Abstract
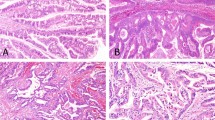
Due to its poor prognosis and the late stage at which it is typically diagnosed, early detection of pancreatic cancer is a pressing clinical problem. Advances in genomic analysis of human pancreatic tissue and other biospecimens such as pancreatic cyst fluid, pancreatic juice and blood have opened the possibility of DNA-based molecular approaches for early detection of pancreatic cancer. In this Review, we discuss and focus on the pathological and molecular features of precancerous lesions of the pancreas, including pancreatic intraepithelial neoplasia, intraductal papillary mucinous neoplasm and mucinous cystic neoplasm, which are target lesions of early detection approaches. We also discuss the most prevalent genetic alterations in these precancerous lesions, including somatic mutations in the oncogenes KRAS and GNAS as well as tumour suppressor genes CDKN2A, TP53 and SMAD4. We highlight the latest discoveries related to genetic heterogeneity and multifocal neoplasia in precancerous lesions. In addition, we review specific approaches, challenges and clinically available assays for early detection of pancreatic cancer using DNA-based molecular techniques. Although detection and risk stratification of precancerous pancreatic neoplasms are difficult problems, progress in this field highlights the promise of molecular approaches for improving survival of patients with this disease.
Key points
-
The target lesions for pancreatic cancer screening are high-grade precancerous lesions and early-stage invasive cancers.
-
Precancerous lesions can be microscopic (pancreatic intraepithelial neoplasia (PanIN)) or macroscopic (intraductal papillary mucinous neoplasm (IPMN) and mucinous cystic neoplasm (MCN)), and these lesions are classified as low-grade or high-grade based on the morphological grade of dysplasia of their lining epithelium; although low-grade lesions share early oncogene mutations such as KRAS, mutations in other genes (CDKN2A, TP53 and SMAD4) are limited to more advanced lesions.
-
Studies have highlighted genetic heterogeneity in precancerous lesions and multifocal neoplasia in the pancreas, which should be considered when designing early detection approaches.
-
The evolving understanding of the genetics of precancerous lesions has led to the development of clinically available assays for pancreatic cyst classification and detection of high-grade dysplasia and early-stage pancreatic cancers.
-
Mutations in KRAS and/or GNAS are highly specific for mucinous cysts, such as IPMNs, while alterations in CDKN2A, TP53 and/or SMAD4 are almost exclusively seen in the setting of advanced lesions.
-
The assessment of genetic alterations using a non-invasive method, such as from a patient’s blood specimen, holds promise not only for early detection of pancreatic cancer but also for the identification of precancerous lesions.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Siegel, R. L., Miller, K. D., Fuchs, H. E. & Jemal, A. Cancer statistics, 2021. CA Cancer J. Clin. 71, 7–33 (2021).
Rahib, L. et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 74, 2913–2921 (2014).
Kommalapati, A., Tella, S. H., Goyal, G., Ma, W. W. & Mahipal, A. Contemporary management of localized resectable pancreatic cancer. Cancers 10, 24 (2018).
Groot, V. P. et al. Patterns, timing, and predictors of recurrence following pancreatectomy for pancreatic ductal adenocarcinoma. Ann. Surg. 267, 936–945 (2018).
Matsuda, Y. et al. The prevalence and clinicopathological characteristics of high-grade pancreatic intraepithelial neoplasia: autopsy study evaluating the entire pancreatic parenchyma. Pancreas 46, 658–664 (2017).
Basturk, O. et al. A revised classification system and recommendations from the Baltimore Consensus Meeting for neoplastic precursor lesions in the pancreas. Am. J. Surg. Pathol. 39, 1730–1741 (2015).
Canto, M. I. et al. Surgical outcomes after pancreatic resection of screening-detected lesions in individuals at high risk for developing pancreatic cancer. J. Gastrointest. Surg. 24, 1101–1110 (2020).
Bassi, C. et al. Pancreatoduodenectomy at the Verona Pancreas Institute: the evolution of indications, surgical techniques and outcomes: a retrospective analysis of 3000 consecutive cases. Ann. Surg. https://doi.org/10.1097/sla.0000000000004753 (2021).
