Abstract
Tumours of the anterior part of the pituitary gland represent just 1% of all childhood (aged <15 years) intracranial neoplasms, yet they can confer high morbidity and little evidence and guidance is in place for their management. Between 2014 and 2022, a multidisciplinary expert group systematically developed the first comprehensive clinical practice consensus guideline for children and young people under the age 19 years (hereafter referred to as CYP) presenting with a suspected pituitary adenoma to inform specialist care and improve health outcomes. Through robust literature searches and a Delphi consensus exercise with an international Delphi consensus panel of experts, the available scientific evidence and expert opinions were consolidated into 74 recommendations. Part 1 of this consensus guideline includes 17 pragmatic management recommendations related to clinical care, neuroimaging, visual assessment, histopathology, genetics, pituitary surgery and radiotherapy. While in many aspects the care for CYP is similar to that of adults, key differences exist, particularly in aetiology and presentation. CYP with suspected pituitary adenomas require careful clinical examination, appropriate hormonal work-up, dedicated pituitary imaging and visual assessment. Consideration should be given to the potential for syndromic disease and genetic assessment. Multidisciplinary discussion at both the local and national levels can be key for management. Surgery should be performed in specialist centres. The collection of outcome data on novel modalities of medical treatment, surgical intervention and radiotherapy is essential for optimal future treatment.
Similar content being viewed by others
Introduction
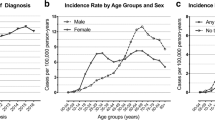
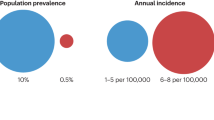
The diagnosis and management of pituitary adenomas in children and young people under 19 years of age (hereafter referred to as CYP) is challenging owing to the rarity of these tumours in this age group, their potential to disrupt maturation, as well as their more aggressive nature and increased potential for familial or genetic aetiology in this age group compared with adults1,2,3. Pituitary adenomas increase in incidence during late adolescence, from 1% of all intracranial neoplasms before 15 years of age to 18% for patients aged 15–24 years4. These patients can present, often late, to a range of different paediatric or adult specialists: endocrinologists, ophthalmologists, neuro-oncologists, medical oncologists or neurosurgeons.
Pituitary adenomas are neoplasms (usually non-malignant) arising from the hormone-secreting cells of the anterior pituitary. In CYP, they often secrete hormones in excess but the resulting characteristic signs and symptoms, such as pubertal delay, amenorrhoea, features of Cushing disease or rapid growth velocity, might be occult or missed during development, leading to late diagnoses5,6. Pituitary adenomas are defined as macroadenomas if they measure ≥1 cm and microadenomas if they measure <1 cm, whereas neoplasms of >4 cm in size are referred to as giant adenomas. Large pituitary adenomas are more prevalent in CYP than in adults6. Mass effects are more common at presentation in CYP than in adults and cause deficits of pituitary hormones, visual field defects, hypothalamic dysfunction, and even raised intracranial pressure or oculo-motor nerve palsy. Of note, the 2022 edition of the WHO Classification of Endocrine Tumours and of Central Nervous System Tumours proposed a pathology-based classification of pituitary adenomas as pituitary neuroendocrine tumours (abbreviated to PitNETs), a term that is currently being debated in the field7,8,9,10,11,12,13.
Pituitary adenomas have a high survival rate but might confer potentially serious, life-changing and life-limiting sequelae. They increase in incidence with increasing age over childhood and represent 78% of pituitary fossa lesions in CYP14. Between 1997 and 2016 in the UK, 5 children with pituitary adenoma were diagnosed aged 0–4 years, 14 children aged 5–9 years, 78 young people aged 10–14 years and 282 young people aged 15–19 (ref. 15). As children with pituitary adenomas can, on average, expect to live for a further 6–7 decades, their health-related quality of life is paramount. The treatment of CYP with pituitary adenomas is challenging due to the lack of high-quality evidence for treatment recommendations for this age group.
In order to achieve optimal care, improve quality of life, and reduce secondary and long-term health-related morbidity, CYP with pituitary adenomas should be treated by a pituitary-specific multidisciplinary team (MDT), with experts from both paediatric and adult practice. Such a level of care could also improve and expedite diagnosis (including complex endocrine and genetic screening of patients with suspected familial aetiology), acute decision-making, perioperative care and long-term surveillance. In contrast to oncology care for CYP, which is usually well organized with centralized units, a less well-developed management provision exists for CYP with pituitary neoplasms. The UK and many other countries lack a dedicated pituitary MDT for CYP.
Having recognized these challenges, a Guideline Development Group (GDG) and an international Delphi panel were formed to develop consensus on diagnostic and management recommendations for CYP with pituitary adenomas according to rigorous methodology approved by the UK National Institute for Health and Care Excellence (NICE). The GDG made 74 recommendations that are included in this two-part consensus guideline. This consensus guideline is intended to provide an evidence-based and eminence-based document for clinicians in several disciplines to whom CYP present to optimize the management of suspected pituitary adenomas in CYP and improve the quality of clinical care and, thus, health outcomes. Part 1 of this consensus guideline provides 17 recommendations regarding neuroimaging, visual assessment, histopathology, genetics, pituitary surgery and radiotherapy relevant to all pituitary adenomas, whereas Part 2 contains 57 recommendations for each of the individual pituitary adenoma types16 (Supplementary Table 1).
Methodology
This consensus guideline was commissioned by the British Society for Paediatric Endocrinology and Diabetes and the Children’s Cancer and Leukaemia Group (CCLG), and was developed in accordance with Appraisal of Guidelines Research and Evaluation Instrument II (AGREE II)17 criteria and the CCLG guideline development standard operating procedure18. Members of the Project Board, GDG and Delphi consensus panel (Supplementary Table 2) were selected based on clinical and academic experience in pituitary tumour diagnosis and management. The methodology is summarized in Fig. 1. All stages of the development process were appraised by the Quality Improvement Committee of the UK Royal College of Paediatrics and Child Health.
Flowchart of the consensus guideline development process for recommendations for the diagnosis and management of pituitary adenomas in children and young people under 19 years of age. The Guideline Development Group (GDG) established the objectives and identified and refined recommendations using Population, Intervention, Comparison, Outcome (PICO) clinical questions19 to undertake systematic literature reviews. Evidence was graded using Grading of Recommendations, Assessment, Development and Evaluations (GRADE) criteria20. Recommendations supported by insufficient, low-quality, or conflicting evidence or evidence that was largely extrapolated from adult experiences, were reviewed by a Delphi consensus process. Recommendations that achieved consensus, alongside those with sufficient evidence not to require a consensus process, were reviewed, and this Consensus Guideline was published following the National Institute for Health and Care Excellence-approved Appraisal of Guidelines Research and Evaluation Instrument II (AGREE II) criteria17.
Developing the clinical questions
The GDG identified its objectives and summarized these as a series of 155 Population, Intervention, Comparison, Outcome (PICO) clinical questions19 that were circulated to stakeholder organizations (listed later and in the Acknowledgements) for comments and then finalized by the GDG. The clinical questions guided the systematic literature search (Supplementary Table 3), critical appraisal, and synthesis of evidence and facilitated the development of recommendations by the GDG.
Identifying, reviewing and synthesizing evidence
The GDG screened titles and abstracts published in English since January 1990 and identified by three systematic literature searches conducted on the core data bases Ovid MEDLINE, PubMed, EMBASE and Cochrane Library in October 2014, February 2021 and April 2022 (Supplementary Fig. 1). Full-text articles relevant to development of this consensus guideline were reviewed and appraised using the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) criteria20. For inclusion and exclusion criteria, search terms, and strategies, see Supplementary Box 1. For detailed evidence tables for recommendations in Part 1, see Supplementary Table 4. Given the rarity of pituitary adenomas in CYP, especially in the youngest developing children aged <15 years, most paediatric evidence was of low quality and the authors have often drawn on evidence from the adult literature, which is noted where relevant. This is an abbreviated version of the guideline; full-text and additional references will be available on the CCLG website (Rare endocrine tumour guidelines).
Developing recommendations
Where there was sufficient moderate-quality evidence to answer the PICO questions, the GDG originally made 54 recommendations whose strength was determined using the GRADE criteria20 by a trade-off between benefits and harms given the quality of the underpinning evidence. Where the evidence base was lacking, of low quality, conflicting or largely extrapolated from adult experiences, the GDG formulated consensus recommendations and submitted these to experts outside the GDG (the international Delphi consensus panel, Supplementary Table 2) in three rounds of a Delphi consensus process (first round, 74 recommendations; second round, 41 recommendations; third limited round for 1 question; see Supplementary Table 5 for full details of the voting for each recommendation). In some cases, a strong recommendation was paired with moderate-quality evidence: these recommendations were based on adult data and strong recommendations in adult guidelines that are applicable to CYP. High-quality evidence is unlikely to be prospectively generated in the CYP age group in the future due to the rarity of these conditions.
Following a revised literature review in 2021, the GDG finalized a total of 74 main recommendations with a total of 89 statements as some of the recommendations included 2 or more interrelated statements. Of 89 statements, 34 were evidence based (with 13 of these also having Delphi consensus) and 55 were eminence based (49 based on Delphi consensus, 10 of these with additional GDG consensus and 6 based on GDG consensus). We followed a consistent NICE terminology, using the verbs ‘should’ and ‘offer’ to indicate strong recommendations, whereas ‘consider’ was used to indicate moderate or weak recommendations. The evidence levels are shown as strong, moderate or low quality using GRADE criteria with any Delphi or GDG consensus. Recommendations supported by ≥70% of consensus group respondents are included in these guidelines. Areas where the GDG felt that further research was required have been proposed as research recommendations (Box 1).
As part of the consensus guideline development process, the draft article was submitted to two paediatric endocrinology international experts for external peer review between August and November 2018. A second round of external peer review took place before submission for publication in February 2022 by four national and four international experts (three adult endocrinologists, four paediatric endocrinologists and one histopathologist).
