Abstract
Endocrine-disrupting chemicals (EDCs) are exogenous chemicals that interfere with hormone action, thereby increasing the risk of adverse health outcomes, including cancer, reproductive impairment, cognitive deficits and obesity. A complex literature of mechanistic studies provides evidence on the hazards of EDC exposure, yet there is no widely accepted systematic method to integrate these data to help identify EDC hazards. Inspired by work to improve hazard identification of carcinogens using key characteristics (KCs), we have developed ten KCs of EDCs based on our knowledge of hormone actions and EDC effects. In this Expert Consensus Statement, we describe the logic by which these KCs are identified and the assays that could be used to assess several of these KCs. We reflect on how these ten KCs can be used to identify, organize and utilize mechanistic data when evaluating chemicals as EDCs, and we use diethylstilbestrol, bisphenol A and perchlorate as examples to illustrate this approach.
Similar content being viewed by others
Introduction
The endocrine system is composed of glands that secrete chemical messengers (hormones) that interact with specific targets (receptors). These interactions lead to the regulation of a vast set of functions, including growth, development, reproduction, energy balance, metabolism and body weight regulation1. Exogenous chemicals can inadvertently interfere with this complex communication system and cause adverse health effects. Throughout their lives, humans and other animals are exposed to a wide array of these so-called endocrine-disrupting chemicals (EDCs) through their encounters with work, consumer products, medications, natural resources, military service and other circumstances. This exposure can increase the risk of reproductive impairment2,3,4, cognitive deficits5,6,7, metabolic diseases and disorders8,9 and various cancers10,11,12,13, among others. The mechanisms by which hormones and EDCs exert specific actions are dependent on specific actions at the cellular and tissue levels as well as on circadian rhythms, seasonal changes, life stage and sex14. Moreover, the developmental, circadian or pulsatile pattern of hormone secretion can be an important component of their signalling mechanism and EDCs can interfere with this pattern15,16,17. Indeed, the risk of lifelong adverse health effects is enhanced when periods of EDC exposure coincide with the formation and differentiation of organ systems in early development18.
Although defining a chemical as an EDC is not a primary concern in all jurisdictions, an important key first step in governing exposures to chemicals with EDC properties is the identification of their intrinsic hazard. Regulatory agencies use various approaches to evaluate the available evidence, including for EDC identification19,20,21,22,23,24, but they can differ in the end points analysed and in their methods for gathering and interpreting the scientific evidence. Thus, standard, systematic approaches to organize and evaluate the often complex mechanistic data on a given chemical would reduce the likelihood of different jurisdictions arriving at different conclusions for hazard evaluations25,26.
Similar challenges were previously encountered in the evaluation of mechanistic data for cancer hazard identification. Therefore, the key characteristics (KCs) of human carcinogens were developed, providing a uniform basis for searching, organizing and evaluating mechanistic evidence to support the identification of carcinogens27. This KC-based approach is becoming widely applied by authoritative bodies, including the International Agency for Research on Cancer (IARC) and the National Toxicology Program, as according to the National Academies it “avoids a narrow focus on specific pathways and hypotheses and provides for a broad, holistic consideration of the mechanistic evidence”28. Indeed, the same National Academies report noted that KCs of other hazards, not just for carcinogens, should be developed28.
In this Expert Consensus Statement, we propose that chemicals that interfere with hormone action have identifiable KCs that relate to their ability to interact with key regulatory steps of hormone systems and that these KCs can be used to identify EDCs. Here, we identify the KCs that comprise the properties of all hormone systems. Ten KCs for EDCs are identified, representing the categories for the organization of the mechanistic evidence. Additionally, as with the KCs for carcinogens, the strength of the evidence is categorized for each KC during the hazard evaluation process28.
Methods
We assembled an international group of experts with knowledge of hormone systems, EDCs, hazard evaluations and risk assessments, in vitro and in vivo screening tools, and carcinogenesis, with the goal of advancing the KC framework. A list of KCs for EDCs was developed by panel discussions to achieve consensus during a 2-day workshop and biweekly teleconferences. We next selected three chemicals to illustrate how these KCs can be used to identify the hazard of endocrine disruption: bisphenol A (BPA), diethylstilbestrol (DES) and perchlorate (Box 1). M.T.S., M.A.L.M. and R.T.Z. conceived the project and L.Z. facilitated the meeting funding. M.T.S. organized and chaired the workshop. M.A.L.M. developed the original set of KCs that were subsequently modified by the whole group. M.A.L.M. and R.T.Z. led the group discussions and subsequent biweekly teleconferences. All authors contributed ideas to these discussions and wrote specific sections of the manuscript.
Key characteristics of EDCs
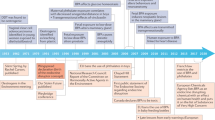
The KCs of EDCs were developed by recognizing that there are common features of hormone regulation and action that are independent of the diversity of the effects of hormones during the life cycle. It follows that there are also features that characterize the actions of chemicals that interfere with hormone regulation and action. Thus, the ten KCs identified (Fig. 1; Table 1) are based on our evaluation of the scientific literature, both in the field of endocrinology and in endocrine disruptor research, including high-quality reports documenting the effects of chemical exposures on hormone systems (for example, see refs29,30). Indeed, as no internationally harmonized ‘list’ of EDCs exists, we could not simply use the strategy of identifying ‘commonalities’ among EDCs in terms of their mechanisms. Moreover, such a list of commonalities among chemicals would be biased toward chemicals that are well studied, such as carcinogens and reproductive or thyroid toxicants, which represent the bulk of EDC research. Therefore, we capitalized on the extensive knowledge of hormone action to generate the ten KCs described in this Expert Consensus Statement. This list of KCs reflects current scientific knowledge and will probably evolve over time with new scientific discovery.
Arrows identify the ten specific key characteristics (KCs) of endocrine-disrupting chemicals (EDCs). The ± symbol indicates that an EDC can increase or decrease processes and effects. KC1 states that an EDC can interact with or activate hormone receptors. KC2 states that an EDC can antagonize hormone receptors. KC3 states that an EDC can alter hormone receptor expression. KC4 states that an EDC can alter signal transduction (including changes in protein or RNA expression, post-translational modifications and/or ion flux) in hormone-responsive cells. KC5 states that an EDC can induce epigenetic modifications in hormone-producing or hormone-responsive cells. KC6 states that an EDC can alter hormone synthesis. KC7 states that an EDC can alter hormone transport across cell membranes. KC8 states that an EDC can alter hormone distribution or circulating hormone levels. KC9 states that an EDC can alter hormone metabolism or clearance. KC10 states that an EDC can alter the fate of hormone-producing or hormone-responsive cells. Depicted EDC actions include amplification and attenuation of effects. Ac, acetyl group; Me, methyl group.
KC1: Interacts with or activates hormone receptors
All hormones act by binding to a specific receptor or receptors1. Inappropriate receptor activation can have profound negative effects on development and health, as illustrated by the formation of a scrotum and penis in genetic female humans exposed to androgens during gestation31. EDCs that inappropriately bind to and/or activate hormone receptors can produce adverse biological effects. There are numerous examples of chemicals that cause adverse effects after binding to nuclear hormone receptors. For example, EDCs that inappropriately activate the oestrogen receptors (ERα and ERβ) during development increase the risk of infertility in both sexes as well as reproductive tract cancer in women and prostate cancer in men32, in addition to other reproductive effects. Another example of an EDC that activates hormone receptors is that of dichlorodiphenyltrichloroethane (DDT; Box 1), which binds to ERα and ERβ33 and stimulates ER-dependent transcriptional activation and proliferation34 in a variety of species, including humans. Likewise, a specific hydroxylated congener of a polychlorinated biphenyl (PCB; Box 1) can activate human thyroid hormone receptor-β-mediated transcription1,35. EDCs can also activate cell membrane receptors of peptide and steroid hormones. For instance, DDT binds to the transmembrane domain of the follicle-stimulating hormone receptor, a G protein-coupled receptor (GPCR), to allosterically enhance its stimulation of cAMP production36.
KC2: Antagonizes hormone receptors
EDCs can inhibit or block effects of endogenous hormones by acting as receptor antagonists30. Although antagonism of membrane hormone receptors or intracellular hormone receptors can occur (as exemplified by drug discovery efforts37,38,39), most exogenous chemical research into antagonization of receptors has focused on antagonization of nuclear hormone receptors. Nuclear receptors that act as ligand-dependent transcription factors by mediating genomic regulatory responses can be antagonized by some EDCs. For example, dichlorodiphenyldichloroethylene, an organochlorine pesticide (Box 1), inhibits androgen binding to the androgen receptor (AR) and inhibits androgen-dependent transactivation of the AR in human40 and rat prostrate cells41. Other organochlorine pesticides (such as lindane and dieldrin, which is closely related to the organochlorine insecticide aldrin) also inhibit dihydrotestosterone binding to the AR. As androgens are key regulators of male sexual differentiation during fetal development, disruption of androgen action through AR antagonism in this period can permanently demasculinize male fetuses and lead to malformations of the genital tract42,43.
