Abstract
Papillary neoplasms of the breast are a heterogeneous group of epithelial tumors nearly entirely composed of papillae. Their classification rests on the characteristics of the epithelium and the presence and distribution of the myoepithelial cells along the papillae and around the tumor. Papillary neoplasms of the breast can be diagnostically challenging, especially if only core needle biopsy (CNB) material is available. This review summarizes salient morphological and immunohistochemical features, clinical presentation, and differential diagnoses of papillary neoplasms of the breast. We include a contemporary appraisal of the upgrade rate to carcinoma (invasive carcinoma and ductal carcinoma in situ [DCIS]) and atypical hyperplasias in surgical excision specimens obtained following CNB diagnosis of papilloma without atypia, and a review of the available follow-up data in cases without immediate surgical excision.
Similar content being viewed by others
Introduction
Most papillary neoplasms of the breast occur in women, but men can also be affected [1]. The majority of papillary neoplasms in men and in postmenopausal women are malignant.
A papillary neoplasm consists predominantly of papillae. Each papilla has a fibrovascular core covered by epithelium with or without a myoepithelial cell (MEC) layer, depending on the type of tumor. The characteristics of the epithelium determine whether a papillary neoplasm is benign, atypical, or carcinoma. Assessing the presence and distribution of the MECs in a papillary neoplasm is also important for classification and may require immunohistochemical stains with a panel of MEC markers, including p63, calponin, and/or smooth muscle myosin heavy chain. P63 may stain scattered epithelial cells in some papillary carcinomas [2, 3].
Papillary neoplasms of the breast can be diagnostically challenging. They accounted for 9 and 17% of all expert pathology consultation cases in two series [4, 5], and were the second most frequent type of consultation cases after borderline atypical ductal proliferations at one center [5].
Papillary neoplasms of the breast include: intraductal papilloma (IDP) with or without atypia, papillary ductal carcinoma in situ (papillary DCIS), encapsulated papillary carcinoma (EPC), solid-papillary carcinoma (SPC), and invasive papillary carcinoma (IPC) [6] (Table 1—WHO classification of papillary neoplasms).
Herein we provide a summary outline of the morphology and immunohistochemical profile of papillary neoplasms, with emphasis on novel information. We also include a contemporary assessment of the management of asymptomatic IDP without atypia diagnosed at radiology–pathology concordant core needle biopsy (CNB), with discussion of the upgrade rate to carcinoma and long-term imaging follow-up without excision. Given that at most centers the management of IDP without atypia diagnosed at CNB is trending toward clinical and imaging follow-up without excision, we also discuss the differential diagnosis of IDP and possible pitfalls.
Intraductal papilloma
IDP is the only benign papillary neoplasm of the breast. It consists of fibrovascular cores covered by non-atypical ductal epithelium and myoepithelium (Fig. 1). IDP can be single or multiple, central/subareolar or peripheral. Central single IDPs are more common than multiple peripheral IDPs, probably because they are more frequently symptomatic [7].
A single central IDP typically presents with unilateral clear nipple discharge, rarely as palpable mass, and is most common in pre- and perimenopausal women. Ultrasound examination is the best imaging modality to detect an IDP, which usually appears as a well-defined, smooth-walled cystic lesion with or without a solid component. Rarely, galactography is required to identify a symptomatic IDP that is mammographically and sonographically occult.
Histologically, an IDP is attached to the inner wall of a cystic duct through a stalk that further branches into smaller papillae. Sclerosis of the stalk and fibrovascular cores may distort the papillae and mimic stromal invasion. IDP is the only papillary neoplasm with a continuous layer of MECs along the papillae and around the dilated duct/cyst that contains it. The epithelium is benign without atypia, and often shows UDH and apocrine metaplasia. Molecular studies showed that most IDPs are monoclonal epithelial proliferations with activating point mutations in the PIK3CA/AKT1 pathway [8, 9].
Intraductal papilloma with ADH or DCIS
Foci of ductal epithelial atypia may sometimes be present in an IDP. The same criteria used in the evaluation of intraductal epithelial proliferations are used to assess ductal atypia in an IDP, but a 3 mm size cutoff is used to separate ADH and low-grade DCIS [6]. Immunohistochemical stains for MEC antigens, estrogen receptor (ER), and basal cytokeratins (CK5, CK5/6, CK14, and 34βE12) can be used to assess the presence and extent of ductal epithelial atypia in an IDP [10,11,12] (Fig. 2).
A Core biopsy of a partially fragmented papillary lesion. The epithelium is focally expanded. The fibrovascular cores vary slightly in size, and some are more fibrotic, while others are inconspicuous. B Immunohistochemical staining with ER shows strong and diffuse positivity of the epithelium throughout the papillary lesion and highlights the expanded and focally cribriform areas. C Immunohistochemical staining with CK5/6 shows linear distribution of the myoepithelium along the fibrovascular cores and at the periphery of the papillary lesion, but most of the ER-positive epithelium is CK5/6-negative. These findings support the diagnosis of atypical intraductal papilloma, which warrants surgical excision.
Atypical papilloma (ADH in a papilloma or papilloma with ADH)
If ADH is present in an IDP, it is reported as such. Atypical IDP or IDP with ADH are equivalent and acceptable terms [6] (Table 1).
The term atypical papilloma does not include IDP with ALH [6]. Although the relative risk of subsequent carcinoma associated with ALH is comparable to that of ADH, the surgical management of these two high risk lesions is significantly different. In particular, the diagnosis of IDP with ALH in CNB material with radiology–pathology concordance may not warrant surgical excision.
Lewis et al. compared the long-term follow-up (F/U) of women with IDPs (single or multiple, with or without atypia) in breast excision specimens with the F/U of a control group of women with or without atypia and no IDPs [7]. The risk of carcinoma [expressed as standardized incidence ratio (SIR)] associated with a single IDP without atypia was similar to the risk of proliferative changes (SIR 2.04 vs. 1.90, respectively), but was slightly higher for patients with multiple IDPs without atypia (SIR 3.01). In the same study, IDPs with atypia (including ADH and/or ALH) had slightly increased risk compared to ADH and/or ALH not associated with IDPs (SIR 5.11 vs. 4.17, respectively). Multiple IDPs with atypia were associated with the highest risk of subsequent carcinoma (SIR 7.01). In this study, none of the patients with IDP and only ALH developed breast carcinoma at F/U.
DCIS in intraductal papilloma
An atypical ductal proliferation with high or intermediate nuclear grade in an IDP qualifies as DCIS regardless of size. The diagnosis of low nuclear grade DCIS in an IDP requires a low-grade ductal proliferation spanning at least 3 mm [6]. DCIS may be limited to the IDP or also involve the adjacent breast parenchyma.
