Abstract
Background/objectives
Experimental studies of time-restricted eating suggest that limiting the daily eating window, shifting intake to the biological morning, and avoiding eating close to the biological night may promote metabolic health and prevent weight gain.
Subjects/methods
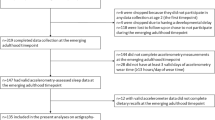
We used the Eating & Health Module of the 2006–2008 and 2014–2016 American Time Use Survey to examine cross-sectional associations of timing of eating in relation to sleep/wake times as a proxy for circadian timing with body mass index (BMI). The analytical sample included 38 302 respondents (18–64 years; BMI 18.5–50.0 kg/m2). A single 24-hour time use diary was used to calculate circadian timing of eating variables: eating window (time between first and last eating activity); morning fast (time between end of sleep and start of eating window); and evening fast (time between end of eating window and start of sleep). Multinomial logistic regression and predictive margins were used to estimate adjusted population prevalences (AP) by BMI categories and changes in prevalences associated with a one-hour change in circadian timing of eating, controlling for sociodemographic and temporal characteristics.
Results
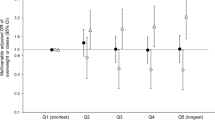
A one-hour increase in eating window was associated with lower adjusted prevalence of obesity (AP = 27.1%, SE = 0.1%). Conversely, a one-hour increase in morning fast (AP = 28.7%, SE = 0.1%) and evening fast (AP = 28.5%, SE = 0.1%) were each associated with higher prevalence of obesity; interactions revealed differing patterns of association by combination of eating window with morning/evening fast (p < 0.0001).
Conclusions
Contrary to hypotheses, longer eating windows were associated with a lower adjusted prevalence of obesity and longer evening fasts were associated with a higher prevalence of obesity. However, as expected, longer morning fast was associated with a higher adjusted prevalence of obesity. Studies are needed to disentangle the contributions of diet quality/quantity and social desirability bias in the relationship between circadian timing of eating and BMI.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Chaix A, Manoogian ENC, Melkani GC, Panda S. Time-restricted eating to prevent and manage chronic metabolic diseases. Annu Rev Nutr. 2019;39:291–315.
Wilkinson MJ, Manoogian ENC, Zadourian A, Lo H, Fakhouri S, Shoghi A, et al. Ten-hour time-restricted eating reduces weight, blood pressure, and atherogenic lipids in patients with metabolic syndrome. Cell Metab. 2020;31:92–104 e5.
Moon S, Kang J, Kim SH, Chung HS, Kim YJ, Yu JM, et al. Beneficial effects of time-restricted eating on metabolic diseases: a systemic review and meta-analysis. Nutrients. 2020;12:1267.
Swiatkiewicz I, Wozniak A, Taub PR. Time-restricted eating and metabolic syndrome: current status and future perspectives. Nutrients. 2021;13:221.
Mattson MP, Allison DB, Fontana L, Harvie M, Longo VD, Malaisse WJ, et al. Meal frequency and timing in health and disease. Proc Natl Acad Sci USA. 2014;111:16647–53.
Paoli A, Tinsley G, Bianco A, Moro T. The influence of meal frequency and timing on health in humans: the role of fasting. Nutrients. 2019;11:719.
Ma Y, Bertone ER, Stanek EJ 3rd, Reed GW, Hebert JR, Cohen NL, et al. Association between eating patterns and obesity in a free-living US adult population. Am J Epidemiol. 2003;158:85–92.
Kahleova H, Lloren JI, Mashchak A, Hill M, Fraser GE. Meal frequency and timing are associated with changes in body mass index in adventist health study 2. J Nutr. 2017;147:1722–8.
Xiao Q, Garaulet M, Scheer F. Meal timing and obesity: interactions with macronutrient intake and chronotype. Int J Obes. 2019;43:1701–11.
Roenneberg T, Kuehnle T, Juda M, Kantermann T, Allebrandt K, Gordijn M, et al. Epidemiology of the human circadian clock. Sleep Med Rev. 2007;11:429–38.
Fischer D, Lombardi DA, Marucci-Wellman H, Roenneberg T. Chronotypes in the US–Influence of age and sex. PLoS One. 2017;12:e0178782.
Innominato PF, Roche VP, Palesh OG, Ulusakarya A, Spiegel D, Levi FA. The circadian timing system in clinical oncology. Ann Med. 2014;46:191–207.
Patterson RE, Sears DD. Metabolic effects of intermittent fasting. Annu Rev Nutr. 2017;37:371–93.
Zarrinpar A, Chaix A, Panda S. Daily eating patterns and their impact on health and disease. Trends Endocrinol Metab. 2016;27:69–83.
de Cabo R, Mattson MP. Effects of intermittent fasting on health, aging, and disease. N Engl J Med. 2019;381:2541–51.
