Abstract
Cancer stem cells (CSCs) are involved in the resistance of estrogen (ER)-positive breast tumors against endocrine therapy. On the other hand, nitric oxide (NO) plays a relevant role in CSC biology, although there are no studies addressing how this important signaling molecule may contribute to resistance to antihormonal therapy in ER+ breast cancer. Therefore, we explored whether targeting NO in ER+ breast cancer cells impacts CSC subpopulation and sensitivity to hormonal therapy with tamoxifen. NO was targeted in ER+ breast cancer cells by specific NO depletion and NOS2 silencing and mammosphere formation capacity, stem cell markers and tamoxifen sensitivity were analyzed. An orthotopic breast tumor model in mice was also performed to analyze the efficacy of NO-targeted therapy plus tamoxifen. Kaplan–Meier curves were made to analyze the association of NOS2 gene expression with survival of ER+ breast cancer patients treated with tamoxifen. Our results show that targeting NO inhibited mamosphere formation, CSC markers expression and increased the antitumoral efficacy of tamoxifen in ER+ breast cancer cells, whereas tamoxifen-resistant cells displayed higher expression levels of NOS2 and Notch-1 compared with parental cells. Notably, NO-targeted therapy plus tamoxifen was more effective than either treatment alone in an orthotopic breast tumor model in immunodeficient mice. Furthermore, low NOS2 expression was significantly associated with a higher metastasis-free survival in ER+ breast cancer patients treated with tamoxifen. In conclusion, our data support that NO-targeted therapy in ER+ breast cancer may contribute to increase the efficacy of antihormonal therapy avoiding the development of resistance to these treatments.
Similar content being viewed by others
Introduction
Breast cancer is the most frequent malignant tumor diagnosed in women worldwide, representing a quarter of all tumors diagnosed in the female population [1]. Approximately 75% of breast cancers are estrogen receptor-positive (ER+) and progesterone receptor-positive (PR+), and estrogens contribute primarily to the development and growth of these tumors [2, 3]. The effects of estrogens, such as 17β-estradiol (E2), are mediated by their binding to ER which activates a cellular signaling pathway that leads to cell proliferation. Therefore, the deprivation of this estrogenic signaling has been the basis of hormonal therapy in those patients with ER+/PR+ tumors. Tamoxifen is the most commonly used selective ER Modulator (SERM) in the treatment of both early and advanced breast cancer patients with ER+ tumors [4, 5]. However, almost 50% of ER+ breast cancer patients acquire resistance to hormonal therapy with tamoxifen and do not respond to treatment [6].
There is a growing evidence supporting that cancer stem cells (CSCs) drive cancer evolution and resistance to therapies used in clinic [7], including resistance to hormonal therapy in ER+ breast cancer [7]. A large body of knowledge has been generated on the signaling pathways and proteins involved in generating and maintaining CSCs in breast cancer. In this regard, the Notch signaling pathway, which has been identified as a key driver in breast cancer progression and CSC activity [8] also has been reported to play a key role in the resistance of ER-positive breast cancer against endocrine therapy [9].
Nitric oxide (NO) plays an important role in tumor biology, participating in processes such as cell death, angiogenesis, metastatic dissemination and antitumoral immune response [10,11,12,13]. Elevated tumor inducible NO synthase (NOS2) expression has been shown to predict poor outcome in ER− breast cancer patients and high NOS2 tumors also exhibited elevated expression of basal-like and stem cell markers [14]. Remarkably, NOS2 expression has been associated with a worse prognosis in basal breast cancer, a more aggressive type of tumor with molecular characteristics similar to CSCs [15]. However, there is a limited number of studies on the role of NO in CSC biology. In this regard, we and others have described an important role of NO in CSCs, and that the impairment of NO production through NOS2 silencing in glioblastoma [16, 17] or NO depletion in colorectal cancer [18] target CSC subpopulation. Also, NO released from the tumor endothelium has been reported to activate Notch signaling and promote stem-like characteristics in glioblastoma [19]. Besides, we have previously shown that nitrosative stress in hormone-sensitive MCF7 cells, not only induced a ER-dependent cell growth response but also expanded the CD44+/CD24−/low CSC subpopulation and enhanced the mammosphere formation efficiency [20].
It is therefore conceivable that NO-targeted therapy may not only impact on the capacity of generation and maintenance of breast CSCs but also counteracts the development of resistance against endocrine therapy. Thus, in this study we aimed to explore whether the inhibition of NO production in ER+ breast cancer cells impacts on the CSC subpopulation and enhances the efficacy of hormonal therapy with tamoxifen.
Materials and methods
Chemicals
Carboxy-PTIO (c-PTIO), 4-Hydroxytamoxifen (4HT) and Tamoxifen (Tam) were from Sigma-Aldrich (St Louis, MO, USA). DETANONOate was obtained through Cayman Chemical (Ann Arbor, MI, USA) and IL-1β, IFN-γ, and TNF-α were from R&D Systems (Minneapolis, M, USA).
Cell culture
All media and supplements were from Biowest (Nuaillé, France) unless otherwise stated. MCF-7 (ATCC HTB-22TM, Sigma-Aldrich), BT-474 (DSMZ, Braunschweig, Germany), SKBR-3 (ATCC Cell Lines Services, CLS GmbH, Eppelheim, Germany) and MDA-MB-361 cells (ECACC, Salisbury, UK) were cultured as previously described [18, 20].
