Abstract
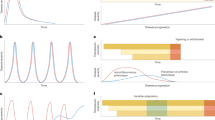
Juvenile idiopathic arthritis (JIA) is an umbrella term for arthritis of unknown origin, lasting for >6 weeks with onset before 16 years of age. JIA is the most common chronic inflammatory rheumatic condition of childhood. According to the International League Against Rheumatism (ILAR) classification, seven mutually exclusive categories of JIA exist based on disease manifestations during the first 6 months of disease. Although the ILAR classification has been useful to foster research, it has been criticized mainly as it does not distinguish those forms of chronic arthritis observed in adults and in children from those that may be unique to childhood. Hence, efforts to provide a new evidence-based classification are ongoing. Similar to arthritis observed in adults, pathogenesis involves autoimmune and autoinflammatory mechanisms. The field has witnessed a remarkable improvement in therapeutic possibilities of JIA owing to the availability of new potent drugs and the possibility to perform controlled trials with support from legislative interventions and large networks availability. The goal of drug therapy in JIA is to rapidly reduce disease activity to inactive disease or clinical remission, minimize drug side effects and achieve a quality of life comparable to that of healthy peers. As JIA can influence all aspects of a child’s and their family’s life, researchers increasingly recognize improvement of health-related quality of life as a key treatment goal.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$99.00 per year
only $99.00 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Ravelli, A. & Martini, A. Juvenile idiopathic arthritis. Lancet 369, 767–778 (2007).
Prakken, B., Albani, S. & Martini, A. Juvenile idiopathic arthritis. Lancet 377, 2138–2149 (2011).
Brewer, E. J. Jr. et al. Current proposed revision of JRA criteria. JRA Criteria Subcommittee of the Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Section of the Arthritis Foundation. Arthritis Rheum. 20, 195–199 (1977).
Wood, P. H. N. in The Care of Rheumatic Children (ed. Munthe, E.) 47–50 (EULAR, 1987).
Petty, R. E. et al. Revision of the proposed classification criteria for juvenile idiopathic arthritis: Durban, 1997. J. Rheumatol. 25, 1991–1994 (1998).
Petty, R. E. et al. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J. Rheumatol. 31, 390–392 (2004).
Viola, S. et al. Development and validation of a clinical index for assessment of long-term damage in juvenile idiopathic arthritis. Arthritis Rheum. 52, 2092–2102 (2005).
Giancane, G. et al. Disease activity and damage in juvenile idiopathic arthritis: methotrexate era versus biologic era. Arthritis Res. Ther. 21, 168 (2019).
Thierry, S., Fautrel, B., Lemelle, I. & Guillemin, F. Prevalence and incidence of juvenile idiopathic arthritis: a systematic review. Jt. Bone Spine 81, 112–117 (2014).
Hyrich, K. L. et al. Disease activity and disability in children with juvenile idiopathic arthritis one year following presentation to paediatric rheumatology. Results from the Childhood Arthritis Prospective Study. Rheumatology 49, 116–122 (2010).
McDougall, C., Hurd, K. & Barnabe, C. Systematic review of rheumatic disease epidemiology in the indigenous populations of Canada, the United States, Australia, and New Zealand. Semin. Arthritis Rheum. 46, 675–686 (2017).
Consolaro, A. et al. Phenotypic variability and disparities in treatment and outcomes of childhood arthritis throughout the world: an observational cohort study. Lancet Child. Adolesc. Health 3, 255–263 (2019).
Horton, D. B. & Shenoi, S. Review of environmental factors and juvenile idiopathic arthritis. Open. Access. Rheumatol. 11, 253–267 (2019).
Xin, L., He, F., Li, S., Zhou, Z. X. & Ma, X. L. Intestinal microbiota and juvenile idiopathic arthritis: current understanding and future prospective. World J. Pediatr. 17, 40–51 (2021).
van Dijkhuizen, E. H. P. et al. Microbiome analytics of the gut microbiota in patients with juvenile idiopathic arthritis: a longitudinal observational cohort study. Arthritis Rheumatol. 71, 1000–1010 (2019).
Smolen, J. S. et al. Rheumatoid arthritis. Nat. Rev. Dis. Prim. 4, 18001 (2018).
Macaubas, C., Nguyen, K., Milojevic, D., Park, J. L. & Mellins, E. D. Oligoarticular and polyarticular JIA: epidemiology and pathogenesis. Nat. Rev. Rheumatol. 5, 616–626 (2009).
Mijnheer, G. & van Wijk, F. T-cell compartmentalization and functional adaptation in autoimmune inflammation: lessons from pediatric rheumatic diseases. Front. Immunol. 10, 940 (2019).
Lopez-Isac, E. et al. Combined genetic analysis of juvenile idiopathic arthritis clinical subtypes identifies novel risk loci, target genes and key regulatory mechanisms. Ann. Rheum. Dis. 80, 321–328 (2020).
Hinks, A. et al. Dense genotyping of immune-related disease regions identifies 14 new susceptibility loci for juvenile idiopathic arthritis. Nat. Genet. 45, 664–669 (2013).
McIntosh, L. A. et al. Genome-wide association meta-analysis reveals novel juvenile idiopathic arthritis susceptibility loci. Arthritis Rheumatol. 69, 2222–2232 (2017).
Ombrello, M. J. et al. Genetic architecture distinguishes systemic juvenile idiopathic arthritis from other forms of juvenile idiopathic arthritis: clinical and therapeutic implications. Ann. Rheum. Dis. 76, 906–913 (2017).
Prahalad, S. et al. Juvenile rheumatoid arthritis– linkage to HLA demonstrated by allele sharing in affected sibpairs. Arthritis Rheum. 43, 2335–2338 (2000).
Prahalad, S. et al. Hierarchy of risk of childhood-onset rheumatoid arthritis conferred by HLA-DRB1 alleles encoding the shared epitope. Arthritis Rheum. 64, 925–930 (2012).
Ombrello, M. J. et al. HLA-DRB1*11 and variants of the MHC class II locus are strong risk factors for systemic juvenile idiopathic arthritis. Proc. Natl Acad. Sci. USA 112, 15970–15975 (2015).
Nigrovic, P. A., Martinez-Bonet, M. & Thompson, S. D. Implications of juvenile idiopathic arthritis genetic risk variants for disease pathogenesis and classification. Curr. Opin. Rheumatol. 31, 401–410 (2019).
Hinks, A. et al. Fine-mapping the MHC locus in juvenile idiopathic arthritis (JIA) reveals genetic heterogeneity corresponding to distinct adult inflammatory arthritic diseases. Ann. Rheum. Dis. 76, 765–772 (2017).
Burren, O. S. et al. Genetic feature engineering enables characterisation of shared risk factors in immune-mediated diseases. Genome Med. 12, 106 (2020).
Meng, X. et al. Association of novel rare coding variants with juvenile idiopathic arthritis. Ann. Rheum. Dis. 80, 626–631 (2021).
Albani, S. et al. Positive selection in autoimmunity: abnormal immune responses to a bacterial dnaJ antigenic determinant in patients with early rheumatoid arthritis. Nat. Med. 1, 448–452 (1995).
Massa, M. et al. Differential recognition of heat-shock protein dnaJ-derived epitopes by effector and Treg cells leads to modulation of inflammation in juvenile idiopathic arthritis. Arthritis Rheum. 56, 1648–1657 (2007).
Kamphuis, S. et al. Tolerogenic immune responses to novel T-cell epitopes from heat-shock protein 60 in juvenile idiopathic arthritis. Lancet 366, 50–56 (2005).
