Abstract
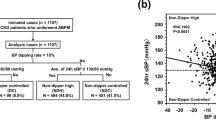
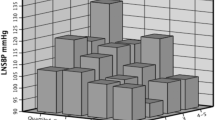
Albuminuria is a prognostic marker of worsening renal outcomes in people with hypertension and type 2 diabetes. High home systolic blood pressure is associated with the development of diabetic nephropathy. We assessed the impact of chronic high home blood pressure on diabetic nephropathy progression 10 years after study entry. The participants measured their blood pressure three times in the morning for 14 days at study entry and 10 years after study entry. A retrospective cohort of 165 people with type 2 diabetes at a single hospital was classified into four groups (good control maintenance, improvement, deterioration, and continuous high blood pressure groups) according to a morning home systolic blood pressure ≥125 mmHg at study entry and 10 years after study entry. Logistic regression analysis was performed to determine the association between home blood pressure control and the progression of diabetic nephropathy. After 10 years of entry, the status of nephropathy improved for 5.5% of the participants, remained unchanged for 72.1%, and progressed for 22.4%. The odds ratio of the continuous high blood pressure group versus that of the good control maintenance group for the progression of diabetic nephropathy was 10.41 (95% CI, 1.26–86.15). After adjusting for the introduction of renin-angiotensin-aldosterone system inhibitors during the follow-up period, there was no significant difference in the odds ratio of worsening nephropathy between these groups. The deterioration and improvement groups did not have significant diabetic nephropathy progression compared to the good control maintenance group. Chronic high home blood pressure was associated with the progression of diabetic nephropathy, and RAAS inhibitors could attenuate the negative effect.

We demonstrated that chronic home blood pressure was associated with the progression of diabetic nephropathy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
NCD Risk. Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017;389:37–55.
World Health Organization. World health statistics 2016: monitoring Health for the SDGs [cited Jun 2022]. Available from: https://www.who.int/publications/i/item/9789241565264.
Sun D, Zhou T, Heianza Y, Li X, Fan M, Fonseca VA, et al. Type 2 diabetes and hypertension. Circ Res. 2019;124:930–7.
Basi S, Fesler P, Mimran A, Lewis JB. Microalbuminuria in type 2 diabetes and hypertension: a marker, treatment target, or innocent bystander? Diabetes Care. 2008;31:S194–201.
Gerstein HC, Mann JF, Yi Q, Zinman B, Dinneen SF, Hoogwerf B, et al. Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA. 2001;286:421–6.
Leehey DJ, Kramer HJ, Daoud TM, Chatha MP, Isreb MA. Progression of kidney disease in type 2 diabetes—Beyond blood pressure control: an observational study. BMC Nephrol. 2005;6:8.
Ismail-Beigi F, Craven T, Banerji MA, Basile J, Calles J, Cohen RM, et al. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the Accord randomised trial. Lancet. 2010;376:419–30.
ADVANCE Collaborative Group, Patel A, MacMahon S, Chalmers J, Neal B, Billot L, et al. Intensive blood glucose control and vascular outcomes in people with type 2 diabetes. N Engl J Med. 2008;358:2560–72.
Bakris GL, Weir MR, Shanifar S, Zhang Z, Douglas J, van Dijk DJ, et al. Effects of blood pressure level on progression of diabetic nephropathy: results from the RENAAL Study. Arch Intern Med. 2003;163:1555–65.
Ushigome E, Hamaguchi M, Matsumoto S, Oyabu C, Omoto A, Tanaka T, et al. Optimal home SBP targets for preventing the progression of diabetic nephropathy in people with type 2 diabetes mellitus. J Hypertens. 2015;33:1853–9. discussion 1859
Ushigome E, Fukui M, Sakabe K, Tanaka M, Inada S, Omoto A, et al. Uncontrolled home blood pressure in the morning is associated with nephropathy in Japanese type 2 diabetes. Heart Vessels. 2011;26:609–15.
Niiranen TJ, Jula AM, Kantola IM, Karanko H, Reunanen A. Home-measured blood pressure is more strongly associated with electrocardiographic left ventricular hypertrophy than is clinic blood pressure: the Finn-HOME study. J Hum Hypertens. 2007;21:788–94.
Oyabu C, Ushigome E, Matsumoto S, Tanaka T, Hasegawa G, Nakamura N, et al. Maximum home blood pressure is a useful indicator of diabetic nephropathy in people with type 2 diabetes mellitus: KAMOGAWA-HBP study. Diab Vasc Dis Res. 2017;14:477–84.