Stakeholder, patient and public involvement
This consensus guideline received scientific comments and endorsement from various stakeholders, listed here and in the Acknowledgements. Stakeholders were given the opportunity to comment on the PICO questions, on the first draft of the recommendations (September and December 2016) and on the final draft (November 2021–January 2022). The following learned societies endorse Parts 1 and 2 (ref. 16) of this consensus guideline: Society for Endocrinology, Society of British Neurological Surgeons, British Paediatric Neurosurgical Group, Royal College of Physicians, British Society for Paediatric Endocrinology and Diabetes, British Society of Paediatric Radiology, Royal College of Paediatrics and Child Health, British Neuropathology Society, and the Association for Clinical Biochemistry and Laboratory Medicine. In addition, views from patients with pituitary adenoma, survivors and their families were sought through various patient organizations in October and November 2021, including the Association of Multiple Endocrine Neoplastic Disorders (AMEND), Success Charity and the Pituitary Foundation. All feedback was considered by the GDG before the consensus guideline was finalized and submitted for publication.
Implementation and update
To facilitate the implementation of the recommendations in this consensus guideline, we strongly recommend cooperative paediatric and adult, pituitary-specific multidisciplinary meetings and staff training in nominated specialist centres. Potential barriers to implementation include lack of funding for novel medical therapies, lack of paediatric-specific expertise for diagnostic procedures (petrosal sinus sampling) or treatments (surgical expertise or proton beam therapy), and lack of access to expert centres due to geography or insurance restrictions. Our consensus guideline could support health-care providers, patient advocates and policy-makers to overcome these barriers and might facilitate these services where they are currently not available. The literature will be reviewed again 5 years after the publication of this consensus guideline; if, prior to this, any new evidence is identified that notably changes the recommendations, then the update will occur sooner.
Recommendations
General statements
-
Part 1: R1. Offer CYP with suspected or confirmed pituitary adenoma management in a specialist age-appropriate endocrine and neuro-oncology centre by an MDT working collaboratively with appropriate local health-care professionals (strong recommendation, low-quality evidence, Delphi 100%).
-
Part 1: R2. Offer all CYP with a pituitary mass growth and pubertal assessment and baseline pituitary hormone measurements (strong recommendation, high-quality evidence).
-
Part 1: R3. Clinicians treating CYP with pituitary adenomas should have access to a national paediatric pituitary-specific advisory panel in order to discuss the management of complex patients (strong recommendation, low-quality evidence, Delphi 90%).
-
Part 1: R4.1. Report CYP with a confirmed pituitary adenoma to an appropriate national registry (strong recommendation, low-quality evidence, Delphi 90%).
-
Part 1: R4.2. Offer transfer to adult pituitary services for continued surveillance at completion of growth and puberty (strong recommendation, low-quality evidence, Delphi 89%).
No published evidence is available to guide the organization of age-specific services for the management of pituitary and other rare endocrine tumours in CYP. All CYP with a suspected pituitary adenoma or any radiological abnormality in the region of the pituitary fossa and stalk require clinical assessment of growth and puberty and its age-appropriate timing. Baseline assessment for pituitary hormone deficiencies and specific investigations for hormone excess21 should be performed, coordinated and interpreted by a paediatric endocrinologist with expertise in pituitary disorders at a specialist centre. The availability of paediatric pituitary-specific advisory panels is scarce in various countries and setting these up would benefit the management of pituitary adenomas in CYP22. Consultation with an adult endocrinologist specializing in pituitary adenomas for the interpretation of results is key for care in the majority of patients. Close interaction between paediatric and adult endocrine services is required to coordinate long-term medical care and the transition to adult services. The timing of this transition depends on local guidelines but could be variable for patients with pituitary adenoma due to potential developmental delays. Patient support groups for pituitary patients (for example, the Pituitary Foundation, Child Growth Foundation, AMEND, Success Charity, Pituitary Network Association and World Alliance of Pituitary Organizations) offer educational resources and support communities that highlight the unique challenges affecting this developmental age group and could provide help for people living with pituitary disease.
Neuroimaging
-
Part 1: R5. Offer pre-contrast (T1 and T2) and post-contrast-enhanced (T1) thin-sliced pituitary MRI, including post-contrast volumetric (gradient (recalled) echo) sequences for increased sensitivity, to CYP presenting with a visual field defect or with signs and symptoms of pituitary hypersecretion or hyposecretion (strong recommendation, low-quality evidence, Delphi 92%).
-
Part 1: R6. Consider 3-Tesla MRI for surgical planning or intraoperative MRI as it enhances anatomical definition and might improve completeness of resection without altering complication rates (moderate recommendation, low-quality evidence, Delphi 92%).
In CYP undergoing investigation for suspected pituitary adenoma, a dedicated pituitary MRI before (T1 and T2) and after gadolinium contrast enhancement (T1) is the imaging investigation of choice and should be reported by a neuroradiologist. The standard pituitary protocol (2 mm slice, spin echo T1-weighted sequences performed before and after contrast, and fast or turbo spin echo T2-weighted sequences pre-contrast) can be supplemented by a volumetric (gradient (recalled) echo) acquisition after contrast, and some evidence suggests that this strategy could improve the sensitivity for adenoma detection23,24,25,26,27,28. The differential diagnosis of pituitary fossa lesions in CYP (for example, Rathke cleft cysts or craniopharyngioma) is beyond the scope of this consensus guideline, but these entities have separate guidelines29,30.
In patients with suspected pituitary adenoma where MRI is negative or equivocal, molecular (functional) imaging might aid neoplasm localization31. Specifically, hybrid imaging techniques (for example, PET–CT co-registered with MRI or PET–MRI) using ligands such as 11C-methionine or 18F-fluoroethyltyrosine have shown promising results in both de novo and recurrent functioning pituitary adenomas; however, the successful use of these imaging modalities has only been reported in a small number of CYP to date31,32 and these techniques are currently in the research stage.
The better resolution of a 3-Tesla MRI can improve anatomical delineation of pituitary adenomas and might enhance surgical planning but, as yet, there is no evidence of an increased sensitivity for adenoma detection33. Intraoperative MRI might improve complete resection rates of adenomas without increasing complication rates34,35,36,37,38,39,40. Low-level gadolinium deposits in the dentate nucleus and globus pallidus have unknown neurological impact. Therefore, unenhanced T1-weighted and T2-weighted MRI sequences should be considered during follow-up in paediatric patients41,42,43, especially if good quality enhanced images have been obtained at diagnosis. Macrocyclic or newer linear gadolinium-containing contrast agents should be used in weight-adapted doses. In patients with an estimated glomerular filtration rate of <30 ml/min/1.73 m2 or on dialysis, administration of gadolinium-containing contrast should be considered individually, and alternative imaging modalities utilized whenever possible. If gadolinium-containing contrast agents are necessary, macrocyclic or newer linear gadolinium-containing contrast agents could be administered with patient or parental consent citing an exceedingly low risk (much less than 1%) of developing nephrogenic systemic fibrosis44.
Visual assessment
-
Part 1: R7. In CYP with suspected or confirmed pituitary adenoma, offer assessment of visual acuity (ideally logarithm of the minimum angle of resolution measurement), visual fields (ideally Goldmann perimetry) and fundoscopy, with or without colour vision (strong recommendation, low-quality evidence, Delphi 94%).
-
Part 1: R8. In CYP with confirmed pituitary adenoma with potentially severe acuity or field deficits, consider baseline optical coherence tomography (weak recommendation, low-quality evidence, GDG consensus).
-
Part 1: R9.1. Consider visual assessment (including acuity and fields if age appropriate) in all CYP with a pituitary macroadenoma within 3 months of first-line therapy (moderate recommendation, low-quality evidence, Delphi 94% and GDG consensus).
-
Part 1: R9.2. Ongoing visual follow-up should be based on individual indications (moderate recommendation, low-quality evidence, Delphi 81% and GDG consensus).
Pituitary macroadenomas can impinge on the optic chiasm and optic nerves. Visual disturbances are more often encountered in CYP with pituitary adenoma than in adult patients. Data on visual function testing in patients with paediatric pituitary adenomas are scarce. Yet, studies of children with other lesions of the sellar or suprasellar region that affect vision and various other causes of visual impairment suggest that visual acuity, visual field testing and assessment of optical nerve integrity as well as fundoscopy can detect abnormalities at diagnosis45,46,47,48,49. Visual acuity is a psychophysical measure that relies on patient cooperation and attention. Qualitative measures of visual acuity are insufficient and subtle and even large changes in visual acuity might not be adequately detected by these methods. Instead, visual acuity should be measured with age-specific tests and recorded as the internationally recognized logarithm of the minimum angle of resolution measurement50.
Age-appropriate visual field testing is of key importance in patients with pituitary macroadenomas as well as in those with microadenomas after surgery. No data are available on optical coherence tomography in paediatric patients with pituitary adenomas, but optical coherence tomography can be a surrogate for visual field loss and visual dysfunction as a thinner retinal nerve fibre layer is present in patients with visual field loss, reduced visual acuity or evidence of optic neuropathy51. Although the use of optical coherence tomography is limited by patient cooperation, this is required to a lesser extent than in visual field testing. Despite variability in cooperation among children aged under 6 years, reliable optical coherence tomography imaging was obtained in children from as young as 3 years of age52. No data are available for visual evoked potentials (a measure of the electrical signal generated at the visual cortex in response to visual stimulation) in CYP with pituitary adenomas. Visual evoked potentials have been used for non-verbal or disabled children, where standard visual assessment is difficult, but should not be used for long-term surveillance29,53.
If CYP with pituitary adenomas are treated with surgery, further recovery of visual field deficits is unlikely after the first post-operative month54,55, with age <6 years and the presence of visual symptoms at diagnosis indicating an increased risk of poor visual outcomes56,57. Monitoring of CYP with pituitary adenomas should be determined on an individual patient basis, depending on baseline visual assessment and MRI appearance. Given the data from adults with pituitary adenoma58 and from paediatric patients with craniopharyngioma (a neoplasm of the sellar or suprasellar region that can also affect vision)29, the GDG strengthened the visual assessment recommendations (Part 1: R8 and R9).