Spreafico, R. et al. Epipolymorphisms associated with the clinical outcome of autoimmune arthritis affect CD4+ T cell activation pathways. Proc. Natl Acad. Sci. USA 113, 13845–13850 (2016).
Spreafico, R. et al. A circulating reservoir of pathogenic-like CD4+ T cells shares a genetic and phenotypic signature with the inflamed synovial micro-environment. Ann. Rheum. Dis. 75, 459–465 (2016).
Rossetti, M. et al. TCR repertoire sequencing identifies synovial Treg cell clonotypes in the bloodstream during active inflammation in human arthritis. Ann. Rheum. Dis. 76, 435–441 (2017).
Petrelli, A. et al. PD-1+CD8+ T cells are clonally expanding effectors in human chronic inflammation. J. Clin. Invest. 128, 4669–4681 (2018).
Fischer, J. et al. IL-21(+) CD4(+) T helper cells co-expressing IFN-γ and TNF-α accumulate in the joints of antinuclear antibody positive patients with juvenile idiopathic arthritis. Clin. Immunol. 217, 108484 (2020).
Bending, D., Giannakopoulou, E., Lom, H. & Wedderburn, L. R. Synovial regulatory T cells occupy a discrete TCR niche in human arthritis and require local signals to stabilize FOXP3 protein expression. J. Immunol. 195, 5616–5624 (2015).
Henderson, L. A. et al. Next-generation sequencing reveals restriction and clonotypic expansion of Treg cells in juvenile idiopathic arthritis. Arthritis Rheumatol. 68, 1758–1768 (2016).
Wilkinson, M. G. L. & Rosser, E. C. B cells as a therapeutic target in paediatric rheumatic disease. Front. Immunol. 10, 214 (2019).
Morbach, H. et al. Activated memory B cells may function as antigen-presenting cells in the joints of children with juvenile idiopathic arthritis. Arthritis Rheum. 63, 3458–3466 (2011).
Mahmud, S. A. & Binstadt, B. A. Autoantibodies in the pathogenesis, diagnosis, and prognosis of juvenile idiopathic arthritis. Front. Immunol. 9, 3168 (2019).
Schmidt, T. et al. Children with oligoarticular juvenile idiopathic arthritis have skewed synovial monocyte polarization pattern with functional impairment–a distinct inflammatory pattern for oligoarticular juvenile arthritis. Arthritis Res. Ther. 22, 186 (2020).
Arve-Butler, S. et al. Synovial fluid neutrophils in oligoarticular juvenile idiopathic arthritis have an altered phenotype and impaired effector functions. Arthritis Res. Ther. 23, 109 (2021).
de Jesus, A. A. et al. Distinct interferon signatures and cytokine patterns define additional systemic autoinflammatory diseases. J. Clin. Invest. 130, 1669–1682 (2020).
McClain, K. L. & Allen, C. E. Fire behind the fury: IL-18 and MAS. Blood 131, 1393–1394 (2018).
Crayne, C. B., Albeituni, S., Nichols, K. E. & Cron, R. Q. The immunology of macrophage activation syndrome. Front. Immunol. 10, 119 (2019).
Alehashemi, S. & Goldbach-Mansky, R. Human autoinflammatory diseases mediated by NLRP3-, Pyrin-, NLRP1-, and NLRC4-inflammasome dysregulation updates on diagnosis, treatment, and the respective roles of IL-1 and IL-18. Front. Immunol. 11, 1840 (2020).
Petty, R. E. et al. in Textbook of Pediatric Rheumatology (Elsevier, 2021).
Glaesener, S. et al. Distinct effects of methotrexate and etanercept on the B cell compartment in patients with juvenile idiopathic arthritis. Arthritis Rheumatol. 66, 2590–2600 (2014).
Bulatovic Calasan, M. et al. Methotrexate treatment affects effector but not regulatory T cells in juvenile idiopathic arthritis. Rheumatology 54, 1724–1734 (2015).
Petrelli, A. et al. Self-sustained resistance to suppression of CD8+ Teff cells at the site of autoimmune inflammation can be reversed by tumor necrosis factor and interferon-γ blockade. Arthritis Rheumatol. 68, 229–236 (2016).
Marasco, E. et al. Switched memory B cells are increased in oligoarticular and polyarticular juvenile idiopathic arthritis and their change over time is related to response to tumor necrosis factor inhibitors. Arthritis Rheumatol. 70, 606–615 (2018).
Leong, J. Y. et al. Immunome perturbation is present in patients with juvenile idiopathic arthritis who are in remission and will relapse upon anti-TNFα withdrawal. Ann. Rheum. Dis. 78, 1712–1721 (2019).
Choy, E. H. et al. Translating IL-6 biology into effective treatments. Nat. Rev. Rheumatol. 16, 335–345 (2020).
Yeo, J. G. et al. The Extended Polydimensional Immunome Characterization (EPIC) web-based reference and discovery tool for cytometry data. Nat. Biotechnol. 38, 679–684 (2020).
Martini, A. Are the number of joints involved or the presence of psoriasis still useful tools to identify homogeneous disease entities in juvenile idiopathic arthritis? J. Rheumatol. 30, 1900–1903 (2003).
Martini, A. It is time to rethink juvenile idiopathic arthritis classification and nomenclature. Ann. Rheum. Dis. 71, 1437–1439 (2012).
Nigrovic, P. A., Raychaudhuri, S. & Thompson, S. D. Review: genetics and the classification of arthritis in adults and children. Arthritis Rheumatol. 70, 7–17 (2018).
Martini, A. et al. Toward new classification criteria for juvenile idiopathic arthritis: first steps, Pediatric Rheumatology International Trials Organization international consensus. J. Rheumatol. 46, 190–197 (2019).
Nigrovic, P. A. et al. Biological classification of childhood arthritis: roadmap to a molecular nomenclature. Nat. Rev. Rheumatol. 17, 257–269 (2021).
Ruperto, N. & Martini, A. Current and future perspectives in the management of juvenile idiopathic arthritis. Lancet Child. Adolesc. Health 2, 360–370 (2018).
Lee, J. J. Y. & Schneider, R. Systemic juvenile idiopathic arthritis. Pediatr. Clin. North Am. 65, 691–709 (2018).
Martini, A. Systemic juvenile idiopathic arthritis. Autoimmun. Rev. 12, 56–59 (2012).
Saper, V. E. et al. Emergent high fatality lung disease in systemic juvenile arthritis. Ann. Rheum. Dis. 78, 1722–1731 (2019).
Martini, A. et al. Intravenous iron therapy for severe anaemia in systemic-onset juvenile chronic arthritis. Lancet 344, 1052–1054 (1994).
Cazzola, M. et al. Defective iron supply for erythropoiesis and adequate endogenous erythropoietin production in the anemia associated with systemic-onset juvenile chronic arthritis. Blood 87, 4824–4830 (1996).
Grom, A. A., Horne, A. & De Benedetti, F. Macrophage activation syndrome in the era of biologic therapy. Nat. Rev. Rheumatol. 12, 259–268 (2016).
Ravelli, A., Davi, S., Minoia, F., Martini, A. & Cron, R. Q. Macrophage activation syndrome. Hematol. Oncol. Clin. North Am. 29, 927–941 (2015).
Ravelli, A. et al. 2016 classification criteria for macrophage activation syndrome complicating systemic juvenile idiopathic arthritis: a European League Against Rheumatism/American College of Rheumatology/Paediatric Rheumatology International Trials Organisation Collaborative Initiative. Ann. Rheum. Dis. 75, 481–489 (2016).
