Abstract
Orthosiphon stamineus Benth. (Lambiaceae) is an important traditional plant for the treatment of hypertension. Previous studies have demonstrated that the sinensetin content in O. stamineus is correlated with its vasorelaxant activity. However, there is still very little information regarding the vasorelaxant effect of sinensetin due to a lack of scientific studies. Therefore, the present study was designed to investigate the underlying mechanism of action of sinensetin in vasorelaxation using an in vitro precontraction aortic ring assay. The changes in the tension of the aortic ring preparations were recorded using a force–displacement transducer and the PowerLab system. The mechanisms of the vasorelaxant effect of sinensetin were determined in the presence of antagonists. Sinensetin caused relaxation of the aortic ring precontracted with PE in the presence and absence of the endothelium and with potassium chloride in endothelium-intact aortic rings. In the presence of Nω-nitro-L-arginine methyl ester (nitric oxide synthase inhibitor), methylene blue (cyclic guanosine monophosphate lowering agent), ODQ (selective soluble guanylate cyclase inhibitor), indomethacin (a nonselective cyclooxygenase inhibitor), tetraethylammonium (nonselective calcium activator K+ channel blocker), 4-aminopyridine (voltage-dependent K+ channel blocker), barium chloride (inwardly rectifying Kir channel blocker), glibenclamide (nonspecific ATP-sensitive K+ channel blocker), atropine (muscarinic receptor blocker), or propranolol (β-adrenergic receptor blocker), the relaxation stimulated by sinensetin was significantly reduced. Sinensetin was also active in reducing Ca2+ release from the sarcoplasmic reticulum (via IP3R) and in blocking calcium channels (VOCC). The present study demonstrates the vasorelaxant effect of sinensetin, which involves the NO/sGC/cGMP and indomethacin pathways, calcium and potassium channels, and muscarinic and beta-adrenergic receptors.
Similar content being viewed by others
Introduction
Orthosiphon stamineus is a medicinal plant that is widely used in Southeast Asia, especially in Malaysia, for the treatment of hypertension and kidney stones. In clinical studies, it has been tested as an additional regimen for antihypertensive treatment [1]. Our previous results have shown that the chloroform fraction of O. stamineus, which contains 4.6% eupatorin and 2.99% sinensetin, possesses considerable vasorelaxant effects in an in vitro isolated rat aorta model [2]. The most noteworthy result is from the statistical analysis, which revealed that the amount of eupatorin and sinensetin in the fractions correlated with the strength of their vasorelaxant effects. After comparing the amount of eupatorin in the chloroform fraction of O. stamineus with its vasorelaxation, we found that eupatorin is not the only active ingredient that contributes to the vasorelaxant effect of O. stamineus [3]. Xu and colleagues suggested that flavonoids are required to have 5-OH (i), 7-OH (ii), 4′-OH (iii), C2═C3 (iv), and C4═O (v) configurations in order to possess significant vasorelaxant activity [4]. Considering its chemical structure, sinensetin fulfilled criteria (iv) and (v); therefore, we hypothesized that sinensetin (Fig. 1) may be one of the active ingredients of O. stamineus that contributes to its vasorelaxant activity. Hence, we designed the present study to investigate the vasorelaxant effect and the mechanism of action of sinensetin.
Materials and methods
Acetylcholine (ACh), nifedipine, and phenylephrine (PE) were purchased from Acros Organics (Belgium). Nω-nitro-L-arginine methyl ester (L-NAME), indomethacin, tetraethylammonium (TEA), barium chloride (BaCl2), glibenclamide, 1H-[1,2,4]oxadiazolo[4,3-a]quinoxalin-1-one (ODQ), 2-aminoethyl diphenylborinate (2-APB), atropine, sinensetin, and propranolol were purchased from Sigma Aldrich (USA). 4-Aminopyridine was purchased from Merck (Germany). Ethylene glycol tetraacetic acid (EGTA) was purchased from Calbiochem (Germany). Methylene blue was purchased from Promedipharm Sdn. Bhd. (Malaysia). All the chemicals (blockers or antagonists) were dissolved in distilled water, except sinensetin, indomethacin, nifedipine, ODQ, 2-APB, and glibenclamide, which were dissolved in 1% Tween 80.
