Abstract
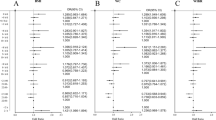
Evidence about the relationship between meal and sleep time and CVD in children is scarce. The aims of this study were to describe the association between life rhythm patterns and blood pressure in children. This research was conducted among 5,608 children aged 6 to 15 years old in Chongqing and Sichuan provinces in 2021 and 2022. Dietary and sleep rhythms information was collected. The time of the first meal and last meal, and sleep time, were obtained. The mean age was 10.48 ± 2.24 years old, with 2958 (52.75%) male participants. The mean feeding window on weekdays was 11.69 h, 12.42 h, and 13.23 h for participants aged 6–7 years old, 8–12 years old and 13–15 years old, respectively. Weekday feeding window and last mealtime were positively correlated with blood pressure levels. And the changes in the feeding window between weekdays and weekends were significantly correlated with BP. Sleep duration and change in wake time were significantly correlated with SBP. Based on these results, this study identified the optimal combination of dietary and sleep rhythm interventions for children younger than 12 years of age and aged 12 and older, respectively. Disorder dietary and sleep rhythms disorders may correlate with elevated blood pressure levels, suggesting developing optimal dietary and sleep rhythm patterns could prevent the incidence of CVDs in children.

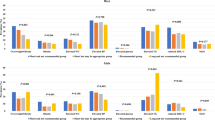
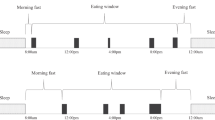
The optimal dietary rhythm was defined by the indexes of breakfast time, dinner time and daily feeding window. As good meal patterns are defined as satisfied the following three items: for children younger than 12 years should have breakfast after 7:30 am; aged 12 years and over should have breakfast after 7 am; having dinner before 6 pm; daily feeding window less than 12.5 h. And less optimal dietary rhythm should satisfy any condition or eat dinner between 6 pm and 8 pm; and poor dietary rhythm should not satisfy any of the three criteria and eat dinner after 8 pm. Children with optimal dietary rhythm (in group A) had lower SBP (P < 0.001), DBP (P = 0.002) and MAP (P < 0.001) than those in group C.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data are available from the corresponding author Xiaohua Liang (Email: xiaohualiang@hospital.cqmu.edu.cn, or liangxiaohua666@sina.com).
References
Kant AK, Graubard BI. 40-year trends in meal and snack eating behaviors of American adults. J Acad Nutr Diet. 2015;115:50–63. https://doi.org/10.1016/j.jand.2014.06.354.
Gupta NJ, Kumar V, Panda S. A camera-phone based study reveals erratic eating pattern and disrupted daily eating-fasting cycle among adults in India. Plos One. 2017;12:e172852. https://doi.org/10.1371/journal.pone.0172852.
Ha K, Song Y. Associations of meal timing and frequency with obesity and metabolic syndrome among Korean adults. Nutrients. 2019;11. https://doi.org/10.3390/nu11102437.
Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–9. https://doi.org/10.1016/S0140-6736(99)01376-8.
Mesas AE, Jimenez-Lopez E, Martinez-Vizcaino V, Fernandez-Rodriguez R, Bizzozero-Peroni B, Garrido-Miguel M, et al. Are adherence to the Mediterranean diet and siesta individually or jointly associated with blood pressure in Spanish adolescents? Results from the EHDLA study. Front Public Health. 2022;10:934854. https://doi.org/10.3389/fpubh.2022.934854.
Pirojsakul K, Aekplakorn W, Siwarom S, Paksi W, Kessomboon P, Neelapaichit N, et al. Sleep duration and risk of high blood pressure in Thai adolescents: the Thai National Health Examination Survey V, 2014 (NHES-V). BMC Public Health. 2022;22:1983. https://doi.org/10.1186/s12889-022-14430-z.
Chang SW, Kang JW. Association between sleep time and blood pressure in Korean adolescents: cross-sectional analysis of KNHANES VII. Children-Basel. 2021;8. https://doi.org/10.3390/children8121202.
Gill S, Panda S. A smartphone app reveals erratic diurnal eating patterns in humans that can be modulated for health benefits. Cell Metab. 2015;22:789–98. https://doi.org/10.1016/j.cmet.2015.09.005.