KC3: Alters hormone receptor expression
As hormone receptors mediate hormone actions1, their physiotemporal pattern of expression dictates their response to hormone signals44,45. For example, receptor abundance can determine both the concentration of hormones that produces an effect as well as the magnitude of the effect itself in some situations46. EDCs can modulate hormone receptor expression, internalization and degradation. For example, di(2‐ethylhexyl) phthalate decreases the expression of the mineralocorticoid (aldosteron) receptor (MR) in the testis of adult mice47, where under normal conditions, MR acts as a positive modulator of testosterone biosynthesis48. Further, BPA (Box 1) alters the expression of oestrogen, oxytocin and vasopressin receptors in brain nuclei49,50,51,52,53, and also reduces the proteasome-mediated degradation of ERβ54. The internalization of cell surface receptors is also disrupted by chemicals. For example, DDT prevents the internalization of the TSH receptor55.
KC4: Alters signal transduction in hormone-responsive cells
The binding of a hormone to a receptor triggers specific intracellular responses that are dependent on the receptor and tissue-specific properties of the target cell. Signal transduction mediated through both membrane and intracellular hormone receptors is altered by some EDCs. The signalling of two classes of receptors will be discussed here as they are the most extensively studied in the field of endocrinology and have EDC effects; these receptors are cell surface membrane receptors (such as GPCRs, receptor kinases, and kinase-linked and ionotropic receptors) and nuclear steroid hormone receptors.
Ionotropic receptor signalling can be perturbed by EDCs. For example, BPA blocks low glucose-induced calcium signalling in isolated pancreatic glucagon-secreting α-cells from adult male mice56. Furthermore, in 2018 it was shown that chemicals in ultraviolet filters disrupt calcium signalling in human sperm57,58.
Some membrane GPCRs bind steroids; among these, G protein-coupled oestrogen receptor (GPER; previously called GPR30) signalling is the best studied regarding the EDC effects (for example, BPA59). Further, EDCs can attenuate or potentiate hormone action through signal transduction. For instance, in in vitro studies, the fungicide tolylfluanid impairs insulin action by reducing insulin receptor substrate 1 (ref.60), while methoxyacetic acid (Box 1) potentiates ligand-activated transcription and progesterone receptor-mediated transcription in a manner dependent on MEK1 and MEK2 activity61.
EDCs also affect signal transduction initiated by nuclear receptors. These effects include their interactions with coregulatory factors such as activators and repressors, which are a key part of the molecular machinery determining the downstream response to nuclear hormone receptor activation. The coregulatory factors for the steroid receptor coactivator (SRC) family are among the most studied in exogenous chemical research. For example, xenoestrogens (such as DES, PCBs, octylphenol and BPA; Box 1) induce the recruitment of SRC1 by ERα and ERβ in a dose-dependent manner62. BPA and its analogues also recruit SRC1 to thyroid hormone receptor-β63. Substantial evidence suggests that xenoestrogens, especially BPA, increase SRC1 expression, as shown in the rat hypothalamus64,65 and in human breast cancer cell lines66. Another EDC, 4-methylbenzylidene camphor (which is used in ultraviolet filters), also increases SRC1 expression in female rat hypothalamus67.
KC5: Induces epigenetic modifications in hormone-producing or hormone-responsive cells
Hormones can exert permanent effects — especially during development and differentiation — by modifying epigenetic processes, including DNA and histone modifications and non-coding RNA expression. An EDC that interferes with hormone action can do so by interfering with the ability of a hormone to induce these epigenetic changes or by inducing these epigenetic changes to interfere with hormone action (such as by altering the expression or action of a hormone receptor or the transcription of hormone-responsive genes68,69). For example, the pesticide methoxychlor increases the expression of the DNA methyltransferase DNMT3B to hypermethylate DNA, including ESR2 (which encodes ERβ) in the ovary of developmentally exposed rats70. In addition, di(2-ethylhexyl) phthalate inappropriately demethylates MR DNA in the testis of male mice47. EDCs can also change the expression of non-coding RNAs, as is seen with PCBs altering the developmental trajectories of hypothalamic microRNA expression in a sexually dimorphic manner71 as well as BPA and phthalates affecting microRNA expression in placental, Sertoli and breast cancer cell lines72.
Further to these data, a study on long non-coding RNAs found that oestradiol, BPA and DES induced HOX antisense intergenic RNA (termed HOTAIR) in human breast cancer cells73. In the presence of BPA and DES, the ER-binding region of the HOTAIR promoter was enriched by trimethylation on lysine 4 of histone 3 (H3K4) and by H3K4-specific methyltransferases, which are known to activate transcription73 (Table 2). Moreover, developmental BPA exposure enhances H3K4 trimethylation on genes, which are subsequently more sensitive to regulation by testosterone68. Oestradiol and DES also reduce trimethylation of lysine 27 on histone H3 in the developing uterus of rats74.
KC6: Alters hormone synthesis
Hormone synthesis is regulated by both intracellular and distant endocrine feedback mechanisms. For example, thyroid hormone synthesis is controlled by a combination of TSH activation of their receptors on thyrotrophs as well as intracellular cAMP, iodine uptake and the activation of various enzymes16. After transcription and translation, proteins and peptide hormones are packaged into secretory vesicles where they can be stored75. By contrast, steroid hormone synthesis, including the transformation of a pro-hormone to a hormone, occurs more or less simultaneously with hormone activity1. Some EDCs are known to interfere with hormone synthesis. For example, perchlorate can block the uptake of iodine into thyroid cells, thereby inhibiting thyroid hormone synthesis76 (Box 1; Table 2) and phthalates can reduce testosterone synthesis in the fetal rat testis, resulting in testosterone insufficiency77,78.
By contrast, the herbicide atrazine apparently increases oestrogen synthesis in peripubertal male mice, as evidenced by a decrease in serum levels of testosterone coupled to an increase in circulating levels of oestrogen and in the activity of the aromatase that synthesizes oestrogen from testosterone79. Additionally, several neonicotinoid pesticides block the JAK–STAT3 pathway to enhance the promoter usage and expression of CYP19 (aromatase), the gene that encodes the enzyme that converts testosterone to oestrogen80.
KC7: Alters hormone transport across cell membranes
Due to their lipophilicity, steroid hormones (including oestrogens, androgens, progestins and adrenal steroids) can move through membranes passively. Other hormones (such as amine, peptide, protein and thyroid hormones) must be selectively transported across membranes either to gain entrance to and/or to exit the cell81. These selective and passive transport processes can be disrupted by EDCs. One well-delineated example of impaired selective transport by an exogenous chemical is low dose BPA, which reduces calcium entry into mouse pancreatic β-cells to reduce insulin secretion from vesicles82 (Table 2). Additionally, the anti-corrosive and fungicidal chemical imidazoline modulates ions to enhance insulin secretion83, and the passive secretion of corticosterone from rodent adrenal glands is reduced by low-dose dichlorodiphenyldichloroethylene84.
KC8: Alters hormone distribution or circulating levels of hormones
Hormones typically circulate throughout the body in the blood at low concentrations, often in the parts per billion and trillion range85. Depending on its chemistry, a circulating hormone is either transported ‘free’ (not bound to serum protein) with or without conjugation (such as glucuronidation or sulfation) or is circulated bound to various proteins. EDCs can alter hormone bioavailability by interfering with the distribution of hormones in hormone-responsive tissues or with the circulation of hormones, including by displacing hormones from their serum binding proteins, which can lead to impaired active hormone delivery to target tissues. For example, BPA causes a concentration-dependent decrease in circulating levels of testosterone in male rats and men, and the pesticide malathion reduces testosterone levels in serum, testis and ovaries in several animals experimentally30,86,87. When DES is administered to men intravenously, reductions in total (a sixfold reduction) and free (a 20% reduction) testosterone and oestrogen (a fivefold reduction) are concurrent with an over sevenfold increase in serum concentration of sex hormone-binding globulin (SHBG)88 (Table 2).
KC9: Alters hormone metabolism or clearance
The various hormone types (such as protein, peptide, steroid or thyroid) are inactivated differently. For example, after secretion, protein hormones (for example, gonadotropins) are inactivated when they are broken down by proteases in the blood. By contrast, steroid and thyroid hormones are metabolized by enzymes that render them hormonally inactive and increase their water solubility so that they can be removed from the bloodstream and excreted1.
EDCs can alter the rates of inactivation, including the metabolic degradation or clearance, of hormones, which could alter hormone concentrations and ultimately their activity. For example, a large number of chemicals activate glucuronidases, which increase thyroid hormone clearance from the blood89. Furthermore, sulfation by oestrogen sulfotransferase, which reduces the rate of oestrogen clearance from the blood, is inhibited by several coplanar hydroxylated PCB metabolites, a major metabolite of the fungicide hexachlorobenzene and several chlorophenolic wood preservatives90.
