Abstract
Diabetes is increasing in Switzerland, but whether its management has improved is unknown. We aimed to assess diabetes prevalence, diagnosis, treatment, and control in French-speaking Switzerland. Our study used cross-sectional data for years 2005–2019 from a population-based study in Geneva, Switzerland. Overall prevalence (self-reported diagnosis and/or fasting plasma glucose level ≥ 7 mmol/L), diagnosed, treated (among diagnosed participants) and controlled diabetes (defined as a fasting plasma glucose FPG < 6.7 mmol/L among treated participants) were calculated for periods 2005–9, 2010–4 and 2015–9. Data from 12,348 participants (mean age ± standard deviation: 48.6 ± 13.5 years, 51.7% women) was used. Between 2005–9 and 2015–9, overall prevalence and frequency of diagnosed diabetes decreased (from 8.7 to 6.2% and from 7.0 to 5.2%, respectively). Among participants diagnosed with diabetes, treatment and control rates did not change from 44.1 to 51.9%, p = 0.251 and from 30.2 to 34.0%, p = 0.830, respectively. A trend towards higher treatment of participants with diabetes was found after multivariable adjustment, while no changes were found for overall prevalence, diagnosis, nor control. Among antidiabetic drugs, percentage of combinations increased from 12 to 23%; percentage of sulfonylureas and biguanides decreased from 15 to 6% and from 63 to 54%, respectively, while no trend was found for insulin. After multivariable analysis, women with diabetes were less likely to be treated but more likely to be controlled, the opposite association being found for obesity. In conclusion, in Canton Geneva, antidiabetic combination therapy is gaining importance, but only half of participants diagnosed with diabetes are treated, and glycaemic control remains poor.
Similar content being viewed by others
Introduction
Worldwide diabetes prevalence and incidence have increased significantly from 1990 to 2017. Population aging, as well as the rise in overweight and obesity, linked to suboptimal nutrition and sedentary lifestyles, has contributed to this tendency1,2. Diabetes, as one of the major causes of mortality and morbidity around the world, represents a constantly increasing global health burden3. However, control of diabetes and cardiovascular disease in Europe, including Switzerland, remains poor4,5.
National health surveys in Switzerland indicate only a minor increase of diabetes prevalence over the last years6. However, the probability of discovering an undiagnosed case of diabetes in the Swiss population, particularly among men, appears to be rising7. In addition, disparities in diabetes prevalence among various socioeconomic and cardiovascular risk groups in the Geneva population have increased over 13 years. Compared with adults with a higher socioeconomic background,disadvantaged adults were less aware of their diabetic condition8.
Swiss and international guidelines recommend metformin as first-line drug treatment for type 2 diabetes (T2DM), unless not well tolerated or contraindicated9,10. If necessary, other medications can be added to metformin, provided that renal function is normal and neither B12 deficiency nor polyneuropathy are present9. By adding other antidiabetic agents to metformin, improved control of glycated haemoglobin (HbA1c) and blood glucose levels is achieved11. In various countries the use of metformin and dipeptidyl peptidase IV inhibitors has increased12,13,14, whereas the use of sulfonylureas, glitazones, and α-glucosidase inhibitors has decreased15,16,17. However, there is insufficient evidence about how drug prescriptions have changed over time in Switzerland.
We thus aimed to assess the changes in diabetes management and antidiabetic drug administration in French-speaking Switzerland. Our hypothesis was that diabetes control has improved and that the number of antidiabetic drugs available and used in clinical practice has increased over the years.
Materials and methods
Participants
The Bus Santé study conducts annual health examination surveys since 1992 among circa 1000 men and women drawn from independent samples of residents aged 35–74 living in the state of Geneva, Switzerland18. The random selection in age and gender strata was proportional to the corresponding frequencies in the population. A first invitation letter was sent to a potential respondent; in the case of a non-response, up to seven telephone attempts were made to reach the person at different times of the day and on different days of the week, including Saturday and Sunday. If a selected person could not be reached by telephone, two further mailings were sent. One person who had not been reached after three mailings and seven phone calls was replaced following the same selection protocol. The recruitment of a potential subject took between 2 and 2 months19.