Gill S, Panda S. A smartphone app reveals erratic diurnal eating patterns in humans that can be modulated for health benefits. Cell Metab. 2015;22:789–98.
Oike H, Oishi K, Kobori M. Nutrients, clock genes, and chrononutrition. Curr Nutr Rep. 2014;3:204–12.
Aoyama S, Shibata S. Time-of-day-dependent physiological responses to meal and exercise. Front Nutr. 2020;7:18.
Jakubowicz D, Barnea M, Wainstein J, Froy O. High caloric intake at breakfast vs. dinner differentially influences weight loss of overweight and obese women. Obesity. 2013;21:2504–12.
Gu C, Brereton N, Schweitzer A, Cotter M, Duan D, Borsheim E, et al. Metabolic effects of late dinner in healthy volunteers–a randomized crossover clinical trial. J Clin Endocrinol Metab. 2020;105:2789–2802.
Al-Naimi S, Hampton SM, Richard P, Tzung C, Morgan LM. Postprandial metabolic profiles following meals and snacks eaten during simulated night and day shift work. Chronobiology International. 2009;21:937–47.
Okada C, Imano H, Muraki I, Yamada K, Iso H. The association of having a late dinner or bedtime snack and skipping breakfast with overweight in japanese women. J Obes. 2019;2019:2439571.
McHill AW, Phillips AJ, Czeisler CA, Keating L, Yee K, Barger LK, et al. Later circadian timing of food intake is associated with increased body fat. Am J Clin Nutr. 2017;106:1213–9.
Hutchison AT, Regmi P, Manoogian ENC, Fleischer JG, Wittert GA, Panda S, et al. Time-restricted feeding improves glucose tolerance in men at risk for type 2 diabetes: a randomized crossover trial. Obesity (Silver Spring). 2019;27:724–32.
Jamshed H, Beyl RA, Della Manna DL, Yang ES, Ravussin E, Peterson CM. Early time-restricted feeding improves 24-hour glucose levels and affects markers of the circadian clock, aging, and autophagy in humans. Nutrients. 2019;11:1234.
Cienfuegos S, Gabel K, Kalam F, Ezpeleta M, Wiseman E, Pavlou V, et al. Effects of 4- and 6-h time-restricted feeding on weight and cardiometabolic health: a randomized controlled trial in adults with obesity. Cell Metab. 2020;32:366–378.e3.
Pellegrini M, Cioffi I, Evangelista A, Ponzo V, Goitre I, Ciccone G, et al. Effects of time-restricted feeding on body weight and metabolism. A systematic review and meta-analysis. Rev Endocr Metab Disord. 2020;21:17–33.
Czeisler CA, Weitzman E, Moore-Ede MC, Zimmerman JC, Knauer RS. Human sleep: its duration and organization depend on its circadian phase. Science. 1980;210:1264–7.
Sletten TL, Vincenzi S, Redman JR, Lockley SW, Rajaratnam SM. Timing of sleep and its relationship with the endogenous melatonin rhythm. Front Neurol. 2010;1:137.
Lovato N, Micic G, Gradisar M, Ferguson SA, Burgess HJ, Kennaway DJ, et al. Can the circadian phase be estimated from self-reported sleep timing in patients with Delayed Sleep Wake Phase Disorder to guide timing of chronobiologic treatment? Chronobiol Int. 2016;33:1376–90.
American Time Use Survey User’s Guide 2020 https://www.bls.gov/tus/atususersguide.pdf.
American Time Use Survey Data Extract Builder: Version 2.7 [dataset] [Internet]. https://doi.org/10.18128/D060.V2.7.
Zeballos E, Todd JE, Restrepo B. Frequency and time of day that Americans eat: a comparison of frequency and time of day data from the American Data From the American Time Use Survey and the National Health and Nutrition Examination Survey. US Department of Agriculture. 2019; Economic Research Service.
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organization Technical Report Series 2000.
Skeldon AC, Derks G, Dijk DJ. Modelling changes in sleep timing and duration across the lifespan: changes in circadian rhythmicity or sleep homeostasis? Sleep Med Rev. 2016;28:96–107.
Korn E, Graubard B. Epidemiologic studies utilizing surveys: accounting for the sampling design. Am J Public Health. 1991;81:1166–73.
Chow LS, Manoogian ENC, Alvear A, Fleischer JG, Thor H, Dietsche K, et al. Time-restricted eating effects on body composition and metabolic measures in humans who are overweight: a feasibility study. Obesity (Silver Spring). 2020;28:860–9.
Adafer R, Messaadi W, Meddahi M, Patey A, Haderbache A, Bayen S, et al. Food timing, circadian rhythm and chrononutrition: a systematic review of time-restricted eating’s effects on human health. Nutrients. 2020;12:3770.
Lean ME, Malkova D. Altered gut and adipose tissue hormones in overweight and obese individuals: cause or consequence? Int J Obes. 2016;40:622–32.