Coleman A, Freeman P, Steel S, Shennan A. Validation of the Omron 705IT (HEM-759-E) oscillometric blood pressure monitoring device according to the British Hypertension Society protocol. Blood Press Monit. 2006;11:27–32.
Ushigome E, Fukui M, Hamaguchi M, Senmaru T, Sakabe K, Tanaka M, et al. The coefficient variation of home blood pressure is a novel factor associated with macroalbuminuria in type 2 diabetes mellitus. Hypertens Res. 2011;34:1271–5.
Ushigome E, Matsumoto S, Oyabu C, Kitagawa N, Tanaka T, Hasegawa G, et al. Prognostic significance of day-by-day variability of home blood pressure on progression to macroalbuminuria in people with diabetes. J Hypertens. 2018;36:1068–75.
Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003;26:S5–20.
Wada T, Haneda M, Furuichi K, Babazono T, Yokoyama H, Iseki K, et al. Clinical impact of albuminuria and glomerular filtration rate on renal and cardiovascular events, and all-cause mortality in Japanese people with type 2 diabetes. Clin Exp Nephrol. 2014;18:613–20.
Yasuda H, Sanada M, Kitada K, Terashima T, Kim H, Sakaue Y, et al. Rationale and usefulness of newly devised abbreviated diagnostic criteria and staging for diabetic polyneuropathy. Diabetes Res Clin Pr. 2007;77:S178–83.
Gæde P, Oellgaard J, Carstensen B, Rossing P, Lund-Andersen H, Parving HH, et al. Years of life gained by multifactorial intervention in people with type 2 diabetes mellitus and microalbuminuria: 21 years follow-up on the Steno-2 randomised trial. Diabetologia. 2016;59:2298–307.
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HAW. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359:1577–89.
Chalmers J, Cooper ME. UKPDS and the legacy effect. N Engl J Med. 2008;359:1618–20.
ACCORD Study Group. Nine-year effects of 3.7 years of intensive glycemic control on cardiovascular outcomes. Diabetes Care. 2016;39:701–8.
Reaven PD, Emanuele NV, Wiitala WL, Bahn GD, Reda DJ, McCarren M, et al. Intensive glucose control in people with type 2 diabetes—15-year follow-up. N Engl J Med. 2019;380:2215–24.
Holman RR, Paul SK, Bethel MA, Neil HAW, Matthews DR. Long-term follow-up after tight control of blood pressure in type 2 diabetes. N. Engl J Med. 2008;359:1565–76.
Menne J, Ritz E, Ruilope LM, Chatzikyrkou C, Viberti G, Haller H. The randomized olmesartan and diabetes microalbuminuria prevention (ROADMAP) observational follow‐up study: benefits of RAS blockade with olmesartan treatment are sustained after study discontinuation. J Am Heart Assoc. 2014;3:e000810.
ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in moderately hypercholesterolemic, hypertensive people randomized to pravastatin vs usual care: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT-LLT). JAMA. 2002;288:2998–3007.
Ford I, Murray H, McCowan C, Packard CJ. Long-Term Safety and Efficacy of Lowering Low-Density Lipoprotein Cholesterol With Statin Therapy: 20-Year Follow-Up of West of Scotland Coronary Prevention Study. Circulation. 2016;133:1073–80.
UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ. 1998;317:703–13.
Zoungas S, Chalmers J, Neal B, Billot L, Li Q, Hirakawa Y, et al. Follow-up of blood-pressure lowering and glucose control in type 2 diabetes. N Engl J Med. 2014;371:1392–406.
Gæde P, Lund-Andersen H, Parving H-H, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008;358:580–91.
Asayama K, Ohkubo T, Metoki H, Obara T, Inoue R, Kikuya M, et al. Cardiovascular outcomes in the first trial of antihypertensive therapy guided by self-measured home blood pressure. Hypertens Res. 2012;35:1102–10.
Yano Y, Hoshide S, Shimizu M, Eguchi K, Ishikawa J, Ishikawa S, et al. Association of home and ambulatory blood pressure changes with changes in cardiovascular biomarkers during antihypertensive treatment. Am J Hypertens. 2012;25:306–12.
Ishikawa J, Hoshide S, Eguchi K, Ishikawa S, Shimada K, Kario K, et al. Nighttime home blood pressure and the risk of hypertensive target organ damage. Hypertension. 2012;60:921–8.