DCIS in an IDP should not be confused with papillary DCIS, which is entirely carcinomatous and consists of papillae devoid of MECs, while IDP with DCIS has a continuous layer of MECs along the papillae.
While in most prior studies the diagnosis of IDP with ADH or DCIS also included IDPs without atypia present near foci ADH or DCIS, the terminology endorsed by the WHO 2019 Expert Panelists is intended only for IDP with ADH or DCIS.
Carcinomas associated with intraductal papilloma
Rarely invasive carcinomas may arise in association with an IDP without any epithelial atypia. In particular, fibromatosis-like metaplastic spindle cell carcinoma [13,14,15] and low-grade adenosquamous carcinoma [16] have been described in this setting.
Fibromatosis-like spindle cell carcinoma is composed of spindle cells with low-grade nuclear atypia and inconspicuous cytoplasm, and this morphology accounts for at least 95% of the tumor [6, 15, 17]. “Epithelioid” spindle cells with dense eosinophilic cytoplasm are usually present, and may form linear arrays that mimic capillary vessels. Scattered mitoses are identified. The diagnosis of fibromatosis-like spindle cell carcinoma requires evidence of epithelial origin, such as an associated low-grade invasive carcinoma with frankly epithelial morphology accounting for no more than 5% of the tumor, and/ or low-grade DCIS, and/or expression of epithelial antigens in the neoplastic spindle cells [6].
Low-grade adenosquamous carcinoma consists of infiltrating angular glands composed of epithelium and myoepithelium, squamous cysts and small squamous clusters with low-grade nuclear atypia. Scattered mitoses and apoptotic cells are also present [6, 16]. Immunohistochemical staining for MEC markers yields a pattern of complete, partially complete or absent staining around the neoplastic glands, while the squamous nests are uniformly positive for p63 [6, 18]. The infiltrating glands and squamous nests are usually surrounded by myofibroblasts in a lamellar arrangement parallel to the major axis of the epithelial structures. The combination of glands and squamous nests surrounded by cellular stroma and infiltrating between normal ducts and lobules is helpful to differentiate this tumor from benign mammary sclerosing lesions.
Any type of invasive carcinomas may also arise in the setting of IDP with ADH or DCIS or may develop near an IDP and involve it secondarily.
Management of intraductal papilloma without atypia diagnosed at core needle biopsy
In the past, all papillary lesions diagnosed at CNB underwent F/U surgical excision. Currently, surgical excision is routinely recommended for all papillary lesions with ductal atypia or carcinoma in CNB material, regardless of radiologic–pathologic concordance, and for all papillary lesions with discordant imaging and pathologic findings.
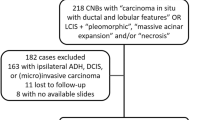
In the last decade, the management of patients with IDP without ductal atypia diagnosed at CNB has been the subject of intense investigation. Many series reporting the upgrade rate to carcinoma (invasive carcinoma or DCIS) at follow-up (F/U) excision have been published, but all studies have been retrospective and have not always included detailed information regarding radiologic–pathologic concordance, introducing possible bias. A recently published multi-institutional prospective study reported a low rate (<2%) of upgrade to carcinoma at excision of asymptomatic and concordant IDP [19].
Surgical excision: upgrade rates to carcinoma and atypical hyperplasias
Based on studies with upgrade rates ranging between 5 and 10%, some investigators have recommended surgical excision for all IDPs diagnosed at CNB, regardless of atypia or radiology–pathology concordance [20,21,22,23,24,25]. However, some of the cases with upgrade in these series were described as radiology–pathology discordant, which by itself would mandate excision. In other studies, the investigators assessed radiologic–pathologic concordance of each case or of all the cases that yielded carcinoma at excision and excluded from the analysis those that were deemed discordant [26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45]. The upgrade rates in these series ranged between 0 and 6.6%, leading the investigators to conclude that surgical excision of concordant IDPs without atypia is not required, and imaging follow-up is a suitable alternative.
Most of the upgrades at excision of IDP without atypia have consisted of DCIS, with only few invasive carcinomas (Table 2). Parameters found to be significantly associated with upgrade included clinical symptoms (nipple discharge and/or a palpable mass), large size of the lesion (>1–1.5 cm), contralateral breast carcinoma, multifocality and peripheral location. Older age was significantly associated with upgrade to carcinoma in some series [26, 32, 37, 39, 40, 46]. Investigators have also compared the upgrade rate following stereotactic CNB versus vacuum-assisted CNB and found that the latter CNB modality to be preferable, as it correlates with low to no upgrade at excision [38, 41, 47].
Based on analysis of these studies, nowadays asymptomatic radiology–pathology concordant IDPs without atypia are not excised at most centers, but they are followed with sonographic imaging. Excision is still recommended for IDPs without atypia with imaging size larger than 1.0 or 1.5 cm. Small (<2 mm) “incidental” IDPs (so called “micropapillomas”) do not require excision, as they are not associated with upgrade to carcinoma [32, 44, 48, 49]. Although these guidelines have been endorsed by the American Society of Breast Surgeons [50], they are not followed uniformly and many IDPs are still excised regardless of radiologic–pathologic concordance. A recent survey of breast radiology practices at academic teaching centers accredited by the Society of Breast Imaging found that surgical excision of IDP without atypia was recommended at 16 (39%) of 41 surveyed institutions, short interval follow-up at 7 (17%), return to screening at 4 (10%), and case-by case management at 14 (34%) [51].
Atypical epithelial proliferations (including ADH, ALH, and classic LCIS) are present in up to 20% of the surgical excision specimens of asymptomatic IDP without atypia diagnosed at CNB (Table 2). Based on these findings, some investigators have suggested that excision of IDP could benefit those women who are found to have atypical lesions on excision, as they can be prescribed tamoxifen or aromatase inhibitors to reduce the risk of breast carcinoma and/or they can undergo more frequent imaging studies, including magnetic resonance imaging evaluation.
IDPs without atypia and imaging follow-up: subsequent ipsilateral carcinomas and atypical hyperplasias
Because in the past most IDPs diagnosed at CNB were excised, very few IDPs without atypia have been followed only with imaging studies. These cases were probably selected as having a low risk of upgrade due to small size of the imaging target or its complete removal by CNB, or because of patient’s preference or comorbidities. The length of available imaging F/U also varies in different studies. Therefore, information regarding ipsilateral carcinomas in patients with IDPs without atypia that did not undergo immediate excision is very limited and intrinsically biased (Table 3).