Histopathology
-
Part 1: R10 Offer histopathological assessment of the operated pituitary adenoma tissue, including immunostaining for pituitary hormones and Ki-67, and additional immunoprofiling when relevant, to accurately classify the pituitary neoplasm (strong recommendation, moderate-quality evidence, Delphi 100%).
Data from adult patients with pituitary adenoma who undergo surgery and the recent WHO guidelines12,59 suggest that Ki-67 staining and mitotic activity might help predict clinical outcomes in adults60,61,62. While available data on the prognostic value of Ki-67 is controversial, the 2022 WHO guideline encourages accurate quantification (positive staining per 500–1,000 neoplastic cells in two hotspots). Therefore, prospective evaluation is recommended in CYP to identify correlates with outcomes (Box 1).
A paediatric pituitary adenoma surgical series found that 55% (28/51) of patients had Ki-67 of ≥3%5. Furthermore, data on 42 paediatric pituitary tumours suggested that the combination of ≥3% Ki-67 and local invasion on imaging predicts a 25% recurrence rate after surgery63. Recommendations from the European Pituitary Pathology Group for standardized reporting of paediatric and adult pituitary neoplasms suggest a multilevel approach, with pituitary hormones, cytokeratin and Ki-67 as the most basic report64. Transcription factors should be added if the sample is immunonegative or has scanty hormonal staining or if there is a plurihormonal or unusual combination of hormone staining. In selected cases, chromogranin, somatostatin receptor and p53 staining can be added based on further clinical information64. O6-methylguanine-DNA methyltransferase immunohistochemistry can be useful if considering temozolomide therapy for aggressively growing tumours65 as strong staining might predict a lack of response. Electron microscopy is not routinely used in molecular pathology of pituitary neoplasms from CYP but might assist in selected patients. Several studies have provided data on the molecular pathology of pituitary neoplasms, which might have a role in their future classification61,66. Given data from adult pituitary adenoma guidelines65 and the recent WHO classifications12,59, the GDG strengthened recommendation R10.
Genetics
-
Part 1: 11.1. Offer genetic assessment to all CYP with a pituitary adenoma to inform management and family surveillance (strong recommendation, high-quality evidence).
-
Part 1: 11.2. Given the high prevalence of genetic abnormalities in somatotroph and lactotroph tumours, offer genetic testing to all CYP with growth hormone (GH) and prolactin excess (strong recommendation, high-quality evidence).
Several genes have been identified in association with pituitary adenomas in CYP occurring as isolated pituitary adenomas (familial isolated pituitary adenoma) or as part of a syndromic disease67,68,69,70,71. Although these conditions are rare, the number of identified germline (and somatic) genetic alterations is expected to increase in the future with the implementation of wider genetic testing. This knowledge could inform prognosis, treatment and screening for other manifestations in the proband, while family members could benefit from genetic testing and clinical screening72,73,74,75,76. Genetic testing is available in several laboratories that also support testing for international patients.
Genetic assessment of potential mutation carriers of known mutations should be performed prior to the typical age at onset of symptoms (variable for different diseases). Some advocate genetic screening from the age of the youngest known patient (for example, aged 4 years for AIP mutations77), whereas others suggest genetic screening at the point where biochemical screening is advised if the patient is a carrier (for example, aged 5–10 years for multiple endocrine neoplasia type 1 syndrome (MEN1)78). Follow-up of gene mutation carriers might include yearly clinical and biochemical follow-up. Timing of pituitary MRI screening and assessment of other potentially associated features depend on the genetic disease in question. Treatment of pituitary neoplasms of genetic origin, in general, is similar but might require more treatment modalities compared with patients without genetic aetiology72,74.
If mutations in known genes have been ruled out in a proband with young-onset or familial disease, no clinical assessment is recommended for family members as genetic background is uncertain, penetrance is probably incomplete and regular long-term screening could lead to anxiety and increased health expenses77.
GH excess in CYP
Among all pituitary adenomas, childhood-onset GH-secreting adenomas (with or without prolactin co-secretion) are most likely to have an identifiable genetic cause79; for example, almost 50% of patients with gigantism have an identifiable genetic alteration79,80. Germline genetic abnormalities in CYP with GH-secreting pituitary adenomas have been identified in patients with familial isolated pituitary adenoma (AIP, GPR101 (female predominance, causing X-linked acrogigantism; X-LAG)) or with syndromic disease (MEN1, CDKN1B, PRKAR1A, PRKACB, SDHx and MAX). In X-LAG, duplications in the Xq26.3 region lead to enhanced GPR101 gene expression via disruption of the topologically associating domain (TAD) surrounding the gene, so X-LAG represents a TADopathy81. Mosaic mutations have been seen in GNAS (McCune–Albright syndrome) and GPR101 (in boys), whereas somatic GNAS mutations restricted to the pituitary are rare in CYP unlike in adults, where they have been identified in 20–40% of tumour samples82,83,84. In CYP with GH-secreting adenoma, AIP mutations (29% of patients with gigantism) and duplication in GPR101 (10%) occur most frequently, followed by McCune–Albright syndrome (5%), Carney complex (1%), MEN1 (1%)79 and, rarely, MEN1-like disease or phaeochromocytoma–paraganglioma-related gene alterations.
Prolactinomas in CYP
MEN1 and AIP germline abnormalities occur in both familial and apparently sporadic forms of prolactinoma73,74,85,86, while MEN1-like (MEN4 or the recently suggested MEN5 (ref. 87) due to MAX variants) or phaeochromocytoma–paraganglioma gene-related pituitary disease (also known as the three P Association or 3PA due to SDHx variants) is rare. In patients with a macroprolactinoma diagnosed before their twentieth birthday, 14% have a genetic aetiology (5% MEN1 and 9% AIP)86, while 34% of patients with MEN1 under 21 years of age have a pituitary adenoma, 70% of these being prolactinomas73. In an AIP mutation-positive patient cohort, 10% had a prolactinoma, and a third of these had childhood-onset disease74. Of note, patients with microprolactinomas and AIP mutation have been described in a familial setting, but only extremely rarely in a sporadic setting74. It has been reported that some patients with hyperprolactinaemia but no detectable pituitary mass and variable phenotype have prolactin receptor mutations; however, none manifested symptoms in childhood88,89. No other gene has been reliably identified in familial or sporadic childhood-onset prolactinomas. For follow-up of patients with MEN1 mutations, we refer to the MEN1 guidelines78.
Corticotroph pituitary tumours in CYP
Germline mutations are rare in CYP with corticotroph adenomas85,90. MEN1 mutations have occasionally been identified in both microadenomas and macroadenomas (2 of 55 patients with MEN1 aged <21 years)73,91,92. Variants in CABLES1 (2 of 146 paediatric patients with corticotrophinomas) and CDKN1B (3 of 190 paediatric patients with or without additional MEN1-like manifestations) have also been identified90,93. A unique form of Cushing disease due to infant-onset pituitary blastoma has been associated with DICER1 syndrome, with very low penetrance (<1%); pituitary blastoma is pathognomic for DICER1 mutations based on the 18 cases published94,95. One patient has also been identified with DICER1 syndrome-related pituitary blastoma diagnosed later in childhood96,97.
Somatic mutations of the USP8 deubiquitinase gene have been implicated in over a third of childhood98 and adult-onset99,100,101 corticotrophinomas, most typically in female patients with corticotroph microadenomas. In one case report, developmental delay was associated with a germline USP8 mutation and Cushing disease102. Large somatic genomic aberrations in the DNA of paediatric corticotrophinomas might indicate a more aggressive neoplasm compared to tumours without large genomic aberrations103.
TSHomas
TSHomas have not been associated with germline genetic alterations in CYP, except in one patient with resistance to thyroid hormone due to THRB mutation and a TSHoma104. TSHomas have rarely been described in adult patients with MEN1 and AIP variants71.
Non-functioning pituitary adenomas in CYP
Non-functioning pituitary adenomas (NFPAs) occur in 25% of CYP with MEN1 syndrome. Non-functioning microadenomas, not dissimilar to incidentalomas, have been identified as part of clinical screening in MEN1 and AIP mutation-positive CYP72,73,74. In a few AIP mutation-positive CYP, clinically non-functioning but GH and prolactin immunostaining-positive macroadenomas have been identified74,85. Functioning gonadotroph adenoma in childhood has not been described with a germline mutation.
Pituitary surgery
-
Part 1: R12. If surgery is indicated in CYP with pituitary adenoma, offer transsphenoidal surgery as the technique of choice, even in patients with incompletely pneumatized sphenoid sinuses (strong recommendation, low-quality evidence, Delphi 100% and GDG consensus).
-
Part 1: R13. In CYP with pituitary adenoma, consider endoscopic rather than microscopic transsphenoidal surgery for its potentially superior efficacy in preserving pituitary function (weak recommendation, low-quality evidence, Delphi 86%).
-
Part 1: R14. In all CYP with pituitary adenoma who undergo surgery, offer strict fluid and electrolyte balance monitoring peri-operatively and post-operatively (strong recommendation, moderate-quality evidence, Delphi 100%).
In patients with pituitary adenoma, surgery is often a necessary primary or secondary intervention. In CYP with pituitary adenoma, transsphenoidal resection by pituitary surgeons in age-appropriate neurosurgical units with extensive experience (at least 50 pituitary operations per year per unit105,106,107), including in children, is a safe and effective procedure108,109,110,111,112.
In CYP, transsphenoidal surgery by an experienced pituitary surgeon is the definitive treatment of choice for most pituitary adenomas, even in children with incompletely pneumatized sinuses; intraoperative image guidance might be additionally helpful. In a study of 66 children with pituitary adenomas113, 17% of patients required drilling of incompletely pneumatized sphenoid sinuses; however, anatomical differences related to patient age or size were not a limiting factor to the surgical procedure or its outcome. Likewise, further transsphenoidal surgery, if necessary, was performed with minimal difficulty and with results approaching those in adults undergoing debulking or removal of recurrent or residual lesions113.