Kamarajah, S. K., Burns, W. R., Frankel, T. L., Cho, C. S. & Nathan, H. Validation of the American Joint Commission on Cancer (AJCC) 8th edition Staging System for Patients with Pancreatic Adenocarcinoma: a Surveillance, Epidemiology and End Results (SEER) Analysis. Ann. Surg. Oncol. 24, 2023–2030 (2017).
Pfluger, M. J. et al. The impact of clinical and pathological features on IPMN recurrence after surgical resection: long-term follow-up analysis. Ann. Surg. https://doi.org/10.1097/SLA.0000000000004427 (2020).
Rezaee, N. et al. Intraductal papillary mucinous neoplasm (IPMN) with high-grade dysplasia is a risk factor for the subsequent development of pancreatic ductal adenocarcinoma. HPB 18, 236–246 (2016).
Oyama, H. et al. Long-term risk of malignancy in branch-duct intraductal papillary mucinous neoplasms. Gastroenterology 158, 226–237.e5 (2020).
Winter, J. M. et al. 1423 pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. J. Gastrointest. Surg. 10, 1199–1210 (2006).
Andea, A., Sarkar, F. & Adsay, V. N. Clinicopathological correlates of pancreatic intraepithelial neoplasia: a comparative analysis of 82 cases with and 152 cases without pancreatic ductal adenocarcinoma. Mod. Pathol. 16, 996–1006 (2003).
Goggins, M. et al. Management of patients with increased risk for familial pancreatic cancer: updated recommendations from the International Cancer of the Pancreas Screening (CAPS) Consortium. Gut 69, 7–17 (2020).
Hutchings, D. et al. Cancerization of the pancreatic ducts: demonstration of a common and under-recognized process using immunolabeling of paired duct lesions and invasive pancreatic ductal adenocarcinoma for p53 and Smad4 expression. Am. J. Surg. Pathol. 42, 1556–1561 (2018).
Waddell, N. et al. Whole genomes redefine the mutational landscape of pancreatic cancer. Nature 518, 495–501 (2015).
Raphael, B. J. et al. Integrated genomic characterization of pancreatic ductal adenocarcinoma. Cancer Cell 32, 185–203.e13 (2017).
Kanda, M. et al. Presence of somatic mutations in most early-stage pancreatic intraepithelial neoplasia. Gastroenterology 142, 730–733.e9 (2012).
Murphy, S. J. et al. Genetic alterations associated with progression from pancreatic intraepithelial neoplasia to invasive pancreatic tumor. Gastroenterology 145, 1098–1109.e1 (2013).
van Heek, N. T. et al. Telomere shortening is nearly universal in pancreatic intraepithelial neoplasia. Am. J. Pathol. 161, 1541–1547 (2002).
Hosoda, W. et al. Genetic analyses of isolated high-grade pancreatic intraepithelial neoplasia (HG-PanIN) reveal paucity of alterations in TP53 and SMAD4. J. Pathol. 242, 16–23 (2017).
Hong, S. M. et al. Genome-wide somatic copy number alterations in low-grade PanINs and IPMNs from individuals with a family history of pancreatic cancer. Clin. Cancer Res. 18, 4303–4312 (2012).
Hata, T. et al. Genome-wide somatic copy number alterations and mutations in high-grade pancreatic intraepithelial neoplasia. Am. J. Pathol. 188, 1723–1733 (2018).
Furukawa, T. et al. Classification of types of intraductal papillary-mucinous neoplasm of the pancreas: a consensus study. Virchows Arch. 447, 794–799 (2005).
Amato, E. et al. Targeted next-generation sequencing of cancer genes dissects the molecular profiles of intraductal papillary neoplasms of the pancreas. J. Pathol. 233, 217–227 (2014).
Ban, S. et al. Intraductal papillary mucinous neoplasm (IPMN) of the pancreas: its histopathologic difference between 2 major types. Am. J. Surg. Pathol. 30, 1561–1569 (2006).