However, even considering all these limitations, the number of patients who developed ipsilateral carcinomas appears to be low. In one study [52] 114 IDPs diagnosed at ultrasound-guided vacuum-assisted biopsy were followed for a period of 2–81 months. Seventeen lesions were excised, including 14 that showed changes in the sonographic size or shape. Four of the 17 excisions yielded carcinoma, which consisted of two papillary DCIS (both excised at 4 months F/U), one EPC with microinvasion (excised at 4 months F/U), and one papilloma with DCIS (excised at 12 months F/U). The crude rate of carcinoma in this study was 3.5%, comparable to the rate of upgrade to carcinoma for cases with immediate surgical excision. (Note: an additional case of invasive carcinoma with papillary DCIS was also identified, but the authors did not interpret it as a true upgrade because the index core biopsy showed only a micropapilloma. Based on these findings the index core biopsy of this case likely was discordant). Some of the patients with excision during imaging F/U were found to have atypical hyperplasias, but the number of patients found to have atypia is substantially lower compared to patients with atypia in surgical excisions performed soon after the index CNB (Table 3).
It is worth noting that most of the carcinomas diagnosed at immediate surgical excision or during imaging F/U were papillary (Tables 2, 3). It is possible that some individuals may be predisposed to develop multiple and biologically different papillary lesions of the breast. On the other hand, the high frequency of papillary carcinomas in patients with CNB diagnosis of IDP could also be secondary, at least in part, to misclassification of some IDPs without atypia in the CNB material. Notably, in the study by Nakhlis et al. [19], central pathology review did not confirm the original diagnosis of IDP without atypia in 31/116 (27%) of enrolled cases. Given that the management of radiology–pathology concordant IDP without atypia diagnosed at CNB is trending toward imaging F/U without excision, it is even more critical for pathologists to be well acquainted with the diagnosis of IDP without atypia and its implications for patient management.
Differential diagnosis of intraductal papilloma
The differential diagnosis of IDP without atypia includes IDP with ADH or DCIS, papillary DCIS, solid-papillary carcinoma in situ (SPC in situ), and EPC. Because IDP is the only papillary neoplasm with a continuous layer of MECs along the papillae, immunohistochemical stains for MEC markers are particularly useful in supporting the diagnosis of IDP. In addition, immunohistochemical stains for ER and basal-type keratins can be used to assess the presence and extent of epithelial atypia or carcinoma (see also differential diagnosis of papillary DCIS, EPC, and SPC in situ).
The differential diagnosis of IDP (with or without atypia) also includes tumors that are not entirely papillary but often have a papillary component, such as adenomyoepithelioma (AME), tall cell carcinoma with reversed polarity (TCCRP), fibroepithelial tumors with polypoid fronds, radial scar/sclerosing lesions with focal papillary architecture, nipple duct adenoma, hidradenoma papilliferum, and eccrine acrospiroma.
Adenomyoepithelioma (AME) is a biphasic epithelial–myoepithelial neoplasm [53]. AMEs frequently have papillary foci and can closely resemble IDPs histologically. Genetically, most ER-positive AMEs harbor activating point mutations in the PIK3CA/AKT1 pathway akin to IDPs [54], suggesting that the two neoplasms may be closely related. Based on these findings, one could hypothesize that the expression of ER in a biphasic epithelial–myoepithelial papillary neoplasm favors its classification and management as IDP but at present there is no definitive statement to support this conclusion [6]. Most ER-negative AMEs, which can be associated with triple negative carcinomas, harbor HRAS Q61R or Q61K mutations in combination with PI3KCA or PIKR1 mutations [54]. Presently, the differential diagnosis of IDP and AME remains challenging (Fig. 3), particularly if only CNB material is available. The diagnosis of AME mandates surgical excision while only imaging follow-up will be recommended for IDP without atypia.
A Surgical excision of a large papillary lesion within a cystic space. The tumor consists of large sclerotic fibrovascular cores (right) adjacent to a more solid and papillary proliferation (left). B Immunohistochemical staining with CK5/6 shows strong and diffuse positivity both within the cellular component of the tumor (left) and along the sclerotic fibrovascular cores (right). This solid and uniform staining pattern with CK5/6 is incompatible with the diagnosis of intraductal papilloma without atypia and suggests an atypical basaloid epithelial and/or myoepithelial proliferation. C High magnification view of the sclerotic fibrovascular cores shows epithelial and myoepithelial cells. The epithelial cells have enlarged nuclei and prominent nucleoli, an atypical finding in this context (similar findings were also present in the more solid area). D The biphasic composition of the lesion is confirmed with a triple stain. (brown chromogen = p63, CK5, and CK14; red chromogen = CK7 and CK18). The tumor cells showed very minimal to absent expression of the estrogen receptor (not shown). This biphasic tumor was initially classified as intraductal papilloma with usual ductal hyperplasia, but the morphologic and immunohistochemical findings support the diagnosis of atypical adenomyoepithelioma.
Tall cell carcinoma with reversed polarity (TCCRP) consists predominantly of solid nests, but a few papillae may be present. The tumor cells are columnar and have round to oval nuclei with grooves and intranuclear cytoplasmic inclusions. The nuclei are located toward the apical aspect of the cells (reversed cell polarity), a feature most evident in the cells at the periphery of the solid nests or around the fibrovascular cores. Although many papillary carcinomas of the breast may have focal tall cell morphology, or areas suggestive of reversed cell polarity and nuclear stratification [55], these morphologic features are present throughout the tumor and correlate with pathognomonic molecular alterations only in TCCRP. Especially in CNB material, TCCRP may resemble an IDP with UDH histologically and immunohistochemically, because it is positive for CK5/6 and shows nuclear staining for ER in a low percentage (0–10%) of the cells. However, TCCRP is composed of monotonous cells with low-grade nuclear atypia and lacks MECs (Fig. 4). TCCRP is driven by pathogenic mutations of IDH2 (See [53] for detailed information on the molecular alterations immunohistochemical profile of TCCRP).
A Core biopsy of a papillary lesion consisting of an epithelial proliferation with sclerotic and hyalinized fibrovascular cores. (Not shown: the epithelial cells composing the tumor were monotonous, showed reversed polarity, and had nuclear grooves and intranuclear inclusions; see images representative of tall cell carcinoma with reversed polarity in [53]). B Immunohistochemical staining with CK5/6 shows patchy positivity in the epithelium, but there is no staining along the fibrovascular cores, indicative of the absence of myoepithelium. C Immunohistochemical stain with ER highlights rare epithelial cells. D A p63 immunohistochemical stain shows that the tumor is devoid of myoepithelium and highlights only the myoepithelial cells of a small entrapped benign duct. These findings are incompatible with the diagnosis of intraductal papilloma with usual ductal hyperplasia and support a diagnosis of tall cell carcinoma with reversed polarity as long as the tumor cells show the characteristic morphologic features.