Changes in water metabolism and regulation of arginine vasopressin (AVP) are common complications of pituitary surgery114,115. Several patterns have been observed, for example, transient or permanent AVP deficiency, biphasic response with signs of AVP deficiency followed by inappropriate antidiuresis (SIADH), and triphasic pattern with usually permanent AVP deficiency after the two phases of the biphasic pattern. Patients must be managed in a setting where close observations (including careful monitoring of fluid input and output) can occur so that any concerns can be flagged and raised with an expert endocrinologist at an early stage116,117. In a retrospective study of 160 children undergoing transsphenoidal surgery for pituitary neoplasms, the post-operative incidence of AVP deficiency (diabetes insipidus) and SIADH was 26% and 14%, respectively114. Risk factors for AVP deficiency or SIADH were female sex, cerebrospinal fluid leak, drain after surgery, invasion of the posterior pituitary by the tumour or manipulation of the posterior pituitary during surgery.
In CYP with pituitary apoplexy, the GDG suggests adopting the recommendations of available adult guidelines118 given the limited case reports and case series in CYP115,119,120,121,122,123,124. However, paediatric pituitary apoplexy can be more severe than in adults and selected patients might benefit from early surgery123.
Endoscopic over microscopic transsphenoidal techniques are increasingly used in pituitary surgery and are perceived as providing better operative visualization and fewer perioperative complications and hormone deficiencies125. While further data are needed to show the clear advantage of endoscopic surgery, most adult guidelines agree that surgeon experience is more important to the outcome than surgical technique (microscopic or endoscopic)126. Endoscopic transsphenoidal pituitary surgery in CYP with Cushing disease shows an excellent efficacy outcome125 and improved safety, reducing surgical trauma, pain perception, paediatric intensive care unit admissions, blood transfusions, anterior pituitary deficiencies and incidence of AVP deficiency125,127,128. Over time, this strategy could become the standard surgical approach in children as is current practice in adults. Post-operative high-quality outpatient support for CYP for biochemical assessment can shorten the hospital stay129.
Indications for repeat pituitary surgery in recurrent or progressive disease are detailed for each pituitary adenoma type in Part 2 of this consensus guideline16.
Radiotherapy
-
Part 1: R15. In CYP with pituitary adenoma, offer radiotherapy when the tumour is symptomatic, growing, resistant to medical therapy and surgically inaccessible (strong recommendation, low-quality evidence, Delphi 94%).
-
Part 1: R16. Consider clinical radiation treatment protocols for CYP according to adult guidelines or paediatric regimens for similarly located tumours (moderate recommendation, low-quality evidence, Delphi 94%).
-
Part 1: R17. Consider external beam fractionated radiotherapy at a total dose of 45–50.4 Gy in 1.8 Gy daily fractions to CYP with pituitary adenomas indicated for radiotherapy; offer fractionated radiotherapy as proton beam therapy, where available, or as highly conformal photon therapy; single-fraction radiosurgery might be appropriate in older patients in individual circumstances (moderate recommendation, low-quality evidence, Delphi 100% and GDG consensus).
The evidence for radiotherapy in CYP with pituitary adenomas is both limited and inconsistently reported. Some studies consider all adenomas108,130,131,132,133, while others report on specific tumour types separately110,134,135,136,137,138,139. While focal radiotherapy (photon or proton beam therapy) is consistently administered to salvage those CYP with pituitary adenomas who have relapsed following surgery, no standardized timing of treatment indication has been developed (for example, number of surgeries offered prior to radiotherapy)140. Moreover, there is a lack of data on dose fractionation or radiation modality comparisons that assess effectiveness or risk–benefit outcomes. Thus, few data are available on which to base recommendations regarding conventional photon radiation versus high-energy proton beam therapy or stereotactic radiosurgery. Even fewer toxicity data exist, particularly regarding cognitive outcomes, vasculopathies, secondary tumours and wider endocrinopathies, especially relevant to CYP.
If radiotherapy is needed, highly conformal radiotherapeutic techniques should be used according to availability. Options include high-energy photon-based therapy (delivered as intensity-modulated radiotherapy or conventionally fractionated stereotactic radiotherapy), proton beam fractionated radiotherapy or hypo-fractionated stereotactic radiosurgery.
In CYP with pituitary adenomas, the largest clinical experience comes from conventionally fractionated external beam photons. Intensity-modulated radiation therapy (including volumetric modulated and tomotherapy arc techniques) and stereotactic radiotherapy with photons have more conformal coverage than older 3D-conformal radiotherapy techniques, thereby reducing high radiation doses to organs at risk outside the treated volume141,142,143,144,145,146, however, intensity-modulated radiation therapy still exposes surrounding normal tissue to a low dose of radiation.
In adults with pituitary adenomas, the total radiation dose recommendation is usually 45–50.4 Gy, 1.8 Gy per fractionation, once a day, 5 days per week over 25 or 30 days146. This regimen has been demonstrated to cure children with Cushing disease147. All regimens should limit radiation delivery to no more than 1.8 Gy per fraction in keeping with modern paediatric cranial radiation schedules.
Despite the restrictions of cost and availability, modern fractionated external beam therapy with protons is increasingly applied to paediatric neoplasms driven by the expected decrease in late effects148,149,150. Prospective data collection for long-term endocrine, vascular, secondary malignancy and cognitive outcomes for proton beam therapy in CYP is ongoing already in the UK and represents one of our research recommendations (Box 1).
Stereotactic radiosurgery delivers a single large radiotherapeutic fraction to a limited volume with a restricted margin. This technique is routinely used for irradiating pituitary neoplasms in adults. Single-fraction radiosurgery lacks long-term safety data in CYP and concerns have been raised regarding late toxicity, with younger children, especially under 5 years, possibly being at increased risk of vasculopathy and cognitive impairment.
In CYP with NFPA, radiotherapy might be considered as an adjuvant therapy after subtotal resection or where surgery is contraindicated. Radiotherapy might also be considered as second-line therapy for radiological progression or recurrence. In CYP with hormone-secreting pituitary adenomas, radiotherapy should be considered in patients with biochemical progression despite maximal surgery and medical therapy147, although no clear risk–benefit analysis has been performed to identify the number of times surgery should be attempted before proceeding to radiotherapy. An age-appropriate pituitary MDT should determine radiation treatment options on an individual patient basis29,151.
Risk–benefit outcome data is insufficient to support one radiotherapy treatment modality over another139,152,153. However, where the planned target volume includes the optic chiasm or optic nerves, stereotactic radiosurgery should be avoided and fractionated radiotherapy should be employed instead as the stereotactic radiosurgery dose typically exceeds tissue tolerance. On the two Delphi consensus rounds performed, individual experts held particularly strong positions and disagreements occurred, with those who expressed a preference for stereotactic radiosurgery139 against those who have concerns about the late effects of high doses per fraction in children. Both sides agreed that fairly little data exist on important long-term health, well-being and cognitive function following single-fraction radiation in CYP.
Radiotherapy: outcomes
Adjuvant radiotherapy after transsphenoidal surgery achieves long-term tumour control in over 90% of adult patients with NFPA134,154,155. Endocrinological criteria determining biochemical remission vary across reported series, making it difficult to compare tumour control in functioning pituitary adenomas. Specific data for Cushing disease can be found in Part 2 data16. Of note, 4 out of 12 CYP with GH excess achieved remission after radiosurgery139.
Radiotherapy: adverse effects
Hypopituitarism is one of the most common adverse effects in CYP with pituitary adenomas who undergo radiotherapy. GH deficiency could be present at diagnosis due to tumour location and is universally present by 5 years after radiotherapy. Hypopituitarism with multiple hormone deficiencies evolves over time to an incidence of ~20% at 5 years after radiotherapy and 80% at 10–15 years155,156, although late effects of surgery or the evolving tumour also have a role. In CYP who undergo radiotherapy, follow-up for hypopituitarism needs to be lifelong, with planned transition to specialist adult services.
The young brain, although more plastic than the adult brain, is also more vulnerable to injury; for example, stereotactic radiosurgery might carry a higher risk of radionecrosis in CYP than standard fractionated external beam radiotherapy157. Other late effects of concern, particularly in children, include neurocognitive sequelae137, cerebrovascular events and second malignancies158. In a group of 462 patients with pituitary adenoma (age range 10–83 years), Sattler et al.159 reported no increased incidence of secondary tumours or mortality in patients receiving adjuvant post-operative radiotherapy compared with those treated with surgery alone. By contrast, Minniti et al.160 reported a 2.4% risk of secondary brain tumours at 20 years after surgery and radiotherapy for pituitary adenoma in adults. However, long-term mortality from secondary brain tumours was minimal and mortality predominantly arose from cerebrovascular events of complex multifactorial aetiology. Thus, these authors concluded that the low incidence of secondary brain tumours should not preclude the use of radiotherapy as an effective treatment modality in patients with otherwise uncontrolled pituitary adenomas.
In a large cohort of adult patients with GH deficiency from a GH treatment data base, secondary tumour incidence rate ratios for those who underwent radiotherapy to treat their primary pituitary tumour (pituitary adenoma or craniopharyngioma) versus no radiotherapy was 3.34 for malignant brain tumours and 4.06 for meningiomas. With every 10 years of younger age, the risk of developing a malignant brain tumour increased by 2.4 fold and the risk of meningioma increased by 1.6-fold161. Incidence rates were similar in patients treated with conventional and stereotactic radiotherapy. The authors concluded that there was a statistically significant increased risk of developing a malignant brain tumour and a meningioma after radiotherapy for pituitary tumours, especially when given at age <30 years, and emphasized the need for caution in balancing the risk–benefit ratio of radiotherapy in young patients161. A very high meningioma risk (standardized incidence ratio of 658) was also found after cranial radiotherapy in the Safety and Appropriateness of Growth Hormone Treatments in Europe cohort (10,403 children treated with GH), but GH in replacement doses to children with GH deficiency was not implicated in the risk of secondary malignancies162,163.
