Abstract
Background
The relationship of insufficient sleep with the increased risk of obesity has been reported, but less is known about other sleep dimensions in the sleep-obesity associations.
Objectives
To assess the associations of multiple sleep dimensions with overall and abdominal obesity among Chinese students.
Methods
This was a cross-sectional study involving 10,686 Han students aged 9–18 from Chinese National Survey on Students’ Constitution and Health (CNSSCH). We collected sex, age, regions, parental educational levels, physical activity duration and sleep-related information by questionnaire survey, and also conducted anthropometric measurements including height, weight and waist circumference (WC). Unadjusted and adjusted binary logistic regression models were used to estimate the associations of sleep-related dimensions with obesity-related indicators.
Results
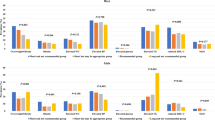
Short sleep duration was associated with higher body mass index (BMI), larger WC and higher waist-to-height ratio (WHtR) in 9–12 and 16–18 age groups, whereas prolonged sleep duration on weekday was associated with higher BMI in 13–15 age group. Non-habitual midday napping and midday napping ≤0.5 h/d (vs 0.5 to 1 h/d) increased the risk of higher BMI in 13–15 age group, and the former was also associated with larger WC in 9–12 age group. Late bedtime was associated with larger WC and higher WHtR in 9–12 age group and with higher BMI and WHtR in 13–15 age group. Students aged 9–12 with social jet lag ≥2 h were found to have greater BMI after adjustment (Odds Ratio: 1.421; 95% confidence interval: 1.066–1.894).
Conclusions
Short or overlong sleep duration, late bedtime and great social jet lag were associated with higher prevalence of overall or abdominal obesity, while moderate midday napping can effectively decrease the risk. Those findings may assist in developing preventive strategies to combat obesity epidemic.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data generated or analyzed during this study can be applied under the data holder’s permission.
References
Jaacks LM, Vandevijvere S, Pan A, McGowan CJ, Wallace C, Imamura F, et al. The obesity transition: stages of the global epidemic. Lancet Diabetes Endocrinol. 2019;7:231–40.
Pan XF, Wang L, Pan A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 2021;9:373–92.
WHO. Global status report on non-communicable diseases 2014. 2014 Available from: http://www.who.int/nmh/publications/ncd-status-report-2014/en/.
Poddar M, Chetty Y, Chetty VT. How does obesity affect the endocrine system? A narrative review. Clin Obes. 2017;7:136–44.
Alpert MA, Omran J, Bostick BP. Effects of obesity on cardiovascular hemodynamics, cardiac morphology, and ventricular function. Curr Obes Rep. 2016;5:424–34.
Berenson GS. Bogalusa Heart Study g. Health consequences of obesity. Pediatr Blood Cancer. 2012;58:117–21.
Yang HJ, Kim MJ, Hur HJ, Lee BK, Kim MS, Park S. Association between Korean-style balanced diet and risk of abdominal obesity in Korean adults: an analysis using KNHANES-VI (2013–2016). Front Nutr. 2021;8:772347.
Chaput JP, Perusse L, Despres JP, Tremblay A, Bouchard C. Findings from the quebec family study on the etiology of obesity: genetics and environmental highlights. Curr Obes Rep. 2014;3:54–66.
Chaput JP, Dutil C. Lack of sleep as a contributor to obesity in adolescents: impacts on eating and activity behaviors. Int J Behav Nutr Phys Act. 2016;13:103.
Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Med Rev. 2008;12:289–98.
Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring). 2008;16:643–53.
Knutson KL. Sleep duration and cardiometabolic risk: a review of the epidemiologic evidence. Best Pract Res Clin Endocrinol Metab. 2010;24:731–43.
Asarnow LD, McGlinchey E, Harvey AG. Evidence for a possible link between bedtime and change in body mass index. Sleep. 2015;38:1523–7.
Malone SK, Zemel B, Compher C, Souders M, Chittams J, Thompson AL, et al. Social jet lag, chronotype and body mass index in 14–17-year-old adolescents. Chronobiol Int. 2016;33:1255–66.
Zeron-Rugerio MF, Cambras T, Izquierdo-Pulido M. Social jet lag associates negatively with the adherence to the mediterranean diet and body mass index among young adults. Nutrients. 2019;11:1756.
Sa J, Choe S, Cho BY, Chaput JP, Kim G, Park CH, et al. Relationship between sleep and obesity among U.S. and South Korean college students. BMC Public Health. 2020;20:96.