Cellular proliferation assay
Real-time cell confluence data were obtained for cell proliferation assay using an IncuCyte® ZOOM live-cell imaging and analysis platform (Essen BiosScience, Ann Arbor, Michigan). Cells were plated (3000 cells per well, 96-well plates) and, after culture for 24 h for cell attachment, they were treated with c-PTIO (60 μM in MCF-7 and 40 μM in MDA-MB-361 and BT-474), 4HT (0.05 μM in MCF-7 and 0.1 μM in MDA-MB-361 and BT-474) or vehicle. Cell confluence increases after each treatment were used to calculate cell proliferation as percentage of corresponding control.
Mammosphere and organoid formation assays
Cells were treated as described above while growing in adherence, and then were seeded in ultra-low attachment plates or embedded in Matrigel for mammospheres or organoid culture, respectively, as previously described [18, 20]. Two weeks after seeding mammospheres were counted and organoids were harvested for total protein extraction and western blot analyses.
Western blot analysis
Cells were lysed as described previously [20], and then total cell lysate was obtained by centrifugation (10,000 × g, 15 min at 4 °C). To extract protein from cytosolic and nuclear fractions, cells were lysed in 10 mM Hepes (pH 7.9), 10 mM KCl, 0.1 mM EGTA, 0.1 mM EDTA, 0.1 M DTT, 0.1 M PMSF, 10% IGEPAL and 1% v/v protease inhibitor cocktail, at 4 °C for 15 min. Cell suspension was then centrifuged (15,000 × g, 4 °C for 5 min) and supernatant was collected (cytosolic protein fraction). The remaining pellet was incubated on ice for 15 min in lysis buffer composed by 10 mM Hepes (pH 7.9), 0.4 M NaCl, 1 mM EGTA, 1 mM EDTA, 0.1 M DTT, 0.1 M PMSF, 10% IGEPAL and 1% v/v protease inhibitor cocktail, centrifuged at 15,000 × g for 5 min at 4 °C and the supernatant (nuclear protein fraction) was collected. Protein was quantified by Bradford assay, separated in MiniProtean TGX Stain-free or Criterion TGX Stain-free gels (BioRad) and transferred to PVDF membranes. Membranes were immunodetected by chemiluminiscence (Clarity Western ECL Substrate, BioRad) after incubation with the specific primary antibodies and with secondary horseradish peroxidase conjugated secondary antibodies. Imaging and densitometric analyses were performed using a ChemiDoc XRS Imaging System with Image Lab software (BioRad). Stain-free technology (BioRad) was used for total protein normalization. Antibodies used were as follows: Notch1 (Abcam, Cambridge, UK, 1:2000), NOS pan (Cell Signaling Technologies, 1:2000) and Sox-2 (R&D Systems, MN, USA, 1:1000).
Flow cytometry
Aldehyde dehydrogenase (ALDH) activity analysis, was performed with the Aldefluor assay (Stemcell Technologies, NC, USA) following the manufacturer’s instructions. To evaluate the expression of CD44 and CD24 surface markers, cells were incubated with different antibodies conjugated with fluorochromes: anti-CD44-PerCP-Cy5.5, anti-CD24-PE and the corresponding IgG isotypes as controls (eBioscience). Flow cytometry was performed on a FACScanto II flow cytometer using FACSDiva software (BD Biosciences).
Stem cell protein array
Proteome Profiler Human Pluripotent Stem Cell Array Kit (R&D Systems, UK) was used according to the manufacturer’s instructions for assessing the expression of specific stem cell markers. Identical amounts of protein lysates (200 μg) were loaded on each membrane. Densitometric analyses were performed using ChemiDoc XRS Imaging System and Image Lab software (Bio-Rad).
Silencing of NOS2 expression
NOS2 silencing was performed using lentiviral particles containing NOS2 shRNA or non-target control shRNA (Sigma-Aldrich), as previously described [18]. Quantitative real-time RT-PCR was used to confirm the downregulation of NOS2 gene.
Quantitative real-time RT-PCR
RNA extraction, cDNA synthesis and RT-PCR were performed as previously described [18]. RPL13A was used as housekeeping gene. Sequence of primers used for study were: NOS2: Forward primer: 5’-GCTGCCAAGCTGAAATTGAAT-3’; Reverse primer: 5’-GATATCTTCGTGATAGCGCTTCTG-3; CD44: Forward primer: 5’-CTGCCGCTTTGCAGGTGTA-3’; Reverse primer: 5’-CATTGTGGGCAAGGTGCTATT-3’; RPL13A: Forward primer: 5’-CCTGGAGGAGAAGAGGAAAGAGA-3’; Reverse primer: 5’-TTGAGGACCTCTGTGTATTTGTCAA-3. Data were normalized to RPL13A and relative expression was calculated using the 2−ΔΔCt method.
Immunohistochemistry
Tissue sections (4 μm) were mounted on poly-L-lysine coated slides and immunohistochemistry was performed as previously described [18]. Anti-Notch-1 antibody was used as primary antibody and immunostaining was evaluated using an optical microscope (40x) by counting the number of Notch-1 positive cells from 15 representative zones within the same preparation.