Fibroepithelial neoplasms with focal polypoid fronds, such as fibroadenomas or benign phyllodes tumors, may sometimes raise the differential diagnosis of IDP, particularly if only CNB material is available. Usually IDP tends to have papillae with a more complex arborescent pattern and more pronounced UDH, while the pseudopapillary fragments of a fibroadenoma or benign phyllodes tumor tend to be few and are wider in size and not branching.
Radial scar, complex sclerosing lesions, and nipple duct adenoma (florid papillomatosis of the nipple) are benign proliferative and sclerosing lesions that often have papillary areas and may resemble sclerosing IDPs.
Some benign skin adnexal tumors may present as superficial nodules in the breast or axilla and mimic IDP. Hidradenoma papilliferum resembles IDP histologically, as it has papillary architecture and consists of epithelial and MECs. It shares the same genetic alterations as IDP and may be an IDP-related neoplasm [56]. Eccrine acrospiroma (also known as nodular or poroid hidradenoma) may arise in the skin near the nipple or even deep into the breast. Histologically, it is a solid and papillary neoplasm composed of varying proportions of clear and polygonal cells, mucinous cells, and columnar to cuboidal cells forming ductule-like structures. It lacks MECs and usually is negative for ER and PR, and diffusely positive for p63 and CK5/6. Eccrine acrospiroma is a benign neoplasm genetically unrelated to IDP [57]. Examples of eccrine acrospiroma arising in the breast have been misclassified as IDP, atypical IDP, and IPC.
In addition to mammary and skin adnexal neoplasms, the differential diagnosis of IDP also includes benign epithelial proliferations that may be focally papillary, such as usual ductal hyperplasia or apocrine metaplasia as well as papillary-appearing infoldings of the duct wall at a branching point.
All papillary neoplasms, including IDP, are intrinsically fragile and may have areas of hemorrhage, infarction or necrosis, especially following fine needle aspiration or CNB. When dealing with an infarcted/necrotic papillary neoplasm of the breast, sometimes immunohistochemical stains for keratins (i.e., CK7 and AE1:AE3), ER, and MEC antigens may unveil the architecture and cell composition of the tumor, aiding its classification. In this setting, only a positive stain that is consistent with the usual staining pattern of the specific antigen tested may be interpreted with some confidence (Fig. 5). Displacement of malignant or benign epithelial clusters into the stroma is especially common after CNB of papillary neoplasms, including IDP [58], and may mimic stromal invasion.
A Surgical excision of a large infarcted and necrotic papillary tumor within a cystic duct. The outlines of the papillary fronds can still be appreciated despite the extensive infarction and necrosis. B, C Immunohistochemical staining with CK5/6 shows patchy positive staining in the infarcted tumor. The myoepithelium around the cystic duct containing infarcted papillary neoplasm appears as a continuous layer (B). Immunohistochemical staining for CK5/6 highlights the continuous layer of myoepithelium in a non-infarcted area of the papilloma and shows it extending along the infarcted papillae. Taken all together, the immunohistochemical findings in this case support the diagnosis of infarcted intraductal papilloma.
Papillary DCIS
Papillary DCIS is a ductal carcinoma covering fibrovascular cores devoid of myoepithelium, but contained within a duct surrounded by MECs [6]. The nuclear grade of the epithelium composing the papillary DCIS determines the grade of the DCIS. Papillary DCIS may occur in isolation or as one of the various architectural patterns in a case of DCIS.
Information on the frequency and clinical features of papillary DCIS alone is limited, as until 2012, when EPC was formally recognized as a separate neoplasm [59], papillary DCIS and EPC were often reported together as intracystic papillary carcinoma [3, 60, 61]. Papillary DCIS is the most common type of DCIS in males [1].
A dimorphic variant of papillary DCIS was described in 1994 by Leftkowitz et al. [60]. Dimorphic papillary DCIS is composed of cells with conventional ductal morphology and of cells with round to oval shape (“globoid cells”). The nuclei of conventional and globoid carcinoma cells are morphologically similar, and the nuclear grade usually is high or intermediate. The “globoid cells” are located between the conventional-appearing carcinoma cells and the basement membrane, in a position usually occupied by MECs. Leftkowitz et al. [60], however, stated that the “globoid cells” were not MECs because they did not express S100 and SMA. Papillary dimorphic DCIS is very rare, and has not been reevaluated using a contemporary panel of myoepithelial markers.
The differential diagnosis of papillary DCIS and EPC is discussed in the section dedicated to EPC. The management of papillary DCIS is the same as for DCIS with the same nuclear grade and ER status.
Encapsulated papillary carcinoma
EPC tends to occur in postmenopausal women and may occur in men. Clinically, EPC usually presents as a retroareolar palpable mass with or without bloody nipple discharge. It appears sonographically as a round to oval circumscribed mass and may have a cystic component. Histologically EPC is a papillary ductal carcinoma with low to intermediate nuclear grade. It lacks MECs along the papillae and around the tumor, but is often surrounded by a thick fibrous capsule [6].
EPC is a variant of IPC with a blunt front of invasion, but it is classified separately from other IPCs because it has an indolent behavior, more akin to DCIS. The diagnosis of invasive carcinoma associated with EPC requires unequivocal evidence of invasive carcinoma beyond the fibrous capsule of the EPC. Thorough sampling of the interface of the EPC with the adjacent breast tissue is recommended to rule out an associated invasive component, which usually consists of invasive carcinoma of no special type (NST) or may be invasive cribriform carcinoma [62], mucinous carcinoma, or tubular carcinoma. Invasive carcinoma associated with EPC is diffusely ER- and PR-positive and HER2 negative, with no ERBB2 amplification. Staging of invasive carcinoma associated with EPC is based on the invasive component alone, and the size of the EPC should not be included. In the absence of frank invasion beyond the fibrous capsule, EPC is staged as in situ carcinoma (pTis) and managed accordingly.
EPC has genetic alterations similar to those of low-grade, ER-positive invasive carcinoma NST, and a comparable rate of PIK3CA mutations.