Turak O, Afsar B, Siriopol D, Ozcan F, Cagli K, Yayla C, et al. Morning blood pressure surge as a predictor of development of chronic kidney disease. J Clin Hypertens (Greenwich). 2016;18:444–8.
Fuchs SC, Mello RG, Fuchs FC. Home blood pressure monitoring is better predictor of cardiovascular disease and target organ damage than office blood pressure: a systematic review and meta-analysis. Curr Cardiol Rep. 2013;15:413.
Yoda K, Inaba M, Hamamoto K, Yoda M, Tsuda A, Mori K, et al. Association between glycemic control and morning blood pressure surge with vascular endothelial dysfunction in type 2 diabetic people. Diabetes Care. 2014;37:644–50.
Tofler GH, Brezinski D, Schafer AI, Czeisler CA, Rutherford JD, Willich SN, et al. Concurrent morning increase in platelet aggregability and the risk of myocardial infarction and sudden cardiac death. N Engl J Med. 1987;316:1514–8.
Dodt C, Breckling U, Derad I, Fehm HL, Born J. Plasma epinephrine and norepinephrine concentrations of healthy humans associated with nighttime sleep and morning arousal. Hypertension. 1997;30:71–76.
Ting RZW, Luk AOY, Chan JCN. Treatment and landmark clinical trials for renoprotection. Contrib Nephrol. 2011;170:184–95.
Lin YC, Chang YH, Yang SY, Wu KD, Chu TS. Update of pathophysiology and management of diabetic kidney disease. J Formos Med Assoc. 2018;117:662–75.
Ninčević V, Omanović Kolarić T, Roguljić H, Kizivat T, Smolić M, Bilić Ćurčić I. Renal benefits of SGLT 2 inhibitors and GLP-1 receptor agonists: evidence supporting a paradigm shift in the medical management of type 2 diabetes. Int J Mol Sci. 2019;20:5831–51.
Tomino Y, Gohda T. The prevalence and management of diabetic nephropathy in Asia. Kidney Dis (Basel). 2015;1:52–60.
Acknowledgements
We thank Dr. Atsushi Omoto and Dr. Wataru Fukuda at Kyoto First Red Cross Hospital and Dr. Shinichi Mogami and Dr. Yoshihiro Kitagawa at Osaka General Hospital of West Japan Railway Company for their assistance in collecting data. We are grateful to Sayoko Tanaka at the Kyoto Prefectural University of Medicine for her secretarial assistance and Naoko Higo, Terumi Kaneko, and Machiko Hasegawa at the Kyoto Prefectural University of Medicine for instructing the study participants on how to measure their BP. We are grateful to Editage (www.editage.com) for English language editing.
Funding
EU received grant support from the Japanese Study Group for Physiology and Management of Blood Pressure, the Astellas Foundation for Research on Metabolic Disorders (Grant number: 4024), and the Mishima Kaiun Memorial Foundation. Names of grants: The Japanese Study Group for Physiology and Management of Blood Pressure, the Astellas Foundation for Research on Metabolic Disorders, and the Mishima Kaiun Memorial Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SH reports personal fees from Kowa Pharmaceutical Company Ltd., outside the submitted work. EU received grant support from the Japan Society for the Promotion of Science and received personal fees from Nippon Boehringer Ingelheim Co., Ltd., Mitsubishi Tanabe Pharma Corporation, Daiichi Sankyo Company, Limited, Takeda Pharmaceutical Company Ltd., MSD K.K., Kyowa Hakko Kirin Co., Ltd., Sumitomo Dainippon Pharma Co., Ltd., Kowa Pharmaceutical Co., Ltd., Novo Nordisk Pharma Ltd., Ono Pharmaceutical Co., Ltd., Taisho Pharmaceutical Co., Ltd., AstraZeneca K.K., and Sanofi K.K., outside the submitted work. The donated fund laboratory of diabetes therapeutics is an endowment department supported by an unrestricted grant from Ono Pharmaceutical Co., Ltd., Taiyo Kagaku Co., Ltd. and Taisho Pharmaceutical Co., Ltd. TY reports personal fees from Sumitomo Dainippon Pharma Co., Ltd., outside the submitted work. Isao Yokota reports grants from Kakenhi, Amed, and Health, Labor and Welfare Policy Research Grants, research funding by Nihon Medi-Physics, and