Abstract
The association between the fluctuation in blood pressure (BP) and the early outcomes of patients with subarachnoid hemorrhage (SAH) remains unclear. Our study aimed to evaluate the value of blood pressure variability (BPV) for predicting the short-term outcomes of patients with acute spontaneous SAH. We collected data from 303 patients hospitalized for acute spontaneous SAH. BP values were recorded at admission and subsequently every 2 h during the initial 24 h of hospitalization. BPV was determined as the standard deviation (SD), the difference between the maximum and the minimum (ΔBP), the coefficient of variation (CV), and successive variation (SV). The outcome at discharge was assessed according to the Glasgow Outcome Scale (GOS). The association between BPV and the outcome was identified by multivariable analysis. The findings showed that the parameters of systolic BPV were independently associated with the outcome in a graded fashion. The odds ratios (OR) for the highest tertiles were as follows: SD 13.9 (95% confidence interval [CI], 4.8–40.4), ΔBP 4.4 (95% CI, 1.6–11.9), CV 16.4 (95% CI, 5.6–48.8), SV 15.8 (95% CI, 5.3–46.9). However, there was no association between a poor outcome and diastolic BPV (all p > 0.05). In conclusion, systolic BPV within the first 24 h after admission was independently associated with the outcomes in SAH patients; the greater the variability was, the worse the outcome.
Similar content being viewed by others
Introduction
Subarachnoid hemorrhage (SAH) is a devastating cerebrovascular disease that threatens brain perfusion and function. SAH is a serious and significant health problem, especially given its high rates of mortality and disability and its poor prognosis [1]. Although blood pressure (BP) is regarded as a major parameter for SAH, BP management and the prognostic value of BP during the acute phase of SAH are still controversial [2, 3]. Many recent studies have shown that blood pressure variability (BPV) is a newly defined concept that appears to be a strong predictor of stroke [4,5,6]. However, the relationship between BPV and the clinical outcome of patients with acute SAH remains uncertain, and only a few studies have investigated the prognostic effects of BPV in SAH patients [7,8,9,10]. The degree of BPV in the acute phase of SAH and its relationship with prognosis have not been explored. In our study, within the first 24 h after admission, BP was recorded every 2 h in acute SAH patients, and the BPV parameters were categorized into tertiles. We aimed to investigate the strength of the relationship between BPV and the short-term clinical outcome in patients with acute SAH.
Materials and Methods
Diagnostic criteria and ethics
We retrospectively identified patients with acute spontaneous SAH who were admitted to the Department of Neurology at the First Affiliated Hospital of Guangxi Medical University from January 2015 to May 2018. The diagnosis of spontaneous SAH was made by the patient’s medical history, brain computed tomography, or cerebrospinal fluid examinations. All patients underwent either digital subtraction angiography (DSA) or computed tomographic angiography (CTA) to evaluate the presence of an intracranial aneurysm [11]. The Alcohol Dependence Scale was used to assess excessive drinking [12]. A panel of neurologists and neuroimaging experts worked together to recruit patients for this study. The approval regarding the medical ethics of this study was obtained from the First Affiliated Hospital of Guangxi Medical University (No. 2018 [KY-E-088]). Informed consent was obtained from the patients or their guardians.
Inclusion and exclusion criteria
Patients who met the following criteria were included in the study: (1) patients who were admitted to the hospital within 7 days of the onset of spontaneous SAH; (2) patients whose BP values were recorded at admission and subsequently every 2 h during the initial 24 h in hospital; (3) patients who underwent CT, CTA and DAS examinations at admission; and (4) patients with complete medical data. Patients in any of the situations below were excluded from the study: (1) patients who were admitted to the hospital more than 7 days after symptom onset; (2) patients who died within 24 h of admission; (3) patients who underwent trauma or surgical clipping during the course of SAH; (4) patients who experienced a stroke or other intracranial lesion that was the cause of neurological damage before SAH occurred; (5) patients who had heart failure, renal failure, coagulopathy, malignancies, and serious intercurrent illnesses; and (6) patients who were missing data.