Animals
Healthy adult male Sprague–Dawley rats (200–240 g) were used in this experiment. The animals were kept under a 12/12 h light/dark cycle and were allowed free access to food and water. The investigation conforms to the Guide for the Care and Use of Laboratory Animal by the Universiti Sains Malaysia and Fujian University of Tradition Chinese Medicine. All the procedures described herein were approved by the Animal Ethics Committee USM; Animal Ethics Approval No.: USM/Animal Ethics Approval/2016/(103)(772).
Preparation of aortic rings
Healthy male Sprague–Dawley rats, weighing 250–300 g, were used in this experiment. The rats were restrained in a restrainer and were administered 8 psi of CO2 for 2 min for euthanasia. The aorta was excised carefully and immersed in Krebs–Henseleit (Krebs’) solution in a Petri dish. The aorta was gently drained with Krebs’ solution to remove excess blood and the adjoining tissue and fat. The isolated aorta was then cut into 3–5 mm long segments. The clean aortic ring was incubated in an organ bath containing 10 mL Krebs’ solution, which was continuously aerated with carbogen (95% O2 and 5% CO2) at 37 °C. The suspended aortic ring was allowed to equilibrate for 30 min under a tension of 1 g. The Krebs’ solution was replaced every 10 min, and the tension was readjusted to 1 g if necessary. The condition of the aortic ring endothelium was tested by precontracting the ring using PE (1 µM), followed by relaxation with the addition of ACh (1 µM). Aortic rings that produced more than 60% relaxation in response to ACh were considered to be endothelium intact. In some preparations, the endothelium was mechanically removed, and the removal was confirmed by the absence of relaxation or relaxation of less than 10% with ACh treatment (1 µM) after being precontracted with PE (1 µM). The aortic ring was then rinsed with Krebs’ solution at least three times to allow the tension to return to baseline before it was precontracted with PE. When the contraction achieved a plateau, a concentration–response curve was produced from the cumulative addition of sinensetin (100 µL of 0.125–4 mg/mL equivalent to 0.3–2.11 µM, pipetted into the organ bath) at 20 min intervals for each concentration. The tension was measured using the PowerLab system (AD Instrument, Australia) equipped with a force–displacement transducer (GRASS Force–Displacement Transducer FT03 C) and LabChart 5 (AD Instrument, Australia).
Vasorelaxation, which is a measure of the inhibition of contraction in aortic rings precontracted with PE or KCl (60 mM), was determined as the percentage and was calculated as follows:
where Ci = the contraction of aortic rings with treatment; and C0 = plateau contraction of aortic rings after being precontracted with PE.
Determination of the effect of sinensetin on PE-induced contraction in the presence of indomethacin, L-NAME, methylene blue, ODQ, or indomethacin
To determine the effects of PGI2, NO, sGC, and cGMP on the vasorelaxant activity of sinensetin, endothelium-intact aortic rings were incubated with indomethacin (COX inhibitor) (10 μM), L-NAME (NO synthase inhibitor) (10 μM), ODQ (sGC inhibitor) (10 μM), or methylene blue (cGMP-lowering agent) (10 μM) for 20 min prior to precontraction with PE. Comparisons were made between the cumulative concentration–response of sinensetin on the aortic rings with and without preincubation with the above-mentioned inhibitors [5].
Determination of the effect of sinensetin on PE-induced contraction in the presence of K+ channel blockers
To determine the involvement of K+ channels in the vasorelaxant effect of sinensetin, TEA (KCa blocker) (1 mM), 4-AP (KV blocker) (1 mM), BaCl2 (Kir blocker) (10 μM), or glibenclamide (nonselective KATP) (10 μM) was applied to endothelium-intact aortic rings for 20 min prior to precontraction with PE. Comparisons were made between the cumulative concentration–response of sinensetin on the aortic rings with and without pre-incubation with the above-mentioned inhibitors [6, 7].