Ichida, H. et al. Clinical manifestations of adult-onset Still’s disease presenting with erosive arthritis: association with low levels of ferritin and Interleukin-18. Arthritis Care. Res. 66, 642–646 (2014).
Shimizu, M. et al. Interleukin-18 for predicting the development of macrophage activation syndrome in systemic juvenile idiopathic arthritis. Clin. Immunol. 160, 277–281 (2015).
Gattorno, M. et al. The pattern of response to anti-interleukin-1 treatment distinguishes two subsets of patients with systemic-onset juvenile idiopathic arthritis. Arthritis Rheum. 58, 1505–1515 (2008).
Wakil, S. M. et al. Association of a mutation in LACC1 with a monogenic form of systemic juvenile idiopathic arthritis. Arthritis Rheumatol. 67, 288–295 (2015).
Colbert, R. A. Classification of juvenile spondyloarthritis: enthesitis-related arthritis and beyond. Nat. Rev. Rheumatol. 6, 477–485 (2010).
Tse, S. M. & Laxer, R. M. New advances in juvenile spondyloarthritis. Nat. Rev. Rheumatol. 8, 269–279 (2012).
Weiss, P. F. & Colbert, R. A. Juvenile spondyloarthritis: a distinct form of juvenile arthritis. Pediatr. Clin. North Am. 65, 675–690 (2018).
Martini, A. & Hachulla, E. in EULAR Textbook on Paediatric Rheumatology (BMJ, 2018).
Bray, T. J. et al. Association of the apparent diffusion coefficient with maturity in adolescent sacroiliac joints. J. Magn. Reson. Imaging 44, 556–564 (2016).
Watkin, L. B. et al. COPA mutations impair ER-Golgi transport and cause hereditary autoimmune-mediated lung disease and arthritis. Nat. Genet. 47, 654–660 (2015).
Sen, E. S. & Ramanan, A. V. Juvenile idiopathic arthritis-associated uveitis. Clin. Immunol. 211, 108322 (2020).
Ravelli, A. et al. Patients with antinuclear antibody-positive juvenile idiopathic arthritis constitute a homogeneous subgroup irrespective of the course of joint disease. Arthritis Rheum. 52, 826–832 (2005).
Ravelli, A. et al. Antinuclear antibody-positive patients should be grouped as a separate category in the classification of juvenile idiopathic arthritis. Arthritis Rheum. 63, 267–275 (2011).
Stoll, M. L. et al. Patients with juvenile psoriatic arthritis comprise two distinct populations. Arthritis Rheum. 54, 3564–3572 (2006).
Southwood, T. R. et al. Psoriatic arthritis in children. Arthritis Rheum. 32, 1007–1013 (1989).
Stoll, M. L., Lio, P., Sundel, R. P. & Nigrovic, P. A. Comparison of Vancouver and International League of Associations for Rheumatology classification criteria for juvenile psoriatic arthritis. Arthritis Rheum. 59, 51–58 (2008).
von Schuckmann, L., Klotsche, J., Suling, A., Kahl-Nieke, B. & Foeldvari, I. Temporomandibular joint involvement in patients with juvenile idiopathic arthritis: a retrospective chart review. Scand. J. Rheumatol. 49, 271–280 (2020).
Frid, P. et al. Temporomandibular joint involvement in association with quality of life, disability, and high disease activity in juvenile idiopathic arthritis. Arthritis Care. Res. 69, 677–686 (2017).
Weiss, P. F. & Chauvin, N. A. Imaging in the diagnosis and management of axial spondyloarthritis in children. Best. Pract. Res. Clin. Rheumatol. 34, 101596 (2020).
Chhabra, A. et al. Long-term outcomes and disease course of children with juvenile idiopathic arthritis in the ReACCh-Out cohort: a two-centre experience. Rheumatology 59, 3727–3730 (2020).
Glerup, M. et al. Long-term outcomes in juvenile idiopathic arthritis: eighteen years of follow-up in the population-based Nordic Juvenile Idiopathic Arthritis cohort. Arthritis Care. Res. 72, 507–516 (2020).
Palman, J., Shoop-Worrall, S., Hyrich, K. & McDonagh, J. E. Update on the epidemiology, risk factors and disease outcomes of juvenile idiopathic arthritis. Best. Pract. Res. Clin. Rheumatol. 32, 206–222 (2018).
Guzman, J., Oen, K. & Loughin, T. Predicting disease severity and remission in juvenile idiopathic arthritis: are we getting closer? Curr. Opin. Rheumatol. 31, 436–449 (2019).
Heiligenhaus, A., Niewerth, M., Ganser, G., Heinz, C. & Minden, K. Prevalence and complications of uveitis in juvenile idiopathic arthritis in a population-based nation-wide study in Germany: suggested modification of the current screening guidelines. Rheumatology 46, 1015–1019 (2007).
Malattia, C., Rinaldi, M. & Martini, A. The role of imaging in juvenile idiopathic arthritis. Expert Rev. Clin. Immunol. 14, 681–694 (2018).
Malattia, C. et al. Current status of MR imaging of juvenile idiopathic arthritis. Best. Pract. Res. Clin. Rheumatol. 34, 101629 (2020).
Windschall, D. & Malattia, C. Ultrasound imaging in paediatric rheumatology. Best. Pract. Res. Clin. Rheumatol. 34, 101570 (2020).
Ravelli, A. et al. Treating juvenile idiopathic arthritis to target: recommendations of an international task force. Ann. Rheum. Dis. 77, 819–828 (2018).
Nusman, C. M. et al. Dynamic contrast-enhanced magnetic resonance imaging of the wrist in children with juvenile idiopathic arthritis. Pediatr. Radiol. 47, 205–213 (2017).
Roth, J. et al. Definitions for the sonographic features of joints in healthy children. Arthritis Care. Res. 67, 136–142 (2015).
Colebatch-Bourn, A. N. et al. EULAR-PReS points to consider for the use of imaging in the diagnosis and management of juvenile idiopathic arthritis in clinical practice. Ann. Rheum. Dis. 74, 1946–1957 (2015).
European Commission. State of Paediatric Medicines in the EU: 10 years of the EU Paediatric Regulation. Report from the Commission to the European Parliament and the Council (European Commission, 2017).
Ruperto, N., Vesely, R., Saint-Raymond, A. & Martini, A., Paediatric Rheumatology International Trials Organisation (PRINTO). Impact of the European paediatric legislation in paediatric rheumatology: past, present and future. Ann. Rheum. Dis. 72, 1893–1896 (2013).
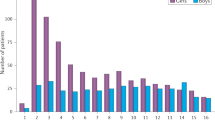
Brunner, H. I. et al. Pediatric Rheumatology Collaborative Study Group – over four decades of pivotal clinical drug research in pediatric rheumatology. Pediatr. Rheumatol. Online J. 16, 45 (2018).
Ruperto, N. & Martini, A. International research networks in pediatric rheumatology: the PRINTO perspective. Curr. Opin. Rheumatol. 16, 566–570 (2004).
Ruperto, N. et al. A randomized, placebo-controlled trial of infliximab plus methotrexate for the treatment of polyarticular-course juvenile rheumatoid arthritis. Arthritis Rheum. 56, 3096–3106 (2007).
Giannini, E. H. et al. Preliminary definition of improvement in juvenile arthritis. Arthritis Rheum. 40, 1202–1209 (1997).