Diabetes information
Fasting plasma blood samples were collected and glucose levels were assayed using commercially available enzymatic kits (Bayer Technicon Diagnostics, CV 1.4%).
Diagnosed diabetes was defined as the participants reporting themselves as being diagnosed with diabetes. Diabetes prevalence was defined as a fasting plasma glucose level ≥ 7 mmol/L and/or being diagnosed with diabetes. Treated diabetes was defined among participants diagnosed with diabetes as the presence of any antidiabetic drug. Controlled diabetes was defined among participants treated for diabetes as a fasting plasma glucose level < 6.7 mmol/L. Antidiabetic drugs were self-reported and categorized into sulfonylureas, biguanides, insulin, others [thiazolidines, sulphonamides, sodium-glucose cotransporter-2 (SGLT-2) inhibitors, dipeptidyl peptidase 4 (DPP4) inhibitors and glucagon-like peptide 1 (GLP-1) agonists] and combinations (medicines containing any two or more of the previous categories).
Covariates
Socio-demographic data were self-reported. Nationality was categorized as Swiss and other. Marital status was categorized as single, married or in couple, divorced, and widowed. Educational level was categorized into primary, secondary, and tertiary. Smoking status was categorized as never, former (irrespective of the time since quitting) and current. Personal history of cardiovascular disease (CVD) was categorized as present/absent.
Height and weight were measured with participants in light clothes using standard procedures. Body mass index (BMI) was calculated and categorized as normal (< 25 kgm2), overweight (≥ 25 and < 30 kg/m2) and obese (≥ 30 kg/m2). Blood pressure (BP) was measured thrice in the sitting position on the right arm after at least 10 min rest using a standard protocol and a validated automated oscillometric sphygmomanometer. Hypertension was defined as a systolic BP ≥ 140 mm Hg and/or a diastolic BP ≥ 90 mm Hg and/or self-reported information of antihypertensive drug therapy.
Exclusion criteria
Participants were excluded if they a) missed any data about diabetes awareness and/or antidiabetic drug medication; b) had missing information for any covariate.
Statistical analysis
Descriptive results were presented as number of participants (percentage) for categorical variables or mean ± standard deviation for continuous variables. Bivariate analyses were performed using the chi-square test for categorical variables and the student’s t-test for continuous variables. Multivariable analysis was performed using logistic regression overall and stratified by gender, and the results were presented as odds ratio (OR) and 95% confidence interval (CI). Possible interactions between gender and BMI categories, hypertension, and history of CVD were also assessed. Statistical analyses were conducted using Stata version 17.0 for windows (Stata Corp, College Station, Texas, USA) and statistical significance was determined with p < 0.05 in a two-sided test.
Ethical statement
The Bus Santé study was approved by the local institutional review board (Commission Cantonale d’Ethique de la Recherche de Genève; IRB00003116). All research was performed in accordance with the relevant guidelines and regulations. All participants provided written informed consent20.
Results
Characteristics of participants
Comparison of the factors between included and excluded participants is summarized in Supplementary Table 1. Included participants were younger, had a lower BMI, and were more likely to have dyslipidaemia compared to excluded participants. The characteristics according to gender are summarized in Table 1. Women presented with a lower educational level, were more frequently of Swiss nationality, divorced, never smokers, with normal weight, and presented less frequently with hypertension or history of CVD.
Trends in diabetes prevalence, awareness, treatment, and control
The trends in diabetes prevalence, awareness, treatment, and control overall and stratified by gender are summarized in Table 2. Total and diagnosed diabetes prevalence (awareness) decreased overall and in men, while no changes were found in women, and in control rates. Treatment rates did not improve overall but increased in men.
Factors associated with diabetes prevalence, awareness, treatment, and control
The results of the bivariate analysis of the factors associated with diabetes prevalence, awareness, treatment, and control are summarized in Table 3. Participants with prevalent or diagnosed diabetes were less frequently women, older, had a lower educational level, were more frequently divorced and less frequently single, were more frequently former smokers, had a higher BMI and a higher frequency of obesity, hypertension, dyslipidaemia, and history of CVD.
