Abstract
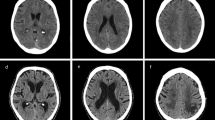
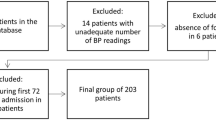
Although blood pressure variability (BPV) and reperfusion are associated with parenchymal hematoma (PH) after stroke, the relationship between BPV and PH in atrial fibrillation (AF) patients who are at risk of reperfusion injury with frequent spontaneous recanalization is unknown. This study aimed to investigate whether BPV within the first 48 h is associated with PH within 72 h in patients with AF and stroke in terms of major vessel occlusion status. A total of 131 patients with AF that were admitted within 24 h after stroke onset were enrolled. PH was defined as a confluent hemorrhage with mass effect. The maximum (max), minimum (min), and average blood pressure (BP) during the first 48 h after admission were calculated. BPV was analyzed by using range between maximum and minimum (max–min), successive variation (SV), standard deviation (SD), and coefficient of variation (CV). All parameters were applied for systemic (SBP), diastolic (DBP), and pulse pressure (PP). After adjusting for confounding variables, various BPV parameters were associated with PH, including SBPmax (p = 0.0426), SBPSV (p = 0.0006), DBPmax-min (p = 0.0437), DBPSV (p = 0.0358), DBPSD (p = 0.0393), PPmax-min (p = 0.0478), PPSV (p < 0.0001), PPSD (p = 0.0034), and PPCV (p = 0.0120). The relationship remained significant in patients with a patent major vessel responsible for infarction but not in patients with an occluded major vessel. In conclusion, this study revealed that high BPV was associated with PH in patients with AF and acute stroke, particularly for those with a patent major vessel. The control of BP and BPV after stroke may be considered in patients with AF.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Fiorelli M, Bastianello S, von Kummer R, del Zoppo GJ, Larrue V, Lesaffre E, et al. Hemorrhagic transformation within 36 h of a cerebral infarct: relationships with early clinical deterioration and 3-month outcome in the European Cooperative Acute Stroke Study I (ECASS I) cohort. Stroke. 1999;30:2280–4.
Paciaroni M, Agnelli G, Corea F, Ageno W, Alberti A, Lanari A, et al. Early hemorrhagic transformation of brain infarction: rate, predictive factors, and influence on clinical outcome: results of a prospective multicenter study. Stroke. 2008;39:2249–56.
Simard JM, Kent TA, Chen M, Tarasov KV, Gerzanich V. Brain oedema in focal ischaemia: molecular pathophysiology and theoretical implications. Lancet Neurol. 2007;6:258–68.
Stokum JA, Gerzanich V, Simard JM. Molecular pathophysiology of cerebral edema. J Cereb Blood Flow Metab. 2016;36:513–38.
Ko Y, Park JH, Yang MH, Ko SB, Han MK, Oh CW, et al. The significance of blood pressure variability for the development of hemorrhagic transformation in acute ischemic stroke. Stroke. 2010;41:2512–8.
Yong M, Kaste M. Association of characteristics of blood pressure profiles and stroke outcomes in the ECASS-II trial. Stroke. 2008;39:366–72.
Liu K, Yan S, Zhang S, Guo Y, Lou M. Systolic blood pressure variability is associated with severe hemorrhagic transformation in the early stage after thrombolysis. Transl Stroke Res. 2016;7:186–91.
Kim TJ, Park HK, Kim JM, Lee JS, Park SH, Jeong HB, et al. Blood pressure variability and hemorrhagic transformation in patients with successful recanalization after endovascular recanalization therapy: a retrospective observational study. Ann Neurol. 2019;85:574–81.
Khatri R, McKinney AM, Swenson B, Janardhan V. Blood-brain barrier, reperfusion injury, and hemorrhagic transformation in acute ischemic stroke. Neurology. 2012;79:S52–7.
Yang P, Song L, Zhang Y, Zhang X, Chen X, Li Y, et al. Intensive blood pressure control after endovascular thrombectomy for acute ischaemic stroke (ENCHANTED2/MT): a multicentre, open-label, blinded-endpoint, randomised controlled trial. Lancet. 2022;400:1585–96.
Matusevicius M, Cooray C, Bottai M, Mazya M, Tsivgoulis G, Nunes AP, et al. Blood pressure after endovascular thrombectomy: modeling for outcomes based on recanalization status. Stroke. 2020;51:519–25.
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute Ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50:e344–418.
Sun J, Lam C, Christie L, Blair C, Li X, Werdiger F, et al. Risk factors of hemorrhagic transformation in acute ischaemic stroke: a systematic review and meta-analysis. Front Neurol. 2023;14:1079205.
Tu HT, Campbell BC, Christensen S, Desmond PM, De Silva DA, Parsons MW, et al. Worse stroke outcome in atrial fibrillation is explained by more severe hypoperfusion, infarct growth, and hemorrhagic transformation. Int J Stroke. 2015;10:534–40.
Aryal R, Patabendige A. Blood-brain barrier disruption in atrial fibrillation: a potential contributor to the increased risk of dementia and worsening of stroke outcomes? Open Biol. 2021;11:200396.
Molina CA, Montaner J, Abilleira S, Ibarra B, Romero F, Arenillas JF, et al. Timing of spontaneous recanalization and risk of hemorrhagic transformation in acute cardioembolic stroke. Stroke. 2001;32:1079–84.