Fischer, C. G. & Wood, L. D. From somatic mutation to early detection: insights from molecular characterization of pancreatic cancer precursor lesions. J. Pathol. 246, 395–404 (2018).
Noë, M. et al. Genomic characterization of malignant progression in neoplastic pancreatic cysts. Nat. Commun. 11, 4085 (2020).
Wu, J. et al. Recurrent GNAS mutations define an unexpected pathway for pancreatic cyst development. Sci. Transl. Med. 3, 92ra66 (2011).
Furukawa, T. et al. Whole-exome sequencing uncovers frequent GNAS mutations in intraductal papillary mucinous neoplasms of the pancreas. Sci. Rep. 1, 161 (2011).
Wu, J. et al. Whole-exome sequencing of neoplastic cysts of the pancreas reveals recurrent mutations in components of ubiquitin-dependent pathways. Proc. Natl Acad. Sci. USA 108, 21188–21193 (2011).
Fujikura, K. et al. Multiregion whole-exome sequencing of intraductal papillary mucinous neoplasms reveals frequent somatic KLF4 mutations predominantly in low-grade regions. Gut 70, 928–939 (2021).
Fischer, C. G. et al. Intraductal papillary mucinous neoplasms arise from multiple independent clones, each with distinct mutations. Gastroenterology 157, 1123–1137.e22 (2019).
Kuboki, Y. et al. Single-cell sequencing defines genetic heterogeneity in pancreatic cancer precursor lesions. J. Pathol. 247, 347–356 (2019).
Makohon-Moore, A. P. et al. Limited heterogeneity of known driver gene mutations among the metastases of individual patients with pancreatic cancer. Nat. Genet. 49, 358–366 (2017).
Wang, T. et al. Intraductal oncocytic papillary neoplasms: clinical-pathologic characterization of 24 cases, with an emphasis on associated invasive carcinomas. Am. J. Surg. Pathol. 43, 656–661 (2019).
Singhi, A. D. et al. Recurrent rearrangements in PRKACA and PRKACB in intraductal oncocytic papillary neoplasms of the pancreas and bile duct. Gastroenterology 158, 573–582.e2 (2020).
Vyas, M. et al. DNAJB1-PRKACA fusions occur in oncocytic pancreatic and biliary neoplasms and are not specific for fibrolamellar hepatocellular carcinoma. Mod. Pathol. 33, 648–656 (2020).
Honeyman, J. N. et al. Detection of a recurrent DNAJB1-PRKACA chimeric transcript in fibrolamellar hepatocellular carcinoma. Science 343, 1010–1014 (2014).
Basturk, O. et al. Intraductal tubulopapillary neoplasm of the pancreas: a clinicopathologic and immunohistochemical analysis of 33 cases. Am. J. Surg. Pathol. 41, 313–325 (2017).
Basturk, O. et al. Pancreatic intraductal tubulopapillary neoplasm is genetically distinct from intraductal papillary mucinous neoplasm and ductal adenocarcinoma. Mod. Pathol. 30, 1760–1772 (2017).
Zamboni, G. et al. Mucinous cystic tumors of the pancreas: clinicopathological features, prognosis, and relationship to other mucinous cystic tumors. Am. J. Surg. Pathol. 23, 410–422 (1999).
Elias, K. M. et al. Primordial germ cells as a potential shared cell of origin for mucinous cystic neoplasms of the pancreas and mucinous ovarian tumors. J. Pathol. 246, 459–469 (2018).
Pea, A. et al. Targeted DNA sequencing reveals patterns of local progression in the pancreatic remnant following resection of intraductal papillary mucinous neoplasm (IPMN) of the pancreas. Ann. Surg. 266, 133–141 (2017).
Felsenstein, M. et al. IPMNs with co-occurring invasive cancers: neighbours but not always relatives. Gut 67, 1652–1662 (2018).
Omori, Y. et al. Pathways of progression from intraductal papillary mucinous neoplasm to pancreatic ductal adenocarcinoma based on molecular features. Gastroenterology 156, 647–661.e2 (2019).