Conclusions
The limited evidence base for the diagnosis and management of paediatric pituitary adenomas, combined with the typical lack of dedicated age-appropriate pituitary specialty teams and services within paediatric neuro-oncology centres, inequitably disadvantage CYP with pituitary adenomas with respect to optimal care and compromise their outcomes. The purpose of these recommendations (Supplementary Table 1) is to raise awareness of the potentially occult and sometimes severe nature of this disease in CYP as well as to improve time to diagnosis and long-term health and well-being outcomes and create a future evidence base for audit improvement. Target users of this guideline are health professionals from a variety of disciplines (including paediatric endocrinology, adult endocrinology, pituitary and skull base neurosurgery, paediatric neurosurgery, oncology, paediatric ophthalmology, radiotherapy, radiology, histopathology, and genetics) involved in the management and long-term follow-up of childhood and adolescents with pituitary adenomas. If the level of care required by the patient is best provided in centres with specific expertise in pituitary diseases in CYP, referral to such centres should be considered.
Our recommendations for CYP with a pituitary mass is multidisciplinary assessment and care to include systematic pituitary hormone assessment, access to age appropriate expert neuroimaging, visual review, histopathology, informed genetic assessment, and evaluation by an expert pituitary surgeon working closely with the paediatric endocrinology, neuro-oncology and radiotherapy teams. Paediatric pituitary specialist centres offering expertise in diagnosis, treatment and follow-up of pituitary adenomas require urgent centralization around major adult pituitary and paediatric neuro-oncology treatment centres as these centres improve the evidence base for treatment and long-term patient benefit in such a rare, high survival condition of maturing children. Multi-professional pituitary expert teams will be best placed to meet the specific challenges and complexities of pituitary adenomas in children, gather the evidence needed to evaluate these consensus treatment recommendations in the future and improve the maturational, reproductive, long-term health and functional outcomes for CYP with these eminently curable neoplasms. Having reviewed the evidence and sought consensus opinion on areas where evidence is contradictory or poor, the GDG has suggested some research recommendations (Box 1).
Change history
19 February 2024
In the version of the article initially published, an earlier, incorrect version of the Supplementary Information was posted. This has now been amended, and the correct Supplementary Information file now accompanies the online article.
References
Fisher, B. J., Gaspar, L. E., Stitt, L. W. & Noone, B. E. Pituitary adenoma in adolescents: a biologically more aggressive disease? Radiology 192, 869–872 (1994).
Beckers, A., Petrossians, P., Hanson, J. & Daly, A. F. The causes and consequences of pituitary gigantism. Nat. Rev. Endocrinol. 14, 705–720 (2018).
Barry, S. & Korbonits, M. Update on the genetics of pituitary tumors. Endocrinol. Metab. Clin. North Am. 49, 433–452 (2020).
National Cancer Registration and Analysis Service. Children, Teenagers and Young Adults UK Cancer Statistics Report 2021, Public Health England http://www.ncin.org.uk/cancer_type_and_topic_specific_work/cancer_type_specific_work/cancer_in_children_teenagers_and_young_adults/ (2021).
Kelly, A. P., Greenfield, J. P., Dobri, G. A. & Schwartz, T. H. Pediatric pituitary adenomas are more aggressive, more likely to be hormone producing and are more difficult to cure than adult pituitary adenomas: case series and systematic literature review. Childs Nerv. Syst. 38, 729–738 (2022).
Jayant, S. S. et al. Paediatric pituitary adenomas: clinical presentation, biochemical profile and long-term prognosis. Neurol. India 70, 304–311 (2022).
Asa, S. L. et al. From pituitary adenoma to pituitary neuroendocrine tumor (PitNET): an International Pituitary Pathology Club proposal. Endocr. Relat. Cancer 24, C5–C8 (2017).
Trouillas, J. et al. Aggressive pituitary tumours and carcinomas: two sides of the same coin? Eur. J. Endocrinol. 178, C7–C9 (2018).
Ho, K. K. Y. et al. A tale of pituitary adenomas: to NET or not to NET: Pituitary Society position statement. Pituitary 22, 569–573 (2019).
Ho, K. K. Y. et al. The tale in evolution: clarity, consistency and consultation, not contradiction and confusion. Pituitary 23, 476–477 (2020).
Asa, S. L. et al. Pituitary neuroendocrine tumors (PitNETs): nomenclature evolution, not clinical revolution. Pituitary 23, 322–325 (2020).
Asa, S. L., Mete, O., Perry, A. & Osamura, R. Y. Overview of the 2022 WHO classification of pituitary tumors. Endocr. Pathol. 33, 6–26 (2022).
Ho, K. K. Y. et al. Pituitary adenoma or neuroendocrine tumour: the need for an integrated prognostic classification. Nat. Rev. Endocrinol. 19, 671–678 (2023).
Castellanos, L. E., Misra, M., Smith, T. R., Laws, E. R. & Iorgulescu, J. B. The epidemiology and management patterns of pediatric pituitary tumors in the United States. Pituitary 24, 412–419 (2021).
National Cancer Registration and Analysis Service. Cancer in children, teenagers and young adults, http://ncin.org.uk/cancer_type_and_topic_specific_work/cancer_type_specific_work/cancer_in_children_teenagers_and_young_adults/ (Access date:11/04/2023).
Korbonits, M. et al. Consensus guideline for the diagnosis and management of pituitary adenomas in childhood and adolescence: part 2, specific diseases. Nat. Rev. Endocrinol. https://doi.org/10.1038/s41574-023-00949-7 (2024).
Brouwers, M. C. et al. AGREE II: advancing guideline development, reporting and evaluation in health care. Can. Med. Assoc. J. 182, E839–842 (2010).
Children’s Cancer and Leukaemia Group. Children’s Cancer and Leukaemia Guideline Development Standard Operating Procedure, Version 5 https://www.cclg.org.uk/what-we-do/clinical-treatment-guidelines (Access date: 19/01/2022).
Schardt, C., Adams, M. B., Owens, T., Keitz, S. & Fontelo, P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med. Inform. Decis. Mak. 7, 16 (2007).
Atkins, D. et al. Grading quality of evidence and strength of recommendations. BMJ 328, 1490 (2004).
Perry, A. et al. Pediatric pituitary adenoma: case series, review of the literature, and a skull base treatment paradigm. J. Neurol. Surg. B Skull Base 79, 91–114 (2018).
Freund, K. et al. A 7-year update report of a national, interdisciplinary endeavour to improve outcomes for children and young people under 19 years of age with hypothalamic pituitary axis tumours (HPAT) using multi-site video conferencing. Horm. Res. Paediatr. 90 (Suppl. 1), 496–497 (2018).
Batista, D. et al. Detection of adrenocorticotropin-secreting pituitary adenomas by magnetic resonance imaging in children and adolescents with Cushing disease. J. Clin. Endocrinol. Metab. 90, 5134–5140 (2005).
Patronas, N. et al. Spoiled gradient recalled acquisition in the steady state technique is superior to conventional postcontrast spin echo technique for magnetic resonance imaging detection of adrenocorticotropin-secreting pituitary tumors. J. Clin. Endocrinol. Metab. 88, 1565–1569 (2003).
Chowdhury, I. N., Sinaii, N., Oldfield, E. H., Patronas, N. & Nieman, L. K. A change in pituitary magnetic resonance imaging protocol detects ACTH-secreting tumours in patients with previously negative results. Clin. Endocrinol. 72, 502–506 (2010).
Arbab, A. S. 3D gradient echo sequence provides better images in contrast-enhanced imaging of the pituitary gland at 3 T. Imaging Med. 2, 129–130 (2010).
Kakite, S. et al. Three-dimensional gradient echo versus spin echo sequence in contrast-enhanced imaging of the pituitary gland at 3T. Eur. J. Radiol. 79, 108–112 (2011).
Kasaliwal, R. et al. Volume interpolated 3D-spoiled gradient echo sequence is better than dynamic contrast spin echo sequence for MRI detection of corticotropin secreting pituitary microadenomas. Clin. Endocrinol. 78, 825–830 (2013).
Gan, H. W. et al. National UK guidelines for the management of paediatric craniopharyngioma. Lancet Diabetes Endocrinol. 11, 694–706 (2023).
Cerbone, M. et al. Management of children and young people with idiopathic pituitary stalk thickening, central diabetes insipidus, or both: a national clinical practice consensus guideline. Lancet Child. Adolesc. Health 5, 662–676 (2021).
Bashari, W. A. et al. Using molecular imaging to enhance decision making in the management of pituitary adenomas. J. Nucl. Med. 62, 57S–62S (2021).
Veldhuijzen van Zanten, S. E. M., Neggers, S., Valkema, R. & Verburg, F. A. Positive [18F]fluoroethyltyrosine PET/MRI in suspected recurrence of growth hormone-producing pituitary adenoma in a paediatric patient. Eur. J. Nucl. Med. Mol. Imaging 49, 410–411 (2021).
Pinker, K. et al. The value of high-field MRI (3T) in the assessment of sellar lesions. Eur. J. Radiol. 54, 327–334 (2005).
Berkmann, S., Fandino, J., Muller, B., Remonda, L. & Landolt, H. Intraoperative MRI and endocrinological outcome of transsphenoidal surgery for non-functioning pituitary adenoma. Acta Neurochir. 154, 639–647 (2012).
Szerlip, N. J. et al. Transsphenoidal resection of sellar tumors using high-field intraoperative magnetic resonance imaging. Skull Base 21, 223–232 (2011).
Nimsky, C., von Keller, B., Ganslandt, O. & Fahlbusch, R. Intraoperative high-field magnetic resonance imaging in transsphenoidal surgery of hormonally inactive pituitary macroadenomas. Neurosurgery 59, 105–114 (2006).
Wu, J. S. et al. Transsphenoidal pituitary macroadenomas resection guided by PoleStar N20 low-field intraoperative magnetic resonance imaging: comparison with early postoperative high-field magnetic resonance imaging. Neurosurgery 65, 63–70 (2009).
Fomekong, E. et al. Intraoperative 3T MRI for pituitary macroadenoma resection: initial experience in 73 consecutive patients. Clin. Neurol. Neurosurg. 126, 143–149 (2014).