Lovell, D. J. et al. Etanercept in children with polyarticular juvenile rheumatoid arthritis. Pediatric Rheumatology Collaborative Study Group. N. Engl. J. Med. 342, 763–769 (2000). First pivotal randomized clinical trial of etanercept, an anti-TNF biologic disease-modifying anti-rheumatic drug for the treatment of polyarticular course JIA.
Brunner, H. I., Lovell, D. J., Finck, B. K. & Giannini, E. H. Preliminary definition of disease flare in juvenile rheumatoid arthritis. J. Rheumatol. 29, 1058–1064 (2002).
Lovell, D. J. et al. Adalimumab with or without methotrexate in juvenile rheumatoid arthritis. N. Engl. J. Med. 359, 810–820 (2008). Pivotal randomized clinical trial of adalimumab, an anti-TNF biologic disease-modifying anti-rheumatic drug for the treatment of polyarticular course JIA.
Ruperto, N. et al. Abatacept in children with juvenile idiopathic arthritis: a randomised, double-blind, placebo-controlled withdrawal trial. Lancet 372, 383–391 (2008). Pivotal randomized clinical trial of abatacept, an anti-T cell biologic disease-modifying anti-rheumatic drug for the treatment of polyarticular course JIA.
Ruperto, N. et al. Is it time to move to active comparator trials in juvenile idiopathic arthritis? A review of current study designs. Arthritis Rheum. 62, 3131–3139 (2010).
De Benedetti, F. et al. Randomized trial of tocilizumab in systemic juvenile idiopathic arthritis. N. Engl. J. Med. 367, 2385–2395 (2012). Pivotal randomized clinical trial of tocilizumab and anti-IL-6 biologic disease-modifying anti-rheumatic drug for the treatment of systemic JIA in a Caucasian population.
Ruperto, N. et al. Two randomized trials of canakinumab in systemic juvenile idiopathic arthritis. N. Engl. J. Med. 367, 2396–2406 (2012). Pivotal randomized clinical trial of canakinumab and anti-IL-1 biologic disease-modifying anti-rheumatic drug for the treatment of systemic JIA.
Ruperto, N. et al. Pharmacokinetic and safety profile of tofacitinib in children with polyarticular course juvenile idiopathic arthritis: results of a phase 1, open-label, multicenter study. Pediatr. Rheumatol. Online J. 15, 86 (2017).
Brunner, H. I. et al. Subcutaneous golimumab for children with active polyarticular-course juvenile idiopathic arthritis: results of a multicentre, double-blind, randomised-withdrawal trial. Ann. Rheum. Dis. 77, 21–29 (2018).
Ruperto, N. et al. Subcutaneous dosing regimens of tocilizumab in children with systemic or polyarticular juvenile idiopathic arthritis. Rheumatology 60, 4568–4580 (2021).
Ruperto, N. et al. Tofacitinib in juvenile idiopathic arthritis: a double-blind, placebo-controlled, withdrawal phase 3 randomised trial. Lancet 398, 1984–1996 (2021). Pivotal randomized clinical trial of tofacitinib, the first oral anti-JAK disease-modifying anti-rheumatic drug for the treatment of polyarticular course JIA.
Brunner, H. I. et al. Efficacy and safety of tocilizumab for polyarticular-course juvenile idiopathic arthritis in the open-label two-year extension of a phase III trial. Arthritis Rheumatol. 73, 530–541 (2021).
Ruperto, N. et al. Open-label phase 3 study of intravenous golimumab in patients with polyarticular juvenile idiopathic arthritis. Rheumatology 60, 4495–4507 (2021).
Martini, A. & Lovell, D. J. Juvenile idiopathic arthritis: state of the art and future perspectives. Ann. Rheum. Dis. 69, 1260–1263 (2010).
Beukelman, T. et al. 2011 American College of Rheumatology recommendations for the treatment of juvenile idiopathic arthritis: initiation and safety monitoring of therapeutic agents for the treatment of arthritis and systemic features. Arthritis Care. Res. 63, 465–482 (2011).
Ruperto, N. & Martini, A. Emerging drugs to treat juvenile idiopathic arthritis. Expert Opin. Emerg. Drugs 16, 493–505 (2011).
Giancane, G. & Ruperto, N. & Paediatric Rheumatology International Trials Organisation (PRINTO). Treatment of juvenile idiopathic arthritis: what’s new? Curr. Opin. Rheumatol. 31, 428–435 (2019).
Ruperto, N. et al. A randomized, double-blind clinical trial of two doses of meloxicam compared with naproxen in children with juvenile idiopathic arthritis: short- and long-term efficacy and safety results. Arthritis Rheum. 52, 563–572 (2005).
Reiff, A. et al. Evaluation of the comparative efficacy and tolerability of rofecoxib and naproxen in children and adolescents with juvenile rheumatoid arthritis: a 12-week randomized controlled clinical trial with a 52-week open-label extension. J. Rheumatol. 33, 985–995 (2006).
Ravelli, A., Lattanzi, B., Consolaro, A. & Martini, A. Glucocorticoids in paediatric rheumatology. Clin. Exp. Rheumatol. 29, S148–S152 (2011).
Zulian, F. et al. Comparison of intra-articular triamcinolone hexacetonide and triamcinolone acetonide in oligoarticular juvenile idiopathic arthritis. Rheumatology 42, 1254–1259 (2003).
Zulian, F. et al. Triamcinolone acetonide and hexacetonide intra-articular treatment of symmetrical joints in juvenile idiopathic arthritis: a double-blind trial. Rheumatology 43, 1288–1291 (2004).
Ravelli, A. et al. Intra-articular corticosteroids versus intra-articular corticosteroids plus methotrexate in oligoarticular juvenile idiopathic arthritis: a multicentre, prospective, randomised, open-label trial. Lancet 389, 909–916 (2017). Pivotal academic randomized clinical trial of intra-articular corticosteroid injection plus methotrexate in oligoarticular JIA, the most common JIA category.
Tynjala, P. et al. Aggressive combination drug therapy in very early polyarticular juvenile idiopathic arthritis (ACUTE-JIA): a multicentre randomised open-label clinical trial. Ann. Rheum. Dis. 70, 1605–1612 (2011).
Wallace, C. A. et al. Trial of early aggressive therapy in polyarticular juvenile idiopathic arthritis. Arthritis Rheum. 64, 2012–2021 (2012).
Hissink Muller, P. et al. Treat to target (drug-free) inactive disease in DMARD-naive juvenile idiopathic arthritis: 24-month clinical outcomes of a three-armed randomised trial. Ann. Rheum. Dis. 78, 51–59 (2019).
Klein, A. et al. Treat-to-target study for improved outcome in polyarticular juvenile idiopathic arthritis. Ann. Rheum. Dis. 79, 969–974 (2020).
Kimura, Y. et al. Optimizing the start time of biologics in polyarticular juvenile idiopathic arthritis: a comparative effectiveness study of childhood arthritis and rheumatology research alliance consensus treatment plans. Arthritis Rheumatol. 73, 1898–1909 (2021).
Ong, M. S. et al. Improved disease course associated with early initiation of biologics in polyarticular juvenile idiopathic arthritis: trajectory analysis of a Childhood Arthritis and Rheumatology Research Alliance consensus treatment plans study. Arthritis Rheumatol. 73, 1910–1920 (2021).
Ruperto, N., Martini, A. & Pistorio, A., Paediatric Rheumatology International Trials Organisation. “To Randomize, or Not to Randomize, That is the Question”. Arthritis Rheumatol. 73, 1776–1779 (2021).
