemic factors, including anemia due to iron deficiency or malaria, certain hemoglobin variants (for example, HbS and HbF), other hemoglobinopathies, polycythemia due to living in high altitude, liver and kidney diseases, HIV and certain drugs such as antiretroviral therapy for HIV, can also affect HbA1c and FPG differently65,66,67,68,69,70,71,72,73,74,75,76,77. Some of these factors, including malaria-induced and iron deficiency anemia, hemoglobinopathies such as sickle cell disease and thalassemia, and antiretroviral therapy, are more prevalent in parts of Asia and Africa78,79,80, and may have shifted the population distribution of HbA1c or affected its measurement77. One study from South Africa found that the impact of these factors on HbA1c were small81. Guidelines recommend the use of a glucose test for diabetes diagnosis in those with such conditions10. Smoking and alcohol use, which vary geographically, may differentially affect HbA1c and FPG82,83. Finally, the composition of diabetes that was detected through screening in the survey depends on whether those with a previous diagnosis were identified based on FPG or HbA1c. For example, with increasing use of HbA1c in clinical settings in high-income countries84, a smaller proportion of people with screen-detected diabetes would have elevated HbA1c.
Although both FPG and HbA1c are associated with increased risk of microvascular and macrovascular complications2,85,86, the current evidence on the health implications of having discordant versus concordant elevation of FPG and HbA1c is limited. The few available studies found worse outcomes on the health risks associated with concordant elevation of FPG and HbA1c than discordant elevation, but had mixed findings about how isolated elevation of the two biomarkers compare39,87,88. To the extent that both FPG and HbA1c are predictors of risk of complications and mortality, reliance on a single biomarker may miss or delay diagnosis of diabetes in some people and hence increase their risk of complications. This issue is especially relevant in low- and middle-income countries where resource constraints make FPG the more common approach to diagnosis, possibly because the measurement of HbA1c requires equipment or reagents that are more costly or because standardization of the HbA1c laboratory process requires specialist training that is not as widely available89,90,91,92,93. With finite resources, our prediction equations can help to triage some people for the measurement of a second biomarker, often HbA1c, and enhance early detection of diabetes and close the global diagnosis shortfall14. For surveillance, the use of a single biomarker, so far largely FPG44,45,46, underestimates the burden of diabetes and does so to a larger extent in low- and middle-income countries where a larger share of conditions such as diabetes (and hypertension52) remains undiagnosed. Our prediction equations can help provide a more complete picture of the burden of diabetes in different regions.
Methods
The pooled analysis was approved by Imperial College London Research Ethics Committee and complies with all relevant ethical regulations. The participating studies followed their institutional approval process at the time of data collection.
Data
We used data collated by the NCD-RisC. The data sources included national and multi-country measurement surveys that were either publicly available or identified and accessed through contacts with relevant government or academic partners. Additionally, we searched and reviewed published studies as detailed previously44 and invited eligible studies to join NCD-RisC, as we did with participating studies in previous pooled analyses of cardiometabolic risk factors96,97,98,99. The NCD-RisC database is continuously updated through the above routes and through periodic requests to NCD-RisC members to suggest additional sources in their countries.
The inclusion criteria for this analysis were (1) data were collected using a probabilistic sampling method with a defined sampling frame; (2) data were from population samples at the national, subnational (defined as covering one or more subnational regions, more than three urban communities or more than five rural communities) or community level (defined as having up to three urban communities or up to five rural communities); and (3) both FPG and HbA1c were measured. Studies were excluded if they had (1) enrolled participants based on health status or cardiovascular risk; (2) were conducted only among ethnic minorities or specific educational, occupational or other socioeconomic subgroups; (3) recruited participants through health facilities, except studies based on the primary care system in high-income and central European countries with universal insurance; (4) had not measured either FPG or HbA1c; (5) had not instructed participants to fast for at least 6 h before FPG measurement; (6) had only measured FPG or HbA1c in the subset of participants who had known diabetes; (7) had measured HbA1c only in a subset of participants selected based on their levels of FPG and vice versa; (8) had not collected information on a previous diagnosis of diabetes; and (9) their mid-year was before 2000, before HbA1c assays were widely standardized100.