Among participants diagnosed with diabetes, participants reporting being treated were less frequently women, were older, had a lower educational level, a higher BMI and a higher frequency of obesity, hypertension, and history of CVD (Table 3).
Among participants treated for diabetes, participants achieving adequate control were more frequently women and less frequently obese, while no significant difference was found for the other covariates (Table 3).
The results of the multivariable analysis of the factors associated with diabetes prevalence, awareness, treatment, and control are summarized in Table 4. Being a woman, increased educational level and being a Swiss national were negatively associated, while increased age, increased BMI, smoking, presence of hypertension or personal history of CVD were positively associated with diabetes prevalence. Similar findings were observed for diagnosis of diabetes, although being a woman, Swiss nationality or smoking status were no longer statistically relevant.
Being a woman was negatively associated with treatment of diabetes. Increased age, obese BMI, presence of hypertension or personal history of CVD were positively associated with treatment of diabetes. Being a woman was positively associated with diabetes control, while increased BMI was negatively associated with diabetes control.
Comparable findings were obtained when the analysis was stratified by gender (Supplementary Tables 2 and 3 for men and women, respectively), although several associations were no longer significant. Interaction analysis showed that women with hypertension had a higher likelihood of presenting with diabetes, being diagnosed, treated, and controlled than men, while men with history of CVD had a higher likelihood of presenting with diabetes than women; no significant interaction was found for BMI categories.
Multivariable analysis including dyslipidaemia is summarized in Supplementary Table 4. Presence of dyslipidaemia was positively associated with diabetes prevalence and awareness. After adjusting for dyslipidaemia, the association between diabetes prevalence and increased educational level or smoking was no longer statistically significant. After adjusting for dyslipidaemia, being a woman was additionally negatively associated with diagnosis of diabetes, while the association with educational level was no longer statistically significant. After adjusting for dyslipidaemia, divorced marital status was additionally positively associated with treatment of diabetes, while the association with presence of personal history of CVD was no longer statistically significant. After adjusting for dyslipidaemia, diabetes control remained positively associated with women gender and negatively associated with increased BMI.
Antidiabetic drugs
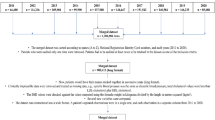
Trends in antidiabetic drugs expressed as percentage of all antidiabetic drugs are summarized overall and for each gender in Fig. 1. Percentage of antidiabetic combinations increased from 12% in 2005–9 to 23% in 2015–9. Percentage of sulfonylureas and biguanides decreased between 2005–9 and 2015–9 (15–6% for sulfonylureas and 63–54% for biguanides). Trends for insulin and other drugs were inconsistent. Similar findings were observed when the analysis was stratified by gender.
Discussion
This study aimed to assess diabetes prevalence, diagnosis, treatment, and control in the adult population of French-speaking Switzerland. Our results suggest that treatment and control rates among people with diabetes remain low and that the combination of different antidiabetic drugs is increasingly used in the treatment of diabetes.
Diabetes prevalence and awareness
Our results suggest that overall diabetes prevalence and awareness have decreased. Our findings do not replicate the global increasing trends in diabetes prevalence and incidence of the last decades1. Nevertheless, our findings are in agreement with data from some high-income countries, where diabetes incidence has been stable or decreasing for the last years21. A possible explanation could be the increase in physical activity levels of the Swiss population, as in 2017, almost three-quarters of the population complied with physical activity recommendations, a 14% increase from 200222. Still, a recruitment bias cannot be excluded, through participation of more health-conscious people. It would thus be important to confirm our findings in other population-based surveys.
Dyslipidaemia and hypertension were positively associated with prevalence and diagnosis of diabetes. Those findings show that CVD risk factors tend to cluster among diabetic patients23, and that presence of one risk factor prompts the physician to search for the other ones.