Howlader, N. et al. SEER cancer statistics review, 1975–2017. https://seer.cancer.gov/csr/1975_2017/ (2020).
United States Census Bureau. American community survey. https://www.census.gov/data.html (2020).
Poruk, K. E., Firpo, M. A., Adler, D. G. & Mulvihill, S. J. Screening for pancreatic cancer: why, how, and who? Ann. Surg. 257, 17–26 (2013).
Gardner, T. B. et al. Pancreatic cyst prevalence and the risk of mucin-producing adenocarcinoma in US adults. Am. J. Gastroenterol. 108, 1546–1550 (2013).
Anand, G. S. et al. Pancreas cancer incidence and pancreas cancer-associated mortality are low in national cohort of 7211 pancreas cyst patients. Dig. Dis. Sci. https://doi.org/10.1007/s10620-021-06923-5 (2021).
Hruban, R. H., Canto, M. I., Goggins, M., Schulick, R. & Klein, A. P. Update on familial pancreatic cancer. Adv. Surg. 44, 293–311 (2010).
Klein, A. P. et al. Prospective risk of pancreatic cancer in familial pancreatic cancer kindreds. Cancer Res. 64, 2634–2638 (2004).
Roberts, N. J. et al. Whole genome sequencing defines the genetic heterogeneity of familial pancreatic cancer. Cancer Discov. 6, 166–175 (2016).
Sharma, A. et al. Model to determine risk of pancreatic cancer in patients with new-onset diabetes. Gastroenterology 155, 730–739.e3 (2018).
Duell, E. J. et al. Pancreatitis and pancreatic cancer risk: a pooled analysis in the International Pancreatic Cancer Case-Control Consortium (PanC4). Ann. Oncol. 23, 2964–2970 (2012).
Lowenfels, A. B. et al. Pancreatitis and the risk of pancreatic cancer. N. Engl. J. Med. 328, 1433–1437 (1993).
Sohn, T. A. et al. Intraductal papillary mucinous neoplasms of the pancreas: an updated experience. Ann. Surg. 239, 788–797 (2004).
Salvia, R. et al. Main-duct intraductal papillary mucinous neoplasms of the pancreas: clinical predictors of malignancy and long-term survival following resection. Ann. Surg. 239, 678–685 (2004).
Basturk, O., Coban, I. & Adsay, N. V. Pancreatic cysts: pathologic classification, differential diagnosis, and clinical implications. Arch. Pathol. Lab. Med. 133, 423–438 (2009).
Scheiman, J. M., Hwang, J. H. & Moayyedi, P. American Gastroenterological Association technical review on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology 148, 824–848.e22 (2015).
Ahmad, N. A. et al. Interobserver agreement among endosonographers for the diagnosis of neoplastic versus non-neoplastic pancreatic cystic lesions. Gastrointest. Endosc. 58, 59–64 (2003).
Khalid, A. & Brugge, W. ACG practice guidelines for the diagnosis and management of neoplastic pancreatic cysts. Am. J. Gastroenterol. 102, 2339–2349 (2007).
Pitman, M. B. et al. Pancreatic cysts: preoperative diagnosis and clinical management. Cancer Cytopathol. 118, 1–13 (2010).
Maker, A. V., Lee, L. S., Raut, C. P., Clancy, T. E. & Swanson, R. S. Cytology from pancreatic cysts has marginal utility in surgical decision-making. Ann. Surg. Oncol. 15, 3187–3192 (2008).
Khalid, A. et al. The role of pancreatic cyst fluid molecular analysis in predicting cyst pathology. Clin. Gastroenterol. Hepatol. 3, 967–973 (2005).
Khalid, A. et al. Pancreatic cyst fluid DNA analysis in evaluating pancreatic cysts: a report of the PANDA study. Gastrointest. Endosc. 69, 1095–1102 (2009).
Shen, J., Brugge, W. R., Dimaio, C. J. & Pitman, M. B. Molecular analysis of pancreatic cyst fluid: a comparative analysis with current practice of diagnosis. Cancer 117, 217–227 (2009).