At least two independent people ascertained that each data source met the inclusion criteria. All NCD-RisC members were asked to review the list of data sources from their country, to verify that the included data met the inclusion criteria and were not duplicates. When FPG and/or HbA1c data were missing for more than 10% of participants in a survey, we checked the study design documentation to verify missingness at random so that the above inclusion criteria were met. Questions and clarifications were discussed with NCD-RisC members and resolved before data were incorporated in the database. For each data source, we recorded the study population, sampling approach, years of measurement and measurement methods, including whether FPG and HbA1c were measured in a laboratory or using a portable point-of-care device. In 11 studies, fasting glucose was measured in capillary whole blood; four of these used equipment that reported plasma-equivalent values. We converted the measurements from the other seven studies to plasma-equivalent using the relationship in a study that compared different types of specimens101. In a sensitivity analysis, we excluded these 11 studies from the analysis.
We established whether a participant had diagnosed diabetes using questions worded as variations of ‘Have you ever been told by a doctor or other health professional that you had diabetes, also called high blood sugar?’ In some surveys, the question on previous diabetes diagnosis was asked only if a participant had answered ‘yes’ to an earlier question, usually worded as ‘Have you ever been screened for diabetes?’ or ‘Have you ever had your blood glucose measured?’. In these cases, participants who answered ‘no’ to the first question were coded as not having been diagnosed with diabetes. We also considered participants who used diabetes medication such as metformin or insulin as having diabetes. Survey data typically do not separate type 1 and type 2 diabetes in adults, but studies that had data on these subtypes show that most (85–95%) cases of diabetes in adults are type 2 diabetes102.
The data cleaning and use process is summarized in Fig. 1 and the list of data sources and their characteristics are stated in Supplementary Table 1.
Statistical analysis
We divided the participants into those who had a previous diagnosis of diabetes (hereafter referred to as diagnosed diabetes), those without a previous diagnosis of diabetes who had elevated FPG (FPG ≥ 7.0 mmol l−1) and/or elevated HbA1c (HbA1c ≥ 6.5%) (referred to as screen-detected diabetes) and the remainder who did not have a previous diagnosis, elevated FPG, or elevated HbA1c. We conducted the following three analyses.
Screen-detected diabetes by FPG and HbA1c
We graphically presented how total diabetes is divided into diagnosed and screen-detected diabetes, and how screen-detected diabetes is further divided into those manifested as only elevated FPG (FPG ≥ 7.0 mmol l−1 and HbA1c < 6.5%, referred to as isolated elevated FPG), only elevated HbA1c (HbA1c ≥ 6.5% and FPG < 7.0 mmol l−1, referred to as isolated elevated HbA1c) or elevated levels of both FPG and HbA1c. We report crude and age-standardized prevalence. We calculated crude prevalence using data from all participants regardless of age. We calculated age-standardized prevalence as the weighted mean of the age-specific values using the World Health Organization standard population103. We also graphically described the relationship of FPG and HbA1c among people without diagnosed diabetes.
Association with individual and study characteristics
We fitted regression models to examine what individual and study-level factors were associated with whether participants with screen-detected diabetes were identified by elevated FPG, elevated HbA1c or elevated levels of both. We fitted three separate log-binomial regressions, with each of the three outcomes (isolated elevated FPG, isolated elevated HbA1c and elevated levels of both) as a distinct dependent variable. A log-binomial regression estimates the association of each independent variable with the probability of a participant falling in each of the three categories as PR. The individual level independent variables were sex, age and BMI; the study-level variables were region, study year, whether FPG and HbA1c were measured in a laboratory or using a portable device (to account for differences in measurement between them53,54) and percentage of participants with diabetes who had been diagnosed before in each study. The regressions also included a study-level random effect to account for unobserved factors that led to systematic differences in each study compared to others104,105.
We fitted the log-binomial regressions using Bayesian model fitting implemented in MultiBUGS (v.2.0)106. Bayesian model fitting has better estimation performance for log-binomial model than a frequentist approach107. We used a normal distribution with mean of zero and s.d. of 0.01 as the prior for the regression coefficients and a uniform distribution on 0.01–2.00 as the prior for the s.d. of study-level random effects. We ran four chains and assessed convergence visually using trace plots. After burn-in and thinning, we kept 50,000 draws to represent the posterior distributions of the PRs. We report PRs and their 95% CrIs as the mean and the 2.5th and 97.5th percentiles of their posterior distributions. We report the posterior probability that a PR with posterior mean estimate >1.0 is less than one and vice versa for PRs <1.0; the posterior probabilities are analogous to P values in a frequentist analysis.