Treatment and control of diabetes
Among participants diagnosed with diabetes, treatment and control rates did not change. Only one-third (34%) of treated participants was controlled, a lower rate than in a study conducted in 16 European countries, where 65.2% achieved the HbA1c target of < 7.0%4. The difference could be partly explained by the different definitions and thresholds for controlled diabetes (target of fasting plasma glucose level < 6.7 mmol/L in our study vs. HbA1c < 7.0% in the European study)24. The reasons for such a low control rate could be due to clinical inertia, participants with diabetes and their doctors not complying with treatment or not willing to intensify it25,26. It would be important that future studies assess compliance to treatment, by for example studying drug prescriptions.
After multivariable analysis, women with diabetes were less likely to be treated but more likely to be controlled. Findings of previous studies on gender differences in the treatment and control of diabetes are inconsistent. Several studies conducted in Iran, China and the EU reported that both genders were equally treated for diabetes27,28,29. Regarding control levels, an Iranian study reported that women were more likely to achieve diabetes control27; the opposite was reported by a Chinese and an European study28,29, while a Pakistani study reported that both genders had similar control levels30. The reasons for a lower treatment rate among women diagnosed with diabetes are currently unknown and should be further assessed. Possible explanations include the underestimation of diabetes severity in women, lack of staff for patient education, doctors’ lack of updated knowledge, or patients’ lack of willingness to be treated31,32.
After multivariable analysis, obese participants with diabetes were more likely to be treated but less likely to be controlled. Those findings are in agreement with a previous study, where high BMI was a strong predictor of receiving antidiabetic treatment33. As obesity is frequently associated with concomitant diseases such as cardiovascular diseases and cancer34, doctors might feel more compelled to prescribe treatment. However, treatment of obese patients with diabetes is complicated by metabolic and drug interactions that could prevent glycaemic control35.
Trends in antidiabetic drugs
Use of antidiabetic combinations increased, while use of sulfonylureas and biguanides decreased. The trend of combination therapy has not been studied frequently, but increased use has been noted previously15. Sulfonylureas and biguanides are the oldest noninsulin injectable antidiabetic agents36. In previous studies, use of sulfonylureas decreased similarly, but contrary to our results, use of metformin (biguanide) increased13,15,17.
In our study, no trend was found for insulin and other drugs. Contrary to our results, insulin use increased in several other studies12,13,15,17. The European Medicine Agency and the US Food and Drug Administration authorized use of three SGLT-2 inhibitors (dapagliflozin, canagliflozin, and empagliflozin) between 2012 and 201537. The first GLP-1 receptor agonists exenatide was approved in 2005 (US) and 2006 (Europe)38. Although some drugs were relatively new, others could have been prescribed for almost 10 years as it is the case for GLP-1 agonists, or for five years for some SGLT-2 inhibitors. Overall, our results suggest that physicians in Geneva appear to be reluctant to prescribe the newest antidiabetic drugs. Whether such attitude is due to clinical inertia or to a constraint by health insurances (as the newest antidiabetic drugs are more expensive and thus less likely to be reimbursed) remains to be assessed.
Clinical implications
Our results suggest that certain subgroups of individuals with diabetes are more likely to be treated or to achieve diabetes control. Particular attention should be paid to patients with high BMI, who are more likely to have long-term hyperglycaemia and are therefore at higher risk of adverse diabetes-related complications. Efforts to increase diabetes control should be implemented among patients and their physicians, as inadequately controlled diabetes leads to increased health and economic costs39,40.
Combination therapy progressively replaced sulfonylureas and biguanides. Newer antidiabetic drugs such as SGLT-2 inhibitors and GLP-1 receptor agonists were less prescribed. These drugs reduce cardiovascular and renal damage and could be of great benefit to participants with diabetes41. Hence, it would be important that doctors be made aware of these benefits, and that health insurers accept to reimburse the drugs42.
Strengths and limitations
This study has several strengths. Firstly, it assessed four important parameters of diabetes management in Switzerland (prevalence, awareness, treatment, and control), and at three different time points. Secondly, it assessed the parameters’ association with a broad spectrum of socio-demographic variables allowing better understanding of the factors that hinder or promote optimal diabetes management.