Ringold, S. et al. 2013 update of the 2011 American College of Rheumatology recommendations for the treatment of juvenile idiopathic arthritis: recommendations for the medical therapy of children with systemic juvenile idiopathic arthritis and tuberculosis screening among children receiving biologic medications. Arthritis Care. Res. 65, 1551–1563 (2013).
Constantin, T. et al. Consensus-based recommendations for the management of uveitis associated with juvenile idiopathic arthritis: the SHARE initiative. Ann. Rheum. Dis. 77, 1107–1117 (2018).
Foeldvari, I. et al. Correction to: Proposal for a definition for response to treatment, inactive disease and damage for JIA associated uveitis based on the validation of a uveitis related JIA outcome measures from the Multinational Interdisciplinary Working Group for Uveitis in Childhood (MIWGUC). Pediatr. Rheumatol. Online J. 18, 14 (2020).
Angeles-Han, S. T. et al. 2019 American College of Rheumatology/Arthritis Foundation guideline for the screening, monitoring, and treatment of juvenile idiopathic arthritis-associated uveitis. Arthritis Care. Res. 71, 703–716 (2019).
Ringold, S. et al. 2019 American College of Rheumatology/Arthritis Foundation guideline for the treatment of juvenile idiopathic arthritis: therapeutic approaches for non-systemic polyarthritis, sacroiliitis, and enthesitis. Arthritis Rheumatol. 71, 846–863 (2019).
Horneff, G. et al. The German etanercept registry for treatment of juvenile idiopathic arthritis. Ann. Rheum. Dis. 63, 1638–1644 (2004).
Horneff, G. et al. Double-blind, placebo-controlled randomized trial with adalimumab for treatment of juvenile onset ankylosing spondylitis (JoAS): significant short term improvement. Arthritis Res. Ther. 14, R230 (2012).
Lovell, D. J., Ruperto, N., Giannini, E. H. & Martini, A. Advances from clinical trials in juvenile idiopathic arthritis. Nat. Rev. Rheumatol. 9, 557–563 (2013).
Giannini, E. H. et al. Methotrexate in resistant juvenile rheumatoid arthritis. Results of the U.S.A.-U.S.S.R. double-blind, placebo-controlled trial. The Pediatric Rheumatology Collaborative Study Group and The Cooperative Children’s Study Group. N. Engl. J. Med. 326, 1043–1049 (1992). Pivotal academic randomized clinical trial of methotrexate for the treatment of JIA.
Woo, P. et al. Randomized, placebo-controlled, crossover trial of low-dose oral methotrexate in children with extended oligoarticular or systemic arthritis. Arthritis Rheum. 43, 1849–1857 (2000).
Ruperto, N. et al. A randomized trial of parenteral methotrexate comparing an intermediate dose with a higher dose in children with juvenile idiopathic arthritis who failed to respond to standard doses of methotrexate. Arthritis Rheum. 50, 2191–2201 (2004).
Foell, D. et al. Methotrexate withdrawal at 6 vs 12 months in juvenile idiopathic arthritis in remission: a randomized clinical trial. JAMA 303, 1266–1273 (2010).
Silverman, E. et al. Leflunomide or methotrexate for juvenile rheumatoid arthritis. N. Engl. J. Med. 352, 1655–1666 (2005). Pivotal randomized clinical trial of leflunomide for the treatment of JIA.
van Rossum, M. A. et al. Sulfasalazine in the treatment of juvenile chronic arthritis: a randomized, double-blind, placebo-controlled, multicenter study. Dutch Juvenile Chronic Arthritis Study Group. Arthritis Rheum. 41, 808–816 (1998).
Burgos-Vargas, R., Vazquez-Mellado, J., Pacheco-Tena, C., Hernandez-Garduno, A. & Goycochea-Robles, M. V. A 26 week randomised, double blind, placebo controlled exploratory study of sulfasalazine in juvenile onset spondyloarthropathies. Ann. Rheum. Dis. 61, 941–942 (2002).
Heijstek, M. W. et al. EULAR recommendations for vaccination in paediatric patients with rheumatic diseases. Ann. Rheum. Dis. 70, 1704–1712 (2011).
Beukelman, T. et al. Rates of hospitalized bacterial infection associated with juvenile idiopathic arthritis and its treatment. Arthritis Rheum. 64, 2773–2780 (2012).
Becker, I. & Horneff, G. Risk of serious infection in juvenile idiopathic arthritis patients associated with tumor necrosis factor inhibitors and disease activity in the German biologics in pediatric rheumatology registry. Arthritis Care. Res. 69, 552–560 (2017).
Swart, J. et al. Pharmacovigilance in juvenile idiopathic arthritis patients treated with biologic or synthetic drugs: combined data of more than 15,000 patients from Pharmachild and national registries. Arthritis Res. Ther. 20, 285 (2018).
Giancane, G. et al. Opportunistic infections in immunosuppressed patients with juvenile idiopathic arthritis: analysis by the Pharmachild Safety Adjudication Committee. Arthritis Res. Ther. 22, 71 (2020).
Horneff, G. et al. Safety and efficacy of combination of etanercept and methotrexate compared to treatment with etanercept only in patients with juvenile idiopathic arthritis (JIA): preliminary data from the German JIA registry. Ann. Rheum. Dis. 68, 519–525 (2009).
Simard, J. F., Neovius, M., Hagelberg, S. & Askling, J. Juvenile idiopathic arthritis and risk of cancer: a nationwide cohort study. Arthritis Rheum. 62, 3776–3782 (2010).
Diak, P. et al. Tumor necrosis factor α blockers and malignancy in children: forty-eight cases reported to the Food and Drug Administration. Arthritis Rheum. 62, 2517–2524 (2010).
Hashkes, P. J., Uziel, Y. & Laxer, R. M. The safety profile of biologic therapies for juvenile idiopathic arthritis. Nat. Rev. Rheumatol. 6, 561–571 (2010).
Horneff, G., Foeldvari, I., Minden, K., Moebius, D. & Hospach, T. Report on malignancies in the German juvenile idiopathic arthritis registry. Rheumatology 50, 230–236 (2011).
Ruperto, N. & Martini, A. Pediatric rheumatology: JIA, treatment and possible risk of malignancies. Nat. Rev. Rheumatol. 7, 6–7 (2011).
Beukelman, T. et al. Rates of malignancy associated with juvenile idiopathic arthritis and its treatment. Arthritis Rheum. 64, 1263–1271 (2012).
Nordstrom, B. L. et al. Risk of malignancy in children with juvenile idiopathic arthritis not treated with biologic agents. Arthritis Care Res. 64, 1357–1364 (2012).
Ruperto, N. & Martini, A. Juvenile idiopathic arthritis and malignancy. Rheumatology 53, 968–974 (2014).
Beukelman, T. et al. Risk of malignancy associated with paediatric use of tumour necrosis factor inhibitors. Ann. Rheum. Dis. 77, 1012–1016 (2018).
Lovell, D. J. et al. Long-term safety and efficacy of etanercept in children with polyarticular-course juvenile rheumatoid arthritis. Arthritis Rheum. 54, 1987–1994 (2006).
Brunner, H. I. et al. Efficacy and safety of tocilizumab in patients with polyarticular-course juvenile idiopathic arthritis: results from a phase 3, randomised, double-blind withdrawal trial. Ann. Rheum. Dis. 74, 1110–1117 (2015).
Bharucha, K. N. et al. Growth during tocilizumab therapy for polyarticular-course juvenile idiopathic arthritis: 2-year data from a phase III clinical trial. J. Rheumatol. 45, 1173–1179 (2018).