Determination of the effect of sinensetin on extracellular calcium-induced vasoconstriction
To determine the effect of sinensetin on L-type calcium channels, three sets of experiments were conducted, namely control, nifedipine, and sinensetin groups. For the control, the endothelium-intact aortic rings were allowed to stabilize in normal Krebs’ solution for 30 min. The solution was then replaced with Ca2+-free Krebs’ solution containing EGTA (0.2 mM) for 30 min (the solution in the organ bath was washed and replaced twice, 15 min each) in order to remove Ca2+ from the tissues. The aortic rings were then rinsed in Ca2+-free, K+-rich (50 mM) Krebs’ solution for 30 min (the solution in the organ bath was washed and replaced twice, 15 min each). Next, Ca2+ (0.01–10.0 mM) was added cumulatively into the organ bath at 3 min intervals. For the nifedipine group, the effects of cumulative additions of Ca2+ (0.01–10.0 mM) into the organ bath were recorded for 3 min at each concentration prior to incubation with nifedipine (0.1, 0.3, and 1 µM) for 20 min. The experiment for the sinensetin group was conducted in a manner similar to that for the nifedipine group; however, the aortic ring was pre-incubated with sinensetin (0.04, 0.15, and 0.58 µM) instead of nifedipine before contraction with Ca2+ [7].
Determination of the effect of sinensetin on intracellular Ca2+ release
The experiment was conducted to determine the relaxant effect of sinensetin on the inhibition of intracellular Ca2+ release. Endothelium-denuded aortic rings were allowed to stabilize in Ca2+-free Krebs’ solution for 20 min. The Krebs’ solution was then replaced with EGTA (0.2 mM) and Ca2+-free Krebs’ solution for 10 min. The aortic rings were pre-incubated with sinensetin (0.04, 0.15, and 0.58 µM) or 2-APB (100 µM) for 20 min before PE (1 µM) was added. The group that did not involve incubation with sinensetin was considered the control [5].
Determination of the effect of sinensetin on PE-induced contraction in the presence of propranolol and atropine
The effects of sinensetin on muscarinic and β-adrenergic receptors were assessed using endothelium-intact aortic rings. The experiments were designed to trigger the effect of sinensetin as either a vasodilator or an agonist when bound to these two receptors. The aortic rings were pre-incubated with either atropine (1 µM) (antagonist of muscarinic receptor) or propranolol (1 µM) (antagonist of β-adrenergic receptor) for 20 min prior to precontraction with PE. Comparisons were made between the cumulative concentration–response of sinensetin on aortic rings with and without pre-incubation with the above-mentioned inhibitors and the control.
Statistical analysis
The values are expressed as the mean ± S.D. Statistical analysis was performed using one-way ANOVA, and Dunnett’s post-hoc test was conducted using SPSS version 20 software. All tests were two-tailed, and the significance was set at P < 0.05. The pD2 value was calculated using the formula pD2 = −log(EC50), where EC50 is the concentration that produces the half-maximal response. The data were then tabulated using Microsoft Excel 2013.
Results
Sinensetin (0.03–2.11 µM) caused concentration-dependent vasorelaxation of PE-contracted endothelium-intact aortic rings (pD2 = 6.97 ± 0.09 and Emax = 108 ± 9.83%) (Fig. 2). Further experiments were conducted to study the precise mechanisms involved in the vasorelaxant effect of sinensetin by utilizing endothelium-denuded preparations of rat aortic rings. As shown in Fig. 2, vasorelaxation was significantly attenuated by endothelial denudation (pD2 < 4.68 and Emax = 31.38 ± 5.09%) (Table 1). In addition to using PE to evoke contraction, the vasorelaxant effect of sinensetin was studied on KCl-constricted aortic rings (pD2 = 6.33 ± 0.22 and Emax = 70.97 ± 12.07%) (Fig. 3) (Table 1).
Role of endothelial factors in the vasorelaxant effects of sinensetin
As shown in Fig. 4, the vasorelaxant activity of sinensetin was significantly reduced by not only indomethacin (pD2 = 6.73 ± 0.18 and Emax = 101.32 ± 8.14%) (Table 1) but also L-NAME, ODQ, and methylene blue with pD2 values of 6.42 ± 0.05, 6.18 ± 0.13, and 5.52 ± 0.36, respectively, and Emax values of 75.46 ± 5.48%, 76.72 ± 5.94%, and 52.69 ± 7.67%, respectively (Table 1).