The differential diagnosis of EPC includes papillary DCIS, SPC in situ, IPC, as well as papilloma, papilloma with ADH, and papilloma with DCIS. Papillary DCIS and EPC often co-exist and may be difficult to distinguish. Ducts involved by papillary DCIS are surrounded by MECs and tend to be smaller than the nodules of EPC, which are completely devoid of myoepithelium. Solid growth may be present focally in an EPC, raising the differential with SPC in situ, but it never constitutes the main architectural pattern; carcinoma arranged in a cribriform pattern is often present in the spaces between the fibrovascular cores. In addition, EPC does not show neuroendocrine differentiation, which is common in SPC. Some IPC may have a rounded contour and mimic EPC, but they usually lack a fibrous capsule, have higher nuclear grade, high mitotic rate and are triple negative or HER2-positive. Given its circumscription and low nuclear morphology EPC sometimes may also raise the differential diagnosis of IDP with or without ADH or DCIS, especially in CNB material or when the tumor is infarcted (Fig. 6). Immunohistochemical stains for MECs, ER and CK5/6 may be used in these settings to assess the presence of MECs and the extent of ductal atypia.
Two separate cases are shown. A Core biopsy of a fragmented papillary tumor. The epithelium covers some of the fibrovascular cores and is also present as many small detached hyperchromatic clusters. Some of the fibrovascular cores were infarcted. This core biopsy had originally been interpreted as intraductal papilloma with infarction, but the fragmented nature of this sample and the hyperchromasia and fragmentation of the epithelial clusters are suspicious for a papillary carcinoma, which is how this case was reported later. Surgical excision yielded an encapsulated papillary carcinoma (not shown). B–E are images of metachronous tumors from the same patient. B Surgical excision of an infarcted papillary neoplasm. The necrotic tumor has a papillary architecture and is surrounded by a thick fibrous capsule. C A magnified view of the tumor in (B) shows focal viable atypical epithelium closely juxtaposed to the fibrous capsule and focally extending into it. The tumor in (B, C) was originally diagnosed as an infarcted papilloma, but the nuclear atypia and the arrangement of the epithelium are most consistent with an infarcted encapsulated papillary carcinoma. D, E Two years later, the patient developed a breast mass at the same site. The recurrent neoplasm resembles the prior tumor and has a thick fibrous capsule (D). The epithelial proliferation has low to intermediate grade nuclear atypia (E). These findings support the diagnosis of recurrent encapsulated papillary carcinoma. Focal invasive carcinoma was also present (not shown). Six years later the patient developed bone metastases.
Solid-papillary carcinoma
Similar to EPC, SPC tends to occur in postmenopausal women and may occur in men [1, 63]. Clinically it presents as a palpable breast mass, a mammographic mass/abnormality, and/or with bloody nipple discharge. Imaging studies of SPC in situ show a round and circumscribed mammographic opacity and a solid, well-defined, hypoechoic or sonographically heterogeneous mass. SPC with invasion may appear as a mass with irregular borders or architectural distortion.
SPC encompasses in situ and invasive carcinomas with a solid growth pattern arranged around inconspicuous fibrovascular cores. SPC often expresses neuroendocrine antigens (such as chromogranin and synaptophysin), but neuroendocrine differentiation is not required for the diagnosis.
In the past, invasive SPC and SPC in situ were often diagnosed together as “SPC invasive and in situ”, without specifying the extent of the invasive component. Diagnostic criteria to separate SPC in situ and SPC with invasion have been outlined in the 2019 WHO Classification of Tumors of the Breast [64].
SPC in situ consists of expansive, round to oval, solid and papillary nodules of carcinoma. The cells may have columnar, round to oval, or spindle cell morphology and usually show mild to moderate nuclear atypia. The nuclear chromatin is fine and granular, and nucleoli are inconspicuous. The tumor cells often are distributed in a palisading arrangement along the fibrovascular cores [65,66,67,68,69]. No MECs are present along the papillae of SPC in situ, but MECs usually surround the ducts that contain it. In accordance to the diagnostic criteria agreed upon by the WHO experts [6], SPC consisting of nests and nodules with smooth and regular outline and a distribution pattern consistent with an in situ process, is also classified as SPC in situ, regardless of the presence of MECs [6].
In addition to SPC with invasion, the differential diagnosis of SPC in situ usually includes IDP with UDH and EPC. The nuclei of SPC are atypical, have no grooves and intranuclear cytoplasmic inclusions, which are commonly seen in UDH. In addition, the nests of SPC with spindle cell morphology are composed of uniformly atypical cells. SPC is diffusely and strongly positive for ER, and does not express basal cytokeratins such as CK5/6, while UDH in an IDP has only sparse ER-positive cells and scattered positivity for CK5/6 with a characteristic “checkerboard” pattern [70]. Rarely, especially in CNB material, classic or florid LCIS involving an IDP may also mimic SPC in situ, as both carcinomas may be composed of plasmacytoid cells and have intracytoplasmic mucin. Extracellular mucin is often associated with SPC, but it is infrequent near LCIS. The cells of florid LCIS do not express E-cadherin and beta-catenin and show diffuse cytoplasmic staining for p120. In addition, an IDP involved by LCIS has a continuous layer of MECs along the papillae, while SPC in situ (or invasive) does not.
SPC with invasion is composed of strands or large clusters of tumor cells infiltrating into the stroma. The invasive carcinoma may have neuroendocrine morphology and/or differentiation or consists of hypercellular mucinous carcinoma (mucinous carcinoma type B) [71]. As a reminder, extracellular stromal mucin is not diagnostic of mucinous carcinoma unless it contains single cells or clusters of carcinoma. The invasive component of SPC may also have solid-papillary architecture, and consist of clusters and nests of different size and shape, with irregular or scalloped edges, directly abutting the adipocytes or distributed in an haphazard pattern that cannot be accounted for by SPC in situ involving pre-existing normal ducts and lobules. Rarely, invasive SPC is associated with invasive carcinoma of NST, lobular, cribriform, or tubular carcinoma patterns [69]. Usually, SPC with invasion is ER and PR-positive, HER2 negative/ERBB2 not amplified.
Molecular alterations in SPC include copy-number aberrations (16q losses, 16p and 1q gains), PIK3CA mutations (in ~40% of cases), and expression of genes related to neuroendocrine differentiation (RET, ASCL1, and DOK7) [72, 73].
Only SPC with invasion is used to determine the tumor stage, Nottingham grade, and ER, PR, and HER2 status. Overall, SPC appears to have an excellent prognosis [74].
Invasive papillary carcinoma
IPC of the breast is rare. It consists entirely of fibrovascular cores covered by neoplastic epithelium with a frankly invasive growth pattern [75] MECs are absent along the papillary stalks and at the periphery of the tumor. Usually no fibrous capsule surrounds the tumor. IPC usually has moderate to high nuclear grade and is graded according to the Nottingham grading system. Most IPCs are ER, PR, and HER2 negative [76]. There is limited to no follow-up information on IPC but given its high grade morphologic features, it is regarded as having poor prognosis [76]. Accordingly, any papillary carcinoma with high nuclear grade that is HER2-positive or triple negative is classified as IPC, even if it has a round and apparently circumscribed outline that could be suggestive of EPC, as the latter has a favorable prognosis [75]. Rarely, focal DCIS is present near IPC. In the absence of DCIS, the differential diagnosis of an IPC in the breast should include metastasis from a non-mammary carcinoma, such as metastases of ovarian serous carcinoma, which is usually positive for PAX-8 and ER, and negative for GATA3 and/or SOX10, while a mammary IPC is usually negative for PAX-8, and positive for GATA3 or SOX10.
