Abstract
While studies on ambient fine particulate matter (PM2.5) exposure effect on child health are available, the differential effects, if any, of exposure to PM2.5 species are unexplored in lower and middle-income countries. Using multiple logistic regression, we showed that for every 10 μg m−3 increase in PM2.5 exposure, anaemia, acute respiratory infection, and low birth weight prevalence increase by 10% (95% uncertainty interval, UI: 9–11), 11% (8–13), and 5% (4–6), respectively, among children in India. NO3-, elemental carbon, and NH4+ were more associated with the three health outcomes than other PM2.5 species. We found that the total PM2.5 mass as a surrogate marker for air pollution exposure could substantially underestimate the true composite impact of different components of PM2.5. Our findings provide key indigenous evidence to prioritize control strategies for reducing exposure to more toxic species for greater child health benefits in India.
Similar content being viewed by others
Introduction
Air pollution poses a significant global health risk, with 6.67 million (95% UI: 5.90–7.49) deaths worldwide attributable to the combined effects of household and ambient air pollution1. In 2019, over 99% of the world’s population inhaled fine particulate matter (PM2.5) concentrations that exceeded the World Health Organization (WHO) annual air quality guideline (AQG) of 5 μg m−3 2. In India, home to one-sixth of the global population, ambient PM2.5 exposure has been rising in the last three decades3. In 2017, the majority (76.8%) of the people in India were exposed to an annual population-weighted mean PM2.5 higher than the national ambient air quality standard (NAAQS) of 40 μg m−3 4.
The latest round of the state-level burden of diseases in India estimated that ambient PM2.5 exposure was responsible for 0.98 million (0.77–1.19) deaths and 17.8 million disability-adjusted life years5. The Lancet Commission has emphasized that children under the age of 5 years (U5) are more vulnerable to the harmful impacts of air pollution, even at low levels, particularly during foetal development and the first few months of life6. Thus, early-life exposure to air pollution7 impacts child health outcomes such as acute respiratory infection (ARI)8, which are the most common cause of global childhood morbidity and mortality9. In addition to mortality, ambient PM2.5 exposure is a risk factor for adverse pregnancy outcomes, including low birth weight (LBW)10, stillbirth11, foetal mortality12, preterm birth13, and birth defects14. In early childhood, it is a risk factor for impaired child growth, stunting6,15, and anaemia16,17. Since the lower and middle-income countries (LMICs) have higher levels of ambient PM2.5 exposure compared to higher-income countries; the LMIC children are likely to have disproportionately higher rates of these morbidities and mortality linked to prenatal and early childhood exposure to ambient PM2.518.
PM2.5, by itself, is a composite mixture of multiple chemical species. The components of PM2.5 may have varying toxicity with varying mass fractions. As a result, the true cumulative impact of ambient PM2.5 on health could be manifold higher than that estimated by the total PM2.5 mass19,20. Moreover, the PM2.5 species can be tagged to specific emitting sectors, providing opportunities to examine their relative importance in mitigation strategies. The association between PM2.5 components and their sectoral contributions and U5 child health outcomes is unknown at the national level in the LMICs.
To address these critical knowledge gaps, we estimated the association of ambient PM2.5 and its components and emitting sectors on three U5 child health outcomes—anaemia, ARI, and LBW, in India and provided a hypothesis to establish a causal inference of the results. We combined anthropometric measurements, blood biomarkers, and socioeconomic information from the fourth round of the national family health survey (NFHS-4) with granular information on sector-specific speciated PM2.5 exposure that was obtained by integrating satellite-derived PM2.5 with outputs from the weather research forecasting (WRF) and community multi-scale air quality modelling system (WRF-CMAQ) model (see ‘Methods’ for details). In this study, we assess the effect of PM2.5 components and their contributing sources on multiple child health outcomes and further assess the expected health benefits of meeting various clean air targets.
Results
Study population and characteristics
There were 259,627 observations in the original NFHS-4 dataset, of which 15,119 children had missing age. After removing missing records of exposure, outcome, and covariates, there were 177,072 observations in the final analytical sample for LBW and ARI (a detailed flowchart is given in Supplementary Fig. 1). In the anaemia analysis, all the anaemia status-missing observations were excluded.
The national prevalence of LBW from the analytical sample was 16.6% (16.4, 16.8). This was slightly higher in girls (17.8%) than in boys (15.5%). A significant variation in the prevalence of LBW was observed across the levels of the mother’s education, socioeconomic status, mother’s body mass index (BMI), age, place of residence, and different levels of PM2.5. The prevalence of anaemia among U5 children was 56.8% (56.6, 57.1). Anaemia was associated with maternal education, religion, socioeconomic, place of residence, levels of PM2.5 exposure, and maternal anaemia status.
The national prevalence of ARI was 2.8% (2.7–2.9). Maternal education, religion, socioeconomic, place of residence, and levels of PM2.5 exposure were significantly associated with ARI. The estimated ARI prevalence was relatively higher in rural areas than in urban (2.9% vs. 2.4%) areas (Supplementary Table 1).
The annual average PM2.5 level at the PSU level was 62 µg m−3 with an interquartile range (IQR) of 52–79 µg m−3. The most dominant PM2.5 components were organic carbon (OC), NO3-, NH4+, SO42-, and others that include chloride, sodium, magnesium, potassium, calcium, soil, and water molecules, and the remaining unspecified components. These were mostly contributed from domestic, industrial, international, agricultural, and transport sectors (Supplementary Table 2).
