Abstract
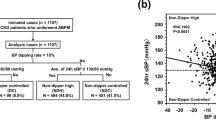
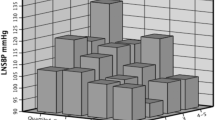
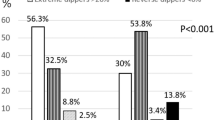
The relationship between declining nocturnal blood pressure (BP) and adverse cardiovascular outcomes is well-recognized. However, the relationship between diurnal BP profile and the risk of chronic kidney disease (CKD) progression is unclear. Herein, we examined the association between nocturnal systolic SBP (SBP) dipping and CKD progression in 1061 participants at the Cardiovascular and Metabolic Disease Etiology Research Center-High Risk (CMERC-HI). The main exposure was diurnal systolic BP (SBP) profile and diurnal SBP difference ([nighttime SBP-daytime SBP] × 100/daytime SBP). The primary outcome was CKD progression, defined as a composite of ≥ a 50% decline in the estimated glomerular filtration rate from baseline or the initiation of kidney replacement therapy. During 4749 person-years of follow-up (median, 4.8 years), the composite outcome occurred in 380 (35.8%) participants. Compared to dippers, the hazard ratios (HRs) for the risk of adverse kidney outcomes were 1.02 (95% confidence interval [CI], 0.64–1.62), 1.30 (95% CI, 1.02–1.66), and 1.40 (95% CI, 1.03–1.90) for extreme dipper, non-dipper, and reverse dipper, respectively. In a continuous modeling, a 10% increase in diurnal SBP difference was associated with a 1.21-fold (95% CI, 1.07–1.37) higher risk of CKD progression. Thus, decreased nocturnal SBP decline was associated with adverse kidney outcomes in patients with CKD. Particularly, patients with non-dipping and reverse dipping patterns were at higher risk for CKD progression than those with a dipping pattern.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
USRD System. 2021 USRDS Annual Data Report: epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2021.
Lee JY, Park JT, Joo YS, Lee C, Yun HR, Yoo TH, et al. Association of blood pressure with the progression of CKD: findings from KNOW-CKD study. Am J Kidney Dis. 2021;78:236–45.
Blood Pressure Lowering Treatment Trialists’ Collaboration, Ninomiya T, Perkovic V, Turnbull F, Neal B, Barzi F, et al. Blood pressure lowering and major cardiovascular events in people with and without chronic kidney disease: meta-analysis of randomised controlled trials. BMJ. 2013;347:f5680.
Malhotra R, Nguyen HA, Benavente O, Mete M, Howard BV, Mant J, et al. Association between more intensive vs less intensive blood pressure lowering and risk of mortality in chronic kidney disease stages 3 to 5: a systematic review and meta-analysis. JAMA Intern Med. 2017;177:1498–505.
Kidney Disease: Improving Global Outcomes Blood Pressure Work Group. KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int. 2021;99:S1–87.
Cohen JB, Lotito MJ, Trivedi UK, Denker MG, Cohen DL, Townsend RR. Cardiovascular events and mortality in white coat hypertension: a systematic review and meta-analysis. Ann Intern Med. 2019;170:853–62.
Pierdomenico SD, Pierdomenico AM, Coccina F, Clement DL, De Buyzere ML, De Bacquer DA, et al. Prognostic value of masked uncontrolled hypertension. Hypertension. 2018;72:862–9.
Son HE, Ryu JY, Go S, Yi Y, Kim K, Oh YK, et al. Association of ambulatory blood pressure monitoring with renal outcome in patients with chronic kidney disease. Kidney Res Clin Pr. 2020;39:70–80.
Pickering TG. The clinical significance of diurnal blood pressure variations. Dippers and nondippers. Circulation. 1990;81:700–2.
Bankir L, Bochud M, Maillard M, Bovet P, Gabriel A, Burnier M. Nighttime blood pressure and nocturnal dipping are associated with daytime urinary sodium excretion in African subjects. Hypertension. 2008;51:891–8.