Conclusions
The diagnosis of papillary neoplasms of the breast can be challenging, and knowledge of their morphologic features and possible differential diagnoses is necessary to ensure accurate patient management.
The prognosis of most papillary carcinomas of the breast varies, but tends to be good overall, except for IPCs.
In general, all papillary lesions diagnosed at CNB require surgical excision, except IDP without atypia. As the management of asymptomatic IDP without atypia diagnosed at radiology–pathology concordant core biopsy is shifting towards imaging follow-up without immediate surgical excision, pathologists need to be familiar with the diagnosis of IDP without atypia and its differential diagnoses and also be cognizant of the need to assess ductal epithelial atypia in a papilloma with the aid of immunohistochemical markers in challenging cases.
References
Zhong E, Cheng E, Goldfischer M, Hoda SA. Papillary lesions of the male breast: a study of 117 cases and brief review of the literature demonstrate a broad clinicopathologic spectrum. Am J Surg Pathol. 2020;44:68–76.
Stefanou D, Batistatou A, Nonni A, Arkoumani E, Agnantis NJ. p63 expression in benign and malignant breast lesions. Histol Histopathol. 2004;19:465–71.
Collins LC, Carlo VP, Hwang H, Barry TS, Gown AM, Schnitt SJ. Intracystic papillary carcinomas of the breast: a reevaluation using a panel of myoepithelial cell markers. Am J Surg Pathol. 2006;30:1002–7.
Putti TC, Pinder SE, Elston CW, Lee AH, Ellis IO. Breast pathology practice: most common problems in a consultation service. Histopathology. 2005;47:445–57.
East EG, Zhao L, Pang JC, Jorns JM. Characteristics of a breast pathology consultation practice. Arch Pathol Lab Med. 2017;141:578–84.
WHO Classification of Tumours Editorial Board. Breast tumours. Vol 2. 5th ed. Lyon, France: IARC; 2019.
Lewis JT, Hartmann LC, Vierkant RA, Maloney SD, Shane Pankratz V, Allers TM, et al. An analysis of breast cancer risk in women with single, multiple, and atypical papilloma. Am J Surg Pathol. 2006;30:665–72.
Troxell ML, Levine J, Beadling C, Warrick A, Dunlap J, Presnell A, et al. High prevalence of PIK3CA/AKT pathway mutations in papillary neoplasms of the breast. Mod Pathol. 2010;23:27–37.
Jahn SW, Kashofer K, Thuringer A, Abete L, Winter E, Eidenhammer S, et al. Mutation profiling of usual ductal hyperplasia of the breast reveals activating mutations predominantly at different levels of the PI3K/AKT/mTOR pathway. Am J Pathol. 2016;186:15–23.
Grin A, O’Malley FP, Mulligan AM. Cytokeratin 5 and estrogen receptor immunohistochemistry as a useful adjunct in identifying atypical papillary lesions on breast needle core biopsy. Am J Surg Pathol. 2009;33:1615–23.
Tse GM, Ni YB, Tsang JY, Shao MM, Huang YH, Luo MH, et al. Immunohistochemistry in the diagnosis of papillary lesions of the breast. Histopathology. 2014;65:839–53.
Tse GM, Tan PH, Moriya T. The role of immunohistochemistry in the differential diagnosis of papillary lesions of the breast. J Clin Pathol. 2009;62:407–13.
Gobbi H, Simpson JF, Jensen RA, Olson SJ, Page DL. Metaplastic spindle cell breast tumors arising within papillomas, complex sclerosing lesions, and nipple adenomas. Mod Pathol. 2003;16:893–901.
Lee AH. Recent developments in the histological diagnosis of spindle cell carcinoma, fibromatosis and phyllodes tumour of the breast. Histopathology. 2008;52:45–57.
Sneige N, Yaziji H, Mandavilli SR, Perez ER, Ordonez NG, Gown AM, et al. Low-grade (fibromatosis-like) spindle cell carcinoma of the breast. Am J Surg Pathol. 2001;25:1009–16.
Van Hoeven KH, Drudis T, Cranor ML, Erlandson RA, Rosen PP. Low-grade adenosquamous carcinoma of the breast. A clinocopathologic study of 32 cases with ultrastructural analysis. Am J Surg Pathol. 1993;17:248–58.
Gobbi H, Simpson JF, Borowsky A, Jensen RA, Page DL. Metaplastic breast tumors with a dominant fibromatosis-like phenotype have a high risk of local recurrence. Cancer. 1999;85:2170–82.
Kawaguchi K, Shin SJ. Immunohistochemical staining characteristics of low-grade adenosquamous carcinoma of the breast. Am J Surg Pathol. 2012;36:1009–20.
Nakhlis F, Baker GM, Pilewskie M, Gelman R, Calvillo KZ, Ludwig K, et al. The Incidence of Adjacent Synchronous Invasive Carcinoma and/or Ductal Carcinoma In Situ in Patients with Intraductal Papilloma without Atypia on Core Biopsy: Results from a Prospective Multi-Institutional Registry (TBCRC 034). Ann Surg Oncol. 2020. https://doi.org/10.1245/s10434-020-09215-w [Epub ahead of print].
Fu CY, Chen TW, Hong ZJ, Chan DC, Young CY, Chen CJ, et al. Papillary breast lesions diagnosed by core biopsy require complete excision. Eur J Surg Oncol. 2012;38:1029–35.
Rizzo M, Linebarger J, Lowe MC, Pan L, Gabram SG, Vasquez L, et al. Management of papillary breast lesions diagnosed on core-needle biopsy: clinical pathologic and radiologic analysis of 276 cases with surgical follow-up. J Am Coll Surg. 2012;214:280–7.
Foley NM, Racz JM, Al-Hilli Z, Livingstone V, Cil T, Holloway CM, et al. An international multicenter review of the malignancy rate of excised papillomatous breast lesions. Ann Surg Oncol. 2015;22 Suppl 3:S385–90.
Glenn ME, Throckmorton AD, Thomison JB III, Bienkowski RS. Papillomas of the breast 15 mm or smaller: 4-year experience in a community-based dedicated breast imaging clinic. Ann Surg Oncol. 2015;22:1133–9.