Effects of PM2.5 and its components and sources on child health
The two-stage model (‘Methods’) estimated the odds ratio, OR of LBW as 1.15 (1.12–1.18), of anaemia as 1.57 (1.54–1.59), and of ARI as 1.32 (1.24–1.4) for every IQR increase in ambient PM2.5 exposure. Further, gestational exposure to NO3- showed the highest association on LBW of children with OR 1.17 (1.14–1.2) per IQR increase in exposure. The estimated ORs of LBW for every IQR increase in gestational exposure of others, NH4+, elemental carbon (EC), soil, SO42-, and OC were 1.14 (1.11–1.17), 1.13 (1.11–1.16), 1.11 (1.08–1.14), 1.09 (1.07–1.11), 1.07 (1.04–1.09), and 1.05 (1.03–1.08), respectively (Fig. 1). For anaemia, we observed the largest impact of NO3- (OR: 1.36, 1.32–1.41), followed by NH4+ (OR: 1.28, 1.25–1.31), others (OR: 1.25, 1.21–1.28), EC (OR: 1.21, 1.18–1.25), soil (OR: 1.18, 1.16–1.20), SO42- (OR: 1.14, 1.12–1.17), OC (OR: 1.12, 1.09–1.15) (Fig. 1). Similarly, the effect of NO3- on ARI was relatively higher than other components. The estimated OR of ARI was 1.52 (1.42–1.61) for every IQR increase in NO3-. EC also had a larger impact on ARI (OR: 1.49, 1.4–1.58), followed by OC (OR: 1.46, 1.37–1.55), others (OR: 1.33, 1.26–1.41) and NH4+ (OR: 1.15, 1.09–1.21) (Fig. 1).
Odds ratio per IQR of PM2.5 components concentrations with their 95% confidence intervals (black dots with error bars) for given health outcomes i.e., LBW, Anaemia, and ARI. The analytical sample size used for each health outcome is provided in the consort diagram (Supplementary Fig. 1).
Among the eight PM2.5 sources analysed using the two-stage model, we found that the IQR increase in PM2.5 from road dust exhibited a higher effect on LBW (OR: 1.13, 1.11–1.14), followed by the international transboundary transport (OR: 1.09, 1.07–1.1), the industry sector (OR: 1.07, 1.05–1.08), the agricultural sector (OR: 1.06, 1.05–1.07), other sectors (OR: 1.04, 1.02–1.07) and transport sector (OR: 1.05, 1.02–1.07). For anaemia, every IQR increase in PM2.5 exposure attributable to the sectoral emissions of unorganized (that includes municipal waste burning and crematorium) sectors (OR, 1.19; 1.18–1.20) showed the highest adverse effect, followed by the international transboundary transport (OR: 1.11, 1.09–1.13), domestic and road dust (ORs: 1.09 (1.06–1.11) and 1.09 (1.08–1.11), respectively), agriculture (OR: 1.08, 1.07–1.09), industry (OR: 1.04, 1.02–1.06), and transport (OR: 1.03, 1.0–1.06) sector. The power sector (OR: 0.96, 0.94–0.98) did not show any effect on anaemia among children (Fig. 2). The domestic sector showed the largest effect on ARI than the rest of the sectors. For every IQR increase of PM2.5 from the domestic sector, we observed OR of ARI as 1.30 (1.24–1.35) followed by the transport sector (OR: 1.21, 1.14–1.28), other sectors (OR: 1.21, 1.14–1.28) and the agricultural sector (OR: 1.1, 1.07–1.13).
Odds ratio per IQR of PM2.5 sectoral concentrations with their 95% confidence intervals (black dots with error bars) for given health outcomes i.e., LBW, Anaemia, and ARI. The analytical sample size used for each health outcome is provided in the consort diagram (Supplementary Fig. 1).
Effects of PM2.5 components on anaemia and ARI stratified by LBW
Stratified estimates were obtained by adding an interaction term of LBW in the second-stage model with air pollutants, one at a time (‘Methods’). For an IQR increase in NO3-, we observed the OR of anaemia as 1.47 (1.41–1.52) for children born with LBW vs. 1.34 (1.3–1.38) for children born with normal weight. Apart from NO3-, a larger difference was observed for EC (OR 1.3 vs. 1.2), and OC (OR 1.2 vs. 1.1). Similarly, OR of ARI was 1.72 (1.6–1.85) and 1.46 (1.37–1.56), respectively, for LBW and normal birth weight children for IQR increase in NO3. EC (OR 1.7 vs. 1.4) and OC (OR 1.6 vs. 1.4) also showed large differences between LBW and normal birth weight (Fig. 3). Exactly similar patterns were observed for PM2.5 emission attributable to different sectors when stratified by LBW (Fig. 4).
The odds ratios with their 95% confidence intervals are represented in black dots with error bars. LBW represents low birth weight; NBW represents normal birth weight. The analytical sample size used for each health outcome is provided in the consort diagram (Supplementary Fig. 1).
Odds ratios with their 95% confidence intervals are represented in black dots with error bars. LBW represents low birth weight; NBW represents normal birth weight. The analytical sample size used for each health outcome is provided in the consort diagram (Supplementary Fig. 1).