Adams HP Jr., Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in acute stroke treatment. Stroke. 1993;24:35–41.
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol. 1987;149:351–6.
Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet. 2000;355:1670–4.
Neuberger U, Kickingereder P, Schonenberger S, Schieber S, Ringleb PA, Bendszus M, et al. Risk factors of intracranial hemorrhage after mechanical thrombectomy of anterior circulation ischemic stroke. Neuroradiology. 2019;61:461–9.
Alvarez-Sabin J, Maisterra O, Santamarina E, Kase CS. Factors influencing haemorrhagic transformation in ischaemic stroke. Lancet Neurol. 2013;12:689–705.
Zhang J, Yang Y, Sun H, Xing Y. Hemorrhagic transformation after cerebral infarction: current concepts and challenges. Ann Transl Med. 2014;2:81.
Yang M, Pan X, Liang Z, Huang X, Duan M, Cai H, et al. Association between blood pressure variability and the short-term outcome in patients with acute spontaneous subarachnoid hemorrhage. Hypertens Res. 2019;42:1701–7.
Kamieniarz-Medrygal M, Lukomski T, Kazmierski R. Short-term outcome after ischemic stroke and 24-h blood pressure variability: association and predictors. Hypertens Res. 2021;44:188–96.
Toyoda K, Yamagami H, Kitagawa K, Kitazono T, Nagao T, Minematsu K, et al. Blood pressure level and variability during long-term prasugrel or clopidogrel medication after stroke: PRASTRO-I. Stroke. 2021;52:1234–43.
Nepal G, Shrestha GS, Shing YK, Muha A, Bhagat R. Systolic blood pressure variability following endovascular thrombectomy and clinical outcome in acute ischemic stroke: a meta-analysis. Acta Neurol Scand. 2021;144:343–54.
Avolio AP, Kuznetsova T, Heyndrickx GR, Kerkhof PLM, Li JK. Arterial flow, pulse pressure and pulse wave velocity in men and women at various ages. Adv Exp Med Biol. 2018;1065:153–68.
Levin RA, Carnegie MH, Celermajer DS. Pulse pressure: an emerging therapeutic target for dementia. Front Neurosci. 2020;14:669.
Park JH, Lee J, Kwon SU, Sung Kwon H, Hwan Lee M, Kang DW. Elevated pulse pressure and recurrent hemorrhagic stroke risk in stroke with cerebral microbleeds or intracerebral hemorrhage. J Am Heart Assoc. 2022;11:e022317.
Selker HP, Beshansky JR, Schmid CH, Griffith JL, Longstreth WT Jr., O’Connor CM, et al. Presenting pulse pressure predicts thrombolytic therapy-related intracranial hemorrhage. Thrombolytic Predictive Instrument (TPI) Project results. Circulation. 1994;90:1657–61.
Katsanos AH, Alexandrov AV, Mandava P, Kohrmann M, Soinne L, Barreto AD, et al. Pulse pressure variability is associated with unfavorable outcomes in acute ischaemic stroke patients treated with intravenous thrombolysis. Eur J Neurol. 2020;27:2453–62.
Kamieniarz-Medrygal M, Kazmierski R. Significance of pulse pressure variability in predicting functional outcome in acute ischemic stroke: a retrospective, single-center, observational cohort study. Sci Rep. 2023;13:3618.
Magoufis G, Safouris A, Raphaeli G, Kargiotis O, Psychogios K, Krogias C, et al. Acute reperfusion therapies for acute ischemic stroke patients with unknown time of symptom onset or in extended time windows: an individualized approach. Ther Adv Neurol Disord. 2021;14:17562864211021182.
Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al. Apixaban versus warfarin in patients with atrial fibrillation. N. Engl J Med. 2011;365:981–92.
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N. Engl J Med. 2009;361:1139–51.
Mehta RH, Cox M, Smith EE, Xian Y, Bhatt DL, Fonarow GC, et al. Race/Ethnic differences in the risk of hemorrhagic complications among patients with ischemic stroke receiving thrombolytic therapy. Stroke. 2014;45:2263–9.
Shen AY, Yao JF, Brar SS, Jorgensen MB, Chen W. Racial/ethnic differences in the risk of intracranial hemorrhage among patients with atrial fibrillation. J Am Coll Cardiol. 2007;50:309–15.
Acknowledgements
This study was supported by a grant from the Kaohsiung Medical University Hospital (grant numbers: KMUH111–1M51). The authors thank the help from Dr. Ming-Yen Lin, a biostatistician in the Division of Medical Statistics and Bioinformatics, Department of Medical Research, Kaohsiung Medical University Hospital, Kaohsiung Medical University.
Funding
This study was supported by a grant from the Kaohsiung Medical University Hospital (grant numbers: KMUH111–1M51), but this funding source had no involvement of study design, collection, analysis, and interpretation of results, writing of the report or any restrictions regarding submission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, MN., Liu, YP., Fong, YO. et al. The impact of blood pressure variability on the development of parenchymal hematoma in acute cerebral infarction with atrial fibrillation. Hypertens Res 47, 618–627 (2024). https://doi.org/10.1038/s41440-023-01479-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01479-5
Keywords
This article is cited by
-
Preface-various factors in the management of blood pressure
Hypertension Research (2024)
-
Blood pressure variability in acute ischemic stroke
Hypertension Research (2024)