Loredo JS, Weng J, Ramos AR, Sotres-Alvarez D, Simonelli G, Talavera GA, et al. Sleep patterns and obesity: Hispanic community health study/study of Latinos Sueno Ancillar study. Chest. 2019;156:348–56.
Ji CY, Cheng TO. Prevalence and geographic distribution of childhood obesity in China in 2005. Int J Cardiol. 2008;131:1–8.
Ma J, Pei T, Dong F, Dong Y, Yang Z, Chen J, et al. Spatial and demographic disparities in short stature among school children aged 7–18 years: a nation-wide survey in China, 2014. BMJ Open. 2019;9:e026634.
Health requirements of daily learning time for secondary and elementary school students 2012. Available from: https://std.samr.gov.cn/gb/search/gbDetailed?id=71F772D7F4BAD3A7E05397BE0A0AB82A.
Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: misalignment of biological and social time. Chronobiol Int. 2006;23:497–509.
Hena M, Garmy P. Social jetlag and its association with screen time and nighttime texting among adolescents in Sweden: a cross-sectional study. Front Neurosci. 2020;14:122.
de Zwart BJ, Beulens JWJ, Elders P, Rutters F. Pilot data on the association between social jetlag and obesity-related characteristics in Dutch adolescents over one year. Sleep Med. 2018;47:32–5.
Li X, Buxton OM, Kim Y, Haneuse S, Kawachi I. Do procrastinators get worse sleep? Cross-sectional study of US adolescents and young adults. SSM Popul Health. 2020;10:100518.
Group of China Obesity Task F. Body mass index reference norm for screening overweight and obesity in Chinese children and adolescents. Zhonghua Liu Xing Bing Xue Za Zhi. 2004;25:97–102.
Ma GS, Ji CY, Ma J, Mi J, Sung R, Xiong F, et al. Waist circumference reference values for screening cardiovascular risk factors in Chinese children and adolescents aged 7–18 years. Zhonghua Liu Xing Bing Xue Za Zhi. 2010;31:609–15.
Dai Y, Fu J, Liang L, Gong C, Xiong F, Liu G.et al. A proposal for the cutoff point of waist-to-height for the diagnosis of metabolic syndrome in children and adolescents in six areas of China. Zhonghua Liu Xing Bing Xue Za Zhi. 2014;35:882–5.
Fan M, Lyu J, He P. Chinese guidelines for data processing and analysis concerning the International Physical Activity Questionnaire. Zhonghua Liu Xing Bing Xue Za Zhi. 2014;35:961–4.
Ke Y, Zhang S, Hao Y, Liu Y. Associations between socioeconomic status and risk of obesity and overweight among Chinese children and adolescents. BMC Public Health. 2023;23:401.
Apfelbacher CJ, Loerbroks A, Cairns J, Behrendt H, Ring J, Kramer U. Predictors of overweight and obesity in five to seven-year-old children in Germany: results from cross-sectional studies. BMC Public Health. 2008;8:171.
Cardenas-Fuentes G, Homs C, Ramirez-Contreras C, Juton C, Casas-Esteve R, Grau M, et al. Prospective association of maternal educational level with child’s physical activity, screen time, and diet quality. Nutrients. 2021;14:160.
Dong X, Ding L, Zhang R, Ding M, Wang B, Yi X. Physical activity, screen-based sedentary behavior and physical fitness in Chinese adolescents: a cross-sectional study. Front Pediatr. 2021;9:722079.
Gong QH, Li SX, Li H, Cui J, Xu GZ. Insufficient sleep duration and overweight/obesity among adolescents in a Chinese population. Int J Environ Res Public Health. 2018;15:997.
Zhang J, Jin X, Yan C, Jiang F, Shen X, Li S. Short sleep duration as a risk factor for childhood overweight/obesity: a large multicentric epidemiologic study in China. Sleep Health. 2015;1:184–90.
Fan J, Ding C, Gong W, Yuan F, Zhang Y, Feng G, et al. Association of sleep duration and overweight/obesity among children in China. Int J Environ Res Public Health. 2020;17:1962.
Danielsen YS, Pallesen S, Stormark KM, Nordhus IH, Bjorvatn B. The relationship between school day sleep duration and body mass index in Norwegian children (aged 10–12). Int J Pediatr Obes. 2010;5:214–20.
Wu J, Wu H, Wang J, Guo L, Deng X, Lu C. Associations between sleep duration and overweight/obesity: results from 66,817 Chinese adolescents. Sci Rep. 2015;5:16686.
Singh M, Drake CL, Roehrs T, Hudgel DW, Roth T. The association between obesity and short sleep duration: a population-based study. J Clin Sleep Med. 2005;1:357–63.
Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62.
Spiegel K, Leproult R, L’Hermite-Baleriaux M, Copinschi G, Penev PD, Van Cauter E. Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. J Clin Endocrinol Metab. 2004;89:5762–71.
St-Onge MP, Wolfe S, Sy M, Shechter A, Hirsch J. Sleep restriction increases the neuronal response to unhealthy food in normal-weight individuals. Int J Obes (Lond). 2014;38:411–6.
Knutson KL, Van, Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. 2008;1129:287–304.
Ayas NT, White DP, Manson JE, Stampfer MJ, Speizer FE, Malhotra A, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163:205–9.
Xin C, Zhang B, Fang S, Zhou J. Daytime napping and successful aging among older adults in China: a cross-sectional study. BMC Geriatr. 2020;20:2.
Wang N, Zou J, Fang S, Zhou J. Association between daytime napping and obesity in Chinese middle-aged and older adults. J Glob Health. 2020;10:020804.
Zhao X, Cheng L, Zhu C, Cen S, Lin W, Zheng W, et al. A double-edged sword: the association of daytime napping duration and metabolism related diseases in a Chinese population. Eur J Clin Nutr. 2021;75:291–8.
Ji X, Li J, Liu J. The relationship between midday napping and neurocognitive function in early adolescents. Behav Sleep Med. 2019;17:537–51.
Olds TS, Maher CA, Matricciani L. Sleep duration or bedtime? Exploring the relationship between sleep habits and weight status and activity patterns. Sleep. 2011;34:1299–307.
Busto-Zapico R, Amigo-Vazquez I, Pena-Suarez E, Fernandez-Rodriguez C. Relationships between sleeping habits, sedentary leisure activities and childhood overweight and obesity. Psychol Health Med. 2014;19:667–72.
Thivel D, Isacco L, Aucouturier J, Pereira B, Lazaar N, Ratel S, et al. Bedtime and sleep timing but not sleep duration are associated with eating habits in primary school children. J Dev Behav Pediatr. 2015;36:158–65.
Skene DJ, Arendt J. Human circadian rhythms: physiological and therapeutic relevance of light and melatonin. Ann Clin Biochem. 2006;435:344–53.
Sun M, Feng W, Wang F, Li P, Li Z, Li M, et al. Meta-analysis on shift work and risks of specific obesity types. Obes Rev. 2018;19:28–40.
Van Cauter E, Leproult R, Plat L. Age-related changes in slow wave sleep and REM sleep and relationship with growth hormone and cortisol levels in healthy men. JAMA. 2000;284:861–8.
Mathew GM, Hale L, Chang AM. Social jetlag, eating behaviours and BMI among adolescents in the USA. Br J Nutr. 2020;124:979–87.
Bray MS, Young ME. Circadian rhythms in the development of obesity: potential role for the circadian clock within the adipocyte. Obes Rev. 2007;8:169–81.
Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141:846–50.
Qian J, Dalla Man C, Morris CJ, Cobelli C, Scheer F. Differential effects of the circadian system and circadian misalignment on insulin sensitivity and insulin secretion in humans. Diabetes Obes Metab. 2018;20:2481–5.
Marcinkevage JA, Alverson CJ, Narayan KM, Kahn HS, Ruben J, Correa A. Race/ethnicity disparities in dysglycemia among U.S. women of childbearing age found mainly in the nonoverweight/nonobese. Diabetes Care. 2013;36:3033–9.
Vgontzas AN, Fernandez-Mendoza J, Miksiewicz T, Kritikou I, Shaffer ML, Liao D, et al. Unveiling the longitudinal association between short sleep duration and the incidence of obesity: the Penn State Cohort. Int J Obes (Lond). 2014;38:825–32.
Funding
This work was supported by the National Natural Science Foundation of China (Grant No.82003478).
Author information
Authors and Affiliations
Contributions
XW designed the study, edited the writing and revised the manuscript; LY and SH independently carried out the literature search and screening of articles, analyzed the data and wrote the manuscript; CM participated in data analysis; XL designed the study, conducted field research and provided data; HL, GG, and CH conducted field research and provided data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The research protocol was approved by the Zhengzhou University Life Science Ethics Committee (ZZUIRB2021–56). Informed consent of parents and their children were obtained.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, L., Han, S., Miao, C. et al. Associations of multiple sleep dimensions with overall and abdominal obesity among children and adolescents: a population-based cross-sectional study. Int J Obes 47, 817–824 (2023). https://doi.org/10.1038/s41366-023-01324-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-023-01324-2