Collection of clinical data
We collected the following data: (1) demographic characteristics, including age and sex; (2) traditional risk factors, such as hypertension, drinking, smoking, the occurrence of stroke, and body mass index, which was calculated as the weight/ height2; (3) the causes of SAH, such as intracranial aneurysm and arteriovenous malformation; (4) the neurological state of the patient at admission (in terms of clinical scoring systems such as the Glasgow Coma Scale [GCS], Hunt and Hess grade, and modified Fisher Scale); (5) the BP readings obtained at 0, 2, 4, 6, 8, 10, 12, 14, 16, 18, 20, 22, and 24 h after admission by an automated electronic device on the nonparetic arm of the supine patient. The average (mean), maximum (max), and minimum (min) values of the 13 systolic and diastolic BP values mentioned above were calculated. The following variability profiles were also calculated: the difference between the maximum and minimum BP values (ΔBP: BPmax − BPmin); the standard deviation (\({\rm{SD}}:\sqrt {\left( {1/\left( {n - 1} \right)\mathop {\sum}\limits_{i = 1}^{n - 1} {\left( {{\rm{BP}}_i - {\rm{BP}}_{{\rm{mean}}}} \right)^2} } \right)}\)), the coefficient of variation (CV [%]: SD/BPmean × 100%), and successive variation (SV), which was calculated as the square root of the average squared difference between 2 successive BP measurements according to the following formula: \({\rm{SV}}:\sqrt {\left( {1/\left( {n - 1} \right)\mathop {\sum}\limits_{i = 1}^{n - 1} {\left( {{\rm{BP}}_{i + 1} - {\rm{BP}}_i} \right)^2} } \right)}\); [13] (6) the blood and imaging examination results, such as the levels of hemoglobin, albumin, creatinine, blood urea nitrogen (BUN), CT, CTA, and DSA; (7) the treatment methods, such as aneurysm embolization and drugs; and (8) the clinical outcome, which was assessed by the modified Rankin Scale (mRS) and the Glasgow Outcome Scale (GOS) at discharge. We further categorized outcomes as favorable (GOS scores 4–5) versus unfavorable (GOS scores 1–3).
Statistical analysis
All statistical analyses were performed with SPSS 19.0 software. Continuous variables values are presented as the mean ± SD, and categorical variables values are presented as the number (percent) of subjects. Quantitative data were analyzed with independent-sample t tests, and qualitative data were analyzed with chi-square tests. To examine the relationship between BPV and the clinical outcome, the analysis of the BPV parameters was repeated using simple dichotomization of the GOS score into 1–3 versus 4–5. The BPV parameters were categorized into tertiles and first analyzed with the Χ2 test for a linear trend. The BPV parameters were then entered into multivariable analysis models after adjusting for the effects of variable confounders. The odds ratios (ORs) and corresponding 95% confidence intervals (CIs) were calculated to evaluate the effects. The results were considered significant if the P value was less than 0.05.
Results
A total of 303 patients with SAH met the inclusion criteria, with 121 (51.16%) males and 119 (48.84%) females. The average age of these 303 patients was 57.04 ± 12.53 years. The average length of hospitalization was 14.8 ± 3.5 days. Favorable outcomes (GOS, 4–5) occurred in 179 (59.08%) patients, and unfavorable outcomes (GOS, 1–3) occurred in 124 (40.92%) patients at discharge. The baseline characteristics and the comparisons of the outcome are summarized in Table 1. When the clinical characteristics of the favorable outcome group were compared with those of the unfavorable outcome group, patients with poor outcomes were older, had a higher body mass index and more frequently had histories of hypertension, aneurysm, and excessive drinking. The neurological status at admission was worse in patients with poor outcomes, as assessed with the GCS, Hunt and Hess grade, and modified Fisher Scale. In the independent-sample t tests, most of the BPV indices (including SBP max–min, SBP SD, SBP CV, DBP max–min, DBP SD, DBP CV, and DBP SV) were significantly higher in patients with poor outcomes than in those with favorable outcomes, with the exception of the SV of systolic BPV (Table 2). Moreover, the mean and maximum SBP and DBP were associated with the outcome as well.