Original isometric force recordings showing the influence of indomethacin, L-NAME, methylene blue, and ODQ (a) on the vasorelaxant effect of sinensetin in endothelium-intact aortic rings (N = 8) (b). ** and *** indicate significance at P < 0.01 and P < 0.001, respectively, compared to the endothelium-intact aortic ring group
Role of K+ channels in sinensetin-induced vasorelaxation
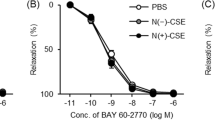
As seen in Fig. 5, 4-AP showed the strongest inhibition of the vasorelaxant effect exerted by sinensetin among the potassium channel antagonists, with pD2 = 6.58 ± 0.11 and Emax = 88.5 ± 7.67%. TEA and glibenclamide significantly reduced the vasorelaxant activity of sinensetin, with pD2 and Emax values of 6.66 ± 0.11 and 105.64 ± 7.37%, respectively, for TEA and 6.74 ± 0.15 and 93.9 ± 10.4%, respectively, for glibenclamide (Fig. 5) (Table 1). On the other hand, sinensetin-induced vasorelaxation was slightly affected by BaCl2 (pD2 = 6.86 ± 0.20 and Emax = 100 ± 5.35%) (Fig. 5) (Table 1).
Original isometric force recordings showing the influence of TEA, 4-AP, glibenclamide, and BaCl2 (a) on the vasorelaxant effect of sinensetin in endothelium-intact aortic rings (N = 8) (b). *, **, and *** indicate significance at P < 0.05, P < 0.01, and P < 0.001, respectively, compared to the endothelium-intact aortic ring group
Role of β-adrenergic and muscarinic receptors in sinensetin-induced vasorelaxation
Figures 6 and 7 show the effects of atropine and propranolol on vasorelaxation by sinensetin. Atropine and propranolol significantly decreased the vasorelaxation effect of sinensetin, with pD2 and Emax values of 6.64 ± 0.13 and 102.66 ± 8.92%, respectively, for atropine and 6.71 ± 0.13 and 95.4 ± 8.35%, respectively, for propranolol.
Original isometric force recordings showing the influence of propranolol (a) on the vasorelaxant effect of sinensetin in endothelium-intact aortic rings (N = 8) (b). *, **, and *** indicate significance at P < 0.05, P < 0.01, and P < 0.001, respectively, compared to the endothelium-intact aortic ring group
Role of calcium channels in sinensetin-induced vasorelaxation
As depicted in Fig. 8, sinensetin (0.04, 0.15, and 0.58 µM) and nifedipine (0.1, 0.3, and 1 µM) significantly reduced the increase in contraction caused by the addition of calcium ions into the organ bath chamber. The maximum contraction elicited by 3 mM calcium ion was 0.838 ± 0.10, and this was diminished to 0.1 ± 0.02, 0.06 ± 0.02, and 0.03 ± 0.02 g by nifedipine at 0.1, 0.3 and 1 µM, respectively. Sinensetin at 0.04, 0.15, and 0.58 µM also produced concentration-dependent vasorelaxation of 0.65 ± 0.06, 0.43 ± 0.12, and 0.31 ± 0.02 g, respectively, in aortic rings treated with 3 mM calcium (Fig. 8). In the intracellular calcium release study, PE induced transient contraction of 0.86 ± 0.09 g due to the release of Ca2+ from the sarcoplasmic reticulum. Pre-incubation of the aortic rings with sinensetin at concentrations of 0.04, 0.15, and 0.58 µM significantly attenuated PE-induced contraction to 0.57 ± 0.08, 0.37 ± 0.08, and 0.115 ± 0.04 g, respectively. 2-APB at 100 µM also significantly decreased the vasorelaxant effect to 0.02 ± 0.03 g (Fig. 9).
Vasorelaxant effect of sinensetin on PE-precontracted endothelium-intact aortic rings in Ca2+-free Krebs’ solution (N=8) (b). Original isometric force recordings showing the influence of 0.04, 0.15, and 0.58 μM of sinensetin on the vasorelaxant effect (a) in endothelium-denuded aortic rings in Ca2+-free Krebs’ solution.
Discussion
Vascular tone is strictly regulated by both the vascular endothelium and smooth muscles via stimulation by internal or external vasoactive compounds acting on channels, receptors, or enzymes in the blood [8, 9]. In the preliminary screen, sinensetin exhibited a concentration-dependent vasorelaxant effect on endothelium-intact aortic rings. This vasorelaxant effect was significantly decreased in endothelium-denuded aortic rings. These findings indicate that the vasorelaxant effect mediated by sinensetin is not solely dependent on the endothelium but may be partially affected by endothelium-independent relaxing factors. Therefore, it can be concluded that sinensetin exerts its effects via multiple mechanisms, including the antagonization of aortic ring contraction through direct (endothelium-independent) and indirect (endothelium-dependent) vasorelaxation.