KC10: Alters the fate of hormone-producing or hormone-responsive cells
Hormones affect tissue structure and organization by affecting cell fate (for example, cellular proliferation, migration or differentiation) and/or death (that is, apoptosis or necrosis) during development and adulthood91,92,93. In adulthood, many healthy endocrine organs have a fairly stable number of cells (including adrenals and pancreas), whereas other endocrine organs or hormone-responsive tissues depend on cell growth for normal function (such as the testicles to form sperm, the uterine endometrium and vaginal lining). EDCs can alter the total number or positioning of cells in hormone-producing or hormone-responsive tissues by disrupting or promoting differentiation, proliferation, migration or cell death. For example, thyroid hormone controls cell proliferation and apoptosis in the developing cerebellum and PCBs can interfere with thyroid hormone signalling to cause abnormal morphology later in life94. Female mice exposed to oxybenzone, a chemical ultraviolet filter found in personal care products, during pregnancy and lactation have increased mammary epithelial cell proliferation, which is observed even weeks after exposures cease95. In cultured human endometrial stromal cells, treatment with the antibacterial agent triclosan increases decidualization96. In the brain (anteroventral periventricular nucleus of the hypothalamus), developmental exposure to a PCB mixture substantially decreases the numbers of cells expressing ERα in adult female but not male rats97. Further, tebuconazole, a common fungicide, impairs placental migration, a process essential to placentation98.
Application of the ten KCs
In the following sections we illustrate how the KCs can be used to organize and integrate mechanistic data with data on adverse endocrine effects in humans and in experimental models in an analysis designed to identify an EDC hazard. Sources of exposure, which could be considered to identify risk, are found in Box 1. Note that, for two of these examples, DES and BPA, substantial evidence exists for almost all the KCs yet for perchlorate strong evidence is available for only one KC (Table 2). Thus, the number of KCs associated with a specific exposure is not predictive of the EDC hazard as much as the relationship of the KC to hormone action.
Example EDC: DES
In the human phenotype (of note, ‘human phenotype’ describes the clinical outcomes and epidemiology that characterize the adverse endocrine effects), women who were exposed in utero exhibit a higher incidence of breast cancer and clear cell carcinoma of the vagina99, in parallel to studies in mice (see below). Prenatal exposure to DES also is associated with disruption of the growth of hormone-sensitive structures in these daughters, with changes such as cellular abnormalities of the vaginal lining, increased breast size and abnormally shaped uteri in adolescents and young women100,101. Boys who were exposed to DES in utero are also prone to genital birth defects such as hypospadias and cryptorchidism102. Emerging evidence suggests that the effects of DES persist into the next (F2) generation; for example, the grandsons of women who took DES during pregnancy are at increased risk of genital defects103.
In the animal phenotype (of note, ‘animal phenotype’ describes the pathology and physiology observed in experimental animal models), DES was first identified as an oestrogen following the discovery that it induces keratinization of the vaginal epithelium — an oestrogenic effect — in mice104,105. In utero exposure to DES induces uterine deformities, reproductive tract cancer and abnormal mammary gland morphology in female rodents, while neonatal exposure leads to penile deformity and low sperm counts in male rodents106. DES increases body weight in livestock and subclinical doses induce obesity in rodents107. Multigenerational effects of DES have been documented in experimental animal studies, including vaginal adenocarcinomas observed in the granddaughters of mice that were exposed in adulthood108.
Mechanistic data (of note, the KCs are revealed in ‘mechanistic data’ from human and model cells, model organisms and through the use of biomarkers) show that DES exhibits nine of the ten KCs of an EDC and is noteworthy for the abundance of mechanistic data in humans (Table 2). DES is an agonist of nuclear and membrane ER56,109, including to SRC1 (ref.62) recruitment and epigenetic modifications73,74 that activate ER-responsive transcription. For example, DES induces gene expression of several oestrogen-responsive HOXA genes necessary for differentiation of human female reproductive tract cells, which is probably responsible for the metaplastic effects of DES110,111. Further, DES exposure alters circulating concentrations of hormone and SHBG in humans. When DES is administered to men intravenously, total and free levels of testosterone and oestrogen are reduced (a sixfold reduction, 20% reduction and fivefold reduction, respectively) concurrently with an over sevenfold increase in levels of SHBG88,108,112. The KCs of DES identified among mechanistic studies, along with the evidence from human and other animal studies, indicate that effects of DES on the reproductive axes of female and male humans and rodents are mediated by numerous DES KCs that perturb oestrogen action.
Example EDC: BPA
In the human phenotype, there are now >100 epidemiology studies that show associations between BPA and adverse outcomes such as obesity, diabetes mellitus, female infertility, male sexual dysfunction, reduced birth weight and atypical neurobehaviours in children, among others113. Although many of these studies are cross-sectional, others are longitudinal, providing stronger evidence for causal relationships between exposures and effects.
In the animal phenotype, hundreds of studies demonstrate that, in rodents, even low doses of BPA can disrupt development of the brain, male and female reproductive tracts, and mammary gland and metabolic tissues under endocrine control, among others114. BPA can also induce precancerous and cancerous lesions of the mammary gland and prostate115.
Mechanistic data show that thousands of mechanistic scientific papers on BPA have been published that provide substantial evidence for nine of the ten KCs described above (Table 2). Experimental studies have shed light on the molecular mechanisms that explain the actions of BPA on human and animal phenotypes. These studies have revealed that BPA binds to ERα and ERβ, as well as GPER, membrane ER, thyroid hormone receptor and AR116. BPA then causes the enrichment of H3K4 trimethylation and H3K4-specific methyltransferases at the ER-binding region of the HOTAIR promoter, and these enrichments are known to activate transcription in oestrogen-responsive cells73. The activation of ER by BPA has multiple effects on organs in various species, for example, BPA activates ERβ-mediated ion flux, which underlies the reduction in insulin secretion from pancreatic β-cells in response to BPA treatment82. The aforementioned KCs of BPA are consistent with the known mechanisms that underlie the diverse adverse effects that have been associated with BPA exposure in humans and other animals.
Example EDC: perchlorate
In the human phenotype, measures of urinary perchlorate — a biomarker of perchlorate exposure — in pregnant women are linked to reduced maternal levels of thyroid hormone in several, but not all, studies117,118,119,120. However, because newborn babies are uniquely sensitive to suppression of thyroid hormone synthesis121, the relationship between perchlorate exposure and circulating levels of thyroid hormones should be evaluated in this population. Among the five studies in which thyroid hormone levels were measured within a day of birth, there is consistent evidence that newborn babies from communities that have been exposed to perchlorate have lower T4 levels and higher TSH levels and thyroid disease than those from unexposed communities122. The sufficiency of dietary iodine intake in a population is also likely to be a contributing factor to the variability in epidemiological associations between circulating perchlorate levels and thyroid hormone levels.
In the animal phenotype, low doses of perchlorate reduces serum levels of T4 in pregnant rats and their pups123 and impairs synaptic function in the adult hippocampus124. This finding supports the negative association between perchlorate and levels of T4 in the human epidemiological studies described in the previous section.
Mechanistic data show that perchlorate has strong evidence for only one KC; yet, it is a critical KC as it provides biological plausibility to the human and animal findings. Perchlorate inhibits thyroid hormone synthesis (KC6; Table 2) by acting as a potent competitive inhibitor of iodide uptake through the sodium–iodide symporter from humans, rodents and other vertebrates76,125. This symporter protein normally transports iodide across cell membranes in the thyroid gland, gut lining, placenta, the lactating breast and the choroid plexus126. Collectively, the aforementioned research on perchlorate suggests that perchlorate reduces thyroid hormone levels in humans and other animals by limiting the amount of iodide available for the synthesis of these hormones.
Application of the ten KCs to identify EDCs
The KCs of carcinogens have been successfully applied by the IARC Monographs Programme to evaluate the mechanistic data for >30 suspected carcinogens127. Within the context of IARC, carcinogens are identified by four separate data streams: human exposure, tumours in humans, tumours in animals and mechanistic. The mechanistic data identified through the KCs of carcinogens support the interpretation of these other data streams by freeing the reviewers from linking specific mechanisms to specific tumours, which is a nearly impossible task. Similarly, we envision that the KCs of EDCs will provide a structure for searching and organizing the relevant literature on mechanistic information in support of an evaluation of a chemical for endocrine disruption (Box 2). These KCs are not a checklist; any specific application of the KC approach to identifying EDCs will depend on the extent of evidence on the chemical as well as on the goals of the end-user (Box 3).