Orthotopic breast tumor model
Animal studies were performed after obtaining the approval of the Bioethics Committee of the University of Córdoba. Six-weeks-old female immunocompromised NOD/SCID mice (NOD.CB17/AlhnRj-Prkdcscid, Janvier Labs) were previously implanted with 17β-estradiol pellets (Innovative Research of America) on the lateral side of the neck. Exponentially growing MCF-7 cells were trypsinized, resuspended in BD Matrigel and implanted (4 × 106 cells) in the fourth mammary fat pad. Ten days after cells implantation tumors were palpable and animals were intraperitoneally injected once a week with c-PTIO (320 mg/kg) or vehicle (PBS) and twice a week with tamoxifen (60 mg/kg) or vehicle (10% DMSO, 10% castor oil, PBS). Tumors were measured each week with a digital caliper. At the end of experiment (20 days), mice were sacrificed, tumors were removed and final tumor volume was calculated as π/6 × (L × W × H) (L: lenght; W: width; H: height), while apparent tumor volume was estimated as L × W2/2.
Statistical analysis
GraphPad Prism 6.0 (GraphPad Software; La Jolla, CA, USA) was used for the analysis of data with unpaired parametric t-test (with Welch correction for unequal variances) or nonparametric Mann–Whitney test. Data are expressed as mean ± SEM (n = 3) and differences were considered significant when p < 0.05 (two-sided test). Free online survival analysis software (http://kmplot.com/analysis/) was used to obtain Kaplan–Meier curves [21].
Results
NO depletion with c-PTIO abolishes the capacity of breast cancer cells to form mammospheres in vitro
To analyze the role of NO in the generation and maintenance of a CSC subpopulation, we performed tumorsphere experiments to analyze the capacity of breast cancer cells to form mammospheres, which is a functional assay of self-renewal capacity. We found that the pre-treatment of MCF-7 cells with c-PTIO, a specific NO scavenger, significantly affected their mammosphere formation capacity (Fig. 1a). Furthermore, when analyzing the expression of Notch-1, which has been shown to be upregulated by NO [19, 22] and is a key cellular signaling pathway in breast CSCs self-renewal, a substantial decrease in its expression was observed with c-PTIO treatment in a dose-response manner (Fig. 1b). To confirm that the c-PTIO effect was specifically due to the removal of NO, MCF-7, MDA-MB-361 and BT-474 cells were additionally treated with the NO-donor DETANONOate. Significantly, the NO donor abolished the capacity of c-PTIO to inhibit the formation of mammospheres (Fig. 1c). Moreover, treatment of BT474 and MDA-MB-361 cells with C-PTIO also decreased Notch1 expression in a dose-response manner (Supplementary Fig. 1), confirming that NO depletion inhibits stemness in ER+ breast cancer cells. The anti-CSCs efficacy of c-PTIO and its elimination by DETANONOate was also confirmed using the SKBR3 breast cancer cell line that expresses aldehyde dehydrogenase (ALDH) enzyme, which is a specific CSC marker [23] (Fig. 2). Treatment of SKBR3 cells with c-PTIO not only inhibited mammosphere formation (Fig. 2a), but also significantly decreased the ALDH+ cell subpopulation (Fig. 2b), and these effects were reverted by with the addition of DETANONOate. Thus, the above results suggest an important regulatory role of NO in the self-renewal capacity of breast CSCs.
a Representative images and percentage of mammospheres formed after 2 weeks of seeding MCF-7 cells pre-treated during 24 h with the indicated doses of c-PTIO. b Immunoblot of Notch-1 in nuclear fractions of MCF-7 cells. Cells were treated with different concentrations of c-PTIO for 24 h and Notch-1 was detected using a specific antibody. Transcription factor II-B (TFIIB) was used as loading control. c Representative images and mammospheres percentage formed from MCF-7, MDA-MB-361 and BT-474 cells pre-treated for 24 h with c-PTIO (100 μM), in the absence or the presence of the NO-donor DETANONOate (100 μM). Scale bars: 50 μm. Data are means ± SEM of three independent experiments (*p < 0.05; **p < 0.01; ***p < 0.001 compared with control).
a Percentage of mammospheres formed after 2 weeks of seeding SKBR-3 cells pre-treated during 24 h with 100 μM c-PTIO in the presence or the absence of 100 μM DETANONOate. b SKBR-3 cells were treated with 100 μM c-PTIO and/or 100 μM DETANONOate for 24 h and ALDH+ expression was analyzed by using the ALDEFLUOR assay and flow cytometry. A specific inhibitor of ALDH (DEAB) was used as control. Quantitative cytometry data from one of these experiments is also shown (right). Data are means ± SEM of three independent experiments (*p < 0.05; **p < 0.01; ***p < 0.001 compared with control).
NOS2 deficiency inhibits mammospheres formation and the expression of CSCs-specific markers in breast cancer cells
We next investigated if the downregulation of the inducible nitric oxide synthase (NOS2) form in breast cancer cells could also impact in the CSCs subpopulation. Thus, we first generated iNOS deficient MCF-7 cells and we confirmed NOS2 silencing by the impairment of NOS2 induction (mRNA and protein) after cytokine treatment in shRNA-iNOS cells compared to control cells (Supplementary Fig. 2). Next, we analyzed the effect of NOS2 silencing in the generation and maintenance of breast CSCs. Thus, tumorosphere formation assays showed that NOS2 deficient cells had only half the capacity of control cells to form mammospheres, and in addition the generated mammospheres were of appreciably smaller size (Fig. 3a). Besides, the expression of specific breast cancer CSCs markers was impaired in NOS2 deficient cells. Hence, a significant decrease in the expression of Notch-1 was observed in MCF7 shRNA-NOS2 cells (Fig. 3b). Furthermore, flow cytometry analyses showed a 40% decrease in CD44+/CD24−/low cell subpopulation of shRNA-NOS2 MCF7 cells (Fig. 3c), whereas RNA expression studies confirmed a significant decrease in CD44 expression in these NOS2 deficient cells (Fig. 3d). Finally, expression arrays studies showed a significant decrease in the expression of several stem cell markers in MCF7 shRNA-NOS2 compared to shRNA-control cells (Supplementary Fig. 3). Therefore, these results support that the impairment of NO production through NOS2 silencing has a significant impact on stemness and CSC subpopulation of estrogen-positive breast cancer cells. Besides, our NOS2 silencing data, along with NO depletion experiments with C-PTIO, suggest that NO production positively regulates Notch1 expression in our model and provide a signaling mechanism explaining why the inhibition of NO production impacts on CSCs subpopulations.