Prediction equations
We tested nine logistic regression models for estimating the probability that a person without diagnosed diabetes at a specific level of FPG had an HbA1c over the clinical threshold for diabetes (HbA1c ≥ 6.5%). The variables in the models were selected based on clinical and epidemiological relevance and data availability. The variables included FPG as well as sex, age, BMI, glycemic measurement method (laboratory based or via a portable device) and region. The nine prediction models (Extended Data Table 2) differed by the predictors included and whether the coefficient of the FPG term was allowed to vary by sex and region. In all models, we included a study-level random effect to account for unobserved factors that led to systematic differences in each study compared to others104,105. We also tested the inclusion of nonlinear (square and cubic) terms of FPG, year of data collection and other interaction terms; these models performed worse than those without the additional terms as evaluated by the metrics below and are not presented. We did not interact age, which is a continuous variable, with FPG and other terms, to avoid overfitting. We fitted and evaluated all prediction models in R (v.4.2.1)108.
We assessed the performance of the models in predicting (1) individual participants’ status of having HbA1c ≥ 6.5% based on their FPG and (2) the prevalence of HbA1c ≥ 6.5% for an entire study. The performance at the individual level reflects how well the prediction equation works for triaging patients for further measurement for diabetes, and the performance at study (or population) level assesses how well it works for diabetes surveillance. We used the C-statistic to assess individual-level performance and mean error and mean absolute error between the predicted and observed prevalence for population-level performance. The C-statistic measures how well a prediction equation distinguishes individuals with higher risk from those with lower risk. Mean error assesses whether there is systematic difference (bias) in the predicted prevalence compared to the observed one and mean absolute error assesses any deviation of the predicted prevalence from the observed prevalence. We calculated error by study, sex and age group (18–39 years, 40–59 years and 60 years and older).
We evaluated the performance of the models in 20 rounds of tenfold cross-validation109. In each fold of each round, we held out all data from a random 10% of studies, fitted the model to the data from the remaining 90% of studies and made estimates for the held-out observations. We repeated this process ten times, each time holding out a different 10% of studies so that each study was held out exactly once. We calculated the above individual-level and population-level performance metrics for all held-out observations. We repeated the tenfold cross-validation 20 times and report the means and ranges of the performance metrics from all 20 rounds.
We repeated the same process for predicting the probability of having FPG ≥ 7.0 mmol l−1 based on HbA1c.
Ethics and inclusion
This research followed the recommendations set out in the Global Code of Conduct for Research in Resource-Poor Settings.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Data used in this research are governed by data-sharing protocols of participating studies. Contact information for data providers can be obtained from www.ncdrisc.org and https://doi.org/10.5281/zenodo.8169145.
Code availability
The computer code for the log-binomial regression in this work is available at www.ncdrisc.org and https://doi.org/10.5281/zenodo.8169145.
References
Tomic, D., Shaw, J. E. & Magliano, D. J. The burden and risks of emerging complications of diabetes mellitus. Nat. Rev. Endocrinol. 18, 525–539 (2022).
Emerging Risk Factors Collaboration. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 375, 2215–2222 (2010).
Cheng, G., Huang, C., Deng, H. & Wang, H. Diabetes as a risk factor for dementia and mild cognitive impairment: a meta-analysis of longitudinal studies. Intern. Med. J. 42, 484–491 (2012).
Tsilidis, K. K., Kasimis, J. C., Lopez, D. S., Ntzani, E. E. & Ioannidis, J. P. Type 2 diabetes and cancer: umbrella review of meta-analyses of observational studies. Brit. Med. J. 350, g7607 (2015).
Mahamat-Saleh, Y. et al. Diabetes, hypertension, body mass index, smoking and COVID-19-related mortality: a systematic review and meta-analysis of observational studies. BMJ Open 11, e052777 (2021).
Foe-Essomba, J. R. et al. Diabetes mellitus and tuberculosis, a systematic review and meta-analysis with sensitivity analysis for studies comparable for confounders. PLoS ONE 16, e0261246 (2021).
The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 20, 1183–1197 (1997).
International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 32, 1327–1334 (2009).
World Health Organization. Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus. https://www.who.int/publications/i/item/use-of-glycated-haemoglobin-(-hba1c)-in-diagnosis-of-diabetes-mellitus (2011).
ElSayed, N. A. et al. 2. Classification and diagnosis of diabetes: standards of care in diabetes-2023. Diabetes Care 46, S19–S40 (2023).
Cosentino, F. et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 41, 255–323 (2020).
International Diabetes Federation. IDF clinical practice recommendations for managing type 2 diabetes in primary care. https://d-net.idf.org/en/library/466-managing-type-2-diabetes-in-primary-care.html (2017).
World Health Organization. Classification of diabetes mellitus. https://www.who.int/publications/i/item/classification-of-diabetes-mellitus (2019).