Zhang, H. et al. Analysis of 137 patients who underwent endoscopic transsphenoidal pituitary adenoma resection under high-field intraoperative magnetic resonance imaging navigation. World Neurosurg. 104, 802–815 (2017).
Staartjes, V. E., Togni-Pogliorini, A., Stumpo, V., Serra, C. & Regli, L. Impact of intraoperative magnetic resonance imaging on gross total resection, extent of resection, and residual tumor volume in pituitary surgery: systematic review and meta-analysis. Pituitary 24, 644–656 (2021).
Holowka, S., Shroff, M. & Chavhan, G. B. Use and safety of gadolinium based contrast agents in pediatric MR imaging. Indian J. Pediatr. 86, 961–966 (2019).
Bonneville, J. F. A plea for the T2W MR sequence for pituitary imaging. Pituitary 22, 195–197 (2019).
Shah, R., D’Arco, F., Soares, B., Cooper, J. & Brierley, J. Use of gadolinium contrast agents in paediatric population: Donald Rumsfeld meets hippocrates! Br. J. Radiol. 92, 20180746 (2019).
Schieda, N. et al. Gadolinium-based contrast agents in kidney disease: a comprehensive review and clinical practice guideline issued by the Canadian Association of Radiologists. Can. J. Kidney Health Dis. 5, 2054358118778573 (2018).
Suharwardy, J. & Elston, J. The clinical presentation of children with tumours affecting the anterior visual pathways. Eye 11, 838–844 (1997).
Drimtzias, E. et al. The ophthalmic natural history of paediatric craniopharyngioma: a long-term review. J. Neurooncol. 120, 651–656 (2014).
Avery, R. A., Bouffet, E., Packer, R. J. & Reginald, A. Feasibility and comparison of visual acuity testing methods in children with neurofibromatosis type 1 and/or optic pathway gliomas. Invest. Ophthalmol. Vis. Sci. 54, 1034–1038 (2013).
Avery, R. A. et al. Visual acuity in children with low grade gliomas of the visual pathway: implications for patient care and clinical research. J. Neurooncol. 110, 1–7 (2012).
Beck, R. W. et al. Visual acuity as an outcome measure in clinical trials of retinal diseases. Ophthalmology 114, 1804–1809 (2007).
Fulton, A. B., Hansen, R., Moskowitz, A. & Mayer, D. In: Pediatric Ophthalmology and Strabismus 4th edn Ch. 4 https://doi.org/10.1016/B978-0-7020-4691-9.00004-2 (2013).
Bialer, O. Y., Goldenberg-Cohen, N., Toledano, H., Snir, M. & Michowiz, S. Retinal NFL thinning on OCT correlates with visual field loss in pediatric craniopharyngioma. Can. J. Ophthalmol. 48, 494–499 (2013).
Rufai, S. R. Handheld optical coherence tomography removes barriers to imaging the eyes of young children. Eye 25, 127–143 (2022).
Wenzel, D., Brandl, U., Beck, J. D., Cedzich, C. & Albert, F. Visual evoked potentials in tumors from orbita to occipital lobe in childhood. Neurosurg. Rev. 11, 279–286 (1988).
Repka, M. X., Miller, N. R. & Miller, M. Visual outcome after surgical removal of craniopharyngiomas. Ophthalmology 96, 195–199 (1989).
Stark, K. L., Kaufman, B., Lee, B. C., Primack, J. & Tychsen, L. Visual recovery after a year of craniopharyngioma-related amaurosis: report of a nine-year-old child and a review of pathophysiologic mechanisms. J. AAPOS 3, 366–371 (1999).
Abrams, L. S. & Repka, M. X. Visual outcome of craniopharyngioma in children. J. Pediatr. Ophthalmol. Strabismus 34, 223–228 (1997).
Fisher, P. G. et al. Outcomes and failure patterns in childhood craniopharyngiomas. Childs Nerv. Syst. 14, 558–563 (1998).
Chanson, P. et al. Management of clinically non-functioning pituitary adenoma. Ann. Endocrinol. 76, 239–247 (2015).
Lopes, M. B. et al. in Central Nervous System Tumours in WHO Classification of Tumours Series 5th edn, Vol. 6 (ed Daniel, J. B.) Ch. 12, 406–414 (International Agency for Research on Cancer, 2021).
Lloyd, R. V., Osamura, R. Y., Kloppel, G. & Rosai, J. WHO Classification of Tumours of Endocrine Organs 4th edn (International Agency for Research on Cancer, 2017).
Neou, M. et al. Pangenomic classification of pituitary neuroendocrine tumors. Cancer Cell 37, 123–134 e125 (2020).
Trouillas, J. et al. A new prognostic clinicopathological classification of pituitary adenomas: a multicentric case-control study of 410 patients with 8 years post-operative follow-up. Acta Neuropathol. 126, 123–135 (2013).
Chen, J., Schmidt, R. E. & Dahiya, S. Pituitary adenoma in pediatric and adolescent populations. J. Neuropathol. Exp. Neurol. 78, 626–632 (2019).
Villa, C. et al. A standardised diagnostic approach to pituitary neuroendocrine tumours (PitNETs): a European Pituitary Pathology Group (EPPG) proposal. Virchows Arch. 475, 687–692 (2019).
Raverot, G. et al. European Society of Endocrinology Clinical Practice Guidelines for the management of aggressive pituitary tumours and carcinomas. Eur. J. Endocrinol. 178, G1–G24 (2018).
Capper, D. et al. DNA methylation-based classification of central nervous system tumours. Nature 555, 469–474 (2018).
Vierimaa, O. et al. Pituitary adenoma predisposition caused by germline mutations in the AIP gene. Science 312, 1228–1230 (2006).
Trivellin, G. et al. Gigantism and acromegaly due to Xq26 microduplications and GPR101 mutation. N. Engl. J. Med. 371, 2363–2374 (2014).
Guaraldi, F., Storr, H. L., Ghizzoni, L., Ghigo, E. & Savage, M. O. Paediatric pituitary adenomas: a decade of change. Horm. Res. Paediatr. 81, 145–155 (2014).
Hannah-Shmouni, F., Trivellin, G. & Stratakis, C. A. Genetics of gigantism and acromegaly. Growth Horm. IGF Res. 30-31, 37–41 (2016).
Denes, J. & Korbonits, M. The clinical aspects of pituitary tumour genetics. Endocrine 71, 663–674 (2021).
Daly, A. F. et al. Clinical characteristics and therapeutic responses in patients with germ-line AIP mutations and pituitary adenomas: an international collaborative study. J. Clin. Endocrinol. Metab. 95, E373–E383 (2010).
Goudet, P. et al. MEN1 disease occurring before 21 years old: a 160-patient cohort study from the Groupe d’etude des Tumeurs Endocrines. J. Clin. Endocrinol. Metab. 100, 1568–1577 (2015).
Marques, P. et al. Significant benefits of AIP testing and clinical screening in familial isolated and young-onset pituitary tumors. J. Clin. Endocrinol. Metab. 105, e2247–2260 (2020).
Salenave, S., Boyce, A. M., Collins, M. T. & Chanson, P. Acromegaly and McCune-Albright syndrome. J. Clin. Endocrinol. Metab. 99, 1955–1969 (2014).
Rodd, C. et al. Somatic GPR101 duplication causing X-Linked acrogigantism (XLAG)-diagnosis and management. J. Clin. Endocrinol. Metab. 101, 1927–1930 (2016).
Korbonits, M., Storr, H. & Kumar, A. V. Familial pituitary adenomas — who should be tested for AIP mutations? Clin. Endocrinol. 77, 351–356 (2012).
Thakker, R. V. et al. Clinical practice guidelines for multiple endocrine neoplasia type 1 (MEN1). J. Clin. Endocrinol. Metab. 97, 2990–3011 (2012).
Rostomyan, L. et al. Clinical and genetic characterization of pituitary gigantism: an international collaborative study in 208 patients. Endocr. Relat. Cancer 22, 745–757 (2015).
Iacovazzo, D. et al. Germline or somatic GPR101 duplication leads to X-linked acrogigantism: a clinico-pathological and genetic study. Acta Neuropathol. Commun. 4, 56 (2016).
Franke, M. et al. Duplications disrupt chromatin architecture and rewire GPR101-enhancer communication in X-linked acrogigantism. Am. J. Hum. Genet. 109, 553–570 (2022).
Johnson, M. C. et al. Gps mutations in Chilean patients harboring growth hormone-secreting pituitary tumors. J. Pediatr. Endocrinol. Metab. 12, 381–387 (1999).
Hernandez-Ramirez, L. C. et al. Landscape of familial isolated and young-onset pituitary adenomas: prospective diagnosis in AIP mutation carriers. J. Clin. Endocrinol. Metab. 100, E1242–E1254 (2015).
Watanabe, D. et al. GH/PRL-secreting pituitary macroadenoma associated with GNAS p.Gln227Leu mutation: pediatric case report and review. Endocr. J. 66, 403–408 (2019).
Cuny, T. et al. Genetic analysis in young patients with sporadic pituitary macroadenomas: besides AIP don’t forget MEN1 genetic analysis. Eur. J. Endocrinol. 168, 533–541 (2013).
Salenave, S. et al. Macroprolactinomas in children and adolescents: factors associated with the response to treatment in 77 patients. J. Clin. Endocrinol. Metab. 100, 1177–1186 (2015).
Seabrook, A. J. et al. Multiple endocrine tumors associated with germline MAX mutations: multiple endocrine neoplasia type 5? J. Clin. Endocrinol. Metab. 106, 1163–1182 (2021).
Kobayashi, T., Usui, H., Tanaka, H. & Shozu, M. Variant prolactin receptor in agalactia and hyperprolactinemia. N. Engl. J. Med. 379, 2230–2236 (2018).
Newey, P. J. et al. Mutant prolactin receptor and familial hyperprolactinemia. N. Engl. J. Med. 369, 2012–2020 (2013).
Chasseloup, F. et al. Germline CDKN1B loss-of-function variants cause pediatric Cushing’s disease with or without an MEN4 phenotype. J. Clin. Endocrinol. Metab. 105, 1983–2005 (2020).