a Representative images and percentage of mammospheres formed by shRNA-control and shRNA-NOS2 MCF-7 cells. Scale bars: 50 μm. b Notch-1 protein expression levels in shRNA-control and shRNA-NOS2 MCF-7 cells. Stain-free technology was used as loading control. c Analysis by flow cytometry of CD44+/CD24−/low subpopulation in shRNA-control and shRNA-NOS2 MCF-7 cells. d Analysis of CD44 mRNA levels in shRNA-control and shRNA-NOS2 MCF-7 cells. Data are means ± SEM of three independent experiments (*p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001 compared with control).
NO depletion with c-PTIO or NOS2-silencing increases the antitumoral efficacy of antihormonal treatment with tamoxifen
Antihormonal treatment with tamoxifen blocks the estrogen activity by competing for the binding of this hormone to the estrogen receptor alpha [4]. Various studies indicate that resistance to treatment with this drug in breast cancer is associated with alterations in breast cancer CSC-related signaling pathways, such as increased expression of CD44, Nanog and Oct3/4 [24]. Other studies have shown that cross-talk between Notch-1 and ER signaling pathways plays a key role in the resistance to antihormonal therapy in breast cancer [25, 26].
Therefore, we decided to investigate the impact of NO depletion or NOS2 deficiency in the sensitivity of breast cancer cells to tamoxifen. To this end, the antiproliferative activity of tamoxifen was analyzed in both breast cancer ER+ cells treated with c-PTIO and in MCF-7 shRNA-NOS2 cells. As shown in Fig. 4a, the selective elimination of NO with c-PTIO in ER+, MCF-7, MDA-MB-361 and BT-474 cells increased the antiproliferative effect of tamoxifen. In agreement with these results, NOS-2-silenced MCF-7 cells were significantly more sensitive to this antihormonal drug than the corresponding controls (Fig. 4b). Moreover, tamoxifen treatment in sh-RNA-NOS2 cells was more effective in reducing their mammosphere formation ability (Fig. 4c) and Notch1 expression levels (Fig. 4d) than in control cells. Therefore, the above results suggest that NO-targeted treatments increase the antitumoral efficacy of tamoxifen in ER+ breast cancer cells.
a Breast cancer cells were treated with c-PTIO (60 μM for MCF-7 and 40 μM for MDA-MB-361 and BT-474) and/or 4-Hydroxytamoxifen (4HT, 0.05 μM for MCF-7 and 0.1 μM for MDA-MB-361 and BT-474). Cell proliferation was determined after 96 h of treatment using the incuCyte ZOOM Software. b Cell proliferation of shRNA-control and shRNA-NOS2 MCF-7 cells treated with different concentrations of 4HT during 96 h. c Representative images and percentage of mammospheres formed by shRNA-control and shRNA-NOS2 MCF-7 cells pre-treated for 24 h with different concentrations of 4HT. Scale bars: 50 μm. d Immunoblot analysis of Notch-1 protein expression levels in shRNA-control and shRNA-NOS2 MCF-7 cells treated with different concentrations of 4HT during 24 h. Stain-free technology was used as loading control. Data are means ± SEM of three independent experiments (*p < 0.05; **p < 0.01; ***p < 0.001 compared with control).
Tamoxifen resistance is associated with increased expression of NOS2 and stem cells markers in ER+ breast cancer cells
We next developed tamoxifen-resistant breast cancer cells as a model for the acquisition of resistance to estrogen antagonists that occurs in breast cancer patients. When MCF-7 cells were cultured in presence of tamoxifen, cell growth rate was greatly reduced, but eventually cells adapted to the new environment, which resulted in two tamoxifen-resistant (TamR) cell lines: MCF-7 0.1μMTamR (cells resistant to 0.1 μM tamoxifen) and MCF-7 2μMTamR (cells resistant to 2 μM tamoxifen). As expected, cell proliferation of parental MCF-7 was effectively reduced by tamoxifen, while MCF-7 TamR cells grew normally, unaffected by the presence of tamoxifen (Fig. 5a). Notably, MCF-7 TamR cells displayed higher NOS2 (Fig. 5b) and Notch-1 (Fig. 5c) protein expression levels, compared to MCF-7 parental cells. Although we did not observe differences in the capacity of TamR MCF-7 cells to form mammospheres in comparison to parental cells, TamR MCF-7 cells-derived organoids not only displayed higher expression levels of Notch 1 but also expressed higher levels of Sox-2 (Supplementary Fig. 4) than their parental counterparts, reinforcing the notion that both NO and CSCs signaling are associated with tamoxifen resistance in ER+ breast cancer cells.