Depending on the end-users’ chosen parameters, such as the definition of the EDC used, the types and availability of data that can inform the evidence stream, and/or budget, end-users might wish to compress several KCs into a larger category or omit certain KCs in their EDC definition. It is critical in all circumstances to recognize that identifying an EDC is not merely counting the sum of KCs with supporting evidence. Hormones generally act through entire systems, and one KC might be sufficient to disrupt an entire system. Strong evidence for one KC could be enough to support identification of an EDC, as is illustrated by perchlorate, which only has one KC yet its endocrine-disrupting activity is strongly supported by human and experimental evidence. Hence, incorporation of mechanistic data into EDC hazard identification should not be thought of in terms of a minimum number of KC ‘hits’, but rather in terms of whether the chemical interferes with a key event in hormone action consistent with causing an adverse effect.
Assays to evaluate KCs
Some mechanistic assays have been developed to screen potential EDCs in a regulatory context, though these are limited to measuring chemicals that interact with sex steroid nuclear receptors or alter the synthesis of sex steroids (such as KCs 1, 2 and 6; Table 1). High-throughput mechanistic assays, on the other hand, are abundantly available in the suite of ToxCast128 and Tox21 (ref.129) assays, which screen thousands of chemicals for a variety of toxicity pathways, including endocrine disruption. These high-throughput assays have not undergone international validation, and therefore regulatory authorities use the resulting data only in certain contexts. For example, results of a ToxCast ER model that integrates data from 18 in vitro assays130,131 are accepted by the US Environmental Protection Agency in lieu of the rodent in vivo uterotrophic assays to screen for the oestrogenic effect of chemicals. In addition, high-throughput mechanistic data can be part of the data used to satisfy the European regulatory criteria of an endocrine disruptor19.
Despite the hundreds of toxicity end points in these high-throughput platforms, assays that assess several KCs of EDCs are not well represented or are absent. This absence of data presents an opportunity to use the KCs of EDCs to identify assay development needs. In addition to the high-throughput platforms used by federal agencies to screen for activity, the published in vitro, in vivo and chemoinformatics literature can inform the evaluation of EDC properties. Indeed, the KCs of EDCs can be used to identify search terms for the transparent acquisition of the extensive research emanating from academic and government research laboratories to contribute to the identification of EDCs (Box 2).
Effect on risk assessment
Over the past several decades, innovative methods for identifying chemical interactions with a molecular target, such as a hormone receptor or enzyme, have become increasingly available. These interactions might initiate a sequence of downstream biological effects that lead to adverse outcomes, yet molecular effects and adverse responses are not usually evaluated in the same test. Establishing causal linkages between these molecular events and adverse outcomes therefore requires an organizational framework to evaluate biologically plausible connections between responses at different levels and from different methods. Mode of action analyses were developed in an attempt to link key events in a theoretical biological sequence (such as carcinogenicity and endocrine effects)132,133. Adverse outcome pathways are an expansion of mode of action concepts that include a molecular initiating event and an adverse outcome in an organism, which are linked by all key events measured at various levels of organization134. Both mode of action and adverse outcome pathways are linear, reductive models of complex physiology but might nonetheless be helpful for understanding how chemicals exert their toxic effects135.
A challenge to the practical application of mode of action and adverse outcome pathway approaches for chemical safety decision-making is the limitation in the current understanding of disease processes, which could be shown to be incorrect or incomplete136. This limitation was recognized by Sir Bradford Hill, who formalized the research of causality in humans while noting that “what is biologically plausible depends upon the biological knowledge of the day”137.
The KCs approach we describe herein can be viewed as identifying molecular initiating events or early key events in both mode of action and adverse outcome pathway frameworks based on our current knowledge of the molecular mechanisms of hormone action as well as the role of hormones in development, health and disease. Using KCs to assemble mechanistic data about a putative EDC does not require an exhaustive understanding of how the characteristics are causally linked to the endocrine response or an a priori hypothesis about the mode of action or adverse outcome pathways. Instead, the KCs are based on the common properties of hormone systems during vertebrate developmental and adult life stages. In this manner, the KC approach avoids “a narrow focus on specific pathways and hypotheses” and instead “provides for a broad, holistic consideration of the mechanistic evidence”28.
Conclusions
The KCs of EDCs are the functional properties of agents that alter hormone action. This emphasis is both unique and powerful in that these KCs comprise the major mechanisms by which hormone systems can be disrupted, including by interfering with what they do, how they do it and how they are controlled. The literature on the fundamental and clinical actions of hormones is extremely large and the KCs, as we have proposed them, open the process of EDC hazard identification to this literature. An essential element of the KC approach is that it superimposes on the fundamental endocrine framework the mechanisms by which chemicals can interfere with these systems. The KC approach is also adaptable in that users can collapse KCs (such as combine KC1 and KC2) if their given situation is advanced by this. The ten KCs described herein can also be mapped to current and future assays used to identify EDCs.
The KCs are agnostic with respect to current or future knowledge of downstream health hazards and mechanistic pathways. As we learn more about chemical actions on endocrine systems, the KCs should be updated to reflect this new information. The value of this approach for EDCs, as for carcinogens, is that the inevitable mechanistic gaps in the delineation of the complete pathway from exposure to downstream health hazards need not hamper the identification of key chemical characteristics that lead to phenotypic end points. Even for the case of BPA, which has been more intensely studied than perhaps any other EDC138, there are gaps in our understanding of the complete molecular pathways by which BPA produces observed health effects. Indeed, the same can be said for well-known exposure–disease relationships such as cancers induced by tobacco smoking and developmental neurotoxicity from lead exposure. In the absence of ‘complete’ knowledge, the recommended KCs of EDCs approach can systematically identify gaps in data and therefore set research priorities through the process of hazard identification. The utility of this approach is evidenced by the 2018 paper demonstrating the effect of KCs in carcinogen hazard identification127.
We recommend that efforts to identify and classify a chemical as an EDC utilize our KCs of EDCs approach in conjunction with other data (including epidemiological and experimental animal data) as we exemplified in the section ‘Application of the ten KCs’. Similar to the KCs of carcinogens, the KCs of EDCs can distil complex EDC mechanistic research from human and animal studies into a transparent approach.
As highlighted by the demonstration that three different well-known EDCs exhibit different characteristics of interference with endocrine systems supporting 1–9 KCs, we emphasize that the KCs should not be used as a checklist. We identify applications for the KCs, including their use by agencies that have been charged with risk evaluation and EDC classification (Box 3). Future directions for the KCs of EDCs should include the development of a controlled ontology of search terms to facilitate their widespread application.
In conclusion, the KCs of EDCs approach provides a universal framework for organizing mechanistic evidence for hazard identification that can be the foundation for the implementation of EDC risk assessments worldwide. This approach is a highly novel advancement in the EDC field.
References
Jameson, J. L. Endocrinology: Adult & Pediatric 7th edn (Elsevier Saunders, 2016).
Axelstad, M. et al. EDC IMPACT: reduced sperm counts in rats exposed to human relevant mixtures of endocrine disrupters. Endocr. Connect. 7, 139–148 (2018).
Johansson, H. K. L., Svingen, T., Fowler, P. A., Vinggaard, A. M. & Boberg, J. Environmental influences on ovarian dysgenesis — developmental windows sensitive to chemical exposures. Nat. Rev. Endocrinol. 13, 400–414 (2017).
Skakkebaek, N. E. A brief review of the link between environment and male reproductive health: lessons from studies of testicular germ cell cancer. Horm. Res. Paediatr. 86, 240–246 (2016).
Amano, I. et al. Effects of mild perinatal hypothyroidism on cognitive function of adult male offspring. Endocrinology 159, 1910–1921 (2018).
Ghassabian, A. & Trasande, L. Disruption in thyroid signaling pathway: a mechanism for the effect of endocrine-disrupting chemicals on child neurodevelopment. Front. Endocrinol. 9, 204 (2018).
Jefferson, W. N. et al. Widespread enhancer activation via ERα mediates estrogen response in vivo during uterine development. Nucleic Acids Res. 46, 5487–5503 (2018).
Alonso-Magdalena, P. et al. Bisphenol A exposure during pregnancy disrupts glucose homeostasis in mothers and adult male offspring. Environ. Health Perspect. 118, 1243–1250 (2010).
Cano-Sancho, G., Salmon, A. G. & La Merrill, M. A. Association between exposure to p,p’-DDT and its metabolite p,p’-DDE with obesity: integrated systematic review and meta-analysis. Environ. Health Perspect. 125, 096002 (2017).
Heindel, J. J., Skalla, L. A., Joubert, B. R., Dilworth, C. H. & Gray, K. A. Review of developmental origins of health and disease publications in environmental epidemiology. Reprod. Toxicol. 68, 34–48 (2017).
Sifakis, S., Androutsopoulos, V. P., Tsatsakis, A. M. & Spandidos, D. A. Human exposure to endocrine disrupting chemicals: effects on the male and female reproductive systems. Environ. Toxicol. Pharmacol. 51, 56–70 (2017).