St-Onge MP, Ard J, Baskin ML, Chiuve SE, Johnson HM, Kris-Etherton P, et al. Meal timing and frequency: implications for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation. 2017;135:e96–e121. https://doi.org/10.1161/CIR.0000000000000476.
Li C, Shang S, Liang W. Sleep and risk of hypertension in general American adults: the National Health and Nutrition Examination Surveys (2015–2018). J Hypertens. 2023;41:63–73. https://doi.org/10.1097/HJH.0000000000003299.
Sutton EF, Beyl R, Early KS, Cefalu WT, Ravussin E, Peterson CM. Early time-restricted feeding improves insulin sensitivity, blood pressure, and oxidative stress even without weight loss in men with prediabetes. Cell Metab. 2018;27:1212–21. https://doi.org/10.1016/j.cmet.2018.04.010.
Liang X, Chen J, An X, Liu F, Liang F, Tang X, et al. The impact of PM2.5 on children’s blood pressure growth curves: a prospective cohort study. Environ Int. 2022;158:107012 https://doi.org/10.1016/j.envint.2021.107012.
Fan H, Yan YK, Mi J. Updating blood pressure references for Chinese children aged 3–17 years. Chin J Hypertens. 2017;25:428–35.
Maffeis C, Provera S, Filippi L, Sidoti G, Schena S, Pinelli L, et al. Distribution of food intake as a risk factor for childhood obesity. Int J Obes Relat Metab Disord. 2000;24:75–80. https://doi.org/10.1038/sj.ijo.0801088.
Goetz AR, Jindal I, Moreno JP, Puyau MR, Adolph AL, Musaad S, et al. The role of sleep and eating patterns in adiposity gain among preschool-aged children. Am J Clin Nutr. 2022;116:1334–42. https://doi.org/10.1093/ajcn/nqac197.
Firouzi S, Poh BK, Ismail MN, Sadeghilar A. Sleep habits, food intake, and physical activity levels in normal and overweight and obese Malaysian children. Obes Res Clin Pract. 2014;8:e70–e78. https://doi.org/10.1016/j.orcp.2012.12.001.
Garaulet M, Ortega FB, Ruiz JR, Rey-Lopez JP, Beghin L, Manios Y, et al. Short sleep duration is associated with increased obesity markers in European adolescents: effect of physical activity and dietary habits. The HELENA study. Int J Obes. 2011;35:1308–17. https://doi.org/10.1038/ijo.2011.149.
Westerlund L, Ray C, Roos E. Associations between sleeping habits and food consumption patterns among 10-11-year-old children in Finland. Br J Nutr. 2009;102:1531–7. https://doi.org/10.1017/S0007114509990730.
Kjeldsen JS, Hjorth MF, Andersen R, Michaelsen KF, Tetens I, Astrup A, et al. Short sleep duration and large variability in sleep duration are independently associated with dietary risk factors for obesity in Danish school children. Int J Obes. 2014;38:32–39. https://doi.org/10.1038/ijo.2013.147.
Thivel D, Isacco L, Aucouturier J, Pereira B, Lazaar N, Ratel S, et al. Bedtime and sleep timing but not sleep duration are associated with eating habits in primary school children. J Dev Behav Pediatr. 2015;36:158–65. https://doi.org/10.1097/DBP.0000000000000131.
Spaeth AM, Hawley NL, Raynor HA, Jelalian E, Greer A, Crouter SE, et al. Sleep, energy balance, and meal timing in school-aged children. Sleep Med. 2019;60:139–44. https://doi.org/10.1016/j.sleep.2019.02.003.
Jansen EC, She R, Rukstalis M, Alexander GL. Changes in fruit and vegetable consumption in relation to changes in sleep characteristics over a 3-month period among young adults. Sleep Health. 2021;7:345–52. https://doi.org/10.1016/j.sleh.2021.02.005.
Moreno JP, Crowley SJ, Alfano CA, Hannay KM, Thompson D, Baranowski T. Potential circadian and circannual rhythm contributions to the obesity epidemic in elementary school age children. Int J Behav Nutr Phys Act. 2019;16:25. https://doi.org/10.1186/s12966-019-0784-7.