a MCF-7 0.1 μMTamR (cells resistant to 0.1 μM tamoxifen) and MCF-7 2 μMTamR (cells resistant to 2 μM tamoxifen) were treated with different concentrations of 4HT and cell proliferation was determined after 96 h of treatment using the incuCyte ZOOM Software. b Immunoblot and analysis of NOS2 protein expression in MCF-7 0.1 μMTamR and MCF-7 2 μMTamR after treatment with a cytokine cocktail (CK) for 24 h to induce NOS2 expression. The graph shows the percentage of induction of NOS2 protein in control and TamR cells. Stain-free technology was used as loading control. c Immunoblot analysis of Notch-1 expression levels in MCF-7 0.1 μMTamR and MCF-7 2 μMTamR. Stain-free technology was used as loading control. Data are means ± SEM of three independent experiments (*p < 0.05; **p < 0.01; ***p < 0.001 compared with control).
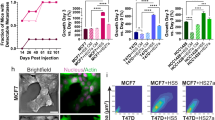
NO-targeted therapy in vivo with c-PTIO increases the efficacy of tamoxifen in an orthotopic breast tumor model
We next decided to explore whether NO-targeted therapy in vivo with c-PTIO could enhance the effectiveness of antitumor treatment with tamoxifen. To this end, we developed an orthotopic breast tumor model in immunodeficient mice by grafting MCF-7 tumor cells into the mammary adipose and then animals were treated with c-PTIO 320 mg/kg once a week and tamoxifen 60 mg/kg twice a week.
Notably, the combined NO-targeted therapy with tamoxifen significantly decreased tumor growth and was more effective than either treatment alone (Fig. 6a). As a result, final tumor volumes in c-PTIO plus tamoxifen treated animals were less than one-third of those in untreated control mice (Fig. 6b). Moreover, when Notch-1 expression was analyzed by immunohistochemistry, it was found more significantly decreased in tumors of mice treated with the combination of c-PTIO with tamoxifen, than with either treatment alone. Thus, NO depletion significantly increased the efficacy of tamoxifen, causing a substantial decrease in Notch-1 expression and tumor size.
a MCF-7 cells were injected into the mammary fat pad of immunocompromised NOD/SCID mice and then animals were treated with c-PTIO (320 mg/kg once a week) and tamoxifen (60 mg/kg twice a week). Apparent tumor volume (mm3) was measured during the course of treatment. b Final tumor volume was analyzed after harvesting. The graph shows final tumor volume (mm3) normalized to initial apparent volume. c Representative images from the immunohistochemical analysis of Notch-1 expression in xenografts. Scale bars: 50 μm. The graph shows the average number of Notch-1 positive cells from 15 representative zones within the same tissue preparation in each experimental group (*p < 0.05; **p < 0.01; ***p < 0.001 compared with control).
Low NOS2 expression was significantly associated with a higher metastasis-free survival in ER+ breast cancer patients treated with tamoxifen
The results described above suggest that NO plays an important role in the mechanisms of resistance to antihormonal treatment with tamoxifen in breast cancer. We therefore decided, to investigate whether the expression of NOS2 in breast cancer also had impact on patient survival in breast cancer patients treated with tamoxifen. To this end, an on-line tool was used to analyze NOS2 expression of patients with breast cancer treated or not with tamoxifen and to obtain Kaplan–Meier curves from gene expression and metastasis-free survival data of about 300 patients [21]. As shown in Fig. 7, a higher expression of NOS2 was significantly associated with lower survival in patients with ER+ tumors treated with tamoxifen. Of note, this difference in metastasis-free survival was not observed in ER+ breast cancer patients treated with chemotherapy. Therefore, survival data support that a higher NOS2 expression provides an adaptive advantage for ER-positive tumors treated with tamoxifen, resulting in lower patient metastasis-free survival rates.
Metastasis-free survival rates of ER+ breast cancer patients treated with tamoxifen or chemotherapy, according to NOS2 gene expression in their tumors. Kaplan–Meier curves were made using the on-line Kaplan–Meier plotter tool (http://kmplot.com/analysis/). All possible cut-off values between the lower and upper quartiles were computed and the best performing threshold was used as a cut-off and the levels of NOS2 expression that are below or above this threshold are considered as low or high expression, respectively.
Discussion
NO is an important mediator involved in important physiological processes, and also plays a significant role in tumor biology, since exposure of cancer cells to low NO concentrations can stimulate cell survival pathways, increasing angiogenesis and contributing to tumor progression and metastasis [27]. NO signaling mediated by NOS2 has been associated with worse survival in patients with breast cancer, as tumor aggressiveness increases [14]. However, although an important role of NO in CSCs has been described in solid tumors [16,17,18,19], to date studies on NO capacity in the generation and maintenance of CSCs in breast cancer have not been performed.