Cyr AE, Novack D, Trinkaus K, Margenthaler JA, Gillanders WE, Eberlein TJ, et al. Are we overtreating papillomas diagnosed on core needle biopsy? Ann Surg Oncol. 2011;18:946–51.
Chen YA, Mack JA, Karamchandani DM, Zaleski MP, Xu L, Dodge DG, et al. Excision recommended in high-risk patients: revisiting the diagnosis of papilloma on core biopsy in the context of patient risk. Breast J. 2019;25:232–6.
Chang JM, Han W, Moon WK, Cho N, Noh DY, Park IA, et al. Papillary lesions initially diagnosed at ultrasound-guided vacuum-assisted breast biopsy: rate of malignancy based on subsequent surgical excision. Ann Surg Oncol. 2011;18:2506–14.
Chang JM, Moon WK, Cho N, Han W, Noh DY, Park IA, et al. Risk of carcinoma after subsequent excision of benign papilloma initially diagnosed with an ultrasound (US)-guided 14-gauge core needle biopsy: a prospective observational study. Eur Radiol. 2010;20:1093–100.
Li X, Weaver O, Desouki MM, Dabbs D, Shyum S, Carter G, et al. Microcalcification is an important factor in the management of breast intraductal papillomas diagnosed on core biopsy. Am J Clin Pathol. 2012;138:789–95.
Swapp RE, Glazebrook KN, Jones KN, Brandts HM, Reynolds C, Visscher DW, et al. Management of benign intraductal solitary papilloma diagnosed on core needle biopsy. Ann Surg Oncol. 2013;20:1900–5.
Nakhlis F, Ahmadiyeh N, Lester S, Raza S, Lotfi P, Golshan M. Papilloma on core biopsy: excision vs. observation. Ann Surg Oncol. 2015;22:1479–82.
Pareja F, Corben AD, Brennan SB, Murray MP, Bowser ZL, Jakate K, et al. Breast intraductal papillomas without atypia in radiologic-pathologic concordant core-needle biopsies: rate of upgrade to carcinoma at excision. Cancer. 2016;122:2819–27.
Hong YR, Song BJ, Jung SS, Kang BJ, Kim SH, Chae BJ. Predictive factors for upgrading patients with benign breast papillary lesions using a core needle biopsy. J Breast Cancer. 2016;19:410–6.
Kim SY, Kim EK, Lee HS, Kim MJ, Yoon JH, Koo JS, et al. Asymptomatic benign papilloma without atypia diagnosed at ultrasonography-guided 14-gauge core needle biopsy: which subgroup can be managed by observation? Ann Surg Oncol. 2016;23:1860–6.
Han SH, Kim M, Chung YR, Yun B, Jang M, Kim SM, et al. Benign intraductal papilloma without atypia on core needle biopsy has a low rate of upgrading to malignancy after excision. J Breast Cancer. 2018;21:80–6.
Ahn SK, Han W, Moon HG, Kim MK, Noh DY, Jung BW, et al. Management of benign papilloma without atypia diagnosed at ultrasound-guided core needle biopsy: scoring system for predicting malignancy. Eur J Surg Oncol. 2018;44:53–8.
Kuehner G, Darbinian J, Habel L, Axelsson K, Butler S, Chang S, et al. Benign papillary breast mass lesions: favorable outcomes with surgical excision or imaging surveillance. Ann Surg Oncol. 2019;26:1695–703.
MacColl C, Salehi A, Parpia S, Hodgson N, Ramonas M, Williams P. Benign breast papillary lesions diagnosed on core biopsy: upgrade rate and risk factors associated with malignancy on surgical excision. Virchows Arch. 2019;475:701–7.
Choi HY, Kim SM, Jang M, Yun B, Kang E, Kim EK, et al. Benign breast papilloma without atypia: outcomes of surgical excision versus US-guided directional vacuum-assisted removal or US follow-up. Radiology. 2019;293:72–80.
Chen P, Zhou D, Wang C, Ye G, Pan R, Zhu L. Treatment and outcome of 341 papillary breast lesions. World J Surg. 2019;43:2477–82.
Yu Y, Salisbury E, Gordon-Thomson D, Yang JL, Crowe PJ. Management of papillary lesions without atypia of the breast diagnosed on needle biopsy. ANZ J Surg. 2019;89:524–8.
Raj SD, Phillips J, Mehta TS, Quintana LM, Fishman MD, Dialani V, et al. Management of BIRADS 3, 4A, and 4B lesions diagnosed as pure papilloma by ultrasound-guided core needle biopsy: is surgical excision necessary? Acad Radiol. 2019;26:909–14.
Grimm LJ, Bookhout CE, Bentley RC, Jordan SG, Lawton TJ. Concordant, non-atypical breast papillomas do not require surgical excision: A 10-year multi-institution study and review of the literature. Clin Imaging. 2018;51:180–5.
Moynihan A, Quinn EM, Smith CS, Stokes M, Kell M, Barry JM, et al. Benign breast papilloma: Is surgical excision necessary? Breast J. 2020;26:705–10.
Genco IS, Tugertimur B, Manolas PA, Hasanovic A, Hajiyeva S. Upgrade rate of intraductal papilloma without atypia on breast core needle biopsy: a clinical, radiological and pathological correlation study. Am J Surg. 2020;220:677–81.
Bennett LE, Ghate SV, Bentley R, Baker JA. Is surgical excision of core biopsy proven benign papillomas of the breast necessary? Acad Radiol. 2010;17:553–7.
Li X, Aho M, Newell MS, Clifford K, Patel JG, Jou S, et al. Papilloma diagnosed on core biopsies has a low upgrade rate. Clin Imaging. 2020;60:67–74.
Kim MJ, Kim SI, Youk JH, Moon HJ, Kwak JY, Park BW, et al. The diagnosis of non-malignant papillary lesions of the breast: comparison of ultrasound-guided automated gun biopsy and vacuum-assisted removal. Clin Radiol. 2011;66:530–5.
Jaffer S, Bleiweiss IJ, Nagi C. Incidental intraductal papillomas (<2 mm) of the breast diagnosed on needle core biopsy do not need to be excised. Breast J. 2013;19:130–3.
Weisman PS, Sutton BJ, Siziopikou KP, Hansen N, Khan SA, Neuschler EI, et al. Non-mass-associated intraductal papillomas: is excision necessary? Hum Pathol. 2014;45:583–8.
American Society of Breast Surgeons. Consensus guideline on concordance assessment of image-guided breast biopsies and management of borderline or high-risk lesions. 2016. https://www.breastsurgeons.org/docs/statements/Consensus-Guideline-on-Concordance-Assessment-of-Image-Guided-Breast-Biopsies.pdf.