Rix, M. et al. Cushing’s disease in childhood as the first manifestation of multiple endocrine neoplasia syndrome type 1. Eur. J. Endocrinol. 151, 709–715 (2004).
Stratakis, C. A. et al. Pituitary macroadenoma in a 5-year-old: an early expression of multiple endocrine neoplasia type 1. J. Clin. Endocrinol. Metab. 85, 4776–4780 (2000).
Hernandez-Ramirez, L. C. et al. Loss-of-function mutations in the CABLES1 gene are a novel cause of Cushing’s disease. Endocr. Relat. Cancer 24, 379–392 (2017).
de Kock, L. et al. Pituitary blastoma: a pathognomonic feature of germ-line DICER1 mutations. Acta Neuropathol. 128, 111–122 (2014).
Liu, A. P. Y. et al. Clinical outcomes and complications of pituitary blastoma. J. Clin. Endocrinol. Metab. 106, 351–363 (2021).
Chhuon, Y. et al. Pituitary blastoma in a 19-year-old woman: a case report and review of literature. World Neurosurg. 139, 310–313 (2020).
Chong, A. S. et al. DICER1 syndrome in a young adult with pituitary blastoma. Acta Neuropathol. 32, 969–977 (2021).
Faucz, F. R. et al. Somatic USP8 gene mutations are a common cause of pediatric Cushing disease. J. Clin. Endocrinol. Metab. 102, 2836–2843 (2017).
Reincke, M. et al. Mutations in the deubiquitinase gene USP8 cause Cushing’s disease. Nat. Genet. 47, 31–38 (2015).
Perez-Rivas, L. G. et al. The gene of the ubiquitin-specific protease 8 is frequently mutated in adenomas causing cushing’s disease. J. Clin. Endocrinol. Metab. 100, E997–1004, (2015).
Ma, Z. Y. et al. Recurrent gain-of-function USP8 mutations in Cushing’s disease. Cell Res. 25, 306–317 (2015).
Cohen, M. et al. Germline USP8 mutation associated with pediatric Cushing disease and other clinical features: a new syndrome. J. Clin. Endocrinol. Metab. 104, 4676–4682 (2019).
Tatsi, C. et al. Large genomic aberrations in corticotropinomas are associated with greater aggressiveness. J. Clin. Endocrinol. Metab. 104, 1792–1801 (2019).
Teng, X. et al. A patient with a thyrotropin-secreting microadenoma and resistance to thyroid hormone (P453T). J. Clin. Endocrinol. Metab. 100, 2511–2514 (2015).
Wass, J. A. H. & Lansdown, M. Endocrinology, Getting It Right First Time (GIRFT) Programme National Specialty Report https://www.gettingitrightfirsttime.co.uk/wp-content/uploads/2021/08/EndocrinologyReport-Aug21o-NEW.pdf (2021).
Casanueva, F. F. et al. Correction to: criteria for the definition of pituitary tumor centers of excellence (PTCOE): a pituitary society statement. Pituitary 21, 663 (2018).
Honegger, J. & Grimm, F. The experience with transsphenoidal surgery and its importance to outcomes. Pituitary 21, 545–555 (2018).
Pandey, P., Ojha, B. K. & Mahapatra, A. K. Pediatric pituitary adenoma: a series of 42 patients. J. Clin. Neurosci. 12, 124–127 (2005).
Kanter, A. S. et al. Single-center experience with pediatric Cushing’s disease. J. Neurosurg. 103, 413–420 (2005).
Joshi, S. M. et al. Cushing’s disease in children and adolescents: 20 years of experience in a single neurosurgical center. Neurosurgery 57, 281–285 (2005).
Gkourogianni, A. et al. Death in pediatric Cushing syndrome is uncommon but still occurs. Eur. J. Pediatr. 174, 501–507 (2015).
Dhandapani, S. et al. Endonasal endoscopic versus microscopic transsphenoidal surgery in pituitary tumors among the young: a comparative study & meta-analysis. Clin. Neurol. Neurosurg. 200, 106411 (2021).
Dyer, E. H., Civit, T., Visot, A., Delalande, O. & Derome, P. Transsphenoidal surgery for pituitary adenomas in children. Neurosurgery 34, 207–212 (1994).
Saldarriaga, C. et al. Postoperative diabetes insipidus and hyponatremia in children after transsphenoidal surgery for adrenocorticotropin hormone and growth hormone secreting adenomas. J. Pediatr. 195, 169–174.e1 (2018).
Koumas, C. et al. Outcomes following endoscopic endonasal resection of sellar and supresellar lesions in pediatric patients. Childs Nerv. Syst. 35, 2099–2105 (2019).
Lamas, C., del Pozo, C. & Villabona, C., Neuroendocrinology Group of the SEEN. Clinical guidelines for management of diabetes insipidus and syndrome of inappropriate antidiuretic hormone secretion after pituitary surgery. Endocrinol. Nutr. 61, e15–e24 (2014).
de Vries, F. et al. Postoperative diabetes insipidus: how to define and grade this complication? Pituitary 24, 284–291 (2021).
Rajasekaran, S. et al. UK guidelines for the management of pituitary apoplexy. Clin. Endocrinol. 74, 9–20 (2011).
Ozcetin, M., Karaci, M., Toroslu, E. & Edebali, N. A pediatric case of pituitary macroadenoma presenting with pituitary apoplexy and cranial nerve involvement: case report. Turk. Pediatr. Ars 51, 162–165 (2016).
Villa, C. et al. Hyperplasia-adenoma sequence in pituitary tumorigenesis related to aryl hydrocarbon receptor interacting protein (AIP) gene mutation. Endocr. Relat. Cancer 18, 347–356 (2011).
Williams, F. et al. Clinical experience in the screening and management of a large kindred with familial isolated pituitary adenoma due to an aryl hydrocarbon receptor interacting protein (AIP) mutation. J. Clin. Endocrinol. Metab. 99, 1122–1131 (2014).
Chao, C. C. & Lin, C. J. Pituitary apoplexy in a teenager-case report. Pediatr. Neurol. 50, 648–651 (2014).
Culpin, E. et al. Pituitary tumour apoplexy within prolactinomas in children: a more aggressive condition? Pituitary 21, 474–479 (2018).
Deopujari, C. E., Shah, N. J., Shaikh, S. T., Karmarkar, V. S. & Mohanty, C. B. Endonasal endoscopic skullbase surgery in children. Childs Nerv. Syst. 35, 2091–2098 (2019).
Storr, H. L. et al. Endonasal endoscopic transsphenoidal pituitary surgery: early experience and outcome in paediatric Cushing’s disease. Clin. Endocrinol. 80, 270–276 (2014).
Deutschbein, T. et al. First German guideline on diagnostics and therapy of clinically non-functioning pituitary tumors. Exp. Clin. Endocrinol. Diabetes 129, 250–264 (2021).
Chivukula, S. et al. Endoscopic endonasal skull base surgery in the pediatric population. J. Neurosurg. Pediatr. 11, 227–241 (2013).
Massimi, L. et al. Quality of postoperative course in children: endoscopic endonasal surgery versus sublabial microsurgery. Acta Neurochir. 153, 843–849 (2011).
Kinoshita, Y. et al. Post-operative hyponatremia in patients with pituitary adenoma: post-operative management with a uniform treatment protocol. Endocr. J. 58, 373–379 (2011).
Grigsby, P. W., Thomas, P. R., Simpson, J. R. & Fineberg, B. B. Long-term results of radiotherapy in the treatment of pituitary adenomas in children and adolescents. Am. J. Clin. Oncol. 11, 607–611 (1988).
Partington, M. D., Davis, D. H., Laws, E. R. Jr. & Scheithauer, B. W. Pituitary adenomas in childhood and adolescence. Results of transsphenoidal surgery. J. Neurosurg. 80, 209–216 (1994).
De Menis, E. et al. Pituitary adenomas in childhood and adolescence. Clinical analysis of 10 cases. J. Endocrinol. Invest. 24, 92–97 (2001).
Mehrazin, M. Pituitary tumors in children: clinical analysis of 21 cases. Childs Nerv. Syst. 23, 391–398 (2007).
van den Bergh, A. C. et al. Immediate postoperative radiotherapy in residual nonfunctioning pituitary adenoma: beneficial effect on local control without additional negative impact on pituitary function and life expectancy. Int. J. Radiat. Oncol. Biol. Phys. 67, 863–869 (2007).
Chang, E. F. et al. Long-term recurrence and mortality after surgery and adjuvant radiotherapy for nonfunctional pituitary adenomas. J. Neurosurg. 108, 736–745 (2008).
Jennings, A. S., Liddle, G. W. & Orth, D. N. Results of treating childhood Cushing’s disease with pituitary irradiation. N. Engl. J. Med. 297, 957–962 (1977).
Yordanova, G. et al. Long-term outcomes of children treated for Cushing’s disease: a single center experience. Pituitary 19, 612–624 (2016).
Fraioli, M. F., Novegno, F., Catena, E., Fraioli, C. & Moschettoni, L. Multidisciplinary treatment of giant invasive prolactinomas in paediatric age: long-term follow-up in two children. Childs Nerv. Syst. 26, 1233–1237 (2010).
Shrivastava, A. et al. Outcomes after gamma knife stereotactic radiosurgery in pediatric patients with Cushing disease or acromegaly: a multi-institutional study. World Neurosurg. 125, e1104–e1113 (2019).
Pomeraniec, I. J., Dallapiazza, R. F., Xu, Z., Jane, J. A. Jr. & Sheehan, J. P. Early versus late Gamma Knife radiosurgery following transsphenoidal resection for nonfunctioning pituitary macroadenomas: a matched cohort study. J. Neurosurg. 125, 202–212 (2016).
Jalali, R. et al. Stereotactic conformal radiotherapy for pituitary adenomas: technique and preliminary experience. Clin. Endocrinol. 52, 695–702 (2000).
Colin, P. et al. Treatment of pituitary adenomas by fractionated stereotactic radiotherapy: a prospective study of 110 patients. Int. J. Radiat. Oncol. Biol. Phys. 62, 333–341 (2005).