McHill AW, Phillips AJ, Czeisler CA, Keating L, Yee K, Barger LK, et al. Later circadian timing of food intake is associated with increased body fat. Am J Clin Nutr. 2017;106:1213–9. https://doi.org/10.3945/ajcn.117.161588.
Bray MS, Young ME. Circadian rhythms in the development of obesity: potential role for the circadian clock within the adipocyte. Obes Rev. 2007;8:169–81. https://doi.org/10.1111/j.1467-789X.2006.00277.x.
Bray MS, Young ME. Chronobiological effects on obesity. Curr Obes Rep. 2012;1:9–15. https://doi.org/10.1007/s13679-011-0005-4.
Coomans CP, Lucassen EA, Kooijman S, Fifel K, Deboer T, Rensen PC, et al. Plasticity of circadian clocks and consequences for metabolism. Diabetes Obes Metab. 2015;17:65–75. https://doi.org/10.1111/dom.12513.
Leung G, Huggins CE, Bonham MP. Effect of meal timing on postprandial glucose responses to a low glycemic index meal: A crossover trial in healthy volunteers. Clin Nutr. 2019;38:465–71. https://doi.org/10.1016/j.clnu.2017.11.010.
Tsuchida Y, Hata S, Sone Y. Effects of a late supper on digestion and the absorption of dietary carbohydrates in the following morning. J Physiol Anthropol. 2013;32:9. https://doi.org/10.1186/1880-6805-32-9.
Bo S, Fadda M, Castiglione A, Ciccone G, De Francesco A, Fedele D, et al. Is the timing of caloric intake associated with variation in diet-induced thermogenesis and in the metabolic pattern? A randomized cross-over study. Int J Obes. 2015;39:1689–95. https://doi.org/10.1038/ijo.2015.138.
McHill AW, Melanson EL, Higgins J, Connick E, Moehlman TM, Stothard ER, et al. Impact of circadian misalignment on energy metabolism during simulated nightshift work. P Natl Acad Sci USA. 2014;111:17302–7. https://doi.org/10.1073/pnas.1412021111.
Morris CJ, Garcia JI, Myers S, Yang JN, Trienekens N, Scheer FA. The human circadian system has a dominating role in causing the morning/evening difference in diet-induced thermogenesis. Obesity. 2015;23:2053–8. https://doi.org/10.1002/oby.21189.
Romon M, Edme JL, Boulenguez C, Lescroart JL, Frimat P. Circadian variation of diet-induced thermogenesis. Am J Clin Nutr. 1993;57:476–80. https://doi.org/10.1093/ajcn/57.4.476.
Matthews KA, Pantesco EJ. Sleep characteristics and cardiovascular risk in children and adolescents: an enumerative review. Sleep Med. 2016;18:36–49. https://doi.org/10.1016/j.sleep.2015.06.004.
Derks I, Kocevska D, Jaddoe V, Franco OH, Wake M, Tiemeier H, et al. Longitudinal associations of sleep duration in infancy and early childhood with body composition and cardiometabolic health at the age of 6 years: the generation R study. Child Obes. 2017;13:400–8. https://doi.org/10.1089/chi.2016.0341.
Carson V, Tremblay MS, Chaput JP, Chastin SF. Associations between sleep duration, sedentary time, physical activity, and health indicators among Canadian children and youth using compositional analyses. Appl Physiol Nutr Metab. 2016;41:S294–S302. https://doi.org/10.1139/apnm-2016-0026.
Navarro-Solera M, Carrasco-Luna J, Pin-Arboledas G, Gonzalez-Carrascosa R, Soriano JM, Codoner-Franch P. Short sleep duration is related to emerging cardiovascular risk factors in obese children. J Pediatr Gastroenterol Nutr. 2015;61:571–6. https://doi.org/10.1097/MPG.0000000000000868.
Paciencia I, Araujo J, Ramos E. Sleep duration and blood pressure: a longitudinal analysis from early to late adolescence. J Sleep Res. 2016;25:702–8. https://doi.org/10.1111/jsr.12433.