Verdecchia P, Schillaci G, Guerrieri M, Gatteschi C, Benemio G, Boldrini F, et al. Circadian blood pressure changes and left ventricular hypertrophy in essential hypertension. Circulation. 1990;81:528–36.
Tadic M, Cuspidi C, Pencic B, Ivanovic B, Scepanovic R, Marjanovic T, et al. Circadian blood pressure pattern and right ventricular and right atrial mechanics: a two- and three-dimensional echocardiographic study. J Am Soc Hypertens. 2014;8:45–53.
Boggia J, Li Y, Thijs L, Hansen TW, Kikuya M, Bjorklund-Bodegard K, et al. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007;370:1219–29.
Salles GF, Reboldi G, Fagard RH, Cardoso CR, Pierdomenico SD, Verdecchia P, et al. Prognostic effect of the nocturnal blood pressure fall in hypertensive patients: The Ambulatory Blood Pressure Collaboration in Patients With Hypertension (ABC-H) Meta-Analysis. Hypertension. 2016;67:693–700.
Debella YT, Giduma HD, Light RP, Agarwal R. Chronic kidney disease as a coronary disease equivalent—a comparison with diabetes over a decade. Clin J Am Soc Nephrol. 2011;6:1385–92.
Briasoulis A, Bakris GL. Chronic kidney disease as a coronary artery disease risk equivalent. Curr Cardiol Rep. 2013;15:340.
Mojón A, Ayala DE, Piñeiro L, Otero A, Crespo JJ, Moyá A, et al. Comparison of ambulatory blood pressure parameters of hypertensive patients with and without chronic kidney disease. Chronobiol Int. 2013;30:145–58.
Cho SMJ, Lee H, Yoo TH, Jhee JH, Park S, Kim HC. Association between nocturnal blood pressure dipping and chronic kidney disease among patients with controlled office blood pressure. Am J Hypertens. 2021;34:821–30.
Agarwal R, Andersen MJ. Blood pressure recordings within and outside the clinic and cardiovascular events in chronic kidney disease. Am J Nephrol. 2006;26:503–10.
Minutolo R, Agarwal R, Borrelli S, Chiodini P, Bellizzi V, Nappi F, et al. Prognostic role of ambulatory blood pressure measurement in patients with nondialysis chronic kidney disease. Arch Intern Med. 2011;171:1090–8.
Rahman M, Wang X, Bundy JD, Charleston J, Cohen D, Cohen J, et al. Prognostic significance of ambulatory BP monitoring in CKD: a report from the Chronic Renal Insufficiency Cohort (CRIC) Study. J Am Soc Nephrol. 2020;31:2609–21.
Levy D, Kannel WB. Cardiovascular risks: new insights from Framingham. Am Heart J. 1988;116:266–72.
Haroun MK, Jaar BG, Hoffman SC, Comstock GW, Klag MJ, Coresh J. Risk factors for chronic kidney disease: a prospective study of 23,534 men and women in Washington County, Maryland. J Am Soc Nephrol. 2003;14:2934–41.
Jung HH. Albuminuria, estimated glomerular filtration rate, and traditional predictors for composite cardiovascular and kidney outcome: a population-based cohort study in Korea. Kidney Res Clin Pr. 2022;41:567–79.
Kado H, Kusaba T, Matoba S, Hatta T, Tamagaki K. Normotensive non-dipping blood pressure profile does not predict the risk of chronic kidney disease progression. Hypertens Res. 2019;42:354–61.
Gabbai FB, Rahman M, Hu B, Appel LJ, Charleston J, Contreras G, et al. Relationship between ambulatory BP and clinical outcomes in patients with hypertensive CKD. Clin J Am Soc Nephrol. 2012;7:1770–6.
Borrelli S, Garofalo C, Gabbai FB, Chiodini P, Signoriello S, Paoletti E, et al. Dipping status, ambulatory blood pressure control, cardiovascular disease, and kidney disease progression: a multicenter cohort study of CKD. Am J Kidney Dis. 2022;81:15–24.e1.