Potential nonlinear association
The exposure-response relationship of components OC, NO3-, and NH4+ exhibited a monotonic increase up to a midrange concentration value, whereas the rest of the components, such as EC, soil, and others, showed an inverted U-shaped pattern for LBW (Supplementary Fig. 2). However, for anaemia (Supplementary Fig. 3), the majority of components, such as EC, NH4+, NO3-, OC, SO42-, and others, showed a monotonic increase in the probability of anaemia prevalence with an increase in pollutant exposure. In contrast, for soil, the trend line witnessed a fall. The nonlinear association between the probability of anaemia prevalence increased with increasing PM2.5 exposure. Similarly, varying nonlinear patterns were observed for ARI (Supplementary Fig. 4).
Cumulative effects
The cumulative effects of PM2.5 components on respective child health endpoints were estimated by summing over individual component-specific estimates of regression coefficients (‘Methods’) adjusted to their respective mass fraction. The cumulative regression coefficient was defined as
where, \({m}_{i}\) was the mass fractions and \({\hat{\beta }}_{i}\) was the estimated regression coefficient for ith component. The standard error of \({\hat{\beta }}_{{cum}}\) was estimated by \(V({\hat{\beta }}_{{cum}})=\mathop{\sum }\nolimits_{i=1}^{k}{m}_{i}^{2}V({\hat{\beta }}_{i})\) assuming independence among regression coefficients of individual components.
The cumulative OR of PM2.5 components for 10 µg m−3 increase in PM2.5 mass was estimated as 1.23 (1.21–1.26) for LBW, 1.49 (1.45–1.52) for anaemia and 1.35 (1.29–1.41) for ARI, while for every 10 µg m−3 increase in PM2.5 mass, ORs were estimated as 1.05 (1.04–1.06), 1.10 (1.09–1.11), and 1.11 (1.08–1.13) for LBW, anaemia, and ARI, respectively.
Expected health benefits of meeting clean air targets
The national ambient air quality standard (NAAQS) for annual PM2.5 was set at 40 μg m−3 in 2009 by the Government of India21. We examined the expected health benefits of meeting the NAAQS (Fig. 5b, e, h) and eventually the WHO-AQG (Fig. 5c, f, i) based on the indigenous exposure-response functions. We first estimated the expected reduction in ambient PM2.5 exposure (\(\triangle\)PM2.5) at the district level if India successfully meets the NAAQS and then the WHO-AQG relative to the current exposure level. Then, we calculated the attributable fraction (AF) as follows:
where \({{{{{{\rm{RR}}}}}}}=\exp (\log ({{{{{{\rm{OR}}}}}}})\times \triangle {{{{{{{\rm{PM}}}}}}}}_{2.5})\), and OR is the estimated odds ratio for each unit increase of PM2.5 exposure reported in previous subsection (ORs were converted for unit increase of PM2.5). Finally, we calculated the expected reduction in district-level prevalence (E) for LBW, anaemia, and ARI due to the reduction in PM2.5 exposure as:
a Low birth weight prevalence (%) across Indian districts, b low birth weight prevalence (%) after NAAQS implementation, c low Birth weight prevalence (%) after next air quality standards implementation; d anaemia prevalence (%) across Indian districts, e anaemia prevalence (%) after NAAQS implementation, f anaemia prevalence (%) after next air quality standards implementation; g ARI prevalence (%) across Indian districts, h ARI prevalence (%) after NAAQS implementation, i ARI prevalence (%) after next air quality standards implementation.
While we consider OR for elevation of PM2.5 mass (i.e., 1.005, 1.01 and 1.011 for LBW, anaemia and ARI, respectively) the overall LBW prevalence could reduce from 16.6% (16.4, 16.7) to 14.5% (14.1, 14.9) if the NAAQS level is achieved. If the exposure is reduced to the WHO-AQG level, the LBW prevalence could reduce to 11.6% (11.1, 12.4). For anaemia, the prevalence could reduce from 56.8% (56.6, 57.1) to 44.8% (43.8, 45.7) and further to 32.9% (32.1, 33.6), respectively, while for ARI, the prevalence could reduce from 2.8% (2.7, 2.9) to 2.1% (1.9, 2.3) and further to 1.5% (1.3, 1.6) if the NAAQS and WHO-AQG levels are achieved.
While we consider cumulative OR for elevation of PM2.5 components (i.e., 1.021, 1.041 and 1.03 for LBW, anaemia and ARI, respectively, the overall LBW prevalence could reduce from 16.6% (16.4, 16.7) to 15.7% (15.3, 16.1) if the NAAQS level is achieved. If the exposure is reduced to the WHO-AQG level, the LBW prevalence could reduce to 14.7% (14.3, 15.09). For anaemia, the prevalence could reduce from 56.8% (56.6, 57.1) to 50.7% (49.7, 51.8) and further to 44.2% (43.3, 45.1), respectively, while for ARI, the prevalence could reduce from 2.8% (2.7, 2.9) to 2.3% (2.1, 2.7) and further to 2.1% (1.8, 2.5) if the NAAQS and WHO-AQG levels are achieved.