Selvin, E., Wang, D., Matsushita, K., Grams, M. E. & Coresh, J. Prognostic implications of single-sample confirmatory testing for undiagnosed diabetes: a prospective cohort study. Ann. Intern. Med. 169, 156–164 (2018).
Higgins, T. HbA1c for screening and diagnosis of diabetes mellitus. Endocrine 43, 266–273 (2013).
Sacks, D. B. A1c versus glucose testing: a comparison. Diabetes Care 34, 518–523 (2011).
Abdul-Ghani, M. A., Tripathy, D. & DeFronzo, R. A. Contributions of β-cell dysfunction and insulin resistance to the pathogenesis of impaired glucose tolerance and impaired fasting glucose. Diabetes Care 29, 1130–1139 (2006).
Ogurtsova, K. et al. IDF Diabetes Atlas: global estimates of undiagnosed diabetes in adults for 2021. Diabetes Res. Clin. Pract. 183, 109118 (2022).
Christensen, D. L. et al. Moving to an A1c-based diagnosis of diabetes has a different impact on prevalence in different ethnic groups. Diabetes Care 33, 580–582 (2010).
Bennett, C. M., Guo, M. & Dharmage, S. C. HbA(1c) as a screening tool for detection of type 2 diabetes: a systematic review. Diabet. Med. 24, 333–343 (2007).
Kaur, G. et al. Diagnostic accuracy of tests for type 2 diabetes and prediabetes: a systematic review and meta-analysis. PLoS ONE 15, e0242415 (2020).
Carson, A. P., Reynolds, K., Fonseca, V. A. & Muntner, P. Comparison of A1c and fasting glucose criteria to diagnose diabetes among US adults. Diabetes Care 33, 95–97 (2010).
Ho-Pham, L. T., Nguyen, U. D. T., Tran, T. X. & Nguyen, T. V. Discordance in the diagnosis of diabetes: comparison between HbA1c and fasting plasma glucose. PLoS ONE 12, e0182192 (2017).
Lipska, K. J. et al. Identifying dysglycemic states in older adults: implications of the emerging use of hemoglobin A1c. J. Clin. Endocrinol. Metab. 95, 5289–5295 (2010).
Nazir, A. et al. Prevalence of diabetes in Asian Indians based on glycated hemoglobin and fasting and 2-h post-load (75-g) plasma glucose (CURES-120). Diabetes Technol. Ther. 14, 665–668 (2012).
Rathmann, W. et al. Hemoglobin A1c and glucose criteria identify different subjects as having type 2 diabetes in middle-aged and older populations: the KORA S4/F4 Study. Ann. Med. 44, 170–177 (2012).
Wade, A. N. et al. Concordance between fasting plasma glucose and HbA1c in the diagnosis of diabetes in black South African adults: a cross-sectional study. BMJ Open 11, e046060 (2021).
Cowie, C. C. et al. Prevalence of diabetes and high risk for diabetes using A1c criteria in the US population in 1988–2006. Diabetes Care 33, 562–568 (2010).
Kharroubi, A. T., Darwish, H. M., Abu Al-Halaweh, A. I. & Khammash, U. M. Evaluation of glycated hemoglobin (HbA1c) for diagnosing type 2 diabetes and prediabetes among Palestinian Arab population. PLoS ONE 9, e88123 (2014).
Abdul Murad, N. A. et al. Discordance between fasting plasma glucose (FPG) and HbA1c in diagnosing diabetes and pre-diabetes in the Malaysian cohort. J. ASEAN Fed. Endocr. Soc. 36, 127–132 (2021).
Davidson, M. B. & Schriger, D. L. Effect of age and race/ethnicity on HbA1c levels in people without known diabetes mellitus: implications for the diagnosis of diabetes. Diabetes Res. Clin. Pract. 87, 415–421 (2010).
Jeon, J. Y. et al. Prevalence of diabetes and prediabetes according to fasting plasma glucose and HbA1c. Diabetes Metab. J. 37, 349–357 (2013).
Mo, M. et al. Combining glycosylated hemoglobin A1c and fasting plasma glucose for diagnosis of type 2 diabetes in Chinese adults. BMC Endocr. Disord. 13, 44 (2013).
Rathod, S. D. et al. Glycated haemoglobin A1c (HbA1c) for detection of diabetes mellitus and impaired fasting glucose in Malawi: a diagnostic accuracy study. BMJ Open 8, e020972 (2018).
Rosella, L. C., Lebenbaum, M., Fitzpatrick, T., Zuk, A. & Booth, G. L. Prevalence of prediabetes and undiagnosed diabetes in Canada (2007-2011) according to fasting plasma glucose and HbA1c screening criteria. Diabetes Care 38, 1299–1305 (2015).