This study also has several limitations. Firstly, it was conducted in a single location, so the results may not be transferable to other environments. Secondly, antidiabetic drugs were self-reported. Self-report has overestimated medication adherence in the past43. Consequently, the overall results might be overoptimistic, and the true status of antidiabetic drug use might actually be worse than reported. Still, self-reporting should not affect the differences between groups and associations with different factors. Thirdly, the sample size might not be sufficient to detect minor differences in the association of the factors with diabetes prevalence, awareness, treatment, and control. Still, such small differences could be clinically irrelevant. Fourthly, no information regarding history of childbearing or gestational diabetes was available for women; hence, we could not adjust for those potential confounders. Finally, the sample size resulted low when adjusting for dyslipidaemia because participants lacked data for dyslipidaemia status. Still, only few of the significant results changed after multivariable analysis leaving out dyslipidaemia status.
Conclusion
In canton Geneva, trends in drug prescription are changing, with combination therapy gaining importance. However, only about half of participants diagnosed with diabetes receive antidiabetic treatment, and only one third of participants treated for diabetes are controlled, with no significant improvements in the last 10 years.
Data availability
Due to the sensitivity of the data and the lack of consent for online posting, individual data cannot be made accessible. Non-identifiable, individual-level data are available for interested researchers, who meet the criteria for access to confidential data sharing. Requests to access the data should be directed to Professor Idris Guessous at Idris.Guessous@hcuge.ch.
References
Liu, J. et al. Trends in the incidence of diabetes mellitus: results from the Global Burden of Disease Study 2017 and implications for diabetes mellitus prevention. BMC Public Health 20(1), 1415 (2020).
Collaboration NCDRF. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 390(10113):2627–42 (2017).
Lin, X. et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: An analysis from 1990 to 2025. Sci. Rep. 10(1), 14790 (2020).
Kotseva, K. et al. Primary prevention efforts are poorly developed in people at high cardiovascular risk: A report from the European Society of Cardiology EURObservational Research Programme EUROASPIRE V survey in 16 European countries. Eur. J. Prev. Cardiol. 28(4), 370–379 (2021).
Lu, W. et al. Prevalence, awareness, treatment and control of hypertension, diabetes and hypercholesterolemia, and associated risk factors in the Czech Republic, Russia, Poland and Lithuania: A cross-sectional study. BMC Public Health 22(1), 883 (2022).
Estoppey, D., Paccaud, F., Vollenweider, P. & Marques-Vidal, P. Trends in self-reported prevalence and management of hypertension, hypercholesterolemia and diabetes in Swiss adults, 1997–2007. BMC Public Health 11, 114 (2011).
de Mestral, C., Stringhini, S., Guessous, I. & Jornayvaz, F. R. Thirteen-year trends in the prevalence of diabetes in an urban region of Switzerland: A population-based study. Diabet. Med. 37(8), 1374–1378 (2020).
de Mestral, C., Stringhini, S., Guessous, I. & Jornayvaz, F. R. Thirteen-year trends in the prevalence of diabetes according to socioeconomic condition and cardiovascular risk factors in a Swiss population. BMJ Open Diabetes Res. Care 8(1), e001273 (2020).
Gastaldi, G. et al. Swiss recommendations of the Society for Endocrinology and Diabetes (SGED/SSED) for the treatment of type 2 diabetes mellitus. Swiss Med Wkly 153, 40060 (2023).
Cosentino, F. et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 41(2), 255–323 (2020).
Roglic, G. & Norris, S. L. Medicines for treatment intensification in type 2 diabetes and type of insulin in type 1 and type 2 diabetes in low-resource settings: Synopsis of the world health organization guidelines on second- and third-line medicines and type of insulin for the control of blood glucose levels in nonpregnant adults with diabetes mellitus. Ann. Intern. Med. 169(6), 394–397 (2018).
Chu, C. H. et al. Trends in antidiabetic medical treatment from 2005 to 2014 in Taiwan. J. Formos. Med. Assoc. 118(Suppl 2), S74–S82 (2019).