Malattia, C. et al. Tocilizumab may slow radiographic progression in patients with systemic or polyarticular-course juvenile idiopathic arthritis: post hoc radiographic analysis from two randomized controlled trials. Arthritis Res. Ther. 22, 211 (2020).
Brunner, H. I. et al. Subcutaneous abatacept in patients with polyarticular-course juvenile idiopathic arthritis: results from a phase III open-label study. Arthritis Rheumatol. 70, 1144–1154 (2018).
Lehman, T. J. et al. Thalidomide for severe systemic onset juvenile rheumatoid arthritis: a multicenter study. J. Pediatr. 145, 856–857 (2004).
Wulffraat, N., van Royen, A., Bierings, M., Vossen, J. & Kuis, W. Autologous haemopoietic stem-cell transplantation in four patients with refractory juvenile chronic arthritis. Lancet 353, 550–553 (1999).
Wulffraat, N. M. et al. Current perspectives of autologous stem cell transplantation for severe juvenile idiopathic rthritis. Autoimmunity 41, 632–638 (2008).
Ruperto, N. et al. A phase II study to evaluate dosing and preliminary safety and efficacy of canakinumab in systemic juvenile idiopathic arthritis with active systemic features. Arthritis Rheum. 64, 557–567 (2011).
Nigrovic, P. A. et al. Anakinra as first-line disease-modifying therapy in systemic juvenile idiopathic arthritis: report of forty-six patients from an international multicenter series. Arthritis Rheum. 63, 545–555 (2011).
Vastert, S. J. et al. Effectiveness of first-line treatment with recombinant interleukin-1 receptor antagonist in steroid-naive patients with new-onset systemic juvenile idiopathic arthritis: results of a prospective cohort study. Arthritis Rheumatol. 66, 1034–1043 (2014).
Ter Haar, N. M. et al. Treatment to target using recombinant interleukin-1 receptor antagonist as first-line monotherapy in new-onset systemic juvenile idiopathic arthritis: results from a five-year follow-up study. Arthritis Rheumatol. 71, 1163–1173 (2019).
Quartier, P. et al. Tapering canakinumab monotherapy in patients with systemic juvenile idiopathic arthritis in clinical remission: results from a phase IIIb/IV open-label, randomized study. Arthritis Rheumatol. 73, 336–346 (2021).
Yokota, S. et al. Efficacy and safety of tocilizumab in patients with systemic-onset juvenile idiopathic arthritis: a randomised, double-blind, placebo-controlled, withdrawal phase III trial. Lancet 371, 998–1006 (2008). Pivotal randomized clinical trial of tocilizumab, an anti-IL-6 biologic disease-modifying anti-rheumatic drug for the treatment of systemic JIA in Japan.
Sandborg, C. & Mellins, E. D. A new era in the treatment of systemic juvenile idiopathic arthritis. N. Engl. J. Med. 367, 2439–2440 (2012).
Nigrovic, P. A. Review: is there a window of opportunity for treatment of systemic juvenile idiopathic arthritis? Arthritis Rheumatol. 66, 1405–1413 (2014).
Richards, J. C., Tay-Kearney, M. L., Murray, K. & Manners, P. Infliximab for juvenile idiopathic arthritis-associated uveitis. Clin. Exp. Ophthalmol. 33, 461–468 (2005).
Simonini, G. et al. Current therapeutic approaches to autoimmune chronic uveitis in children. Autoimmun. Rev. 9, 674–683 (2010).
Simonini, G., Paudyal, P., Jones, G. T., Cimaz, R. & Macfarlane, G. J. Current evidence of methotrexate efficacy in childhood chronic uveitis: a systematic review and meta-analysis approach. Rheumatology 52, 825–831 (2013).
Simonini, G. et al. Superior efficacy of adalimumab in treating childhood refractory chronic uveitis when used as first biologic modifier drug: adalimumab as starting anti-TNF-α therapy in childhood chronic uveitis. Pediatr. Rheumatol. Online J. 11, 16 (2013).
Zannin, M. E. et al. Safety and efficacy of infliximab and adalimumab for refractory uveitis in juvenile idiopathic arthritis: 1-year followup data from the Italian registry. J. Rheumatol. 40, 74–79 (2013).
Ramanan, A. V. et al. Adalimumab plus methotrexate for uveitis in juvenile idiopathic arthritis. N. Engl. J. Med. 376, 1637–1646 (2017). Pivotal academic randomized clinical trial with adalimumab an anti-TNF biologic disease-modifying anti-rheumatic drug for the treatment of JIA-associated uveitis.
Quartier, P. et al. ADJUVITE: a double-blind, randomised, placebo-controlled trial of adalimumab in early onset, chronic, juvenile idiopathic arthritis-associated anterior uveitis. Ann. Rheum. Dis. 77, 1003–1011 (2018).
van Dijken, T. D. et al. Development of inflammatory bowel disease in patients with juvenile idiopathic arthritis treated with etanercept. J. Rheumatol. 38, 1441–1446 (2011).
Lamb, C. A. et al. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut 68, s1–s106 (2019).
Maller, J. et al. Inflammatory bowel disease in children with systemic juvenile idiopathic arthritis. J. Rheumatol. 48, 567–574 (2020).
Ravelli, A. et al. Expert consensus on dynamics of laboratory tests for diagnosis of macrophage activation syndrome complicating systemic juvenile idiopathic arthritis. RMD Open 2, e000161 (2016).
Boom, V. et al. Evidence-based diagnosis and treatment of macrophage activation syndrome in systemic juvenile idiopathic arthritis. Pediatr. Rheumatol. Online J. 13, 55 (2015).
Saha, M. T., Verronen, P., Laippala, P. & Lenko, H. L. Growth of prepubertal children with juvenile chronic arthritis. Acta Paediatr. 88, 724–728 (1999).
Giannini, E. H. et al. Long-term safety and effectiveness of etanercept in children with selected categories of juvenile idiopathic arthritis. Arthritis Rheum. 60, 2794–2804 (2009).
Giannini, E. H. et al. Effects of long-term etanercept treatment on growth in children with selected categories of juvenile idiopathic arthritis. Arthritis Rheum. 62, 3259–3264 (2010).
De Benedetti, F. et al. Catch-up growth during tocilizumab therapy for systemic juvenile idiopathic arthritis: results from a phase III trial. Arthritis Rheumatol. 67, 840–848 (2015).
Shoop-Worrall, S. J. W. et al. Patient-reported wellbeing and clinical disease measures over time captured by multivariate trajectories of disease activity in individuals with juvenile idiopathic arthritis in the UK: a multicentre prospective longitudinal study. Lancet Rheumatol. 3, e111–e121 (2020).
Fair, D. C., Rodriguez, M., Knight, A. M. & Rubinstein, T. B. Depression and anxiety in patients with juvenile idiopathic arthritis: current insights and impact on quality of life, a systematic review. Open Access. Rheumatol. 11, 237–252 (2019).
Singh, G., Athreya, B. H., Fries, J. F. & Goldsmith, D. P. Measurement of health status in children with juvenile rheumatoid arthritis. Arthritis Rheum. 37, 1761–1769 (1994).
Ruperto, N. et al. Cross-cultural adaptation and psychometric evaluation of the Childhood Health Assessment Questionnaire (CHAQ) and the Child Health Questionnaire (CHQ) in 32 countries. Review of the general methodology. Clin. Exp. Rheumatol. 19, S1–S9 (2001).
Filocamo, G. et al. Evaluation of 21-numbered circle and 10-centimeter horizontal line visual analog scales for physician and parent subjective ratings in juvenile idiopathic arthritis. J. Rheumatol. 37, 1534–1541 (2010).