Takahashi, Y. et al. Prevalence of diabetes estimated by plasma glucose criteria combined with standardized measurement of HbA1c among health checkup participants on Miyako Island, Japan. Diabetes Care 23, 1092–1096 (2000).
Unwin, N. et al. Prevalence and phenotype of diabetes and prediabetes using fasting glucose vs HbA1c in a Caribbean population. J. Glob. Health 7, 020407 (2017).
Zhang, Y. H. et al. Diabetes and pre-diabetes as determined by glycated haemoglobin A1c and glucose levels in a developing southern Chinese population. PLoS ONE 7, e37260 (2012).
Selvin, E., Steffes, M. W., Gregg, E., Brancati, F. L. & Coresh, J. Performance of A1c for the classification and prediction of diabetes. Diabetes Care 34, 84–89 (2011).
Rathmann, W., Bongaerts, B. & Kostev, K. Association of characteristics of people with type 2 diabetes mellitus with discordant values of fasting glucose and HbA1c. J. Diabetes 10, 934–941 (2018).
Falguera, M. et al. Prevalence of pre-diabetes and undiagnosed diabetes in the Mollerussa prospective observational cohort study in a semi-rural area of Catalonia. BMJ Open 10, e033332 (2020).
Soulimane, S. et al. Comparing incident diabetes as defined by fasting plasma glucose or by HbA(1c). The AusDiab, Inter99 and DESIR studies. Diabet. Med. 28, 1311–1318 (2011).
NCD Risk Factor Collaboration (NCD-RisC). Effects of diabetes definition on global surveillance of diabetes prevalence and diagnosis: a pooled analysis of 96 population-based studies with 331 288 participants. Lancet Diabetes Endocrinol. 3, 624–637 (2015).
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 387, 1513–1530 (2016).
Sun, H. et al. IDF Diabetes Atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 183, 109119 (2022).
World Health Organization. Global action plan for the prevention and control of noncommunicable diseases 2013–2020. http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf?ua=1 (2013).
Narayan, K. M. V. & Jagannathan, R. Two in one: diagnosing type 2 diabetes with single-sample testing. Ann. Intern. Med. 169, 193–194 (2018).
Ramachandran, A., Riddle, M. C., Kabali, C. & Gerstein, H. C., ORIGIN Investigators. Relationship between A1c and fasting plasma glucose in dysglycemia or type 2 diabetes: an analysis of baseline data from the ORIGIN trial. Diabetes Care 35, 749–753 (2012).
Balkau, B. et al. Are the same clinical risk factors relevant for incident diabetes defined by treatment, fasting plasma glucose, and HbA1c? Diabetes Care 34, 957–959 (2011).
Nathan, D. M. et al. Translating the A1C assay into estimated average glucose values. Diabetes Care 31, 1473–1478 (2008).
ElSayed, N. A. et al. 6. Glycemic targets: standards of care in diabetes-2023. Diabetes Care 46, S97–S110 (2023).
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 398, 957–980 (2021).
Pfutzner, A. et al. Clinical assessment of the accuracy of blood glucose measurement devices. Curr. Med. Res. Opin. 28, 525–531 (2012).
Sutheran, H. L. & Reynolds, T. Technical and clinical accuracy of three blood glucose meters: clinical impact assessment using error grid analysis and insulin sliding scales. J. Clin. Pathol. 69, 899–905 (2016).
Selvin, E., Crainiceanu, C. M., Brancati, F. L. & Coresh, J. Short-term variability in measures of glycemia and implications for the classification of diabetes. Arch. Intern. Med. 167, 1545–1551 (2007).
Colagiuri, S. et al. Glycemic thresholds for diabetes-specific retinopathy: implications for diagnostic criteria for diabetes. Diabetes Care 34, 145–150 (2011).
Ali, M. K. et al. Achievement of goals in US diabetes care, 1999–2010. N. Engl. J. Med. 368, 1613–1624 (2013).
Menke, A., Casagrande, S., Geiss, L. & Cowie, C. C. Prevalence of and trends in diabetes among adults in the United States, 1988-2012. JAMA 314, 1021–1029 (2015).
Kazemian, P., Shebl, F. M., McCann, N., Walensky, R. P. & Wexler, D. J. Evaluation of the cascade of diabetes care in the United States, 2005-2016. JAMA Intern. Med. 179, 1376–1385 (2019).
Kahn, S. E. The relative contributions of insulin resistance and β-cell dysfunction to the pathophysiology of type 2 diabetes. Diabetologia 46, 3–19 (2003).