Vasoactive substances produced by the endothelium to cause vasorelaxation are known as endothelium-derived relaxing factors (EDRFs), which include nitric oxide (NO), prostacyclin (PGI2), and endothelium-derived hyperpolarizing factors (EDHFs). Among these three EDRFs, NO and PGI2 have been well-characterized, which is the main reason that the NO and PGI2 pathways were probed in the vasorelaxation studies of sinensetin. The results from the aortic ring preparations pre-incubated with L-NAME, ODQ, or methylene blue showed a significant reduction in the vasorelaxant effect of sinensetin. This finding suggests that the NO/sGC/cGMP pathways are involved in the vasorelaxant effect of sinensetin. NO is a potent vasodilator produced from L-arginine by eNOS in the endothelium. The vasorelaxant effect of NO is obvious only when it diffuses from the endothelium into smooth muscles through adjacent vascular smooth muscles. NO stimulates soluble guanylyl cyclase (sGC) to convert guanosine triphosphate (GTP) into cyclic 3′,5′-guanosine monophosphate (cGMP) [10]. Hence, the intracellular increase in cGMP activates protein kinase G to decrease the intracellular calcium concentration in smooth muscles, hence promoting the relaxation of vascular smooth muscle cells (VSMCs). Moreover, in VSMCs, NO indirectly stimulates the activation of the KCa, Kir, and KV channels. With the activation of these channels, the efflux of potassium is increased, which results in membrane potential hyperpolarization, causing the closure of voltage-operated calcium channels. This in turn decreases Ca2+ influx, and vasodilatation occurs [11].
In addition to NO, PGI2 is an important EDRF that is involved in regulating vascular tone. PGI2 is produced from the intermediate prostaglandin H2 via catalysis by prostacyclin synthase, while the intermediate prostaglandin H2 is synthesized by COX. Because PGI2 is the key factor in the regulation of vasorelaxation, the effect of sinensetin on PGI2-dependent relaxation was also studied. Indomethacin had an effect on the vasorelaxant effect of sinensetin, which suggests that the PGI2 pathway might have contributed to its effect.
In addition, the muscarinic acetylcholine receptor (M3) plays an important role in the regulation of vasorelaxation. Even though M3 receptors are found in both the endothelium and vascular smooth muscle, the Gαq-protein-coupled receptor is much more dominant in the endothelium than in vascular smooth muscle. Therefore, the vasorelaxant effect of acetylcholine was significantly reduced when the endothelium of the aortic ring was removed. Activation of the M3 receptor stimulates the phospholipase C (PLC) signaling pathway cascade to produce both secondary messengers, IP3 and DAG, which results in an increased concentration of Ca2+ in the cytosol of the endothelium. These events are followed by the formation of calcium-calmodulin complexes, thus causing vasorelaxation [12, 13]. Atropine was shown to significantly reduce the vasorelaxant effect of sinensetin. Therefore, the results suggest that sinensetin employs muscarinic receptors to exert its vasorelaxation effect.
The results showed that the removal of the endothelium markedly attenuated the vasorelaxant effect of sinensetin, which suggested the involvement of endothelium-independent relaxing factors such as the β2-adrenoreceptor. The β2-adrenoreceptor is a Gαs protein-coupled receptor and is present only on the membrane of VSMCs. The activation of this receptor promotes the activity of adenylyl cyclase (AC) to catalyze the breakdown of adenosine triphosphate (ATP) to cyclic 3′,5′-adenosine monophosphate (cAMP), thus inducing vasorelaxation [14]. The results clearly showed that propranolol influenced the vasorelaxant effects of sinensetin. These data suggested that the vasorelaxant effect exhibited by sinensetin might involve the β2-adrenoreceptor pathway.