Morita N, Kambayashi I, Okuda T, Oda S, Takada S, Nakajima T, et al. Inverse relationship between sleep duration and cardio-ankle vascular index in children. J Atheroscler Thromb. 2017;24:819–26. https://doi.org/10.5551/jat.36517.
Orozco-Solis R, Sassone-Corsi P. Epigenetic control and the circadian clock: linking metabolism to neuronal responses. Neuroscience. 2014;264:76–87. https://doi.org/10.1016/j.neuroscience.2014.01.043.
Quist JS, Sjodin A, Chaput JP, Hjorth MF. Sleep and cardiometabolic risk in children and adolescents. Sleep Med Rev. 2016;29:76–100. https://doi.org/10.1016/j.smrv.2015.09.001.
Sparano S, Lauria F, Ahrens W, Fraterman A, Thumann B, Iacoviello L, et al. Sleep duration and blood pressure in children: analysis of the pan-European IDEFICS cohort. J Clin Hypertens. 2019;21:572–8. https://doi.org/10.1111/jch.13520.
Jiang W, Hu C, Li F, Hua X, Zhang X. Association between sleep duration and high blood pressure in adolescents: a systematic review and meta-analysis. Ann Hum Biol. 2018;45:457–62. https://doi.org/10.1080/03014460.2018.1535661.
Guo X, Zheng L, Li Y, Yu S, Liu S, Zhou X, et al. Association between sleep duration and hypertension among Chinese children and adolescents. Clin Cardiol. 2011;34:774–81. https://doi.org/10.1002/clc.20976.
Dos SE, De Souza OF. Association of sleep duration and blood pressure in adolescents: a multicenter study. Am J Hypertens. 2020;33:77–83. https://doi.org/10.1093/ajh/hpz129.
Lucas-de LCL, Martin-Espinosa N, Cavero-Redondo I, Gonzalez-Garcia A, Diez-Fernandez A, Martinez-Vizcaino V, et al. Sleep patterns and cardiometabolic risk in schoolchildren from Cuenca, Spain. Plos One. 2018;13:e191637. https://doi.org/10.1371/journal.pone.0191637.
Zhou M, Lalani C, Banda JA, Robinson TN. Sleep duration, timing, variability and measures of adiposity among 8- to 12-year-old children with obesity. Obes Sci Pr. 2018;4:535–44. https://doi.org/10.1002/osp4.303.
Jansen EC, Dunietz GL, Matos-Moreno A, Solano M, Lazcano-Ponce E, Sanchez-Zamorano LM. Bedtimes and blood pressure: a prospective cohort study of Mexican adolescents. Am J Hypertens. 2020;33:269–77. https://doi.org/10.1093/ajh/hpz191.
Carissimi A, Dresch F, Martins AC, Levandovski RM, Adan A, Natale V, et al. The influence of school time on sleep patterns of children and adolescents. Sleep Med. 2016;19:33–39. https://doi.org/10.1016/j.sleep.2015.09.024.
Mi SJ, Kelly NR, Brychta RJ, Grammer AC, Jaramillo M, Chen KY, et al. Associations of sleep patterns with metabolic syndrome indices, body composition, and energy intake in children and adolescents. Pediatr Obes. 2019;14:e12507. https://doi.org/10.1111/ijpo.12507.
Makarem N, Zuraikat FM, Aggarwal B, Jelic S, St-Onge MP. Variability in sleep patterns: an emerging risk factor for hypertension. Curr Hypertens Rep. 2020;22:19. https://doi.org/10.1007/s11906-020-1025-9.
Proper KI, van de Langenberg D, Rodenburg W, Vermeulen R, van der Beek AJ, van Steeg H, et al. The relationship between shift work and metabolic risk factors: a systematic review of longitudinal studies. Am J Prev Med. 2016;50:e147–e157. https://doi.org/10.1016/j.amepre.2015.11.013.
Gupta N, Maranda L, Gupta R. Differences in self-reported weekend catch up sleep between children and adolescents with and without primary hypertension. Clin Hypertens. 2018;24:7 https://doi.org/10.1186/s40885-018-0092-6.