Panarelli, N. C. et al. Commercial molecular panels are of limited utility in the classification of pancreatic cystic lesions. Am. J. Surg. Pathol. 36, 1434–1443 (2012).
Toll, A. D., Kowalski, T., Loren, D. & Bibbo, M. The added value of molecular testing in small pancreatic cysts. JOP 11, 582–586 (2010).
Nikiforova, M. N. et al. Integration of KRAS testing in the diagnosis of pancreatic cystic lesions: a clinical experience of 618 pancreatic cysts. Mod. Pathol. 26, 1478–1487 (2013).
Singhi, A. D. et al. Preoperative GNAS and KRAS testing in the diagnosis of pancreatic mucinous cysts. Clin. Cancer Res. 20, 4381–4389 (2014).
Tsiatis, A. C. et al. Comparison of Sanger sequencing, pyrosequencing, and melting curve analysis for the detection of KRAS mutations: diagnostic and clinical implications. J. Mol. Diagn. 12, 425–432 (2010).
Jones, M. et al. Impact of next-generation sequencing on the clinical diagnosis of pancreatic cysts. Gastrointest. Endosc. 83, 140–148 (2016).
Singhi, A. D. et al. Preoperative next-generation sequencing of pancreatic cyst fluid is highly accurate in cyst classification and detection of advanced neoplasia. Gut 67, 2131–2141 (2018).
Tanaka, M. et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology 17, 738–753 (2017).
Vege, S. S. et al. American Gastroenterological Association Institute guideline on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology 148, 819–822 (2015).
Elta, G. H., Enestvedt, B. K., Sauer, B. G. & Lennon, A. M. ACG clinical guideline: diagnosis and management of pancreatic cysts. Am. J. Gastroenterol. 113, 464–479 (2018).
Singhi, A. D. et al. American Gastroenterological Association guidelines are inaccurate in detecting pancreatic cysts with advanced neoplasia: a clinicopathologic study of 225 patients with supporting molecular data. Gastrointest. Endosc. 83, 1107–1117.e2 (2016).
Springer, S. et al. A combination of molecular markers and clinical features improve the classification of pancreatic cysts. Gastroenterology 149, 1501–1510 (2015).
Springer, S. et al. A multimodality test to guide the management of patients with a pancreatic cyst. Sci. Transl. Med. 11, eaav4772 (2019).
Siddiqui, A. A. et al. High risk of acute pancreatitis after endoscopic ultrasound-guided fine needle aspiration of side branch intraductal papillary mucinous neoplasms. Endosc. Ultrasound 4, 109–114 (2015).
Pergolini, I. et al. Long-term risk of pancreatic malignancy in patients with branch duct intraductal papillary mucinous neoplasm in a referral center. Gastroenterology 153, 1284–1294.e1 (2017).
Tanaka, M. Intraductal papillary mucinous neoplasm of the pancreas as the main focus for early detection of pancreatic adenocarcinoma. Pancreas 47, 544–550 (2018).
Sadakari, Y. et al. Mutant KRAS and GNAS DNA concentrations in secretin-stimulated pancreatic fluid collected from the pancreatic duct and the duodenal lumen. Clin. Transl. Gastroenterol. 5, e62 (2014).
Yu, J. et al. Digital next-generation sequencing identifies low-abundance mutations in pancreatic juice samples collected from the duodenum of patients with pancreatic cancer and intraductal papillary mucinous neoplasms. Gut 66, 1677–1687 (2017).
Kanda, M. et al. Mutant GNAS detected in duodenal collections of secretin-stimulated pancreatic juice indicates the presence or emergence of pancreatic cysts. Gut 62, 1024–1033 (2013).
Kanda, M. et al. Mutant TP53 in duodenal samples of pancreatic juice from patients with pancreatic cancer or high-grade dysplasia. Clin. Gastroenterol. Hepatol. 11, 719–730.e5 (2013).
Suenaga, M. et al. Pancreatic juice mutation concentrations can help predict the grade of dysplasia in patients undergoing pancreatic surveillance. Clin. Cancer Res. 24, 2963–2974 (2018).