Mackley, H. B. et al. Intensity-modulated radiotherapy for pituitary adenomas: the preliminary report of the Cleveland Clinic experience. Int. J. Radiat. Oncol. Biol. Phys. 67, 232–239 (2007).
Elhateer, H. et al. Fractionated stereotactic radiotherapy in the treatment of pituitary macroadenomas. Curr. Oncol. 15, 286–292 (2008).
Arauz, R. & Rodriguez, M. In: 19th Annual Scientific Meeting of the Society for Neuro-Oncology (Oxford Journals, 2015).
Almeldin, D. et al. Radiotherapy for Pituitary Tumors. ENDOTEXT. https://www.ncbi.nlm.nih.gov/pubmed/25905190 (2023).
Storr, H. L. et al. Clinical and endocrine responses to pituitary radiotherapy in pediatric Cushing’s disease: an effective second-line treatment. J. Clin. Endocrinol. Metab. 88, 34–37 (2003).
Ronson, B. B. et al. Fractionated proton beam irradiation of pituitary adenomas. Int. J. Radiat. Oncol. Biol. Phys. 64, 425–434 (2006).
Merchant, T. E. et al. Proton versus photon radiotherapy for common pediatric brain tumors: comparison of models of dose characteristics and their relationship to cognitive function. Pediatr. Blood Cancer 51, 110–117 (2008).
Combs, S. E. et al. Proton and carbon ion radiotherapy for primary brain tumors and tumors of the skull base. Acta Oncol. 52, 1504–1509 (2013).
Plowman, P. N. Pituitary adenoma radiotherapy-when, who and how? Clin. Endocrinol. 51, 265–271 (1999).
Loeffler, J. S. & Shih, H. A. Radiation therapy in the management of pituitary adenomas. J. Clin. Endocrinol. Metab. 96, 1992–2003 (2011).
Grabenbauer, G. G., Ernst-Stecken, A., Schneider, F., Lambrecht, U. & Ganslandt, O. Radiosurgery of functioning pituitary adenomas: comparison of different treatment techniques including dynamic and conformal arcs, shaped beams, and IMRT. Int. J. Radiat. Oncol. Biol. Phys. 66, S33–S39 (2006).
Sheehan, J. P. et al. Stereotactic radiosurgery for pituitary adenomas: an intermediate review of its safety, efficacy, and role in the neurosurgical treatment armamentarium. J. Neurosurg. 102, 678–691 (2005).
Sheehan, J. P. et al. Gamma Knife radiosurgery for the management of nonfunctioning pituitary adenomas: a multicenter study. J. Neurosurg. 119, 446–456 (2013).
Xu, Z., Lee Vance, M., Schlesinger, D. & Sheehan, J. P. Hypopituitarism after stereotactic radiosurgery for pituitary adenomas. Neurosurgery 72, 630–637 (2013).
Mitsumori, M. et al. Initial clinical results of LINAC-based stereotactic radiosurgery and stereotactic radiotherapy for pituitary adenomas. Int. J. Radiat. Oncol. Biol. Phys. 42, 573–580 (1998).
Brada, M. et al. Cerebrovascular mortality in patients with pituitary adenoma. Clin. Endocrinol. 57, 713–717 (2002).
Sattler, M. G. et al. The incidence of second tumours and mortality in pituitary adenoma patients treated with postoperative radiotherapy versus surgery alone. Radiother. Oncol. 104, 125–130 (2012).
Minniti, G. et al. The long-term efficacy of conventional radiotherapy in patients with GH-secreting pituitary adenomas. Clin. Endocrinol. 62, 210–216 (2005).
Burman, P., van Beek, A. P., Biller, B. M., Camacho-Hubner, C. & Mattsson, A. F. Radiotherapy, especially at young age, increases the risk for de novo brain tumors in patients treated for pituitary/sellar lesions. J. Clin. Endocrinol. Metab. 102, 1051–1058 (2017).
Swerdlow, A. J. et al. Risk of meningioma in European patients treated with growth hormone in childhood: results from the SAGhE cohort. J. Clin. Endocrinol. Metab. 104, 658–664 (2019).
Swerdlow, A. J. et al. Cancer risks in patients treated with growth hormone in childhood: the SAGhE European Cohort Study. J. Clin. Endocrinol. Metab. 102, 1661–1672 (2017).
Acknowledgements
The development of this consensus guideline was sponsored by unrestricted grants from professional societies (The Society of British Neurosurgical Surgeons, Children’s Cancer and Leukaemia Group (CCLG) and British Society for Paediatric Endocrinology and Diabetes), patient support groups (Association of Multiple Endocrine Neoplastic Disorders (AMEND), Success Charity and The Pituitary Foundation) and from Sandoz Pharmaceuticals. All, except Sandoz, were stakeholders. Sandoz supported administrative and travel expenses after the initial seed funding ended and had no role in instigating the endeavour, the development of guideline methodology or the final recommendations. The CCLG provided administrative support throughout the development of these consensus statements and the Royal College of Paediatrics and Child Health (RCPCH) provided advice and appraisal to ensure the process met rigorous AGREE II guideline standards. The CCLG, British Society for Paediatric Endocrinology and Diabetes, AMEND, Success Charity, Society of British Neurosurgical Surgeons or The Pituitary Foundation did not influence the decisions of the Guideline Development Group (GDG) or the recommendations other than through their roles as stakeholders, as described in the main text. We would like to thank all of the stakeholders who contributed comments to this consensus guideline at various stages of development, including members of the Society for Endocrinology, Society of British Neurological Surgeons, British Paediatric Neurosurgical Group, Royal College of Physicians, British Society for Paediatric Endocrinology and Diabetes, British Society of Paediatric Radiology, RCPCH, British Neuropathology Society, and the Association for Clinical Biochemistry and Laboratory Medicine as well as patient organizations AMEND, Success Charity and the Pituitary Foundation. The GDG would like to thank the Project Board members and Delphi panellists (Supplementary Table 2) and our external peer reviewers for their input into this consensus guideline. The GDG would also like to thank Rosa Nieto Hernandez (Clinical Guidelines Manager) and Helen McElroy (Quality Improvement Committee Clinical Lead for Evidence Base Medicine and Appraisals), both at the Research and Quality Improvement Directorate of the RCPCH, for their advice and appraisal of this consensus guideline at different stages. We also wish to thank Stephen Shalet (University of Manchester, UK), William Drake (Queen Mary University of London, London, UK), Mark Gurnell (University of Cambridge, Cambridge, UK), Luis Syro (Hospital Pablo Tobon Uribe and Clinica Medellin, Medellin, Colombia), Di Zou (Great Ormond Street Hospital for Children, London, UK), Lucas Castro (Queen Mary University of London, London, UK), Sarah Farndon (Great Ormond Street Hospital for Children, London, UK), Mary Dang (Queen Mary University of London, London, UK), Amy Ronaldson (Queen Mary University of London, London, UK), Rezvan Salehidoost (Queen Mary University of London, London, UK), Gabriela Mihai (Queen Mary University of London, London, UK) and Benjamin Loughrey (Queen’s University Belfast, Belfast, UK) for their help in updating the literature search, grading the papers from the literature search, reviewing the manuscript and providing administrative support.
Author information
Authors and Affiliations
Contributions
All authors researched data for the article. M.K., J.C.B., J.A., J.H.D., M.R.D., J.E., D.F., N.G., C.E.H., T.S.J., S.S., I.S., N.T., F.M.S., H.L.S. and H.A.S. contributed substantially to discussion of the content. M.K., J.C.B., A.B., J.H.D., J.E., T.S.J., S.S., I.S., N.T., H.L.S. and H.A.S. wrote the article. All authors reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
M.K. received grant funding or served on the Advisory Board for Pfizer, Crinetics, Novo Nordisk, Recordati, and ONO Pharmaceuticals and honoraria from Ipsen, Corcept, Sandoz and Novo Nordisk. J.C.B. has received honoraria, funding and travel bursaries from Novo Nordisk and honoraria from Sandoz and Ipsen. J.H.D. has received travel bursaries from Sandoz, Pfizer, and Novo Nordisk and grant funding from Pfizer. T.S.J. is director and shareholder in Repath Ltd. and Neuropath Ltd. and received an honorarium from Bayer. H.L.S. received grant funding from Ipsen and Sandoz and consultancy fees from Novo Nordisk, Pfizer and Springer. H.A.S. has received honoraria from Ferring and Pfizer and grants from Novo Nordisk and Sandoz. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Endocrinology thanks Bing Xing and the other, anonymous, reviewers for their contribution to the peer review of this work.
Additional information
Disclaimer Health-care providers need to use clinical judgment, knowledge and expertise when deciding whether it is appropriate to apply these guidelines. The recommendations cited here are a guide and might not be appropriate for use in all situations. The decision to adopt any of the recommendations cited here is the responsibility of the treating clinician and must be made in the light of individual patient circumstances, the wishes of the patient and their family, clinical expertise, and resources.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
AMEND: https://www.amend.org.uk/
Child Growth Foundation: https://childgrowthfoundation.org/
NICE terminology: https://www.nice.org.uk/process/pmg20/chapter/glossary#recommendations
Pituitary Foundation: https://www.pituitary.org.uk/
Pituitary Network Association: https://pituitary.org/
Rare endocrine tumour guidelines: https://www.cclg.org.uk/professionals/rare-endocrine-tumour-guidelines
Success Charity: https://successcharity.org.uk/
World Alliance of Pituitary Organizations: https://www.wapo.org/
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Korbonits, M., Blair, J.C., Boguslawska, A. et al. Consensus guideline for the diagnosis and management of pituitary adenomas in childhood and adolescence: Part 1, general recommendations. Nat Rev Endocrinol 20, 278–289 (2024). https://doi.org/10.1038/s41574-023-00948-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-023-00948-8
This article is cited by
-
Consensus guideline for the diagnosis and management of pituitary adenomas in childhood and adolescence: Part 2, specific diseases
Nature Reviews Endocrinology (2024)