Discussion
In this study, we present, to our knowledge, the first comprehensive assessment of the effects of PM2.5 and its components, as well as contributing sectors, on three specific U5 children health outcomes in India. We chose LBW, anaemia, and ARI to represent the health burden of U5 children because these are common public health morbidities reported in India, have pathophysiological frameworks that include air pollution, and occur in disparate frameworks of time or organ systems. PM2.5 is a mixture made up of various components with different sources and toxicities. Each source may produce different PM2.5 components (either in primary form or secondary precursors), and each component of PM2.5 may likewise come from various sources. Our findings suggest that the major health risk was posed by exposure to NO3-, NH4+, EC, and OC. However, other components also indicated a consistent risk to child health. Furthermore, we analysed the impact of sectoral PM2.5 on all three child health outcomes. The PM2.5 exposure attributable to the sectoral emissions from road dust, transport, industry, agriculture, domestic, and others, as well as international sources, depicted adverse effects on at least one health endpoint (see Fig. 2). The estimated varying impacts of different PM2.5 components, as well as those attributable to sectoral emission, can be considered as the direct effects of each component on health, as when estimating the effect for one component, the covariation of the other components with health was adjusted indirectly by the combination of Stage-1 and Stage-2 models.
The estimate of the effects of PM2.5 on LBW was quite similar to the estimates observed in the current literature22,23. Sun et al.23 observed significant effects of specific PM2.5 components, including potassium, zinc, nickel, titanium, elemental carbon, silicon, and ammonium, to be more harmful than aggregated PM2.5. Some studies have reported a significant positive association between anaemia and PM2.5 among U5 children, but not much has been reported with PM2.5 constituents16,17. Several studies have reported adverse effects of PM2.5 on either occurrence or frequency of ARI in U5 children, but none have assessed the impact of different PM components to understand their true cumulative impact24,25. The true impact of every 10 µg m−3 increase in PM2.5, which was an additive effect of PM2.5 chemical components (cumulative effect), was observed to be considerably high (ORs: 1.23 for LBW, 1.49 for anaemia, and 1.35 for ARI) as compared to the estimated effects by total PM2.5 mass (ORs: 1.05 for LBW, 1.10 for anaemia, and 1.11 for ARI). Therefore, the total PM2.5 mass, considered as the key surrogate marker for air pollution exposure, could substantially underestimate the true composite effect of different components of PM2.5.
There is a sufficiently large evidence base that the association of PM2.5 and its components with LBW is possibly causal. It is known that PM2.5 components can translocate into and cross the placental barrier and can induce oxidative stress that can cause placental changes26. Oxidative stress and placental inflammation may impair transplacental nutrient and oxygen exchange in the placenta, preventing enough nutrients and oxygen from reaching the foetus at the right time during gestation and impacting foetal growth27,28. Similarly, in U5 children, the continuous exposure of the lung to pro-oxidants through PM2.5 or its components causes oxidative stress leading to prolonged inflammation and lowered immunity, which is a common physiological pathway for vulnerability to bacterial and viral infections29,30. The causality of anaemia through PM2.5 or its components is probably linked to chronic inflammation. The secretion of inflammatory cytokines like interleukin-6 will signal the liver to secrete hepcidin, which reduces the absorption of dietary iron31. It does so by binding to ferroprotein, the cellular transmembrane iron-exporter, which prevents the internalization of dietary iron from the intestinal epithelium, as well as the recycling of iron within the body by macrophages. These events together reduce the amount of iron available for Hb synthesis. Equally, erythropoiesis can be independently reduced by the inflammatory cytokines32.
Our results contribute to the sparse body of evidence about the impact of PM2.5 components on health, particularly in LMICs, and show that the risk assessment purely based on PM2.5 mass may significantly understate the impact of some of its more dangerous components. These findings call for additional laboratory research to completely comprehend the biological mechanisms through which the diverse PM2.5 components affect human health. There are several limitations of this study. First, we assumed that the child’s residence did not change during the early life exposure period. Second, we considered the mass fractions of each species and sectoral PM2.5 from the model to be representative of the entire exposure duration. We combined this model data with satellite-derived PM2.5 (see ‘Methods’) to get the estimates of the required duration covering gestational and early life exposures. The exposure-response curves were observed to be mostly nonlinear and non-monotonic, unadjusted confounding could be one of the causes. The true causes of the nonlinearity could be difficult to explain from this study based on a cross sectional national survey with a cluster level air pollution exposure. Therefore, the magnitude of the varying effects may require further validation with well-planned cohorts.
An additional aspect of our study is that it provides information on the benefits of meeting clean air targets on child health. The analysis implies that with continued efforts towards mitigating ambient air pollution, the health burden among the children population can be reduced. In fact, meeting the NAAQS would take the anaemia burden closer to the ‘anaemia-free India’ mission target (reducing the prevalence to 40%) of the Government. The sectoral analysis that we presented will be useful for policymakers. For example, the residential and industrial sectors were the major contributors to ambient PM2.5, with shares of 41% and 37%, respectively, followed by agricultural residue burning (8%), other sectors (7%), transport (3%), and power (2.6%) (Supplementary Fig. S5)33. Accelerating the supply of clean energy for household activities through the Pradhan Mantri Ujjwala Yojana scheme, imposing stricter emission norms and gradual transition to clean energy usage in the industries, efficiently managing open burning are expected to provide a greater health benefit to the children. We note that the modelled mass fractions of individual species may have some uncertainties depending on the representativeness of emission inventory, which was also highlighted in the literature33. Nonetheless, this will not alter the broad conclusion of the study that the cumulative impact of PM2.5 components is greater than the impact of PM2.5 mass on child health in India.