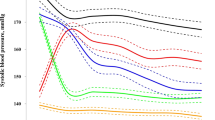
In the Χ2 tests in tertile groups, the systolic and diastolic BPV parameters were all associated in a graded fashion with the outcome (P values ranging from 0.006 to < 0.001, Figs. 1 and 2), while the mean diastolic blood pressure was not associated with the outcome (P value > 0.05, Fig. 2). In the multivariable logistic regression analysis after adjustment for confounding factors, including mean SBP, all 4 systolic BPV parameters were independently associated with the outcome in a graded fashion. The systolic BPV variables in the highest tertile compared with those in the lowest tertile were all associated with higher odds of a poor outcome (4- to 16-fold). The maximum systolic BP was also associated with the outcome (Table 3). However, there was no association between the outcome and diastolic BPV after adjustment for the mean DBP (all p > 0.05, Table 4).
Proportion of patients with favorable outcomes at discharge according to tertiles of the systolic blood pressure variability parameters.The proportion of patients with favorable outcomes decreased significantly across the tertiles of SD, CV, SV, max–min, max, and mean (P values are for the Χ2 test for a linear trend, with the lowest tertile as the reference). SBP systolic blood pressure, SD standard deviation, CV coefficient of variation, SV successive variation, max–min maximum–minimum difference, max maximum, mean average
Proportion of patients with favorable outcomes at discharge according to tertiles of the diastolic blood pressure variability parameters.The proportion of patients with favorable outcomes decreased significantly across the tertiles of SD, CV, SV, max–min, and max. However, the tertiles of mean diastolic blood pressure were not correlated with the outcome (P values are for the Χ2 test for a linear trend, with the lowest tertile as the reference). DBP diastolic blood pressure, SD standard deviation, CV coefficient of variation, SV successive variation, max–min maximum–minimum difference, max maximum; mean, average
Discussion
Hypertension is widely known to be a major risk factor for the development and rupture of cerebral aneurysms [14]. Although the European Stroke Organization suggests that systolic BP in SAH should remain below 180 mm Hg to reduce the risk of rebleeding until the coiling or clipping of ruptured aneurysms can be performed [15], optimal BP thresholds are not well established because of the lack of evidence from randomized trials [16]. In a recent study, BPV was demonstrated to be an important trigger for vascular events [17], and it is also a noninvasive tool that can be used to predict neurological functional outcomes in stroke patients [4, 5]. In 2009, Kirkness et al [7]. continuously monitored BP in 90 patients with SAH for 4 days. The extended GOS was used to assess 6-month functional outcomes after SAH. The results showed that the BPV was more accurate than the mean BP levels for predicting the 6-month outcomes in patients with SAH, and high 24-hour BPV was associated with poor outcomes (P < 0.001). Greater variability in BP was associated with worse outcomes. In 2017, Xu et al [8]. included 368 patients who underwent endovascular coiling to treat SAH, and 308 (83.7%) out of the 368 patients had favorable outcomes. Multivariate analysis was used to analyze the relationship between BPV and prognosis. It was found that systolic BPV is an independent predictor of functional recovery in patients with SAH [8].
In this study, as shown in Table 3, our results were consistent with those of several prior studies [8,9,10], showing that high systolic BPV was independently associated with a poor outcome in patients with SAH. We further found that after categorization into tertiles and adjustment for the mean SBP, the systolic BPV parameters were all strongly associated with the outcome in a graded fashion. However, after adjusting for the mean DBP, there was no association between the outcome and diastolic BPV (Table 4). This finding suggested that fluctuations or changes in SBP during the initial 24-hour after admission in the acute phase of SAH are more critical for determining the prognosis than are fluctuations in DBP.
Several mechanisms may connect BPV during the early period and clinical outcomes. Homeostasis is defined as the ability of the body to maintain a consistent internal environment by regulating its physiological processes and is a healthy adaptive mechanism to maintain physiological variables within the ranges that are compatible with system integrity and function [18]. These variables include heart rate [19] and blood pressure [20]. Excess or insufficient variation in these variables may be present under pathological conditions and could be associated with the disease prognosis [21]. Increased BPV is associated with several factors, including sex, age, and hypertension [22]. Autonomic dysfunction, including sympathetic overactivity and diminished baroreflex sensitivity, may be one of the underlying mechanisms [23]. Cerebral autoregulation is often disturbed in patients with SAH [24, 25]. When autoregulation is affected in patients with SAH, the global cerebral blood flow is passively dependent on the cerebral perfusion pressure and blood viscosity [26]. The greater variability in BP may reflect the worse autoregulation ability under serious conditions, which may be associated with unfavorable outcomes in patients with SAH.