Orlando, V. et al. Prescription patterns of antidiabetic treatment in the elderly. Results from Southern Italy. Curr. Diabetes Rev. 12(2), 100–106 (2015).
Kohro, T. et al. Trends in antidiabetic prescription patterns in Japan from 2005 to 2011. Int. Heart J. 54(2), 93–97 (2013).
Mata-Cases, M., Franch-Nadal, J., Real, J. & Mauricio, D. Glycaemic control and antidiabetic treatment trends in primary care centres in patients with type 2 diabetes mellitus during 2007–2013 in Catalonia: A population-based study. BMJ Open. 6(10), e012463 (2016).
Hampp, C., Borders-Hemphill, V., Moeny, D. G. & Wysowski, D. K. Use of antidiabetic drugs in the U.S. 2003–2012. Diabetes Care. 37(5), 1367–1374 (2014).
Lipska, K. J. et al. Trends in drug utilization, glycemic control, and rates of severe hypoglycemia, 2006–2013. Diabetes Care 40(4), 468–475 (2017).
Morabia, A., Bernstein, M., Heritier, S. & Ylli, A. Community-based surveillance of cardiovascular risk factors in Geneva: Methods, resulting distributions, and comparisons with other populations. Prev. Med. 26(3), 311–319 (1997).
Marques-Vidal, P. et al. Dietary intake according to gender and education: A twenty-year trend in a Swiss adult population. Nutrients 7(11), 9558–9572 (2015).
Humain CCdEdlRslê. CCER-obtenir une autorisation de recherche médicale sur l'être humain Republic and Canton of Geneva, Switzerland [updated 2023 Sept 12. Available from: https://www.ge.ch/ccer-obtenir-autorisation-recherche-medicale-etre-humain.
Magliano, D. J. et al. Trends in incidence of total or type 2 diabetes: Systematic review. BMJ. 366, l5003 (2019).
(OFS) Ofdls. Inégalités sociales en santé physique Neuchâtel, Switzerland2020 [updated 2020 Oct 27. Available from: https://opendata.swiss/fr/dataset/soziale-ungleichheiten-und-korperliche-gesundheit.
Bahiru, E., Hsiao, R., Phillipson, D. & Watson, K. E. Mechanisms and treatment of dyslipidemia in diabetes. Curr. Cardiol. Rep. 23(4), 26 (2021).
Carson, A. P., Reynolds, K., Fonseca, V. A. & Muntner, P. Comparison of A1C and fasting glucose criteria to diagnose diabetes among U.S. adults. Diabetes Care 33(1), 95–97 (2010).
Khunti, S., Khunti, K. & Seidu, S. Therapeutic inertia in type 2 diabetes: Prevalence, causes, consequences and methods to overcome inertia. Ther. Adv. Endocrinol. Metab. 10, 2042018819844694 (2019).
Ampudia-Blasco, F. J., Palanca, A., Trillo, J. L., Navarro, J. & Real, J. T. Therapeutic inertia in patients with type 2 diabetes treated with non-insulin agents. J. Diabetes Complicat. 35(3), 107828 (2021).
Oraii, A. et al. Prevalence, awareness, treatment, and control of type 2 diabetes mellitus among the adult residents of tehran: Tehran Cohort Study. BMC Endocr. Disord. 22(1), 248 (2022).
Sun, Y., Ni, W., Yuan, X., Chi, H. & Xu, J. Prevalence, treatment, control of type 2 diabetes and the risk factors among elderly people in Shenzhen: Results from the urban Chinese population. BMC Public Health 20(1), 998 (2020).
Ferrannini, G. et al. Gender differences in screening for glucose perturbations, cardiovascular risk factor management and prognosis in patients with dysglycaemia and coronary artery disease: Results from the ESC-EORP EUROASPIRE surveys. Cardiovasc. Diabetol. 20(1), 38 (2021).
Aa, K. Impact of gender on type II diabetes glycemic and cardiovascular markers control and treatment. Pak. J. Biol. Sci. 23(12), 1643–1649 (2020).