Ashcroft, F. M. & Rorsman, P. Diabetes mellitus and the β cell: the last ten years. Cell 148, 1160–1171 (2012).
Ramachandran, A., Ma, R. C. & Snehalatha, C. Diabetes in Asia. Lancet 375, 408–418 (2010).
Motala, A. A., Mbanya, J. C., Ramaiya, K., Pirie, F. J. & Ekoru, K. Type 2 diabetes mellitus in sub-Saharan Africa: challenges and opportunities. Nat. Rev. Endocrinol. 18, 219–229 (2022).
Wheeler, E. et al. Impact of common genetic determinants of hemoglobin A1c on type 2 diabetes risk and diagnosis in ancestrally diverse populations: a transethnic genome-wide meta-analysis. PLoS Med. 14, e1002383 (2017).
English, E. et al. The effect of anaemia and abnormalities of erythrocyte indices on HbA1c analysis: a systematic review. Diabetologia 58, 1409–1421 (2015).
Bleyer, A. J. et al. The impact of sickle cell trait on glycated haemoglobin in diabetes mellitus. Diabet. Med. 27, 1012–1016 (2010).
Klonoff, D. C. Hemoglobinopathies and hemoglobin A1c in diabetes mellitus. J. Diabetes Sci. Technol. 14, 3–7 (2020).
Monroe, A. K., Glesby, M. J. & Brown, T. T. Diagnosing and managing diabetes in HIV-infected patients: current concepts. Clin. Infect. Dis. 60, 453–462 (2015).
Christiansen, R., Rasmussen, L. M., Nybo, H., Steenstrup, T. & Nybo, M. The relationship between HbA1c and fasting plasma glucose in patients with increased plasma liver enzyme measurements. Diabet. Med. 29, 742–747 (2012).
Jung, M. et al. Performance of non-traditional hyperglycemia biomarkers by chronic kidney disease status in older adults with diabetes: results from the Atherosclerosis Risk in Communities Study. J. Diabetes 10, 276–285 (2018).
Little, R. R., La’ulu, S. L., Hanson, S. E., Rohlfing, C. L. & Schmidt, R. L. Effects of 49 different rare Hb variants on HbA1c measurement in eight methods. J. Diabetes Sci. Technol. 9, 849–856 (2015).
Cohen, R. M. et al. Red cell life span heterogeneity in hematologically normal people is sufficient to alter HbA1c. Blood 112, 4284–4291 (2008).
Bazo-Alvarez, J. C. et al. Glycated haemoglobin (HbA1c) and fasting plasma glucose relationships in sea-level and high-altitude settings. Diabet. Med. 34, 804–812 (2017).
Unnikrishnan, R., Anjana, R. M. & Mohan, V. Drugs affecting HbA1c levels. Indian J. Endocrinol. Metab. 16, 528–531 (2012).
Kasujja, F. X., Nuwaha, F., Ekirapa, E. K., Kusolo, R. & Mayega, R. W. The association between asymptomatic malaria and blood glucose among outpatients in a rural low-income setting. Diabetes Epidemiol. Manage. 9, 100112 (2023).
Ahmad, J. & Rafat, D. HbA1c and iron deficiency: a review. Diabetes Metab. Syndr. 7, 118–122 (2013).
National Glycohemoglobin Standardization Program. Factors that interfere with HbA1c test results. https://ngsp.org/factors.asp (2022).
Williams, T. N. & Weatherall, D. J. World distribution, population genetics, and health burden of the hemoglobinopathies. Cold Spring Harb. Perspect. Med. 2, a011692 (2012).
Stevens, G. A. et al. National, regional, and global estimates of anaemia by severity in women and children for 2000-19: a pooled analysis of population-representative data. Lancet Glob. Health 10, e627–e639 (2022).
Piel, F. B. et al. Global epidemiology of sickle haemoglobin in neonates: a contemporary geostatistical model-based map and population estimates. Lancet 381, 142–151 (2013).
Hird, T. R. et al. HIV infection and anaemia do not affect HbA1c for the detection of diabetes in black South Africans: evidence from the Durban Diabetes Study. Diabet Med. 38, e14605 (2021).
Soulimane, S. et al. HbA1c, fasting and 2 h plasma glucose in current, ex- and never-smokers: a meta-analysis. Diabetologia 57, 30–39 (2014).
Schrieks, I. C., Heil, A. L., Hendriks, H. F., Mukamal, K. J. & Beulens, J. W. The effect of alcohol consumption on insulin sensitivity and glycemic status: a systematic review and meta-analysis of intervention studies. Diabetes Care 38, 723–732 (2015).