Our results indicate that NO removal with c-PTIO in breast cancer cells ER+ (MCF-7, MDA-MB-361, BT-474) or ER− (SKBR-3) decreased their ability to form mammospheres, which is a functional assay for the characteristic self-renewal capacity of CSCs [28]. Moreover, this effect of c-PTIO was specifically due to NO removal, since the pre-treatment with a NO donor abolished the anti-CSC capacity of NO scavenging. Notch-1 signaling pathway is important in CSCs self-renewal, cell proliferation and differentiation and apoptosis in breast cells [8]. In fact, endothelial nitric oxide synthase (eNOS) has been reported to activate Notch signaling and to promote in vitro neurospheres formation after NO treatment in gliobastoma [19]. Also, more recently we reported that NO depletion in colorectal cancer cells impaired CSC-specific signaling pathways, including Notch [18]. In the present study, the anti-CSCs capacity of NO elimination in breast cancer cells was associated with a decrease in Notch-1 expression. Another important CSC marker in breast cancer is ALDH1, which is expressed selectively in ER− or triple negative breast tumors [29]. Therefore, its expression was analyzed in SKBR-3 cells, an ER− breast cancer cell line, confirming that ALDH+ population decreased significantly in c-PTIO presence, while this anti-CSCs effect was significantly attenuated in the presence of a NO donor. These results indicate, as a whole, that NO plays an important role in the maintenance of stem characteristics in breast cancer cells. Given that iNOS is the main source of NO production in epithelial cells, we decided to functionally address its participation in the generation and maintenance of CSCs subpopulation in MCF-7 cells. In this regard, our study shows that a significant decrease in iNOS mRNA and protein levels in shRNA-NOS2 MCF-7 cells was associated with a decrease in their ability to form mammospheres. Therefore, these data support that NOS2 also plays an important role in CSC generation and maintenance in ER+ breast cancer cells. Similarly, NOS2 downregulation in glioblastoma cells [16] and colon cancer cells [17] has been reported to reduce their ability to form neurospheres and colonospheres, respectively. Moreover, we show that NOS2 silencing also downregulated CSCs markers such as CD44, Notch, and stem cells specific markers, with a significant decrease in OCT-4 and Nanog expression, among others. Actually, CD44+/CD24− breast cancer cells have been reported to express high levels of OCT-4, which can also be a biomarker of progression and prognosis in breast cancer [30]. On the other hand, a decrease in Nanog expression has been shown to suppress the CSCs population in breast cancer [31]. Moreover, CD44+ and ALDH1+ breast cancer cells populations have been associated with adverse features in ER+ breast cancers, including Ki67 as well as basal markers [32], and with poor prognosis [33]. Therefore, all these data indicate that the impairment of NO production through NOS2 silencing has a significant impact on stemness and CSC subpopulation in ER+ breast cancer cells.
CSCs are more resistant than differentiated tumor cells to therapies used in clinics [34, 35]. This suggests that the alteration of NO production in breast cancer cells, and therefore in the development and maintenance of CSCs, could help to increase the sensitivity to antitumor therapies. Tamoxifen is the most common and effective antiestrogenic therapy for ER+ breast cancer patients and is also used to prevent breast cancer development in high risk patients [36]. Tamoxifen blocks estrogen activity by competing for the binding site of ER-α receptor, resulting in the inhibition of ER-α-regulated gene transcription and estrogen-dependent tumors growth [37, 38]. However, almost 50% of ER+ breast cancer patients acquire resistance to tamoxifen and do not respond to treatment [6]. Importantly, our results show that both NO depletion with c-PTIO and NOS2-silencing enhanced the response of MCF-7 cells antihormonal treatment with tamoxifen. This higher efficacy of tamoxifen in NO-impaired MCF-7 cells may be related to alteration of CSC-related characteristics. Thus, a number of studies have reported that resistance to treatment with tamoxifen in breast cancer is associated with CSC-related signaling pathways [7]. Besides, the acquired resistance to tamoxifen in MCF-7 cells has been shown to be accompanied by an increase in CD44 [39], Nanog and Oct3/4 expression [40]. Other studies have shown that the cross-talk between Notch and ER plays a fundamental role in resistance to antihormonal therapy in breast cancer [7]. Thus, the Notch silencing in breast cancer cells is capable of increasing their sensitivity to tamoxifen [26]. In agreement with these studies, our results support that tamoxifen treatment in NOS-2-silenced cells was more effective in the reduction of their mammosphere formation ability and Notch1 expression levels. In agreement with the results obtained in vitro, we found an impaired tumor growth capacity in mice treated with NO-targeted therapy plus tamoxifen, which formed tumors significantly smaller than those of untreated mice. Notably, the tumors in those mice treated with tamoxifen plus NO depletion showed a diminished expression of Notch-1 expression in comparison with either treatment alone. Therefore, the combination of tamoxifen with the inhibition of NO production can be an effective treatment in ER+ breast cancer patients, by decreasing the resistance to this antitumor drug. Furthermore, because the development of resistance to tamoxifen remains an important clinical problem in breast cancer patients, we demonstrate that tamoxifen-resistant MCF-7 cells express higher levels of NOS2 and Notch-1 than parental breast cancer cells. Consequently, these signaling pathways are associated with tamoxifen resistance in ER+ breast cancer cells.
A number of reports have demonstrated the association between NOS2 and poor outcome in a variety of cancers, including ER− breast cancer [14, 41]. However, our results suggest that NOS2 expression in ER+ tumors may also have a prognostic value in patients receiving antihormonal treatment with tamoxifen. Actually, we show that a higher NOS2 expression was significantly associated with lower metastasis-free survival rate in ER+ breast cancer patients treated with tamoxifen. Importantly, NOS2 expression was not associated with survival in ER+ patients receiving chemotherapy, indicating that NOS2 expression in ER+ tumors is specifically associated with their sensitivity to tamoxifen and is not due to the correlation with grade or other prognostic histopathological and immunophenotypical factors.