Shim JS, Song BM, Lee JH, Lee SW, Park JH, Choi DP, et al. Cardiovascular and Metabolic Diseases Etiology Research Center (CMERC) cohort: study protocol and results of the first 3 years of enrollment. Epidemiol Health. 2017;39:e2017016.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12.
O'Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–68.
Pogue V, Rahman M, Lipkowitz M, Toto R, Miller E, Faulkner M, et al. Disparate estimates of hypertension control from ambulatory and clinic blood pressure measurements in hypertensive kidney disease. Hypertension. 2009;53:20–7.
Braun WJ, Huang L-S. Kernel spline regression. Can J Stat/La Revue Canadienne de Statistique. 2005;33:259–78.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Himmelfarb CD, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension. 2018;71:e13–115.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36:1953–2041.
Bianchi S, Bigazzi R, Baldari G, Sgherri G, Campese VM. Diurnal variations of blood pressure and microalbuminuria in essential hypertension. Am J Hypertens. 1994;7:23–9.
Grassi G, Seravalle G, Quarti-Trevano F, Dell'Oro R, Bombelli M, Cuspidi C, et al. Adrenergic, metabolic, and reflex abnormalities in reverse and extreme dipper hypertensives. Hypertension. 2008;52:925–31.
Myredal A, Friberg P, Johansson M. Elevated myocardial repolarization lability and arterial baroreflex dysfunction in healthy individuals with nondipping blood pressure pattern. Am J Hypertens. 2010;23:255–9.
Sachdeva A, Weder AB. Nocturnal sodium excretion, blood pressure dipping, and sodium sensitivity. Hypertension. 2006;48:527–33.
Shin J, Lee CH. The roles of sodium and volume overload on hypertension in chronic kidney disease. Kidney Res Clin Pr. 2021;40:542–54.
von Kanel R, Jain S, Mills PJ, Nelesen RA, Adler KA, Hong S, et al. Relation of nocturnal blood pressure dipping to cellular adhesion, inflammation and hemostasis. J Hypertens. 2004;22:2087–93.
Castelpoggi CH, Pereira VS, Fiszman R, Cardoso CR, Muxfeldt ES, Salles GF. A blunted decrease in nocturnal blood pressure is independently associated with increased aortic stiffness in patients with resistant hypertension. Hypertens Res. 2009;32:591–6.
Satoh M, Kikuya M, Ohkubo T, Mori T, Metoki H, Hashimoto T, et al. Aldosterone-to-renin ratio and nocturnal blood pressure decline in a general population: the Ohasama study. J Hypertens. 2011;29:1940–7.
Minutolo R, Gabbai FB, Chiodini P, Garofalo C, Stanzione G, Liberti ME, et al. Reassessment of ambulatory blood pressure improves renal risk stratification in nondialysis chronic kidney disease: long-term cohort study. Hypertension. 2015;66:557–62.
Wang C, Ye Z, Li Y, Zhang J, Zhang Q, Ma X, et al. Prognostic value of reverse dipper blood pressure pattern in chronic kidney disease patients not undergoing dialysis: prospective cohort study. Sci Rep. 2016;6:34932.
Funding
This research was supported by the “National Institute of Health” research project (project No. 2021-ER0903-02; SP) and a grant from the Korean Health Technology Research and Development Project through the Korean Health Industry Development Institute, funded by the Ministry of Health and Welfare, Republic of Korea (grant number HI13C0715; SP) and by a research program funded by the Korea Disease Control and Prevention Agency (grant number 2021-ER0903-02; SP). This research was also supported by the Main Research Program (grant number E0210601-03; SP) of the Korea Food Research Institute, funded by the Korean Ministry of Science and ICT. The funders of this study had no role in study design, data collection, analysis, reporting, or the decision to submit for publication.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The opinions, results, and conclusions are those of the authors and are independent from this funding and data sources. All the authors declared no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Park, C.H., Jhee, J.H., Chun, KH. et al. Nocturnal systolic blood pressure dipping and progression of chronic kidney disease. Hypertens Res 47, 215–224 (2024). https://doi.org/10.1038/s41440-023-01368-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01368-x