Giulivo, M., Lopez de Alda, M., Capri, E. & Barceló, D. Human exposure to endocrine disrupting compounds: their role in reproductive systems, metabolic syndrome and breast cancer. A review. Environ. Res. 151, 251–264 (2016).
Scsukova, S., Rollerova, E. & Bujnakova Mlynarcikova, A. Impact of endocrine disrupting chemicals on onset and development of female reproductive disorders and hormone-related cancer. Reprod. Biol. 16, 243–254 (2016).
Zoeller, R. T. et al. Endocrine-disrupting chemicals and public health protection: a statement of principles from The Endocrine Society. Endocrinology 153, 4097–4110 (2012).
Kopp, R., Martinez, I. O., Legradi, J. & Legler, J. Exposure to endocrine disrupting chemicals perturbs lipid metabolism and circadian rhythms. J. Environ. Sci. 62, 133–137 (2017).
Zoeller, R. T., Tan, S. W. & Tyl, R. W. General background on the hypothalamic-pituitary-thyroid (HPT) axis. Crit. Rev. Toxicol. 37, 11–53 (2007).
Mimoto, M. S., Nadal, A. & Sargis, R. M. Polluted pathways: mechanisms of metabolic disruption by endocrine disrupting chemicals. Curr. Environ. Health Rep. 4, 208–222 (2017).
WHO & UNEP. State of the Science of Endocrine Disrupting Chemicals — 2012 (World Health Organization, 2013).
Andersson, N. et al. Guidance for the identification of endocrine disruptors in the context of Regulations (EU) No 528/2012 and (EC) No 1107/2009. EFSA J. 16, e05311 (2018).
US Environmental Protection Agency. Framework for human health risk assessment to inform decision making. US EPA https://www.epa.gov/risk/framework-human-health-risk-assessment-inform-decision-making (2014).
Office of Environmental Health Hazard Assessment. Green chemistry hazard traits, section 69403.4 endocrine toxicity, California Code of Regulations, Division 4.5, Title 22, Chapter 54. OEHHA https://oehha.ca.gov/media/downloads/risk-assessment/gcisor121710.pdf (2011).
International Programme on Chemical Safety. Global Assessment of the State of the Science of Endocrine Disruptors, An Assessment Prepared by an Expert Group on Behalf of the World Health Organization, the International Labour Organization, and the United Nations Environment Programme, WHO/PCS/EDC/02.2 (World Health Organization, 2002).
Japan Ministry of Health. The Endocrine Disruptor Page. NIHS http://www.nihs.go.jp/edc/english/actions/index.htm (2015).
OECD. Revised guidance document 150 on standardised test guidelines for evaluating chemicals for endocrine disruption. OECD Series on Testing and Assessment https://doi.org/10.1787/9789264304741-en (2018).
Ruden, C. What influences a health risk assessment? Toxicol. Lett. 167, 201–204 (2006).
Ruden, C. Principles and practices of health risk assessment under current EU regulations. Regul. Toxicol. Pharmacol. 44, 14–23 (2006).
Smith, M. T. et al. Key characteristics of carcinogens as a basis for organizing data on mechanisms of carcinogenesis. Environ. Health Perspect. 124, 713 (2016).
The National Academies of Sciences, Engineering, and Medicine. Using 21st Century Science to Improve Risk-Related Evaluations (The National Academies Press, 2017).
Diamanti-Kandarakis, E. et al. Endocrine-disrupting chemicals: an endocrine society scientific statement. Endocr. Rev. 30, 293–342 (2009).
Gore, A. C. et al. EDC-2: The Endocrine Society’s second scientific statement on endocrine-disrupting chemicals. Endocr. Rev. 36, E1–E150 (2015).
Wadzinski, T. L., Altowaireb, Y., Gupta, R., Conroy, R. & Shoukri, K. Luteoma of pregnancy associated with nearly complete virilization of genetically female twins. Endocr. Pract. 20, e18–e23 (2014).
Lee, H. R. et al. Molecular mechanism(s) of endocrine-disrupting chemicals and their potent oestrogenicity in diverse cells and tissues that express oestrogen receptors. J. Cell. Mol. Med. 17, 1–11 (2013).
Legler, J. et al. Comparison of in vivo and in vitro reporter gene assays for short-term screening of estrogenic activity. Environ. Sci. Technol. 36, 4410–4415 (2002).
Dees, C. et al. Estrogenic and DNA-damaging activity of Red No. 3 in human breast cancer cells. Environ. Health Perspect. 105, 625 (1997).
You, S. H., Gauger, K. J., Bansal, R. & Zoeller, R. T. 4-Hydroxy-PCB106 acts as a direct thyroid hormone receptor agonist in rat GH3 cells. Mol. Cell. Endocrinol. 257-258, 26–34 (2006).
Munier, M. et al. In vitro effects of the endocrine disruptor p,p’-DDT on human follitropin receptor. Environ. Health Perspect. 124, 991–999 (2016).
Yangthara, B., Mills, A., Chatsudthipong, V., Tradtrantip, L. & Verkman, A. S. Small-molecule vasopressin-2 receptor antagonist identified by a G-protein coupled receptor “pathway” screen. Mol. Pharmacol. 72, 86–94 (2007).
Yu, H. N. et al. Discovery of substituted benzamides as follicle stimulating hormone receptor allosteric modulators. Bioorg. Med. Chem. Lett. 24, 2168–2172 (2014).
Wacker, D., Stevens, R. C. & Roth, B. L. How ligands illuminate GPCR molecular pharmacology. Cell 170, 414–427 (2017).
Schrader, T. J. & Cooke, G. M. Examination of selected food additives and organochlorine food contaminants for androgenic activity in vitro. Toxicol. Sci. 53, 278–288 (2000).
Kelce, W. R. et al. Persistent DDT metabolite p,p’-DDE is a potent androgen receptor antagonist. Nature 375, 581–585 (1995).
Gray, L. E. Jr., Ostby, J., Monosson, E. & Kelce, W. R. Environmental antiandrogens: low doses of the fungicide vinclozolin alter sexual differentiation of the male rat. Toxicol. Ind. Health 15, 48–64 (1999).
Gray, L. E. et al. Effects of environmental antiandrogens on reproductive development in experimental animals. Hum. Reprod. Update 7, 248–264 (2001).
Grimm, S. L. et al. Disruption of steroid and prolactin receptor patterning in the mammary gland correlates with a block in lobuloalveolar development. Mol. Endocrinol. 16, 2675–2691 (2002).
Mongan, N. P., Tadokoro-Cuccaro, R., Bunch, T. & Hughes, I. A. Androgen insensitivity syndrome. Best Pract. Res. Clin. Endocrinol. Metab. 29, 569–580 (2015).
Charlton, S. J. Agonist efficacy and receptor desensitization: from partial truths to a fuller picture. Br. J. Pharmacol. 158, 165–168 (2009).
Martinez-Arguelles, D. B., Culty, M., Zirkin, B. R. & Papadopoulos, V. In utero exposure to di-(2-ethylhexyl) phthalate decreases mineralocorticoid receptor expression in the adult testis. Endocrinology 150, 5575–5585 (2009).
Ge, R. S. et al. Stimulation of testosterone production in rat Leydig cells by aldosterone is mineralocorticoid receptor mediated. Mol. Cell. Endocrinol. 243, 35–42 (2005).
Patisaul, H. B. Endocrine disruption of vasopressin systems and related behaviors. Front. Endocrinol. 8, 134 (2017).
Sullivan, A. W. et al. A novel model for neuroendocrine toxicology: neurobehavioral effects of BPA exposure in a prosocial species, the prairie vole (Microtus ochrogaster). Endocrinology 155, 3867–3881 (2014).
Cao, J., Mickens, J. A., McCaffrey, K. A., Leyrer, S. M. & Patisaul, H. B. Neonatal Bisphenol A exposure alters sexually dimorphic gene expression in the postnatal rat hypothalamus. Neurotoxicology 33, 23–36 (2012).
Adewale, H. B., Todd, K. L., Mickens, J. A. & Patisaul, H. B. The impact of neonatal bisphenol-A exposure on sexually dimorphic hypothalamic nuclei in the female rat. Neurotoxicology 32, 38–49 (2011).
Wolstenholme, J. T. et al. Gestational exposure to bisphenol A produces transgenerational changes in behaviors and gene expression. Endocrinology 153, 3828–3838 (2012).
Masuyama, H. & Hiramatsu, Y. Involvement of suppressor for Gal 1 in the ubiquitin/proteasome-mediated degradation of estrogen receptors. J. Biol. Chem. 279, 12020–12026 (2004).
Picchietti, S. et al. Thyroid disruptor 1,1,1-trichloro-2,2-bis(p-chlorophenyl)ethane (DDT) prevents internalization of TSH receptor. Cell Tissue Res. 336, 31–40 (2009).