Gong QH, Li SX, Wang SJ, Li H. Dinner-to-bed time is independently associated with overweight/obesity in Chinese school-aged children. Eat Weight Disord. 2021;26:2657–63. https://doi.org/10.1007/s40519-021-01129-0.
Yoshida J, Eguchi E, Nagaoka K, Ito T, Ogino K. Association of night eating habits with metabolic syndrome and its components: a longitudinal study. BMC Public Health. 2018;18:1366. https://doi.org/10.1186/s12889-018-6262-3.
Xiao Q, Garaulet M, Scheer F. Meal timing and obesity: interactions with macronutrient intake and chronotype. Int J Obes. 2019;43:1701–11. https://doi.org/10.1038/s41366-018-0284-x.
Berg C, Lappas G, Wolk A, Strandhagen E, Toren K, Rosengren A, et al. Eating patterns and portion size associated with obesity in a Swedish population. Appetite. 2009;52:21–26. https://doi.org/10.1016/j.appet.2008.07.008.
Green MB, Beckman M. Obesity and hypertension. N Y State J Med. 1948;48:1250–3.
Ayer JG, Harmer JA, David C, Steinbeck KS, Seale JP, Celermajer DS. Severe obesity is associated with impaired arterial smooth muscle function in young adults. Obesity. 2011;19:54–60. https://doi.org/10.1038/oby.2010.114.
Morris CJ, Purvis TE, Hu K, Scheer FA. Circadian misalignment increases cardiovascular disease risk factors in humans. Proc Natl Acad Sci USA. 2016;113:E1402–11. https://doi.org/10.1073/pnas.1516953113.
Leproult R, Holmback U, Van Cauter E. Circadian misalignment augments markers of insulin resistance and inflammation, independently of sleep loss. Diabetes. 2014;63:1860–9. https://doi.org/10.2337/db13-1546.
Wright KJ, Drake AL, Frey DJ, Fleshner M, Desouza CA, Gronfier C, et al. Influence of sleep deprivation and circadian misalignment on cortisol, inflammatory markers, and cytokine balance. Brain Behav Immun. 2015;47:24–34. https://doi.org/10.1016/j.bbi.2015.01.004.
Barrows IR, Ramezani A, Raj DS. Inflammation, immunity, and oxidative stress in hypertension-partners in crime? Adv Chronic Kidney Dis. 2019;26:122–30. https://doi.org/10.1053/j.ackd.2019.03.001.
Acknowledgements
The authors would like to acknowledge all of the staff members of the 6 elementary schools in the two provinces.
Funding
This work was supported by the Major Health Project of Chongqing Science and Technology Bureau (No. CSTC2021jscx-gksb-N0001), Program for Youth Innovation in Future Medicine from Chongqing Medical University (No.W0088), National key research and development project (No.2017YFC0211705), Intelligent Medicine Project (No.ZHYX202109), the Basic Research Project of Key Laboratory of Ministry of Education of China in 2021(GBRP-202106), Joint Medical Research Project of Chongqing Municipal Health Commission and Chongqing Science and Technology Bureau (No.2020MSXM062), the Technology Foresight and Institutional Innovation Project of Chongqing Science and Technology Bureau (No.cstc2020jsyj-zzysbAX0016), the Natural Science Foundation Project (No.81502826, 82373590), the Education Commission of Chongqing Municipality (No.KJQN201900443). The funders had no role in the whole study research process, including study design, the data collection and analysis, the decision to publish, or the preparation of the manuscript
Author information
Authors and Affiliations
Contributions
XH: conceptualization, methodology, writing - review & editing; YL, QL, and LH: investigation, supervision; FM, YB,and ZL: validation, resources; XH, YL, QL, and LH: writing – original draft, writing - review & editing; XH: writing - review & editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Consent to publish
All of the authors reviewed and approved the publication of this paper
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liang, X., He, X., Liu, Q. et al. The impact of dietary and sleep rhythms on blood pressure in children and adolescents: a cross-sectional study. Hypertens Res 47, 649–662 (2024). https://doi.org/10.1038/s41440-023-01493-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01493-7
Keywords
This article is cited by
-
Preface-various factors in the management of blood pressure
Hypertension Research (2024)