speaker fees from Chugai Pharmaceutical Co, AstraZeneca plt, Japan Tobacco Pharmaceutical Division, and Nippon Shinyaku Co., outside the submitted work. MA received personal fees from Takeda Pharmaceutical Co., Ltd., Abbott Japan Co., Ltd., Sumitomo Dainippon Pharma Co., Ltd., Kowa Pharmaceutical Co., Ltd., Novo Nordisk Pharma Ltd., Ono Pharmaceutical Co., Ltd., AstraZeneca K.K., and Chugai Pharmaceutical Co., Ltd., outside the submitted work. MH received grants from AstraZeneca K.K., Ono Pharma Co. Ltd., Oishi Kenko Inc., Yamada Bee Farm, Nippon Boehringer Ingelheim Co. Ltd., and received personal fees from AstraZeneca K.K., Ono Pharma Co. Ltd., Eli Lilly, Japan, Sumitomo Dainippon Pharma Co., Ltd., Daiichi Sankyo Co. Ltd., Mitsubishi Tanabe Pharma Corp., Sanofi K.K., Kowa Pharma Co. Ltd., outside the submitted work. MY reports personal fees from MSD K.K., personal fees from Sumitomo Dainippon Pharma Co., Ltd.; personal fees from Kowa Company, Limited; personal fees from AstraZeneca PLC; personal fees from Takeda Pharmaceutical Company Limited; personal fees from Kyowa Hakko Kirin Co., Ltd.; personal fees from Daiichi Sankyo Company, Limited; personal fees from Kowa Pharmaceutical Company Ltd.; and personal fees from Ono Pharmaceutical Co., LTD., outside the submitted work. Michiaki Fukui received grants from Ono Pharma Co. Ltd., Oishi Kenko Inc., Yamada Bee Farm, Nippon Boehringer Ingelheim Co. Ltd., Kissei Pharma Co. Ltd., Mitsubishi Tanabe Pharma Corp., Daiichi Sankyo Co. Ltd., Sanofi K.K., Takeda Pharma Co. Ltd., Astellas Pharma Inc., MSD K.K., Kyowa Kirin Co., Ltd., Sumitomo Dainippon Pharma Co., Ltd., Kowa Pharma Co. Ltd., Novo Nordisk Pharma Ltd., Sanwa Kagagu Kenkyusho CO., Ltd., Eli Lilly, Japan, K.K., Taisho Pharma Co., Ltd., Terumo Corp., Tejin Pharma Ltd., Nippon Chemiphar Co., Ltd., Abbott Japan Co. Ltd., and Johnson & Johnson K.K. Medical Co., Terumo Corporation, and received personal fees from Nippon Boehringer Ingelheim Co., Ltd., Kissei Pharma Co., Ltd., Mitsubishi Tanabe Pharma Corp., Daiichi Sankyo Co. Ltd., Sanofi K.K., Takeda Pharma Co. Ltd., Astellas Pharma Inc., MSD K.K., Kyowa Kirin Co. Ltd., Sumitomo Dainippon Pharma Co. Ltd., Kowa Pharma Co. Ltd., Novo Nordisk Pharma Ltd., Ono Pharma Co. Ltd., Sanwa Kagaku Kenkyusho Co. Ltd., Eli Lilly Japan K.K., Taisho Pharma Co., Ltd., Bayer Yakuhin, Ltd., AstraZeneca K.K., Mochida Pharma Co. Ltd., Abbott Japan Co. Ltd., Teijin Pharma Ltd., Arkray Inc., Medtronic Japan Co. Ltd., and Nipro Corp., Terumo Corporation, outside the submitted work. The sponsors were not involved in the study design, collection, analysis, or interpretation of the data; the writing of this manuscript; or the decision to submit the article for publication. The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article. The authors declare that although they are affiliated with a department that is supported financially by a pharmaceutical company, the authors received no current funding for this study, and their department affiliation does not alter their adherence to all the full journal policies on sharing data and materials.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hata, S., Ushigome, E., Hosomi, Y. et al. Impact of continued high blood pressure on the progression of diabetic nephropathy after 10 years: KAMOGAWA-HBP study. Hypertens Res 46, 565–574 (2023). https://doi.org/10.1038/s41440-022-01136-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-01136-3
Keywords
This article is cited by
-
Home blood pressure measurement: the original and the best for predicting the risk
Hypertension Research (2023)
-
Lifetime home BP-centered approach is the core from onset to aggravation of hypertension
Hypertension Research (2023)
-
The clinical significance of home and office blood pressure in diabetic nephropathy
Hypertension Research (2023)