Alonso-Magdalena, P. et al. Low doses of bisphenol A and diethylstilbestrol impair Ca2+ signals in pancreatic α-cells through a nonclassical membrane estrogen receptor within intact islets of Langerhans. Environ. Health Perspect. 113, 969 (2005).
Rehfeld, A. et al. EDC IMPACT: chemical UV filters can affect human sperm function in a progesterone-like manner. Endocr. Connect. 7, 16–25 (2018).
Schiffer, C. et al. Direct action of endocrine disrupting chemicals on human sperm. EMBO Rep. 15, 758–765 (2014).
Bouskine, A., Nebout, M., Brucker-Davis, F., Benahmed, M. & Fenichel, P. Low doses of bisphenol A promote human seminoma cell proliferation by activating PKA and PKG via a membrane G-protein-coupled estrogen receptor. Environ. Health Perspect. 117, 1053–1058 (2009).
Sargis, R. M. et al. The novel endocrine disruptor tolylfluanid impairs insulin signaling in primary rodent and human adipocytes through a reduction in insulin receptor substrate-1 levels. Biochim. Biophys. Acta 1822, 952–960 (2012).
Jansen, M. S. et al. Short-chain fatty acids enhance nuclear receptor activity through mitogen-activated protein kinase activation and histone deacetylase inhibition. Proc. Natl. Acad. Sci. USA 101, 7199–7204 (2004).
Routledge, E. J., White, R., Parker, M. G. & Sumpter, J. P. Differential effects of xenoestrogens on coactivator recruitment by estrogen receptor (ER) α and ERβ. J. Biol. Chem. 275, 35986–35993 (2000).
Zhang, Y.-F. et al. Bisphenol A alternatives bisphenol S and bisphenol F interfere with thyroid hormone signaling pathway in vitro and in vivo. Environ. Pollut. 237, 1072–1079 (2018).
Monje, L., Varayoud, J., Munoz-de-Toro, M., Luque, E. & Ramos, J. Neonatal exposure to bisphenol A alters estrogen-dependent mechanisms governing sexual behavior in the adult female rat. Reprod. Toxicol. 28, 435–442 (2009).
Monje, L., Varayoud, J., Muñoz-de-Toro, M., Luque, E. & Ramos, J. Exposure of neonatal female rats to bisphenol A disrupts hypothalamic LHRH pre-mRNA processing and estrogen receptor alpha expression in nuclei controlling estrous cyclicity. Reprod. Toxicol. 30, 625–634 (2010).
Wang, T. et al. Melatonin inhibits the proliferation of breast cancer cells induced by bisphenol A via targeting estrogen receptor-related pathways. Thorac. Cancer 9, 368–375 (2018).
Maerkel, K., Durrer, S., Henseler, M., Schlumpf, M. & Lichtensteiger, W. Sexually dimorphic gene regulation in brain as a target for endocrine disrupters: developmental exposure of rats to 4-methylbenzylidene camphor. Toxicol. Appl. Pharmacol. 218, 152–165 (2007).
Walker, C. L. Minireview: epigenomic plasticity and vulnerability to EDC exposures. Mol. Endocrinol. 30, 848–855 (2016).
Walker, D. M. & Gore, A. C. Epigenetic impacts of endocrine disruptors in the brain. Front. Neuroendocrinol. 44, 1–26 (2017).
Zama, A. M. & Uzumcu, M. Fetal and neonatal exposure to the endocrine disruptor methoxychlor causes epigenetic alterations in adult ovarian genes. Endocrinology 150, 4681–4691 (2009).
Topper, V. Y., Walker, D. M. & Gore, A. C. Sexually dimorphic effects of gestational endocrine-disrupting chemicals on microRNA expression in the developing rat hypothalamus. Mol. Cell. Endocrinol. 414, 42–52 (2015).
Singh, S. & Li, S. S. Epigenetic effects of environmental chemicals bisphenol A and phthalates. Int. J. Mol. Sci. 13, 10143–10153 (2012).
Bhan, A. et al. Bisphenol-A and diethylstilbestrol exposure induces the expression of breast cancer associated long noncoding RNA HOTAIR in vitro and in vivo. J. Steroid Biochem. Mol. Biol. 141, 160–170 (2014).
Bredfeldt, T. G. et al. Xenoestrogen-induced regulation of EZH2 and histone methylation via estrogen receptor signaling to PI3K/AKT. Mol. Endocrinol. 24, 993–1006 (2010).
Krieger, D. T., Brownstein, M. J. & Martin, J. B. Brain Peptides (John Wiley & Sons, 1983)
Wolff, J. Perchlorate and the thyroid gland. Pharmacol. Rev. 50, 89–105 (1998).
Parks, L. G. et al. The plasticizer diethylhexyl phthalate induces malformations by decreasing fetal testosterone synthesis during sexual differentiation in the male rat. Toxicological Sci. 58, 339–349 (2000).
Mylchreest, E., Sar, M., Wallace, D. G. & Foster, P. M. Fetal testosterone insufficiency and abnormal proliferation of Leydig cells and gonocytes in rats exposed to di(n-butyl) phthalate. Reprod. Toxicol. 16, 19–28 (2002).
Jin, Y., Wang, L. & Fu, Z. Oral exposure to atrazine modulates hormone synthesis and the transcription of steroidogenic genes in male peripubertal mice. Gen. Comp. Endocrinol. 184, 120–127 (2013).
Caron-Beaudoin, E., Viau, R. & Sanderson, J. T. Effects of neonicotinoid pesticides on promoter-specific aromatase (CYP19) expression in Hs578t breast cancer cells and the role of the VEGF pathway. Environ. Health Perspect. 126, 047014 (2018).
Bernal, J., Guadano-Ferraz, A. & Morte, B. Thyroid hormone transporters-functions and clinical implications. Nat. Rev. Endocrinol. 11, 690 (2015).
Villar-Pazos, S. et al. Molecular mechanisms involved in the non-monotonic effect of bisphenol-A on Ca2+ entry in mouse pancreatic β-cells. Sci. Rep. 7, 11770 (2017).
Jakobsen, P., Madsen, P. & Andersen, H. S. Imidazolines as efficacious glucose-dependent stimulators of insulin secretion. Eur. J. Med. Chem. 38, 357–362 (2003).
Lindhe, O., Lund, B. O., Bergman, A. & Brandt, I. Irreversible binding and adrenocorticolytic activity of the DDT metabolite 3-methylsulfonyl-DDE examined in tissue-slice culture. Environ. Health Perspect. 109, 105–110 (2001).
Jones, K. A. Handbook of Endocrinology Vol. I (eds Gass, G. H. & Kaplan, H. M.) 1-42 (CRC Press, 1996).
Zhang, Y., Wu, L., Zhang, G., Guan, Y. & Wang, Z. Effect of low-dose malathion on the gonadal development of adult rare minnow Gobiocypris rarus. Ecotoxicol. Environ. Saf. 125, 135–140 (2016).
Zhou, Q. et al. Serum bisphenol-A concentration and sex hormone levels in men. Fertil. Steril. 100, 478–482 (2013).
Kitahara, S. et al. Effects of intravenous administration of high dose-diethylstilbestrol diphosphate on serum hormonal levels in patients with hormone-refractory prostate cancer. Endocr. J. 46, 659–664 (1999).
Brucker-Davis, F. Effects of environmental synthetic chemicals on thyroid function. Thyroid 8, 827–856 (1998).
Kester, M. H. et al. Potent inhibition of estrogen sulfotransferase by hydroxylated PCB metabolites: a novel pathway explaining the estrogenic activity of PCBs. Endocrinology 141, 1897–1900 (2000).
Toivanen, R. & Shen, M. M. Prostate organogenesis: tissue induction, hormonal regulation and cell type specification. Development 144, 1382–1398 (2017).
Inman, J. L., Robertson, C., Mott, J. D. & Bissell, M. J. Mammary gland development: cell fate specification, stem cells and the microenvironment. Development 142, 1028–1042 (2015).
Rey, R. A. & Grinspon, R. P. Normal male sexual differentiation and aetiology of disorders of sex development. Best Pract. Res. Clin. Endocrinol. Metab. 25, 221–238 (2011).
Bansal, R. & Zoeller, R. T. Polychlorinated biphenyls (Aroclor 1254) do not uniformly produce agonist actions on thyroid hormone responses in the developing rat brain. Endocrinology 149, 4001–4008 (2008).
LaPlante, C. D., Bansal, R., Dunphy, K. A., Jerry, D. J. & Vandenberg, L. N. Oxybenzone alters mammary gland morphology in mice exposed during pregnancy and lactation. J. Endocr. Soc. 2, 903–921 (2018).