Filocamo, G. et al. A new approach to clinical care of juvenile idiopathic arthritis: the Juvenile Arthritis Multidimensional Assessment Report. J. Rheumatol. 38, 938–953 (2011).
Consolaro, A. et al. Development and validation of a composite disease activity score for juvenile idiopathic arthritis. Arthritis Rheum. 61, 658–666 (2009).
Consolaro, A. et al. Remission, minimal disease activity, and acceptable symptom state in juvenile idiopathic arthritis: defining criteria based on the juvenile arthritis disease activity score. Arthritis Rheum. 64, 2366–2374 (2012).
Nordal, E. B. et al. Validity and predictive ability of the juvenile arthritis disease activity score based on CRP versus ESR in a Nordic population-based setting. Ann. Rheum. Dis. 71, 1122–1127 (2012).
Consolaro, A. et al. Defining criteria for high disease activity in juvenile idiopathic arthritis based on the juvenile arthritis disease activity score. Ann. Rheum. Dis. 73, 1380–1383 (2014).
Trincianti, C. et al. Definition and validation of the American College of Rheumatology 2021 juvenile arthritis disease activity score cutoffs for disease activity states in juvenile idiopathic arthritis. Arthritis Rheumatol. 73, 1966–1975 (2021).
McErlane, F. et al. Validity of a three-variable juvenile arthritis disease activity score in children with new-onset juvenile idiopathic arthritis. Ann. Rheum. Dis. 72, 1983–1988 (2013).
Tibaldi, J. et al. Development and initial validation of a composite disease activity score for systemic juvenile idiopathic arthritis. Rheumatology 59, 3505–3514 (2020).
Wallace, C. A. et al. Preliminary criteria for clinical remission for select categories of juvenile idiopathic arthritis. J. Rheumatol. 31, 2290–2294 (2004).
Wallace, C. A. et al. American College of Rheumatology provisional criteria for defining clinical inactive disease in select categories of juvenile idiopathic arthritis. Arthritis Care. Res. 63, 929–936 (2011).
Nielsen, S. et al. Preliminary evidence that etanercept may reduce radiographic progression in juvenile idiopathic arthritis. Clin. Exp. Rheumatol. 26, 688–692 (2008).
Ravelli, A. et al. Radiologic progression in patients with juvenile chronic arthritis treated with methotrexate. J. Pediatr. 133, 262–265 (1998).
Rossi, F. et al. Use of the Sharp and Larsen scoring methods in the assessment of radiographic progression in juvenile idiopathic arthritis. Arthritis Rheum. 55, 717–723 (2006).
Malattia, C. et al. Magnetic resonance imaging, ultrasonography, and conventional radiography in the assessment of bone erosions in juvenile idiopathic arthritis. Arthritis Rheum. 59, 1764–1772 (2008).
European Medicines Agency. Reflection paper on the regulatory guidance for the use of health related quality of life (HRQL) measures in the evaluation of medicinal products. EMA https://www.ema.europa.eu/en/documents/scientific-guideline/reflection-paper-regulatory-guidance-use-healthrelated-quality-life-hrql-measures-evaluation_en.pdf (2005).
Food and Drug Administration. Guidance for industry. Patient-reported outcome measures: use in medical product development to support labeling claims. FDA http://www.fda.gov/downloads/Drugs/Guidances/UCM193282.pdf (2009).
Landgraf, J. M., Abetz, L. & Ware, J. E. The Child Health Questionnaire (CHQ): A User’s Manual (The Health Institute, New England Medical Center, 1996).
Varni, J. W. et al. The PedsQL in pediatric rheumatology: reliability, validity, and responsiveness of the pediatric quality of life inventory generic core scales and rheumatology module. Arthritis Rheum. 46, 714–725 (2002).
Reeve, B. B. et al. Psychometric evaluation and calibration of health-related quality of life item banks: plans for the Patient-Reported Outcomes Measurement Information System (PROMIS). Med. Care 45, S22–S31 (2007).
Angeles-Han, S. T. et al. Development of a vision-related quality of life instrument for children ages 8–18 years for use in juvenile idiopathic arthritis-associated uveitis. Arthritis Care Res. 63, 1254–1261 (2011).
Cassedy, A. et al. Assessing the validity and reliability of the Effects of Youngsters’ Eyesight on Quality of Life (EYE-Q) questionnaire among children with uveitis. Arthritis Care. Res. https://doi.org/10.1002/acr.24491 (2020).
Filocamo, G. et al. Development and validation of a new short and simple measure of physical function for juvenile idiopathic arthritis. Arthritis Rheum. 57, 913–920 (2007).
Filocamo, G. et al. A new short and simple health-related quality of life measurement for paediatric rheumatic diseases: initial validation in juvenile idiopathic arthritis. Rheumatology 49, 1272–1280 (2010).
Bovis, F. et al. Cross-cultural adaptation and psychometric evaluation of the Juvenile Arthritis Multidimensional Assessment Report (JAMAR) in 54 languages across 52 countries: review of the general methodology. Rheumatol. Int. 38, 5–17 (2018).
Oen, K. et al. Health-related quality of life in an inception cohort of children with juvenile idiopathic arthritis: a longitudinal analysis. Arthritis Care. Res. 70, 134–144 (2018).
Listing, M. et al. The majority of patients with newly diagnosed juvenile idiopathic arthritis achieve a health-related quality of life that is similar to that of healthy peers: results of the German Multicenter Inception Cohort (ICON). Arthritis Res. Ther. 20, 106 (2018).
Seid, M., Opipari, L., Huang, B., Brunner, H. I. & Lovell, D. J. Disease control and health-related quality of life in juvenile idiopathic arthritis. Arthritis Rheum. 61, 393–399 (2009).
Oen, K. et al. Causal pathways to health-related quality of life in children with juvenile idiopathic arthritis: results from the ReACCh-Out cohort. Rheumatology 60, 4691–4702 (2021).
Butler, A. et al. Mental disorder in children with physical conditions: a pilot study. BMJ Open 8, e019011 (2018).
Vuorimaa, H. et al. Empirical classification of children with JIA: a multidimensional approach to pain and well-being. Clin. Exp. Rheumatol. 26, 954–961 (2008).
Russo, E. et al. Psychological profile in children and adolescents with severe course juvenile idiopathic arthritis. ScientificWorldJournal 2012, 841375 (2012).
Haverman, L. et al. Health-related quality of life and psychosocial developmental trajectory in young female beneficiaries with JIA. Rheumatology 51, 368–374 (2012).
Zhou, Q. et al. Loss-of-function mutations in TNFAIP3 leading to A20 haploinsufficiency cause an early-onset autoinflammatory disease. Nat. Genet. 48, 67–73 (2016).
Malattia, C. & Martini, A. Paediatric-onset systemic lupus erythematosus. Best. Pract. Res. Clin. Rheumatol. 27, 351–362 (2013).
Zhou, Q. et al. Early-onset stroke and vasculopathy associated with mutations in ADA2. N. Engl. J. Med. 370, 911–920 (2014).
Navon Elkan, P. et al. Mutant adenosine deaminase 2 in a polyarteritis nodosa vasculopathy. N. Engl. J. Med. 370, 921–931 (2014).
Beck, D. B. et al. Somatic mutations in UBA1 and severe adult-onset autoinflammatory disease. N. Engl. J. Med. 383, 2628–2638 (2020).
Martini, A. Are there new targets for juvenile idiopathic arthritis? Semin. Arthritis Rheum. 49, S11–S13 (2019).