Other than the endothelium-independent mechanism studies, the effects of sinensetin on potassium and calcium channels were investigated [9, 15]. The calcium ion content in the cytosol was strictly dependent on the membrane potential of VSMCs. There are two processes for the entry of calcium ions, extracellular influx via VOCC and intracellular influx via IP3R and ryanodine receptor. Once potassium efflux has generated the electrochemical gradient in the cytosol to reach hyperpolarization, the action potential will allow the entry of extracellular calcium ions into the cytosol, which depolarizes the membrane potential of VSMCs and subsequently causes vasoconstriction [9, 15]. Based on our results, we believe that sinensetin inhibits Ca2+ influx through VOCC, as well as through inhibiting IP3R, thereby causing a decrease in intracellular Ca2+ levels that leads to vasorelaxation. In addition, the influx of Ca2+ via calcium channels, especially through ROCC and VOCC, causes a calcium spike in the cytosol and results in calcium-induced calcium release via ryanodine receptors [16, 17]. This results in a further increase in intracellular Ca2+, which causes vasoconstriction. The results show that the vasorelaxant effect of sinensetin not only is associated with the inhibition of Ca2+ influx via VOCC and calcium release via IP3R but also inhibits intracellular Ca2+ release from the ryanodine receptor. These findings were confirmed by studying the PE-evoked contraction of endothelium-denuded aortic rings in calcium-free Krebs’ solution. In this study, intracellular calcium ions were removed with EGTA to ensure that the contraction of the aortic ring after precontraction by PE was caused only by calcium released from the sarcoplasmic reticulum. Sinensetin was able to reduce vasoconstriction evoked by PE in a dose-dependent manner, a finding that clearly shows that sinensetin may antagonize the IP3 receptor, which contributes to calcium release from the sarcoplasmic reticulum.
Potassium channels also play a vital role in the regulation of vascular tone [18]. Potassium channels regulate the electrochemical gradient in VSMCs by controlling the action potential. The activation of potassium channels causes membrane hyperpolarization due to the outward flow of potassium ions, thus inducing the closure of calcium channels and preventing Ca2+ influx, which leads to vasorelaxation. The results of the present study show that sinensetin-induced relaxation in endothelium-intact aortic rings was reduced by treatment with K+ channels blockers, namely, TEA, 4-AP, BaCl2, and glibenclamide. These findings suggest that sinensetin could act as a K+ channel opener to induce vasorelaxation in a manner similar to the pathways that are antagonized by TEA, 4-AP, BaCl2, and glibenclamide, which is evoked via KCa, KV, Kir, and KATP channels.
Sinensetin is an important phytochemical found in O. stamineus. In clinical studies, O. stamineus has been tested as an additional regimen for antihypertensive treatment [1]. Our previous results have shown that the active chloroform fraction of O. stamineus possesses excellent vasodilatory effects on an isolated rat aorta in vitro model [2, 3]. The most noteworthy previous publications showed that the vasodilation effect of the chloroform fraction of O. stamineus occurs via multiple pathways, primarily involving the Kir, KCa, Kv and calcium channels, muscarinic receptors and the NO pathway. The vasodilation effect of sinensetin also occurs via multiple pathways but mainly depends on the NO/sGC/cGMP pathway and calcium receptor, which is not similar to the general trend of O. stamineus activity. This alludes to the fact that sinensetin may not be the only vasodilative phytochemical present in O. stamineus. Moreover, the chloroform fraction of O. stamineus at 8.75 µg/mL (containing 0.262 µg/mL of sinensetin) causes 69.19% vasodilation in a PE-induced aortic ring vasocontraction model, which is considerably higher than the vasodilation effect of sinensetin at 0.262 µg/mL. Based on this finding, we strongly believe that there might be other vasodilative phytochemicals present in O. stamineus that might exhibit synergism with sinensetin and potentiate its effect on vasodilation. Therefore, there is a need to isolate other vasodilative phytochemicals from O. stamineus and investigate the relationships among the compounds on vasodilatory activity.
References
Trimarco V, Cimmino CS, Santoro M, Pagnano G, Manzi MV, Piglia A et al. Nutraceuticals for blood pressure control in patients with high-normal or grade 1 hypertension. High Blood Press Cardiovasc Prev. 2012;19:117–22.
Yam MF, Tan CS, Ahmad M, Shibao R. Vasorelaxant action of the chloroform fraction of Orthosiphon stamineus via NO/cGMP pathway, potassium and calcium channels. Am J Chin Med. 2016;44:1413–39.