Prior studies analyzed BPV during the initial 24 h after endovascular obliteration of ruptured aneurysms [8, 10], and BP was obtained by invasive monitoring [9]. In our study, we investigated BP and BPV within the first 24 h after admission for the first time and further graded those values during the acute period of SAH. This study uniquely shows a strong association of early systolic BPV with poor outcomes; the greater the variability is, the stronger the association.
However, several limitations in this study need to be mentioned. First, although antihypertensive agents can affect BPV [13], we did not analyze the effects of BP-lowering medication in this study. The findings in our study might be potentially confounded by medication effects and other management decisions. Second, BP was recorded every 2 h, and changes on a smaller time scale could not be detected. Third, the optimal BP levels for the management of acute SAH remained unknown. Fourth, the relationship between BPV and long-term outcomes in patients with SAH was not studied. Finally, the single-center retrospective design could limit the validity of the results.
Conclusion
The results of our study show that high systolic BPV during the first 24 h after admission in patients with acute spontaneous SAH was independently associated with a poor outcome at discharge (two weeks); the greater the variability is, the stronger the association. Close monitoring of BP is important during the acute phase of SAH. The stabilization of systolic BPV during this vulnerable period may be a promising therapeutic target for the management of SAH.
References
NieuwkLancamp DJ, Setz LE, Algra A, Linn FH, de Rooij NK, Rinkel GJ. Changes in case fatality of aneurysmal subarachnoid haemorrhage over time, according to age, sex, and region: a metaanalysis. Lancet Neurol. 2009;8:635–42.
Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Engl J Med. 2006;354:387–96.
Rosengart AJ, Schultheiss KE, Tolentino J, Macdonald RL. Prognostic factors for outcome in patients with aneurysmal subarachnoid hemorrhage. Stroke. 2007;38:2315–21.
Manning L, Hirakawa Y, Arima H, Wang X, Chalmers J, Wang J, Lindley R, Heeley E, Delcourt C, Neal B, Lavados P. Blood pressure variability and outcome after acute intracerebral haemorrhage: a post-hoc analysis of INTERACT2, a randomised controlled trial. Lancet Neurol. 2014;13:364–73.
Zhang Y, Wang H, Xu K, Wang P, Li XY, Zhao JB, Tang Y. Ambulatory blood pressure variability within the first 24 h after admission and outcomes of acute ischemic stroke. J Am Soc Hypertens. 2018;12:195–203.
Chung PW, Kim JT, Sanossian N, Starkmann S, Hamilton S, Gornbein J, Conwit R, Eckstein M, Pratt F, Stratton S. Association between hyperacute stage blood pressure variability and outcome in patients with spontaneous intracerebral hemorrhage. Stroke. 2018;49:348–54.
Kirkness CJ, Burr RL, Mitchell PH. Intracranial and blood pressure variability and long-term outcome after aneurysmal sub-arachnoid hemorrhage. Am J Crit Care. 2009;18:241–51.
Xu B, Ji Q, Zhang Y, Shen L, Cao M, Cai K. Postoperative blood pressure variability exerts an influence on clinical outcome after coil embolization of ruptured intracranial aneurysms. Neurol Res. 2017;39:813–18.
Beseoglu K, Unfrau K, Steiger HJ, Hänggi D. Influence of blood pressure variability on short-term outcome in patients with subarachnoid hemorrhage. Cent Eur Neurosurg. 2010;71:69–74.
Cai K, Zhang Y, Shen L, Ji Q, Xu T, Cao M. Characteristics of blood pressure profiles after endovascular coiling as predictors of clinical outcome in poor-grade aneurysmal subarachnoid hemorrhage. World Neurosurg. 2017;104:459–66.
Connolly ES, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, Hoh BL, Kirkness CJ, Naidech AM. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke. 2012;43:1711–37.
Skinner HA, Allen BA. Alcohol dependence syndrome: measurement and validation. J Abnorm Psychol. 1982;91:199–209.
Tanaka E, Koga M, Kobayashi J, Kario K, Kamiyama K, Furui E, Shiokawa Y, Hasegawa Y, Okuda S, Todo K, Kimura K. Blood pressure variability on antihypertensive therapy in acute intracerebral hemorrhage: the Stroke Acute Management with Urgent Risk-factor Assessment and Improvement-intracerebral hemorrhage study. Stroke. 2014;45:2275–79.