Caorsi, R. et al. ADA2 deficiency (DADA2) as an unrecognised cause of early onset polyarteritis nodosa and stroke: a multicentre national study. Ann. Rheum. Dis. 76, 1648–1656 (2017).
Deane, K. D. & Holers, V. M. Rheumatoid arthritis pathogenesis, prediction, and prevention: an emerging paradigm shift. Arthritis Rheumatol. 73, 181–193 (2021).
Ruperto, N. et al. PRINTO/PRES international website for families of children with rheumatic diseases: https://www.printo.it/pediatric-rheumatology/. Ann. Rheum. Dis. 64, 1101–1106 (2005).
Acknowledgements
The authors thank C. Pallotti for editorial assistance (coordination among co-authors, bibliography, English revision).
Author information
Authors and Affiliations
Contributions
Introduction (A.M.); Epidemiology (K.L.H.); Mechanisms/pathophysiology (S.D.T. and S.A.); Diagnosis, screening and prevention (A.M. and H.I.B.); Management (N.R. and D.J.L.); Quality of life (H.I.B.); Outlook (A.M.); Overview of the Primer (A.M.).
Corresponding author
Ethics declarations
Competing interests
A.M. has received honoraria for consultancies or speaker bureaus from Aurinia, Bristol Myers Squibb, Eli Lilly, EMD Serono, Janssen, Pfizer and Roche. D.J.L.’s institution, the Cincinnati Children’s Hospital Medical Center, has received research grants from BMS, Janssen, Novartis, Pfizer Inc., Roche and UBC; and has received consulting fees or other remuneration from AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Novartis, Pfizer Inc., Roche, Takeda and UBC for the work of D.J.L. D.J.L. is a member of the Data Safety and Monitoring Boards for studies funded by the National Institutes of Health and the Canadian Arthritis Society. H.I.B. received speaker fees from Novartis, Pfizer, Roche and GlaxoSmithKline. The Cincinnati Children’s Hospital, where H.I.B. works as a full-time employee, has received contributions from the following companies for consultation and research activities in the past 3 years: AbbVie, AstraZeneca–MedImmune, Biogen, Boehringer, Bristol Myers Squibb, Celgene, Eli Lilly, EMD Serono, Idorsia, Cerocor, F. Hoffmann-La Roche, Merck, Novartis and Sanofi. This funding has been reinvested for the research activities of the hospital in a fully independent manner, without any commitment to third parties. K.L.H. has received honoraria from Abbvie and grant support from Pfizer and Bristol Myers Squibb. K.L.H. is also supported by the NIHR Biomedical Research Centre. S.D.T. is supported by Cincinnati Children’s Research Foundation and the US National Institutes of Health. N.R. has received honoraria for consultancies or speaker bureaus from the following pharmaceutical companies in the past 3 years: 2-Bridge, Amgen, AstraZeneca, Aurinia, Bayer, Brystol Myers and Squibb, Celgene, inMed, Cambridge Healthcare Research, Domain Therapeutic, EMD Serono, Glaxo Smith Kline, Idorsia, Janssen, Lilly, Novartis, Pfizer, Sobi, UCB. S.A. declares no competing interests.
Additional information
Peer review information
Nature Reviews Disease Primers thanks T. Herlin, P. Nigrovic, I. Foeldvari and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Glossary
- Step-up strategy
-
Progressive treatment escalation in order to meet a predefined clinical target.
- Treat-to-target strategy
-
A therapeutic strategy aimed at obtaining a predefined clinical target.
- Macrophage activation syndrome
-
A form of haemophagocytic lymphohistiocytosis characterized by very severe inflammation owing to uncontrolled proliferation of activated lymphocytes and macrophages with production of massive amounts of pro-inflammatory cytokines (also known as cytokine storm).
- Myalgias
-
Pain in the muscle.
- Pericarditis
-
Inflammation of the membrane (pericardium) surrounding the heart.
- Pleuritis
-
Inflammation of the membranes (pleurae) that surround the lungs and line the chest cavity.
- Leukocytosis
-
Increase in the number of circulating leukocytes.
- Hyperferritinaemia
-
Increase in serum ferritin, a protein released by activated macrophages.
- Thrombocytosis
-
Increase in the number of circulating platelets.
- Microcytic anaemia
-
Presence of small, often hypochromic, red blood cells in a peripheral blood smear.
- Tarsitis
-
Inflammation of the intertarsal joints and bones (mid-foot arthritis).
- Enthesitis
-
Inflammation of the sites where tendons, ligaments or fascia insert into bone.
- Iridocyclitis
-
Inflammation of the eye affecting both the iris and ciliary body.
- Acute phase reactants
-
Serum proteins whose levels increase during inflammation.
- Synechiae
-
Adhesions that are formed between adjacent structures within the eye owing to inflammation resulting in an irregular and poorly reactive pupil.
- Cataract
-
A cloudy area in the lens of the eye that leads to a decrease in vision.
- Band keratopathy
-
Linear band of calcium that becomes deposited across the cornea.
- Macular oedema
-
Build-up of fluid in the macula, an area in the centre of the retina.
- Glaucoma
-
Damage of the optic nerve due to increase in intraocular pressure.
- Tenosynovitis
-
Inflammation of the fluid-filled sheath that surrounds tendons.
- Micrognathia
-
A condition in which the lower jaw is under-sized.
- Osteopenia
-
Reduced bone mineral density.
- Biosimilars
-
A biological medical product that is almost an identical copy of an original product (bio-originator) that is manufactured by a different company.
- Bio-originator
-
Original biological medication manufactured by a company.
- Catch-up growth
-
Height velocity above the limits of normal age for at least 1 year after a transient period of growth inhibition.
- Behçet disease
-
Systemic inflammatory disorder, the most common symptoms of which include painful mouth sores, genital sores, inflammation of parts of the eye and arthritis.
- Systemic lupus erythematosus
-
A chronic autoimmune disease that may affect every organ and tissue.
- Panarteritis nodosa
-
A blood vessel disease characterized by inflammation of small and medium-sized arteries (vasculitis).
- Relapsing polychondritis
-
A condition characterized by repeated episodes of inflammation and deterioration of cartilage.
- Sweet syndrome
-
An inflammatory disease causing fever and a painful skin rash that appears mostly on the arms, face and neck.
- Giant cell arteritis
-
A disease that affects the arteries of the scalp and neck, which become red, hot, swollen or painful.
Rights and permissions
About this article
Cite this article
Martini, A., Lovell, D.J., Albani, S. et al. Juvenile idiopathic arthritis. Nat Rev Dis Primers 8, 5 (2022). https://doi.org/10.1038/s41572-021-00332-8
Accepted:
Published:
DOI: https://doi.org/10.1038/s41572-021-00332-8
This article is cited by
-
Screening for juvenile idiopathic arthritis associated uveitis with laser flare photometry in the pediatric rheumatology office: a prospective observational study
Pediatric Rheumatology (2024)
-
Efficacy and safety of gut microbiota-based therapies in autoimmune and rheumatic diseases: a systematic review and meta-analysis of 80 randomized controlled trials
BMC Medicine (2024)
-
Gene association analysis to determine the causal relationship between immune cells and juvenile idiopathic arthritis
Pediatric Rheumatology (2024)
-
Establishment and analysis of a novel diagnostic model for systemic juvenile idiopathic arthritis based on machine learning
Pediatric Rheumatology (2024)
-
Single-cell characterisation of tissue homing CD4 + and CD8 + T cell clones in immune-mediated refractory arthritis
Molecular Medicine (2024)