Kesztyus D, Cermak P, Gulich M, Kesztyus T. Adherence to time-restricted feeding and impact on abdominal obesity in primary care patients: results of a pilot study in a pre-post design. Nutrients. 2019;11:2854
St-Onge MP, Ard J, Baskin ML, Chiuve SE, Johnson HM, Kris-Etherton P, et al. Meal timing and frequency: implications for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation. 2017;135:e96–e121.
Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005;82:222S–225S.
Bonnet JP, Cardel MI, Cellini J, Hu FB, Guasch-Ferre M. Breakfast skipping, body composition, and cardiometabolic risk: a systematic review and meta-analysis of randomized trials. Obesity. 2020;28:1098–1109.
Dashti HS, Scheer F, Saxena R, Garaulet M. Timing of food intake: identifying contributing factors to design effective interventions. Adv Nutr. 2019;10:606–20.
Leech RM, Worsley A, Timperio A, McNaughton SA. Understanding meal patterns: definitions, methodology and impact on nutrient intake and diet quality. Nutr Res Rev. 2015;28:1–21.
Matthews CE, Berrigan D, Fischer B, Gomersall SR, Hillreiner A, Kim Y, et al. Use of previous-day recalls of physical activity and sedentary behavior in epidemiologic studies: results from four instruments. BMC Public Health. 2019;19:478.
Matthews CE, Keadle SK, Sampson J, Lyden K, Bowles HR, Moore SC, et al. Validation of a previous-day recall measure of active and sedentary behaviors. Med Sci Sports Exerc. 2013;45:1629–38.
Harms T, Gershuny J, Doherty A, Thomas E, Milton K, Foster C. A validation study of the Eurostat harmonised European time use study (HETUS) diary using wearable technology. BMC Public Health. 2019;19:455.
Ekelund U, Brage S, Besson H, Sharp S, Wareham NJ. Time spent being sedentary and weight gain in healthy adults: reverse or bidirectional causality? Am J Clin Nutr. 2008;88:612–7.
Carroll RJ, Ruppert D, Stefanski LA, Crainiceanu CM. Measurement error in nonlinear models: a modern perspective, second edition: CRC Press; 2006. 455 p.
Kaplan RL, Kopp B, Phipps P. Contrasting stylized questions of sleep with diary measures from the American Time Use Survey. Office of Survey Methods Research, Bureau of Labor Statistics; 2016.
Jakubowicz D, Froy O, Wainstein J, Boaz M. Meal timing and composition influence ghrelin levels, appetite scores and weight loss maintenance in overweight and obese adults. Steroids. 2012;77:323–31.
Teixeira GP, Barreto ACF, Mota MC, Crispim CA. Caloric midpoint is associated with total calorie and macronutrient intake and body mass index in undergraduate students. Chronobiol Int. 2019;36:1418–28.
Bo S, Musso G, Beccuti G, Fadda M, Fedele D, Gambino R, et al. Consuming more of daily caloric intake at dinner predisposes to obesity. A 6-year population-based prospective cohort study. PLoS One. 2014;9:e108467.
Kant AK. Eating patterns of US adults: meals, snacks, and time of eating. Physiol Behav. 2018;193:270–8.
Kant AK, Graubard BI. 40-year trends in meal and snack eating behaviors of American adults. J Acad Nutr Diet. 2015;115:50–63.
Goris AH, Westerterp-Plantenga MS, Westerterp KR. Undereating and underrecording of habitual food intake in obese men: selective underreporting of fat intake. Am J Clin Nutr. 2000;71:130–4.
Macdiarmid J, Blundell J. Assessing dietary intake: who, what and why of under-reporting. Nutr Res Rev. 1998;11:231–53.
Scientific Report of the 2020 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Agriculture and the Secretary of Health and Human Services. Washington, DC: U.S. Department of Agriculture, Agricultural Research Service; 2020.
Author information
Authors and Affiliations
Contributions
SGO designed the study, led the statistical analysis, and drafted the manuscript. AKK, JR, and SMC contributed to the interpretation of results and critically revised the manuscript. BIG contributed to the statistical analysis and interpretation of results, and critically revised manuscript. DB contributed to the analytical design, statistical analysis, and interpretation, and critically revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Disclaimer
The opinions expressed in this article are the authors’ own and do not necessarily reflect the view of the National Institutes of Health, the Department of Health and Human Services, or the United States government.
Supplementary information
Rights and permissions
About this article
Cite this article
O’Connor, S.G., Reedy, J., Graubard, B.I. et al. Circadian timing of eating and BMI among adults in the American Time Use Survey. Int J Obes 46, 287–296 (2022). https://doi.org/10.1038/s41366-021-00983-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-00983-3
This article is cited by
-
Association of meal timing with body composition and cardiometabolic risk factors in young adults
European Journal of Nutrition (2023)
-
Sex differences in the association between dinner–bedtime interval and abdominal obesity: a large-scale cross-sectional study
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2022)