In summary, our data show that the impairment of NO production in ER+ breast cancer cells decreases those functional and molecular characteristics related to CSCs, suggesting that NO plays an important role in the biology of this cellular subpopulation in these tumors. Moreover, NO-targeted therapy reduced stem characteristics and increased the sensitivity to treatment with tamoxifen, whereas tamoxifen resistance in ER+ breast cancer cells was associated with NOS2 upregulation. These results may explain why a higher NOS2 expression is associated with lower survival in ER+ breast cancer patients treated with tamoxifen. Therefore, NO-targeted therapy in ER+ breast cancer may contribute to increase the efficacy of antihormonal therapy avoiding the development of resistance to these treatments.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Wang L, Gallo KA, Conrad SE. Targeting mixed lineage kinases in ER-positive breast cancer cells leads to G2/M cell cycle arrest and apoptosis. Oncotarget. 2013;4:1158–71.
Lumachi F, Luisetto G, Basso SMM, Basso U, Brunello A, Camozzi V. Endocrine therapy of breast cancer. Curr Med Chem. 2011;18:513–22.
Osborne CK. Tamoxifen in the treatment of breast cancer. N Engl J Med. 1998;339:1609–18.
Jager NG, Linn SC, Schellens JH, Beijnen JH. Tailored tamoxifen treatment for breast cancer patients: a perspective. Clin Breast Cancer. 2015;15:241–4.
García-Becerra R, Santos N, Díaz L, Camacho J. Mechanisms of resistance to endocrine therapy in breast cancer: focus on signaling pathways, mirnas and genetically based resistance. Int J Mol Sci. 2013;14:108–45.
Rodriguez D, Ramkairsingh M, Lin X, Kapoor A, Major P, Tang D. The central contributions of breast cancer stem cells in developing resistance to endocrine therapy in estrogen receptor (ER)-positive breast cancer. Cancers. 2019;11:1028.
Harrison H, Farnie G, Brennan KR, Clarke RB. Breast cancer stem cells: something out of notching? Cancer Res. 2010;70:8973–6.
Acar A, Simões BM, Clarke RB, Brennan K. A role for notch signalling in breast cancer and endocrine resistance. Stem Cells Int. 2016;2016:2498764–6.
Aranda E, López-Pedrera C, De La Haba-Rodriguez JR, Rodríguez-Ariza A. Nitric oxide and cancer: the emerging role of S-nitrosylation. Curr Mol Med. 2012;12:50–67.
Peñarando J, Aranda E, Rodríguez-Ariza A. Immunomodulatory roles of nitric oxide in cancer: tumor microenvironment says ‘NO’ to antitumor immune response. Transl Res. 2019;210:99–108.
Somasundaram V, Basudhar D, Bharadwaj G, No JH, Ridnour LA, Cheng RYS, et al. Molecular mechanisms of nitric oxide in cancer progression, signal transduction, and metabolism. Antioxid Redox Signal. 2019;30:1124–43.
López-Sánchez LM, Aranda E, Rodríguez-Ariza A. Nitric oxide and tumor metabolic reprogramming. Biochem Pharmacol. 2020;176:113769. https://doi.org/10.1016/j.bcp.2019.113769
Glynn SA, Boersma BJ, Dorsey TH, Yi M, Yfantis HG, Ridnour LA, et al. Increased NOS2 predicts poor survival in estrogen receptor-negative breast cancer patients. J Clin Invest. 2010;120:3843–54.
Ambs S, Glynn SA. Candidate pathways linking inducible nitric oxide synthase to a basal-like transcription pattern and tumor progression in human breast cancer. Cell Cycle. 2011;10:619–24.
Eyler CE, Wu Q, Yan K, MacSwords JM, Chandler-Militello D, Misuraca KL, et al. Glioma stem cell proliferation and tumor growth are promoted by nitric oxide synthase-2. Cell. 2011;146:53–66.
Puglisi MA, Cenciarelli C, Tesori V, Cappellari M, Martini M, Di Francesco AM, et al. High nitric oxide production, secondary to inducible nitric oxide synthase expression, is essential for regulation of the tumour-initiating properties of colon cancer stem cells. J Pathol. 2015;236:479–90.
Peñarando J, López-Sánchez LM, Mena R, Guil-Luna S, Conde F, Hernández V, et al. A role for endothelial nitric oxide synthase in intestinal stem cell proliferation and mesenchymal colorectal cancer. BMC Biol. 2018;16:1–14.
Charles N, Ozawa T, Squatrito M, Bleau AM, Brennan CW, Hambardzumyan D, et al. Perivascular nitric oxide activates notch signaling and promotes stem-like character in PDGF-induced glioma cells. Cell Stem Cell. 2010;6:141–52.
Cañas A, López-Sánchez LM, Valverde-Estepa A, Hernández V, Fuentes E, Muñoz-Castañeda JR, et al. Maintenance of S-nitrosothiol homeostasis plays an important role in growth suppression of estrogen receptor-positive breast tumors. Breast Cancer Res. 2012;14:R153.
Győrffy B, Lanczky A, Eklund AC, Denkert C, Budczies J, Li Q, et al. An online survival analysis tool to rapidly assess the effect of 22,277 genes on breast cancer prognosis using microarray data of 1,809 patients. Breast Cancer Res Treat. 2010;123:725–31.