Gillett, M. et al. The cost-effectiveness of testing strategies for type 2 diabetes: a modelling study. Health Technol. Assess. 19, 1–80 (2015).
Di Angelantonio, E. et al. Glycated hemoglobin measurement and prediction of cardiovascular disease. JAMA 311, 1225–1233 (2014).
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 37, S81–S90 (2014).
Woerle, H. J. et al. Diagnostic and therapeutic implications of relationships between fasting, 2-hour postchallenge plasma glucose and hemoglobin a1c values. Arch. Intern. Med. 164, 1627–1632 (2004).
Gujral, U. P. et al. Isolated HbA1c identifies a different subgroup of individuals with type 2 diabetes compared to fasting or post-challenge glucose in Asian Indians: the CARRS and MASALA studies. Diabetes Res. Clin. Pract. 153, 93–102 (2019).
Park, P. H. & Pastakia, S. D. Access to hemoglobin A1c in rural Africa: a difficult reality with severe consequences. J. Diabetes Res. 2018, 6093595 (2018).
Little, R. R. & Rohlfing, C. L. The long and winding road to optimal HbA1c measurement. Clin. Chim. Acta 418, 63–71 (2013).
Masis, L. et al. Estimating treatment costs for uncomplicated diabetes at a hospital serving refugees in Kenya. PLoS ONE 17, e0276702 (2022).
Jingi, A. M. et al. Access to diagnostic tests and essential medicines for cardiovascular diseases and diabetes care: cost, availability and affordability in the West Region of Cameroon. PLoS ONE 9, e111812 (2014).
Atun, R. et al. Diabetes in sub-Saharan Africa: from clinical care to health policy. Lancet Diabetes Endocrinol. 5, 622–667 (2017).
Shabbir, S. et al. Type and frequency of hemoglobinopathies, diagnosed in the area of Karachi, in Pakistan. Cogent. Med. 3, 1188875 (2016).
Breunig, M. M., Kriegel, H.-P., Ng, R. T. & Sander, J. LOF: identifying density-based local outliers. In Proc. 2000 ACM SIGMOD International Conference on Management of Data 93–104 (2000).
Farzadfar, F. et al. National, regional, and global trends in serum total cholesterol since 1980: systematic analysis of health examination surveys and epidemiological studies with 321 country-years and 3.0 million participants. Lancet 377, 578–586 (2011).
Finucane, M. M. et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet 377, 557–567 (2011).
Danaei, G. et al. National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5.4 million participants. Lancet 377, 568–577 (2011).
Danaei, G. et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet 378, 31–40 (2011).
American Diabetes Association. Implications of the Diabetes Control and Complications Trial. Diabetes Care 23, S24–S26 (2000).
Carstensen, B. et al. Measurement of blood glucose: comparison between different types of specimens. Ann. Clin. Biochem. 45, 140–148 (2008).
Bullard, K. M. et al. Prevalence of diagnosed diabetes in adults by diabetes type — United States, 2016. MMWR Morb. Mortal. Wkly. Rep. 67, 359–361 (2018).
Ahmad, O. B. et al. Age standardization of rates: a new WHO standard. GPE Discussion Paper Series: No.31 (2001).
Laird, N. M. & Ware, J. H. Random-effects models for longitudinal data. Biometrics 38, 963–974 (1982).
Feller, A. & Gelman, A. Hierarchical Models for Causal Effects. in Emerging Trends in the Social and Behavioral Sciences (eds Scott, R. A. & Kosslyn, S. M.) 1–16 (2015).
Goudie, R. J. B., Turner, R. M., De Angelis, D. & Thomas, A. MultiBUGS: a parallel implementation of the BUGS modelling framework for faster Bayesian inference. J. Stat. Softw. 95, 1–20 (2020).
Torman, V. B. & Camey, S. A. Bayesian models as a unified approach to estimate relative risk (or prevalence ratio) in binary and polytomous outcomes. Emerg. Themes Epidemiol. 12, 8 (2015).
R Core Team. R: a language and environment for statistical computing (2022).
Borra, S. & Di Ciaccio, A. Measuring the prediction error. A comparison of cross-validation, bootstrap and covariance penalty methods. Comput. Stat. Data Anal. 54, 2976–2989 (2010).