To summarize, in a first-of-its-kind study, we demonstrated a significant association between components and sectors contributing to PM2.5 with LBW, anaemia, and ARI among U5 children in India. Our study further showed that the children born with LBW are more highly impacted due to PM2.5 components exposure than the children born with normal birth weight. We recommend further epidemiological and toxicological studies to understand the biological pathways that drive the linkage between air pollution and its causal effects and use these data in driving clean air actions.
Methods
Health data
The health dataset was obtained from Demographic Health Survey (DHS) version seven https://www.dhsprogram.com/data/available-datasets.cfm, which provides national-level health data for India as the NFHS-434. NFHS-4 was a household survey conducted between 20 January 2015 and 4 December 2016 across all 640 districts of India. The survey data provided the necessary information on health and family welfare, along with details on current threats in these areas, to aid policies and programmes in India’s health sector over time. Information on socioeconomic status, reproductive health and family planning, maternal and child health, breastfeeding and nutrition, vaccination coverage, anaemia, and the symptoms of ARI were collected in the survey.
The NFHS-4 sample was a two-stage stratified sample. The sampling frame for the selection of Primary Sampling Units (PSU) was the 2011 census. PSUs in rural areas were villages, and Census Enumeration Blocks (CEBs) were in urban areas. PSUs with less than 40 households were combined with the closest PSU. Probability Proportional to Size (PPS) sampling was used to select the final PSUs. Selected PSUs with more than 300 households were divided into segments of 100–150 households, and two segments were selected at random with probability proportional to segment size. In the second stage, 22 households were selected from each rural and urban cluster using systematic sampling. Data collection was carried out using various questionnaires. The survey included four questionnaires—a household questionnaire, a woman’s questionnaire, a man’s questionnaire, and a biomarker questionnaire. More detailed information on the sample design and selection is available on the International Institute of Population Sciences National Family and Health Survey-4 Report34.
Ambient PM2.5 exposure data
Our primary exposure metric was ambient PM2.5 exposure. Monthly average PM2.5 concentrations at PSU level were used to construct long-term exposure for three different health outcomes. For low birth weight, the average of monthly PM2.5 ambient concentrations at the PSU during the pregnancy with number of months being derived based on individual gestational age was considered as pregnancy period exposure. For anaemia and ARI, the PM2.5 exposure was derived by averaging monthly ambient PM2.5 concentration at the PSU over the period of individual life course. We therefore, estimated the exposure throughout the gestational period and life course of U5 children across all 636 districts from the national PM2.5 database created at a 1 km × 1 km spatial scale for India35. This database was created by converting MODIS-MAIAC aerosol optical depth to surface PM2.5 using a dynamic scaling factor from MERRA-2 reanalysis data. The instantaneous PM2.5 (representing the satellite overpass time) was then converted to a 24-h average using the diurnal scaling factor from MERRA-2. Both these scaling factors were calibrated against the data from the existing ground-based network of the Central Pollution Control Board of India (CPCB). At the annual scale, satellite-derived PM2.5 concentration showed a correlation coefficient of 0.97, and a root mean square error of 7.2 µg m−3 with the coincident ground-based measurements from the CPCB network. The Individual level exposure to ambient PM2.5 was calculated by clustering the exposure using geocode information of each PSU in the NFHS-4 data.
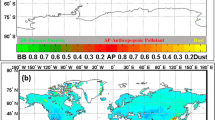
PM2.5 composition
Satellite data cannot provide direct information on PM2.5 composition, and very sparse ground measurements are available in India, that too for a very limited duration. Therefore, we integrated satellite-PM2.5 data with outputs from a published study which employed WRF version 3.9.1-CMAQ version 5.3.1 setup to simulate ambient PM2.5 concentrations at 36 × 36 km2 spatial resolution with 25 vertical levels33. The modelling set-up (Supplementary Table 3) employed ERA5 meteorology and emissions estimated using Greenhouse Gas and Air Pollution Interactions and Synergies (GAINS)-ASIA model (https://gains.iiasa.ac.at) in which government reported energy consumption data for the different sectors was used as an input for the year 2016. ECLIPSE (version 5) database of IIASA (2014) had been used for the national ammonia emissions, ship emissions, and the emissions emitted from the neighbouring countries which fall within the study domain that, includes Bhutan, Nepal, Myanmar, Bangladesh, Sri Lanka, Pakistan, and parts of China and Afghanistan. In addition, transboundary pollutants coming from outside the study domain were taken from boundary conditions developed by the Community Atmosphere Model with Chemistry (CAM-chem) model (https://www.acom.ucar.edu/cam-chem/cam-chem.shtml). The ambient PM2.5 simulated concentrations showed a significant agreement for the coefficient of determination when compared with the observed concentrations at ground-based monitoring stations33. The coefficient of determination between the observed versus simulated monthly averaged concentrations was found to be 0.81, while the index of agreement was 0.94.
We estimated the mass concentrations of each PM2.5 component (Mi) as
where Mi,model and PM2.5,model are the mass of component ‘i’ and total PM2.5 mass derived from the model and PM2.5,satellite is the satellite-derived PM2.5. Since the model estimates were available at 36 km \(\times\) 36 km resolution, we bilinearly re-gridded the model data to 1 km × 1 km to match its resolution with the satellite-based PM2.5 dataset resolution. Once the gridded mass concentrations of each component were estimated, we calculated the exposure for the NFHS clusters.