Forte, M. et al. Triclosan and bisphenol A affect decidualization of human endometrial stromal cells. Mol. Cell. Endocrinol. 422, 74–83 (2016).
Dickerson, S. M., Cunningham, S. L., Patisaul, H. B., Woller, M. J. & Gore, A. C. Endocrine disruption of brain sexual differentiation by developmental PCB exposure. Endocrinology 152, 581–594 (2011).
Zhou, J., Zhang, J., Li, F. & Liu, J. Triazole fungicide tebuconazole disrupts human placental trophoblast cell functions. J. Hazard. Mater. 308, 294–302 (2016).
IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Pharmaceuticals. Volume 100 A. A review of human carcinogens. IARC Monogr. Eval. Carcinog. Risks Hum. 100 (Pt A), 1–401 (2012).
Palmer, J. R. et al. Prenatal DES exposure in relation to breast size. Cancer Causes Control. 24, 1757–1761 (2013).
Herbst, A. L., Poskanzer, D. C., Robboy, S. J., Friedlander, L. & Scully, R. E. Prenatal exposure to stilbestrol. A prospective comparison of exposed female offspring with unexposed controls. N. Engl. J. Med. 292, 334–339 (1975).
Okada, A., Sato, T., Ohta, Y., Buchanan, D. & Iguchi, T. Effect of diethylstilbestrol on cell proliferation and expression of epidermal growth factor in the developing female rat reproductive tract. J. Endocrinol. 170, 539–554 (2001).
Tournaire, M. et al. Adverse health effects in children of women exposed in utero to diethylstilbestrol (DES). Therapie 71, 395–404 (2016).
Dodds, E. C. The new oestrogens. Edinb. Med. J. 48, 1–13 (1941).
Dodds, E. C. The chemistry of oestrogenic compounds and methods of assay. Br. Med. J. 1, 398–399 (1937).
Newbold, R. R. Prenatal exposure to diethylstilbestrol and long-term impact on the breast and reproductive tract in humans and mice. J. Dev. Orig. Health Dis. 3, 73–82 (2012).
Newbold, R. R. Impact of environmental endocrine disrupting chemicals on the development of obesity. Hormones 9, 206–217 (2010).
McLachlan, J. A. Environmental signaling: from environmental estrogens to endocrine-disrupting chemicals and beyond. Andrology 4, 684–694 (2016).
Nam, K., Marshall, P., Wolf, R. M. & Cornell, W. Simulation of the different biological activities of diethylstilbestrol (DES) on estrogen receptor alpha and estrogen-related receptor gamma. Biopolymers 68, 130–138 (2003).
Block, K., Kardana, A., Igarashi, P. & Taylor, H. S. In utero diethylstilbestrol (DES) exposure alters Hox gene expression in the developing mullerian system. FASEB J. 14, 1101–1108 (2000).
Daftary, G. S. & Taylor, H. S. Endocrine regulation of HOX genes. Endocr. Rev. 27, 331–355 (2006).
Newbold, R. R. Prenatal exposure to diethylstilbestrol (DES). Fertil. Steril. 89 (Suppl. 2), e55–e56 (2008).
Rochester, J. R. Bisphenol A and human health: a review of the literature. Reprod. Toxicol. 42, 132–155 (2013).
Vandenberg, L. N. et al. Low dose effects of bisphenol A. An integrated review of in vitro, laboratory animal and epidemiology studies. Endocr. Disruptors 1, e26490 (2013).
Seachrist, D. D. et al. A review of the carcinogenic potential of bisphenol A. Reprod. Toxicol. 59, 167–182 (2016).
Vandenberg, L. N., Maffini, M. V., Sonnenschein, C., Rubin, B. S. & Soto, A. M. Bisphenol-A and the great divide: a review of controversies in the field of endocrine disruption. Endocr. Rev. 30, 75–95 (2009).
Knight, B. A. et al. Effect of perchlorate and thiocyanate exposure on thyroid function of pregnant women from South-West England: a cohort study. Thyroid. Res. 11, 9 (2018).
Rubin, R. et al. Maternal perchlorate exposure in pregnancy and altered birth outcomes. Environ. Res. 158, 72–81 (2017).
Steinmaus, C. et al. Thyroid hormones and moderate exposure to perchlorate during pregnancy in women in southern California. Environ. Health Perspect. 124, 861–867 (2016).
Horton, M. K. et al. Co-occurring exposure to perchlorate, nitrate and thiocyanate alters thyroid function in healthy pregnant women. Environ. Res. 143, 1–9 (2015).
van den Hove, M. F., Beckers, C., Devlieger, H., de Zegher, F. & De Nayer, P. Hormone synthesis and storage in the thyroid of human preterm and term newborns: effect of thyroxine treatment. Biochimie 81, 563–570 (1999).
Pesticide and Environmental Toxicology Branch, Office of Environmental Health Hazard Assessment, California Environmental Protection Agency. Public Health Goal (OEHHA, 2015).
York, R. G. et al. Refining the effects observed in a developmental neurobehavioral study of ammonium perchlorate administered orally in drinking water to rats. I. Thyroid and reproductive effects. Int. J. Toxicol. 24, 403–418 (2005).
Gilbert, M. E. & Sui, L. Developmental exposure to perchlorate alters synaptic transmission in hippocampus of the adult rat. Environ. Health Perspect. 116, 752–760 (2008).
Dohan, O. et al. The Na+/I symporter (NIS) mediates electroneutral active transport of the environmental pollutant perchlorate. Proc. Natl Acad. Sci. USA 104, (20250–20255 (2007).
Zoeller, R. T. Collision of basic and applied approaches to risk assessment of thyroid toxicants. Ann. N. Y. Acad. Sci. 1076, 168–190 (2006).
Guyton, K. Z. et al. Application of the key characteristics of carcinogens in cancer hazard identification. Carcinogenesis 39, 614–622 (2018).
United States Environmental Protection Agency. ToxCast Dashboard. US EPA https://www.epa.gov/chemical-research/toxcast-dashboard (2018).
National Toxicology Program. Tox21: toxicology in the 21st century. NIEHS https://www.ntp.niehs.nih.gov/results/tox21/index.html (2018).
Pinto, C. L., Mansouri, K., Judson, R. & Browne, P. Prediction of estrogenic bioactivity of environmental chemical metabolites. Chem. Res. Toxicol. 29, 1410–1427 (2016).
Judson, R. S. et al. Integrated model of chemical perturbations of a biological pathway using 18 in vitro high-throughput screening assays for the estrogen receptor. Toxicol. Sci. 148, 137–154 (2015).
Boas, M., Feldt-Rasmussen, U. & Main, K. M. Thyroid effects of endocrine disrupting chemicals. Mol. Cell. Endocrinol. 355, 240–248 (2012).
US Environmental Protection Agency. Proposed guidelines for carcinogen risk assessment. Federal Register 61, 17960–18011 (1996).
Carusi, A. et al. Harvesting the promise of AOPs: an assessment and recommendations. Sci. Total Environ. 628–629, 1542–1556 (2018).
Escher, B. I. et al. From the exposome to mechanistic understanding of chemical-induced adverse effects. Environ. Int. 99, 97–106 (2017).
Guyton, K. Z. et al. A reexamination of the PPAR-α activation mode of action as a basis for assessing human cancer risks of environmental contaminants. Environ. Health Perspect. 117, 1664–1672 (2009).
Hill, A. B. The environment and disease: association or causation? Proc. R. Soc. Med. 58, 295–300 (1965).
Nesan, D., Sewell, L. C. & Kurrasch, D. M. Opening the black box of endocrine disruption of brain development: lessons from the characterization of bisphenol A. Horm. Behav. 101, 50–58 (2018).
International Agency for Research on Cancer. Preamble to the IARC Monographs. IARC https://monographs.iarc.fr/preamble-to-the-iarc-monographs (2019).
Andersen, H. R. et al. Comparison of short-term estrogenicity tests for identification of hormone-disrupting chemicals. Environ. Health Perspect. 107, 89–108 (1999).
Li, Y., Burns, K. A., Arao, Y., Luh, C. J. & Korach, K. S. Differential estrogenic actions of endocrine-disrupting chemicals bisphenol A, bisphenol AF, and zearalenone through estrogen receptor α and β in vitro. Environ. Health Perspect. 120, 1029–1035 (2012).
Watson, C. S., Bulayeva, N. N., Wozniak, A. L. & Alyea, R. A. Xenoestrogens are potent activators of nongenomic estrogenic responses. Steroids 72, 124–134 (2007).
Thomas, P. & Dong, J. Binding and activation of the seven-transmembrane estrogen receptor GPR30 by environmental estrogens: a potential novel mechanism of endocrine disruption. J. Steroid Biochem. Mol. Biol. 102, 175–179 (2006).
Sohoni, P. & Sumpter, J. P. Several environmental oestrogens are also anti-androgens. J. Endocrinol. 158, 327–339 (1998).