Bidard, F. C. et al. Circulating tumor cells in locally advanced pancreatic adenocarcinoma: the ancillary CirCe 07 study to the LAP 07 trial. Ann. Oncol. 24, 2057–2061 (2013).
Kulemann, B. et al. Pancreatic cancer: circulating tumor cells and primary tumors show heterogeneous KRAS mutations. Sci. Rep. 7, 4510 (2017).
Rhim, A. D. et al. Detection of circulating pancreas epithelial cells in patients with pancreatic cystic lesions. Gastroenterology 146, 647–651 (2014).
Martini, V., Timme-Bronsert, S., Fichtner-Feigl, S., Hoeppner, J. & Kulemann, B. Circulating tumor cells in pancreatic cancer: current perspectives. Cancers 11, 1659 (2019).
Cohen, J. D. et al. Combined circulating tumor DNA and protein biomarker-based liquid biopsy for the earlier detection of pancreatic cancers. Proc. Natl Acad. Sci. USA 114, 10202–10207 (2017).
Cohen, J. D. et al. Detection and localization of surgically resectable cancers with a multi-analyte blood test. Science 359, 926–930 (2018).
Hata, T. et al. GNAS mutation detection in circulating cell-free DNA is a specific predictor for intraductal papillary mucinous neoplasms of the pancreas, especially for intestinal subtype. Sci. Rep. 10, 17761 (2020).
Tkach, M. & Thery, C. Communication by extracellular vesicles: where we are and where we need to go. Cell 164, 1226–1232 (2016).
Kahlert, C. et al. Identification of double-stranded genomic DNA spanning all chromosomes with mutated KRAS and p53 DNA in the serum exosomes of patients with pancreatic cancer. J. Biol. Chem. 289, 3869–3875 (2014).
Yang, S. et al. Detection of mutant KRAS and TP53 DNA in circulating exosomes from healthy individuals and patients with pancreatic cancer. Cancer Biol. Ther. 18, 158–165 (2017).
Allenson, K. et al. High prevalence of mutant KRAS in circulating exosome-derived DNA from early-stage pancreatic cancer patients. Ann. Oncol. 28, 741–747 (2017).
Roth, S. et al. Noninvasive discrimination of low and high-risk pancreatic intraductal papillary mucinous neoplasms. Ann. Surg. 273, e273–e275 (2021).
Maker, A. V. et al. Cyst fluid biomarkers for intraductal papillary mucinous neoplasms of the pancreas: a critical review from the international expert meeting on pancreatic branch-duct-intraductal papillary mucinous neoplasms. J. Am. Coll. Surg. 220, 243–253 (2015).
Maker, A. V. et al. Cyst fluid biosignature to predict intraductal papillary mucinous neoplasms of the pancreas with high malignant potential. J. Am. Coll. Surg. 228, 721–729 (2019).
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Gastroenterology & Hepatology thanks T. Hackert, E. Costello and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Singhi, A.D., Wood, L.D. Early detection of pancreatic cancer using DNA-based molecular approaches. Nat Rev Gastroenterol Hepatol 18, 457–468 (2021). https://doi.org/10.1038/s41575-021-00470-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41575-021-00470-0
This article is cited by
-
SMAD4 endows TGF-β1-induced highly invasive tumor cells with ferroptosis vulnerability in pancreatic cancer
Acta Pharmacologica Sinica (2024)
-
Pancreatic Cyst Fluid Assessment: Updates in Genetic Analysis and Risk for Progression
Current Treatment Options in Gastroenterology (2024)
-
Patient-derived organoids of pancreatic ductal adenocarcinoma for subtype determination and clinical outcome prediction
Journal of Gastroenterology (2024)
-
Evaluation of the diagnostic efficacy of liquid-based cytology obtained via percutaneous ultrasound-guided fine-needle aspiration for pancreatic masses: a large tertiary center’s 8-year experience
Journal of Cancer Research and Clinical Oncology (2023)
-
Pancreatic Cancer: Genetic Conditions and Epigenetic Alterations
Journal of Gastrointestinal Surgery (2023)