Sectoral contribution to PM2.5
The sectoral contributions to annual PM2.5 were estimated by the subtraction method in the modelling framework. First, the control simulation was carried out with all sectoral emissions on, and then in each subsequent simulation, emissions from a particular sector were switched off, and the difference provided the contribution from that sector. The model outputs33 were analysed to derive PM2.5 contributions of the transport, small and medium-scale industries, brick industry, major industries, power, domestic (due to solid fuel used for cooking and heating), agriculture residue burning, construction, road dust, and others (which includes refuse burning, construction, crematoria, NH3, biogenic emissions, refineries, and evaporative non-methane volatile organic compounds). Here we used these model outputs and combined them with satellite-PM2.5 following the method explained in the previous section (for PM2.5 components) to estimate the exposure to a specific sectoral PM2.5 for the NFHS clusters.
Outcome data
For U5 children, the primary health outcomes considered in this study were LBW, anaemia, and ARI. For LBW, the NFHS-4 recorded birth weight from either written records or the mother’s oral report. LBW was defined by the WHO as a birth weight <2500 g36. Children with LBW were coded as 1, whereas the children with birth weight greater than 2500 g were coded as 0.
Information on anaemia prevalence among U5 children was obtained from NFHS-4, which used the finger or heel prick method to collect blood samples. Haemoglobin concentrations were measured on-site using the HemoCue Hb 201+ analyzer37. Children with haemoglobin levels <11 g/dL were considered anaemic, and children with haemoglobin levels >11 g/dL were considered non-anaemic38. These were coded as 1 and 0, respectively.
ARI in U5 children was diagnosed by the reporting of symptoms like cough, accompanied by short rapid breathing and/or difficulty in breathing that was thought to be chest related. The interviewer asked mothers whether their children experienced any ARI symptoms in the two weeks preceding the survey. ARI was used as a dichotomous variable with the presence of ARI symptoms coded as 1 and the absence of ARI symptoms coded as 0.
Covariates
Several individual-level and household-level variables were identified as potential covariates of LBW39,40, anaemia41 and ARI42. These variables were included in the analysis based on their significance with the respective health outcome. The following individual-level variables were considered for all three outcome variables: sex of the child (male or female), mother’s education (no education, primary, secondary, and higher), and parity (1, or >1). In addition, for the outcome variable ARI, we accounted for the age of the child, for LBW, mother’s age (<20, 20–35, >35) and body mass index (BMI) of the mother (underweight, normal weight, overweight and obesity), lastly, for anaemia, maternal haemoglobin levels, and per capita iron intake. Daily dietary iron intake (per capita) was obtained by converting monthly food purchases captured by the 9th quinquennial Household Consumer Expenditure survey of the 68th round of the NSSO43 which was further triangulated with NFHS-4 by Swaminathan et al.44. Household-level covariates used for both ARI and anaemia were the following: socioeconomic status, which is classified into five wealth quintiles (poorest, poor, middle, rich, and richest), type of residence (rural or urban), and passive smoking (yes or no). Since studies have shown that ambient20 and household36 air pollution are associated with anaemia, we also included the type of cooking fuel in the household as a covariate. This was classified as clean fuel (electricity, LPG/natural gas, biogas), solid fuel (coal/lignite, charcoal, wood, straw/shrubs/grass, agricultural crop waste, and dung cakes), kerosene, and others. For LBW, only the wealth index was used as the household-level covariate.
Statistical analysis
Gestational period exposure was associated with LBW, and life course exposure was associated with ARI and anaemia. PSU level ambient concentration was assigned as the exposure to air pollutants for children residing within the PSU. To account for this cluster effect, we used a logistic mixed effects regression model. We also wanted to estimate the direct effects of all PM2.5 components adjusted for other covariates. Owing to high collinearity among the PM2.5 components, we used a two-stage model to avoid potential multi-collinearity. In the first step, we regressed PM2.5 mass concentration on each component at a time and extracted the residuals as an alternative metric that can capture the total variability of PM2.5 except variability explained by the component. These PM2.5-residuals were then adjusted in the second stage logistic mixed model.
Stage-I:
Stage-II:
Where \({\hat{\delta }}_{0}\) and \({\hat{\delta }}_{1}\) were the estimates of intercept and slope from the first stage model. \({Y}_{{ij}}\) represented the binary outcome (anaemia/LBW/ARI) for the jth individual in ith PSU, Pi was one of the PM2.5 components, (ResPM2.5)i was the residuals at ith PSU, ui was a random intercept corresponding to ith PSU with \({u}_{i}\sim N\left(0,{\sigma }_{{{{{{\rm{u}}}}}}}^{2}\right)\) and \(\gamma {\left({{{{{{\rm{confounders}}}}}}}\right)}_{{ij}}\) represents the linear terms for all confounders adjusted.
Further, the estimates of PM2.5 components on anaemia and ARI were stratified by birth weight status (LBW vs. Normal) using an interaction component of LBW with the component in 2nd stage model. Stratified analysis was performed by adding an interaction term to the stage-II model. Potential nonlinear associations of pollutants on health outcomes were explored by replacing Pi with a penalized cubic smoothing spline function of Pi [i.e., \(f({P}_{i})\)] in the stage-II model.
To compare PM2.5 components specific estimate against the effects estimate for elevation of whole PM2.5 mass we also estimated adjusted OR of PM2.5 mass for LBW, anaemia and ARI by cluster-logistic regression, cluster being the PSU.