Ishimura N, Bronk SF, Gores GJ. Inducible nitric oxide synthase up-regulates Notch-1 in mouse cholangiocytes: implications for carcinogenesis. Gastroenterology. 2005;128:1354–68.
Marcato P, Dean CA, Giacomantonio CA, Lee PW. Aldehyde dehydrogenase: its role as a cancer stem cell marker comes down to the specific isoform. Cell Cycle. 2011;10:1378–84.
Kim SY, Kang JW, Song X, Kim BK, Yoo YD, Kwon YT, et al. Role of the IL-6-JAK1-STAT3-Oct-4 pathway in the conversion of non-stem cancer cells into cancer stem-like cells. Cellular Signal. 2013;25:961–9.
Al-Hussaini H, Subramanyam D, Reedijk M, Sridhar SS. Notch signaling pathway as a therapeutic target in breast cancer. Mol Cancer Ther. 2011;10:9–15.
Rizzo P, Miao H, D’Souza G, Osipo C, Song LL, Yun J, et al. Cross-talk between notch and the estrogen receptor in breast cancer suggests novel therapeutic approaches. Cancer Res. 2008;68:5226–35.
Mocellin S, Bronte V, Nitti D. Nitric oxide, a double edged sword in cancer biology: searching for therapeutic opportunities. Med Res Rev. 2007;27:317–52.
Dontu G, Wicha MS. Survival of mammary stem cells in suspension culture: implications for stem cell biology and neoplasia. J Mammary Gland Biol Neoplasia. 2005;10:75–86.
Charafe-Jauffret E, Ginestier C, Iovino F, Wicinski J, Cervera N, Finetti P, et al. Breast cancer cell lines contain functional cancer stem cells with metastatic capacity and a distinct molecular signature. Cancer Res. 2009;69:1302.
Liu CG, Lu Y, Wang BB, Zhang YJ, Zhang RS, Lu Y, et al. Clinical implications of stem cell gene Oct-4 expression in breast cancer. Ann Surg. 2011;253:1165–71.
Han ML, Wang F, Gu YT, Pei XH, Ge X, Guo GC, et al. MicroR-760 suppresses cancer stem cell subpopulation and breast cancer cell proliferation and metastasis: By down-regulating NANOG. Biomed Pharmacother. 2016;80:304–10.
Tsang JY, Huang YH, Luo MH, Ni YB, Chan SK, Lui PC, et al. Cancer stem cell markers are associated with adverse biomarker profiles and molecular subtypes of breast cancer. Breast Cancer Res Treat. 2012;136:407–17.
Ricardo S, Vieira AF, Gerhard R, Leitão D, Pinto R, Cameselle-Teijeiro JF, et al. Breast cancer stem cell markers CD44, CD24 and ALDH1: expression distribution within intrinsic molecular subtype. J Clin Pathol. 2011;64:937–46.
Li X, Lewis MT, Huang J, Gutierrez C, Osborne CK, Wu MF, et al. Intrinsic resistance of tumorigenic breast cancer cells to chemotherapy. J Natl Cancer Inst. 2008;100:672–9.
Vermeulen L, de Sousa e Melo F, Richel DJ, Medema JP. The developing cancer stem-cell model: clinical challenges and opportunities. Lancet Oncol. 2012;13:e83–9.
Schiff R, Massarweh S, Shou J, Osborne CK. Breast cancer endocrine resistance: how growth factor signaling and estrogen receptor coregulators modulate response. Clin Cancer Res. 2003;9:447S–54S.
Wang Z, Li Y, Ahmad A, Azmi AS, Banerjee S, Kong D, et al. Targeting Notch signaling pathway to overcome drug resistance for cancer therapy. Biochim Biophys Acta. 2010;1806:258–67.
Kotta-Loizou I, Vasilopoulos SN, Coutts RH, Theocharis S. Current evidence and future perspectives on HuR and breast cancer development, prognosis, and treatment. Neoplasia. 2016;18:674–88.
Hiscox S, Baruha B, Smith C, Bellerby R, Goddard L, Jordan N, et al. Overexpression of CD44 accompanies acquired tamoxifen resistance in MCF7 cells and augments their sensitivity to the stromal factors, heregulin and hyaluronan. BMC Cancer. 2012;12:458.
Arif K, Hussain I, Rea C, El-Sheemy M. The role of Nanog expression in tamoxifen-resistant breast cancer cells. Onco Targets Ther. 2015;8:1327–34.
Granados-Principal S, Liu Y, Guevara ML, Blanco E, Choi DS, Qian W, et al. Inhibition of iNOS as a novel effective targeted therapy against triple-negative breast cancer. Breast Cancer Res. 2015;17:25.
Acknowledgements
This work was supported by funding from Consejería de Salud, Junta de Andalucía through the project PI-0268-2014 and Instituto de Salud Carlos III through the projects PI13/00553 and PI16/01508 (co-funded by the European Regional Development Fund/ European Social Fund “Investing in your future”). ARA was funded with a researcher contract through the program “Nicolás Monardes” from Junta de Andalucía. We gratefully acknowledge the technical help of Esther Peralbo from the Citometry Unit at the IMIBIC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
López-Sánchez, L.M., Mena, R., Guil-Luna, S. et al. Nitric oxide-targeted therapy inhibits stemness and increases the efficacy of tamoxifen in estrogen receptor-positive breast cancer cells. Lab Invest 101, 292–303 (2021). https://doi.org/10.1038/s41374-020-00507-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41374-020-00507-z