Rebuli, M. E. et al. Investigation of the effects of subchronic low dose oral exposure to bisphenol A (BPA) and ethinyl estradiol (EE) on estrogen receptor expression in the juvenile and adult female rat hypothalamus. Toxicol. Sci. 140, 190–203 (2014).
Yaoi, T. et al. Genome-wide analysis of epigenomic alterations in fetal mouse forebrain after exposure to low doses of bisphenol A. Biochem. Biophys. Res. Commun. 376, 563–567 (2008).
Wang, Q. et al. Reprogramming of the epigenome by MLL1 links early-life environmental exposures to prostate cancer risk. Mol. Endocrinol. 30, 856–871 (2016).
Aggarwal, R. et al. The mechanism of action of estrogen in castration-resistant prostate cancer: clues from hormone levels. Clin. Genitourin. Cancer 7, E71–E76 (2009).
Geisler, J. et al. Treatment with high-dose estrogen (diethylstilbestrol) significantly decreases plasma estrogen and androgen levels but does not influence in vivo aromatization in postmenopausal breast cancer patients. J. Steroid Biochem. Mol. Biol. 96, 415–422 (2005).
Akingbemi, B. T., Sottas, C. M., Koulova, A. I., Klinefelter, G. R. & Hardy, M. P. Inhibition of testicular steroidogenesis by the xenoestrogen bisphenol A is associated with reduced pituitary luteinizing hormone secretion and decreased steroidogenic enzyme gene expression in rat Leydig cells. Endocrinology 145, 592–603 (2004).
Mahalingam, S. et al. The effects of in utero bisphenol A exposure on ovarian follicle numbers and steroidogenesis in the F1 and F2 generations of mice. Reprod. Toxicol. 74, 150–157 (2017).
Paroder-Belenitsky, M. et al. Mechanism of anion selectivity and stoichiometry of the Na+/I− symporter (NIS). Proc. Natl Acad. Sci. USA 108, 17933–17938 (2011).
Boyns, A. et al. Plasma prolactin, GH, LH, FSH, TSH and testosterone during treatment of prostatic carcinoma with oestrogens. Eur. J. Cancer 10, 445–449 (1974).
Mendiola, J. et al. Are environmental levels of bisphenol A associated with reproductive function in fertile men? Environ. Health Perspect. 118, 1286–1291 (2010).
Troisi, R. et al. Estrogen metabolism in postmenopausal women exposed in utero to diethylstilbestrol. Cancer Epidemiol. Biomarkers Prev. 27, 1208–1213 (2018).
Markey, C. M., Luque, E. H., Munoz De Toro, M., Sonnenschein, C. & Soto, A. M. In utero exposure to bisphenol A alters the development and tissue organization of the mouse mammary gland. Biol. Reprod. 65, 1215–1223 (2001).
Vandenberg, L. N. et al. Perinatal exposure to the xenoestrogen bisphenol-A induces mammary intraductal hyperplasias in adult CD-1 mice. Reprod. Toxicol. 26, 210–219 (2008).
Moral, R. et al. Effect of prenatal exposure to the endocrine disruptor bisphenol A on mammary gland morphology and gene expression signature. J. Endocrinol. 196, 101–112 (2008).
Bosquiazzo, V. L., Varayoud, J., Munoz-de-Toro, M., Luque, E. H. & Ramos, J. G. Effects of neonatal exposure to bisphenol A on steroid regulation of vascular endothelial growth factor expression and endothelial cell proliferation in the adult rat uterus. Biol. Reprod. 82, 86–95 (2010).
Acknowledgements
This project was supported by contract 17-E0023 from the California EPA and by the Research Translation Core of the NIEHS Superfund Research Center at Berkeley under NIH grant P42ES004705. The authors acknowledge funding from the National Institutes of Health (R01ES023254 and R56ES020662 to A.C.G.; 1ZIAES070065 to K.S.K.; R01ES028110 to H.B.P.; P42ES004705 to M.T.S.; P01ES022841 and R01ES027051 to T.J.W.), USEPA (RD-83543301 to T.J.W.), Department of Defense (AR160055 to H.B.P.), Office of Environmental Health Hazard Assessment (17-E0024 to M.A.L.M.; 17-E0023 to M.T.S.) and Japan Society for the Promotion of Science (KAKENHI-PROJECT-15H01749 to H.S.). We thank all other members of the 2018 Working Group who attended the workshop in Berkeley, California, for important discussion, including the following: X. Arzuaga, US EPA; B. Eskenazi, UC Berkeley; C. Gibbons, US EPA; R. Hauser, Harvard; U. Luderer, UC Irvine; C. McHale, UC Berkeley; G. Prins, University of Illinois at Chicago; M. Sandy, OEHHA; T. Schug, NIEHS; N. Skakkebaek, University of Copenhagen; G. Solomon, UC San Francisco; O. Udagawa, NIES, Japan; and L. Zhang, UC Berkeley. The views expressed in this article are those of the authors and do not necessarily represent the views or the policies of the U.S. Environmental Protection Agency, the California Environmental Protection Agency, the National Institute of Environmental Health Sciences, the Organization of Economic Cooperation and Development or the International Agency for Research on Cancer.
Author information
Authors and Affiliations
Contributions
M.A.L.M., L.N.V., W.G., P.B., T.J.W. and A.C.G. researched data for the article. M.A.L.M., L.N.V., M.T.S., W.G., P.B., H.B.P., K.Z.G., A.K., V.J.C., T.J.W., K.S.K., A.C.G., L.Z. and R.T.Z. contributed to discussions on the content. M.A.L.M., L.N.V., M.T.S., W.G., P.B., K.Z.G., V.J.C., T.J.W., L.R., H.S., K.S.K., A.C.G., L.Z. and R.T.Z. wrote the article. M.A.L.M., M.T.S., W.G., P.B., H.B.P., K.Z.G., A.K., V.J.C., T.J.W., L.R., H.S., K.S.K., A.C.G., L.Z. and R.T.Z reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
M.T.S. has served as a consultant and expert witness in US litigation involving chemical and pharmaceutical exposures and various disease outcomes, including neuropathies and cancer. All other authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Risk
-
Probability that an agent will cause a disease or an adverse effect at a given level of exposure.
- Differentiation
-
The process by which a multi-fate cell changes into a different more specialized cell.
- Hazard
-
An agent that can cause disease or an adverse effect.
- Carcinogens
-
Agents capable of causing cancer in living tissue.
- Epigenetic processes
-
Changes to DNA caused by actions, such as acetylation and methylation of DNA and histones and expression of non-coding RNAs, which change gene availability and expression but do not change DNA sequence.
- Distribution
-
The transfer of a substance from one location to another within the body following its absorption.
- Clearance
-
The elimination and removal of a substance from a tissue or the organism as a whole.
- Decidualization
-
A differentiation process that occurs in the uterus to promote placental formation.
- Biomarkers
-
Measurable substances in an organism whose presence is indicative of some phenomenon such as disease, infection or environmental exposure.
- ToxCast
-
A multi-year effort based at the US Environmental Protection Agency and launched in 2007 that uses automated chemical screening technologies, called high-throughput screening assays, to expose living cells, isolated proteins or other biological molecules to chemicals.
- Tox21
-
A federal collaboration among the US Environmental Protection Agency, NIH (including National Center for Advancing Translational Sciences and the National Toxicology Program at the National Institute of Environmental Health Sciences) and the US Food and Drug Administration.
- Mode of action
-
A functional or anatomical change, at the cellular level, resulting from the exposure of a living organism to a substance.
- Adverse outcome pathways
-
The structured representation of biological events leading in a linear way to an adverse effect, beginning with a molecular initiating event and ending in an adverse outcome.
- Molecular initiating event
-
The point at which a chemical first effects a biological target.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
La Merrill, M.A., Vandenberg, L.N., Smith, M.T. et al. Consensus on the key characteristics of endocrine-disrupting chemicals as a basis for hazard identification. Nat Rev Endocrinol 16, 45–57 (2020). https://doi.org/10.1038/s41574-019-0273-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-019-0273-8
This article is cited by
-
Gut microbiota contributes to bisphenol A-induced maternal intestinal and placental apoptosis, oxidative stress, and fetal growth restriction in pregnant ewe model by regulating gut-placental axis
Microbiome (2024)
-
Association of maternal exposure to endocrine disruptor chemicals with cardio-metabolic risk factors in children during childhood: a systematic review and meta-analysis of cohort studies
Diabetology & Metabolic Syndrome (2024)
-
A life-course approach to tackling noncommunicable diseases in women
Nature Medicine (2024)
-
Estrogenic endocrine disruptor exposure directly impacts erectile function
Communications Biology (2024)
-
Changing epidemiology of colorectal cancer — birth cohort effects and emerging risk factors
Nature Reviews Gastroenterology & Hepatology (2024)