Falomo E, Adejumo C, Carson KA, Harvey S, Mullen L, Myers K. Variability in the management recommendations given for high-risk breast lesions detected on image-guided core needle biopsy at U.S. academic institutions. Curr Probl Diagn Radiol. 2019;48:462–6.
Yamaguchi R, Tanaka M, Tse GM, Yamaguchi M, Terasaki H, Hirai Y, et al. Management of breast papillary lesions diagnosed in ultrasound-guided vacuum-assisted and core needle biopsies. Histopathology. 2015;66:565–76.
Pareja F, Weigelt B, Reis-Filho JS. Problematic breast tumors reassessed in light of novel molecular data. Mod Pathol. 2020. https://doi.org/10.1038/s41379-020-00693-7 [Epub ahead of print].
Geyer FC, Li A, Papanastasiou AD, Smith A, Selenica P, Burke KA, et al. Recurrent hotspot mutations in HRAS Q61 and PI3K-AKT pathway genes as drivers of breast adenomyoepitheliomas. Nat Commun. 2018;9:1816.
Toss MS, Billingham K, Egbuniwe IU, Moreno F, Abass A, Rakha EA. Breast tumours resembling the tall cell variant of thyroid papillary carcinoma: are they part of the papillary carcinoma spectrum or a distinct entity? Pathobiology. 2019;86:83–91.
Liau JY, Lan J, Hong JB, Tsai JH, Kuo KT, Chu CY, et al. Frequent PIK3CA-activating mutations in hidradenoma papilliferums. Hum Pathol. 2016;55:57–62.
Hsieh MS, Lien HC, Hua SF, Kuo WH, Lee YH. Clear cell hidradenoma of the breast with MAML2 gene rearrangement. Pathology. 2017;49:84–7.
Nagi C, Bleiweiss I, Jaffer S. Epithelial displacement in breast lesions: a papillary phenomenon. Arch Pathol Lab Med. 2005;129:1465–9.
Lakhani SR, Ellis I, Schnitt SJ, Tan PH, Van de Vijver MJ, editors. WHO Classification of Tumours of the Breast. 4th edition. Geneva, Switzerland: WHO Press; 2012.
Lefkowitz M, Lefkowitz W, Wargotz ES. Intraductal (intracystic) papillary carcinoma of the breast and its variants: a clinicopathological study of 77 cases. Hum Pathol. 1994;25:802–9.
Carter D, Orr SL, Merino MJ. Intracystic papillary carcinoma of the breast. After mastectomy, radiotherapy or excisional biopsy alone. Cancer. 1983;52:14–9.
Wynveen CA, Nehhozina T, Akram M, Hassan M, Norton L, Van Zee KJ, et al. Intracystic papillary carcinoma of the breast: an in situ or invasive tumor? Results of immunohistochemical analysis and clinical follow-up. Am J Surg Pathol. 2011;35:1–14.
Burga AM, Fadare O, Lininger RA, Tavassoli FA. Invasive carcinomas of the male breast: a morphologic study of the distribution of histologic subtypes and metastatic patterns in 778 cases. Virchows Arch. 2006;449:507–12.
Mac Grogan G, Collins LC, Lerwill M, Rakha EA, Tan BY. Solid papillary carcinoma (in situ and invasive). In: Board WCoTE, editor. WHO classification of breast tumours. 5th ed. Vol. 2. Lyon, France: IARC; 2019. p. 63–5.
Maluf HM, Koerner FC. Solid papillary carcinoma of the breast. A form of intraductal carcinoma with endocrine differentiation frequently associated with mucinous carcinoma. Am J Surg Pathol. 1995;19:1237–44.
Tsang WY, Chan JK. Endocrine ductal carcinoma in situ (E-DCIS) of the breast: a form of low-grade DCIS with distinctive clinicopathologic and biologic characteristics. Am J Surg Pathol. 1996;20:921–43.
Nicolas MM, Wu Y, Middleton LP, Gilcrease MZ. Loss of myoepithelium is variable in solid papillary carcinoma of the breast. Histopathology. 2007;51:657–65.
Otsuki Y, Yamada M, Shimizu S, Suwa K, Yoshida M, Tanioka F, et al. Solid-papillary carcinoma of the breast: clinicopathological study of 20 cases. Pathol Int. 2007;57:421–9.
Nassar H, Qureshi H, Adsay NV, Visscher D. Clinicopathologic analysis of solid papillary carcinoma of the breast and associated invasive carcinomas. Am J Surg Pathol. 2006;30:501–7.
Rabban JT, Koerner FC, Lerwill MF. Solid papillary ductal carcinoma in situ versus usual ductal hyperplasia in the breast: a potentially difficult distinction resolved by cytokeratin 5/6. Hum Pathol. 2006;37:787–93.
Capella C, Eusebi V, Mann B, Azzopardi JG. Endocrine differentiation in mucoid carcinoma of the breast. Histopathology. 1980;4:613–30.
Duprez R, Wilkerson PM, Lacroix-Triki M, Lambros MB, MacKay A, A’Hern R, et al. Immunophenotypic and genomic characterization of papillary carcinomas of the breast. J Pathol. 2012;226:427–41.
Piscuoglio S, Ng CK, Martelotto LG, Eberle CA, Cowell CF, Natrajan R, et al. Integrative genomic and transcriptomic characterization of papillary carcinomas of the breast. Mol Oncol. 2014;8:1588–602.
Guo S, Wang Y, Rohr J, Fan C, Li Q, Li X, et al. Solid papillary carcinoma of the breast: a special entity needs to be distinguished from conventional invasive carcinoma avoiding over-treatment. Breast. 2016;26:67–72.
Mac Grogan G, Collins LC, Lerwill M, Rakha EA, Tan BY. Invasive papillary carcinoma. In: Board WCoTE, editor. WHO classification of breast tumours. 5th ed. Vol. 2. Lyon, France: IARC; 2019. p. 66–7.
Rakha EA, Varga Z, Elsheik S, Ellis IO. High-grade encapsulated papillary carcinoma of the breast: an under-recognized entity. Histopathology. 2015;66:740–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brogi, E., Krystel-Whittemore, M. Papillary neoplasms of the breast including upgrade rates and management of intraductal papilloma without atypia diagnosed at core needle biopsy. Mod Pathol 34 (Suppl 1), 78–93 (2021). https://doi.org/10.1038/s41379-020-00706-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-020-00706-5
This article is cited by
-
Upgrade Rısk on Core Needle Bıopsy, Should we Contınue Excısıon of the Papıllomas of the Breast?
Indian Journal of Surgery (2023)
-
Papillary lesions of the breast
Virchows Archiv (2022)