Alhagawy, A. J. et al. Barriers and attitudes of primary healthcare physicians to insulin initiation and intensification in Saudi Arabia. Int. J. Environ. Res. Public Health 19(24), 16794 (2022).
Zafar, A., Stone, M. A., Davies, M. J. & Khunti, K. Acknowledging and allocating responsibility for clinical inertia in the management of Type 2 diabetes in primary care: A qualitative study. Diabet. Med. 32(3), 407–413 (2015).
Safari-Faramani, R. et al. Prevalence, awareness, treatment, control, and the associated factors of diabetes in an Iranian Kurdish population. J. Diabetes Res. 2019, 5869206 (2019).
Guh, D. P. et al. The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis. BMC Public Health 9, 88 (2009).
Sonmez, A. et al. Impact of obesity on the metabolic control of type 2 diabetes: Results of the Turkish nationwide survey of glycemic and other metabolic parameters of patients with diabetes mellitus (TEMD Obesity Study). Obes. Facts. 12(2), 167–178 (2019).
White, J. R. Jr. A brief history of the development of diabetes medications. Diabetes Spectr. 27(2), 82–86 (2014).
Braunwald, E. SGLT2 inhibitors: The statins of the 21st century. Eur. Heart J. 43(11), 1029–1030 (2022).
Nauck, M. A., Quast, D. R., Wefers, J. & Meier, J. J. GLP-1 receptor agonists in the treatment of type 2 diabetes-state-of-the-art. Mol. Metab. 46, 101102 (2021).
Ali, S. N., Dang-Tan, T., Valentine, W. J. & Hansen, B. B. Evaluation of the Clinical and economic burden of poor glycemic control associated with therapeutic inertia in patients with type 2 diabetes in the United States. Adv. Ther. 37(2), 869–882 (2020).
Bain, S. C., Bekker Hansen, B., Hunt, B., Chubb, B. & Valentine, W. J. Evaluating the burden of poor glycemic control associated with therapeutic inertia in patients with type 2 diabetes in the UK. J. Med. Econ. 23(1), 98–105 (2020).
Palmer, S. C. et al. Sodium-glucose cotransporter protein-2 (SGLT-2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists for type 2 diabetes: Systematic review and network meta-analysis of randomised controlled trials. BMJ 372, m4573 (2021).
Groupe de travail de la SGED/SSED: Roger Lehmann (Chair) GG, Astrid Czock, Marc Egli, Doris Fischer-Taeschler, Markus Laimer, Barbara Lucchini, Sebastien Thalmann, Peter Wiesli Recommandations de la Société Suisse d’Endocrinologie et de Diabétologie (SGED-SSED) pour le traitement du diabète de type 2 (2020) Switzerland2020 [Available from: https://www.sgedssed.ch/fileadmin/user_upload/6_Diabetologie/61_Empfehlungen_Facharzt/2020_Swiss_Recomm_Medis_FR_def.pdf.
Stirratt, M. J. et al. Self-report measures of medication adherence behavior: Recommendations on optimal use. Transl. Behav. Med. 5(4), 470–482 (2015).
Acknowledgements
The authors would like to thank all the people who participated in the recruitment of the participants, data collection and validation, and Dr Vanessa Kraege for the thorough revision of the manuscript.
Funding
This work is funded by the Geneva University Hospitals through the General Directorate of Health (Canton of Geneva). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
A.P.: Investigation, Methodology, Writing—Original draft preparation, Visualization. P.M-V.: Conceptualization, Methodology, Data curation, Formal analysis, Writing – Reviewing and editing, Visualization. C.d.M.: Data curation, Writing – Reviewing and editing. P.M.V. had full access to the data and is the guarantor of the study.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pauli, A., de Mestral, C. & Marques-Vidal, P. Trends in diabetes prevalence, awareness, treatment, and control in French-speaking Switzerland. Sci Rep 14, 4839 (2024). https://doi.org/10.1038/s41598-024-54856-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-54856-6
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.