R version 4.1.2 (R Core Team, 2022 Vienna, Austria)45 was used for all statistical analyses.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The Demographic Health Survey data used in this study can be accessed through a restricted access system in accordance with the data access guidelines of the DHS programme. To obtain access, a request should be submitted after registering on the DHS website at the following link: https://dhsprogram.com/data/Using-Datasets-for-Analysis.cfm. Source data are provided as a Source data file and have also been deposited in figshare under accession code https://doi.org/10.6084/m9.figshare.2351375746. Exposure datasets used in this study can be accessed using the same figshare accession code. Source data are provided with this paper.
Code availability
R codes for the statistical models in the main text are available at https://doi.org/10.6084/m9.figshare.23513757. R codes for data processing techniques are available on request from the corresponding authors.
References
Global Health Impacts of Air Pollution | State of Global Air. https://www.stateofglobalair.org (2020).
Health Effects Institute. 2019. State of Global Air 2019. https://www.stateofglobalair.org/sites/default/files/soga_2019_report (2019).
Cohen, A. J. et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet 389, 1907–1918 (2017).
Balakrishnan, K. et al. The impact of air pollution on deaths, disease burden, and life expectancy across the states of India: the Global Burden of Disease Study 2017. Lancet Planet. Health 3, e26–e39 (2019).
Balakrishnan, K., Cohen, A. & Smith, K. R. Addressing the burden of disease attributable to air pollution in India: the need to integrate across household and ambient air pollution exposures. Environ. Health Perspect. 122, A6–A7 (2014).
Lelieveld, J., Haines, A. & Pozzer, A. Age-dependent health risk from ambient air pollution: a modelling and data analysis of childhood mortality in middle-income and low-income countries. Lancet Planet. Health 2, e292–e300 (2018).
Singh, P., Dey, S., Chowdhury, S. & Bali, K. Early Life Exposure to Outdoor Air Pollution: Effect on Child Health in India (2019).
Mishra, V., Smith, K. R. & Retherford, R. D. Effects of cooking smoke and environmental tobacco smoke on acute respiratory infections in young Indian children. Popul. Environ. 26, 375–396 (2005).
World Health Organization. World Health Statistics 2019: Monitoring Health for the SDGs, Sustainable Development Goals. https://apps.who.int/iris/bitstream/handle/10665/324835/9789241565707-eng (2019).
Goyal, N. & Canning, D. The association of in-utero exposure to ambient fine particulate air pollution with low birth weight in India. Environ. Res. Lett. 16, 054034 (2021).
Pope, D. P. et al. Risk of low birth weight and stillbirth associated with indoor air pollution from solid fuel use in developing countries. Epidemiol. Rev. 32, 70–81 (2010).
Karimi, B. & Shokrinezhad, B. Air pollution and mortality among infant and children under five years: a systematic review and meta-analysis. Atmos. Pollut. Res. 11, 61–70 (2020).
Klepac, P., Locatelli, I., Korošec, S., Künzli, N. & Kukec, A. Ambient air pollution and pregnancy outcomes: a comprehensive review and identification of environmental public health challenges. Environ. Res. 167, 144–159 (2018).
Wang, L. et al. Association between early prenatal exposure to ambient air pollution and birth defects: evidence from newborns in Xi’an, China. J. Public Health 41, 494–501 (2019).
Spears, D. et al. The association of early-life exposure to ambient PM2.5 and later-childhood height-for-age in India: an observational study. Environ. Health 18, 62 (2019).
Mehta, U. et al. The association between ambient PM2.5 exposure and anemia outcomes among children under five years of age in India. Environ. Epidemiol. 5, e125 (2021).
Amegbor, P. M. Early-life environmental exposures and anaemia among children under age five in Sub-Saharan Africa: an insight from the Demographic & Health Surveys. Sci. Total Environ. 832, 154957 (2022).
World Health Organization. Air Polution and Child Health: Prescibing Clean Air (2018).
Joshi, P., Dey, S., Ghosh, S., Jain, S. & Sharma, S. K. Association between acute exposure to PM2.5 chemical species and mortality in megacity Delhi, India. Environ. Sci. Technol. 56, 7275–7287 (2022).
Chaudhary, E. et al. Reducing the burden of anaemia in Indian women of reproductive age with clean-air targets. Nat. Sustain. 1–8, https://doi.org/10.1038/s41893-022-00944-2 (2022).
Central Pollution Control Board (CPCB), Ministry of Environment, Forests and Climate Change (MoEF&CC), Government of India. National Ambient Air Quality Standards (2009).
Kirwa, K. et al. Low birth weight and PM2.5 in Puerto Rico. Environ. Epidemiol. 3, e058 (2019).
Sun, X. et al. The associations between birth weight and exposure to fine particulate matter (PM2.5) and its chemical constituents during pregnancy: a meta-analysis. Environ. Pollut. 211, 38–47 (2016).
Larson, P. S. et al. Long-term PM2.5 exposure is associated with symptoms of acute respiratory infections among children under five years of age in Kenya, 2014. Int. J. Environ. Res. Public Health 19, 1–20 (2022).
Davila Cordova, J. E. et al. Association of PM2.5 concentration with health center outpatient visits for respiratory diseases of children under 5 years old in Lima, Peru. Environ. Health.: A Glob. Access Sci. Source 19, 1–6 (2020).