Yam MF, Tan CS, Ahmad M, Ruan S. Mechanism of vasorelaxation induced by eupatorin in the rats aortic ring. Eur J Pharmacol. 2016;789:27–36.
Xu YC, Leung SW, Yeung DK, Hu LH, Chen GH, Che CM et al. Structure–activity relationships of flavonoids for vascular relaxation in porcine coronary artery. Phytochemistry. 2007;68:1179–88.
Senejoux F, Girard C, Kerram P, Aisa HA, Berthelot A, Bévalot F et al. Mechanisms of vasorelaxation induced by Ziziphora clinopodioides Lam. (Lamiaceae) extract in rat thoracic aorta. J Ethnopharmacol. 2010;132:268–73.
Wang J, Dong M, Liu M, Xu D, Luo Y, Zhang B et al. Tanshinone IIA modulates pulmonary vascular response to agonist and hypoxia primarily via inhibiting Ca2+ influx and release in normal and hypoxic pulmonary hypertension rats. Eur J Pharmacol. 2010;640:129–38.
Senejoux F, Demougeot C, Cuciureanu M, Miron A, Cuciureanu R, Berthelot A et al. Vasorelaxant effects and mechanisms of action of Heracleums phondylium L. (Apiaceae) in rat thoracic aorta. J Ethnopharmacol. 2013;147:536–9.
Jakala P, Pere E, Lehtinen R, Turpeinen A, Korpela R, Vapaatalo H. Cardiovascular activity of milk casein-derived tripeptides and plant sterols in spontaneously hypertensive rats. J Physiol Pharmacol. 2009;60:11–20.
Yildiz O, Gul H, Seyrek M. Pharmacology of arterial grafts for coronary artery bypass surgery. In: Aronow WS. editor. Artery bypass. Croatia: Intech Open Access Publisher; 2013.
Goodman LS, Brunton LL, Chabne B, Knollmann BC. Goodman & Gilman’s pharmacological basis of therapeutics. New York: McGraw-Hill; 2011.
Sobey CG. Potassium channel function in vascular disease. Arterioscler Thromb Vasc Biol. 2001;21:28–38.
Caulfield MP, Birdsall NJ. International Union of Pharmacology, XVII. Classification of muscarinic acetylcholine receptors. Pharmacol Rev. 1998;50:279–90.
Ishii M, Kurachi Y. Muscarinic acetylcholine receptors. Curr Pharm Des. 2006;12:3573–81.
Nichols DE, Nichols CD. Serotonin receptors. Chem Rev. 2008;108:1614–41.
McFadzean I, Gibson A. The developing relationship between receptor-operated and store-operated calcium channels in smooth muscle. Br J Pharmacol. 2002;135:1–13.
Imtiaz MS, Katnik CP, Smith DW, Helden van DF. Role of voltage-dependent modulation of store Ca2+release in synchronization of Ca2+oscillations. Biophys J. 2006;90:1–23.
Thorneloe KS, Nelson MT. Ion channels in smooth muscle: regulators of intracellular calcium and contractility. Can J Physiol Pharmacol. 2005;83:215–42.
Nelson MT, Quayle JM. Physiological roles and properties of potassium channels in arterial smooth muscle. Am J Physiol. 1995;268:799–822.
Acknowledgements
We appreciate the contribution of all those who participated in this study. The main author (M.F. Yam) would like to acknowledge the Provincial Government Scholarship of Fujian, China. This project was supported by the Malaysia Toray Science Foundation (MTSF), the Fundamental Research Grant Scheme (FRGS) (203/PFARMASI/6711306), the Exploratory Research Grant Scheme (ERGS) (203/PFARMASI/6730122), the USM-Bridging Grant (304/PFARMASI/6316009), and Universiti Sains Malaysia-Research University Grants (1001/PFARMASI/812195).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Yam, M.F., Tan, C.S. & Shibao, R. Vasorelaxant effect of sinensetin via the NO/sGC/cGMP pathway and potassium and calcium channels. Hypertens Res 41, 787–797 (2018). https://doi.org/10.1038/s41440-018-0083-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-018-0083-8
This article is cited by
-
Mechanism of vasorelaxation induced by 3′-hydroxy-5,6,7,4′-tetramethoxyflavone in the rats aortic ring assay
Naunyn-Schmiedeberg's Archives of Pharmacology (2018)