Tanaka E, Koga M, Kobayashi J, Kario K, Kamiyama K, Furui E, Shiokawa Y, Hasegawa Y, Okuda S, Todo K, Kimura K. Subarachnoid hemorrhage and intracerebral hematoma: incidence, prognostic factors, and outcome. Neurosurgery. 2008;63:1088–93..
Steiner T, Juvela S, Unterberg A, Jung C, Forsting M, Rinkel G. European stroke organization guidelines for the management of intracranial aneurysms and subarachnoid haemorrhage. Cereb Dis. 2013;35:93–112.
Carcel C, Sato S, Anderson CS. Blood pressure management in intracranial hemorrhage: current challenges and opportunities. Curr Treat Options Cardiovasc Med. 2016;18:e259.
Rothwell PM. Limitations of the usual blood-pressure hypothesis and importance of variability, instability, and episodic hypertension. Lancet. 2010;375:938–48.
Lin QS, Ping-Chen, Lin YX, Lin ZY, Yu LH, Dai LS, Kang DZ. Systolic blood pressure variability is a novel risk factor for rebleeding in acute subarachnoid hemorrhage: a case-control study. Medicine. 2016;95:e3028.
West BJ, Shlesinger M. The noise in natural phenomena. Am Sci. 1990;78:40–8.
Kleiger RE, Miller JP, Bigger JT, Moss AJ. Decreased heart rate variability and its association with increased mortality after myocardial infarction. Am J Cardiol. 1987;59:256–62.
Wagner CD, Persson PB. Two ranges in blood pressure power pectrum with different l/f characteristics. Am J Physiol Heart Circ Physiol. 1994;267:H449–54.
Kato T, Kikuya M, Ohkubo T, Satoh M, Hara A, Obara T, Metoki H, Asayama K, Hirose T, Inoue R, Kanno A, Totsune K. Factors associated with day-by-day variability of self-measured blood pressure at home: the Ohasama study. Am J Hypertens. 2010;23:980–6.
Grassi G, Bombelli M, Seravalle G, Dell’Oro R, Quarti-Trevano F. Diurnal blood pressure variation and sympathetic activity. Hypertens Res. 2010;33:381–5.
Que CL, Kenyon CM, Olivenstein R, Macklem PT, Maksym GN. Homeokinesis and short-term variability of human airway caliber. J Appl Physiol. 2001;91:1131–41.
Jaeger M, Schuhmann MU, Soehle M, Nagel C, Meixensberger J. Continuous monitoring of cerebrovascular autoregulation after subarachnoid hemorrhage by brain tissue oxygen pressure reactivity and its relation to delayed cerebral infarction. Stroke. 2007;38:981–6.
Kai H, Kudo H, Takayama N, Yasuoka S, Aoki Y, Imaizumi T. Molecular mechanism of aggravation of hypertensive organ damages by short-term blood pressure variability. Curr Hypertens Rev. 2014;10:125–33.
Funding
This study was supported by grants from the Natural Science Foundation of China (81560205 and 81760217), the Guangxi Natural Science Foundation (2017GXNSFAA198135), the High-Level Medical Expert Training Program of Guangxi “139” Plan Funding, and the Guangxi Colleges and Universities Science and Technology Research Project (KY2015ZD030).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yang, M., Pan, X., Liang, Z. et al. Association between blood pressure variability and the short-term outcome in patients with acute spontaneous subarachnoid hemorrhage. Hypertens Res 42, 1701–1707 (2019). https://doi.org/10.1038/s41440-019-0274-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0274-y
Keywords
This article is cited by
-
The impact of blood pressure variability on the development of parenchymal hematoma in acute cerebral infarction with atrial fibrillation
Hypertension Research (2024)
-
The L-shaped correlation between systolic blood pressure and short-term and long-term mortality in patients with cerebral hemorrhage
BMC Neurology (2023)
-
Guidelines for the Neurocritical Care Management of Aneurysmal Subarachnoid Hemorrhage
Neurocritical Care (2023)
-
ED BP Management for Subarachnoid Hemorrhage
Current Hypertension Reports (2022)
-
Impact of in-hospital blood pressure variability on clinical outcomes in patients with symptomatic peripheral arterial disease
Hypertension Research (2021)