Ruano, C. S. M., Miralles, F., Méhats, C. & Vaiman, D. The impact of oxidative stress of environmental origin on the onset of placental diseases. Antioxidants 11, 106 (2022).
Saenen, N. D. et al. Air pollution-induced placental alterations: an interplay of oxidative stress, epigenetics, and the aging phenotype? Clin. Epigenetics 11, 124 (2019).
Li, Z. et al. Impact of ambient PM2.5 on adverse birth outcome and potential molecular mechanism. Ecotoxicol. Environ. Saf. 169, 248–254 (2019).
Garçon, G. et al. Dunkerque City air pollution particulate matter-induced cytotoxicity, oxidative stress and inflammation in human epithelial lung cells (L132) in culture. Toxicol. Vitr. 20, 519–528 (2006).
Das, A., Habib, G., Vivekanandan, P. & Kumar, A. Reactive oxygen species production and inflammatory effects of ambient PM2.5 -associated metals on human lung epithelial A549 cells “one year-long study”: the Delhi chapter. Chemosphere 262, 128305 (2021).
Pagani, A., Nai, A., Silvestri, L. & Camaschella, C. Hepcidin and anemia: a tight relationship. Front. Physiol. 10, 1294 (2019).
Morceau, F., Dicato, M. & Diederich, M. Pro-inflammatory cytokine-mediated anemia: regarding molecular mechanisms of erythropoiesis. Mediators Inflamm. 2009, 1–11 (2009).
Singh, N., Agarwal, S., Sharma, S., Chatani, S. & Ramanathan, V. Air pollution over India: causal factors for the high pollution with implications for mitigation. ACS Earth Space Chem. https://doi.org/10.1021/acsearthspacechem.1c00170 (2021).
International Institute for Population Sciences (IIPS). National Family Health Survey (NFHS-4), 2015–16. https://dhsprogram.com/pubs/pdf/FR339/FR339.pdf (International Institute for Population Sciences (IIPS) and ICF, 2017).
Dey, S. et al. A satellite-based high-resolution (1-km) ambient PM2.5 database for India over two decades (2000–2019): applications for air quality management. Remote Sens. 12, 3872 (2020).
Global nutrition targets 2025: policy brief series. https://iris.who.int/bitstream/handle/10665/149018/WHO_NMH_NHD_14.2_eng.pdf?sequence=1 (2014).
Sanchis-Gomar, F., Cortell-Ballester, J., Pareja-Galeano, H., Banfi, G. & Lippi, G. Hemoglobin point-of-care testing: the HemoCue System. J. Lab Autom. 18, 198–205 (2013).
WHO. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity. https://iris.who.int/bitstream/handle/10665/85839/WHO_NMH_NHD_MNM_11.1_eng.pdf?sequence=22 (2011).
Khan, N., Mozumdar, A. & Kaur, S. Determinants of low birth weight in India: an investigation from the National Family Health Survey. Am. J. Hum. Biol. 32, e23355 (2020).
Girotra, S., Mohan, N., Malik, M., Roy, S. & Basu, S. Prevalence and Determinants of Low Birth Weight in India: findings from a Nationally Representative Cross-Sectional Survey (2019-21). Cureus 15, e36717 (2023).
Onyeneho, N. G., Ozumba, B. C. & Subramanian, S. V. Determinants of childhood anemia in India. Sci. Rep. 9, 16540 (2019).
Varghese, J. S. & Muhammad, T. Prevalence, potential determinants, and treatment-seeking behavior of acute respiratory infection among children under age five in India: Findings from the National Family Health Survey, 2019-21. BMC Pulm. Med. 23, 195 (2023).
National Sample Survey Office. Nutritional Intake in India, 2011–12. 560, NSS 68th round. National Statistical Organization. Government of India (2014).
Swaminathan, S. et al. Dietary iron intake and anemia are weakly associated, limiting effective iron fortification strategies in India. J. Nutr. 149, 831–839 (2019).
R Core Team. The R Project for Statistical Computing, Vienna, Austria, https://www.R-project.org/ (2022).
Chaudhary, E. Child Health Outcome codes and dataset. Figshare, Dataset, https://doi.org/10.6084/m9.figshare.23513757, (2023).
Acknowledgements
The work is supported by a research grant under the SUPRA scheme from the SERB, Department of Science and Technology, GoI (SPR/2020/000212). The exposure database was generated as part of a project under the NCAP funded by the Ministry of Environment, Forest and Climate Change, GoI. S.D. acknowledges financial support for the Institute Chair fellowship and DST-FIST programme (SR/FST/ESII-016/2014) for computing support.
Author information
Authors and Affiliations
Contributions
E.C., F.G., S.D. and S.G. conceived the study and wrote the initial draft of the article. E.C., F.G. and A.S. analysed the data with the help of S.G. and S.D. S.S., N.S. and S.A. did the model simulations and analysis of the model outputs. A.V.K. and T.T. helped to review the potential causal pathways of the observed association. U.M. provided essential advice about the anaemia outcome. All authors provided comments and contributed to give the final shape of the article.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Hao Guo, Zafar Fatmi and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chaudhary, E., George, F., Saji, A. et al. Cumulative effect of PM2.5 components is larger than the effect of PM2.5 mass on child health in India. Nat Commun 14, 6955 (2023). https://doi.org/10.1038/s41467-023-42709-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-023-42709-1
This article is cited by
-
Some PM2.5 components more harmful to children’s health than others
Nature India (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.