Acknowledgements
This study was funded by the UK Medical Research Council (grant number MR/V034057/1 to M.E.), the UK Research and Innovation (Research England Policy Support Fund to M.E.) and the US Centers for Disease Control and Prevention (to E.W.G.). B. Zhou is supported by a fellowship from the Abdul Latif Jameel Institute for Disease and Emergency Analytics, funded by a donation from Community Jameel, at Imperial College London. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. For the purpose of open access, the author has applied a Creative Commons Attribution license to the Author Accepted Manuscript version arising from this submission.
Author information
Authors and Affiliations
Consortia
Contributions
B. Zhou, K.E.S. and R.K.S. led the data collection and management. B. Zhou, J.E.B., A. Mishra, C.J.P., S.V.H. and M.E. developed the statistical method. B. Zhou coded the statistical method, conducted analyses and prepared results. The other authors contributed to the study design and collected, reanalyzed, checked and pooled the data. B. Zhou and M.E. wrote the first draft of the report. All other authors reviewed and commented on the draft report.
Corresponding author
Ethics declarations
Competing interests
A.N.W. reports an honorarium from Sanofi for serving as a panel member at an educational event on thyroid cancer. The authors are responsible for the views expressed in this article and they do not necessarily represent the views, decisions or policies of the institutions with which they are affiliated.
Peer review
Peer review information
Nature Medicine thanks Sarah Wild and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Jennifer Sargent, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Extent and composition of diagnosed and screen-detected diabetes by region and sex.
(a) Crude and age-standardized proportion of participants with diagnosed or screen-detected diabetes, and, for those without prior diagnosis, whether they had isolated elevated FPG (FPG ≥7.0 mmol/L and HbA1c < 6.5%), isolated elevated HbA1c (HbA1c ≥6.5% and FPG < 7.0 mmol/L) or elevated levels of both, and (b) crude and age-standardized proportion of participants with screen-detected diabetes who had isolated elevated FPG, isolated elevated HbA1c or elevated levels of both, by region and sex. Its contents are the same as the segment of Panel A that is below the zero line, scaled to 100% so that the composition of screen-detected diabetes can be compared across regions, regardless of its total prevalence. Having elevated levels of both biomarkers has high positive predictive value for subsequent clinical diagnosis and risk of complications14,47, and hence this group is similar to clinically-diagnosed diabetes. In panel A, regions are ordered by the total proportion of participants who had diagnosed and screen-detected diabetes. In panel B, regions are ordered by the crude proportion of participants with screen-detected diabetes who had elevated levels of both FPG and HbA1c.
Extended Data Fig. 2 Extent and composition of diagnosed and screen-detected diabetes by region, after removing two studies in Mauritius from sub-Saharan Africa.
(a) Crude and age-standardized proportion of participants with diagnosed or screen-detected diabetes, and, for those without prior diagnosis, whether they had isolated elevated FPG (FPG ≥7.0 mmol/L and HbA1c < 6.5%), isolated elevated HbA1c (HbA1c ≥6.5% and FPG < 7.0 mmol/L) or elevated levels of both, and (b) crude and age-standardized proportion of participants with screen-detected diabetes who had isolated elevated FPG, isolated elevated HbA1c or elevated levels of both, by region. Its contents are the same as the segment of Panel A that is below the zero line, scaled to 100% so that the composition of screen-detected diabetes can be compared across regions, regardless of its total prevalence. Having elevated levels of both biomarkers has high positive predictive value for subsequent clinical diagnosis and risk of complications14,47, and hence this group is similar to clinically-diagnosed diabetes. In panel A, regions are ordered by the total proportion of participants who had diagnosed and screen-detected diabetes. In panel B, regions are ordered by the crude proportion of participants with screen-detected diabetes who had elevated levels of both FPG and HbA1c. Regions are in the same order as in Fig. 2.
Extended Data Fig. 3 Relationship between FPG and HbA1c, among participants who had not been previously diagnosed with diabetes, by region.
The shading indicates the density of participants in each region, with darker shades corresponding to more participants and vice versa. The dotted lines are placed at FPG of 7.0 mmol/L and HbA1c of 6.5%, which are common clinical thresholds for diabetes10,11,12,13. The numbers on the panels indicate the Pearson correlation coefficient between FPG and HbA1c in each region. A total of 623 (0.2%) participants with FPG of 19-28 mmol/L and/or HbA1c of 12-17% are not shown in the figure so that the axes have sufficient resolution in ranges where the great majority of participants were.
Supplementary information
Supplementary Information
Supplementary Table 1.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
NCD Risk Factor Collaboration (NCD-RisC). Global variation in diabetes diagnosis and prevalence based on fasting glucose and hemoglobin A1c. Nat Med 29, 2885–2901 (2023). https://doi.org/10.1038/s41591-023-02610-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-023-02610-2