Abstract
Oncotype DX (Genomic Health, Redwood City, CA, USA, current list price $4,350.00) is a multigene quantitative reverse transcription-polymerase chain reaction-based assay that estimates the risk of distant recurrence and predicts chemotherapy benefit for patients with estrogen receptor (ER)-positive breast cancers. Studies have suggested that standard histologic variables can provide similar information. Klein and Dabbs et al have shown that Oncotype DX recurrence scores can be estimated by incorporating standard histologic variables into equations (Magee equations). Using a simple modification of the Magee equation, we predict the Oncotype DX recurrence score in an independent set of 283 cases. The Pearson correlation coefficient (r) for the Oncotype DX and average modified Magee recurrence scores was 0.6644 (n=283; P<0.0001). 100% of cases with an average modified Magee recurrence score>30 (n=8) or an average modified Magee recurrence score<9 (with an available Ki-67, n=5) would have been correctly predicted to have a high or low Oncotype DX recurrence score, respectively. 86% (38/44) of cases with an average modified Magee recurrence score≤12, and 89% (34/38) of low grade tumors (NS<6) with an ER and PR≥150, and a Ki-67<10%, would have been correctly predicted to have a low Oncotype DX recurrence score. Using an algorithmic approach to eliminate high and low risk cases, between 5% and 23% of cases would potentially not have been sent by our institution for Oncotype DX testing, creating a potential cost savings between $56,550.00 and $282,750.00. The modified Magee recurrence score along with histologic criteria may be a cost-effective alternative to the Oncotype DX in risk stratifying certain breast cancer patients. The information needed is already generated by many pathology laboratories during the initial assessment of primary breast cancer, and the equations are free.
Similar content being viewed by others
Main
Breast cancer is the most common non-cutaneous cancer in women, and the second most frequent cause of cancer death among women.1 Approximately 50% of breast cancer cases are estrogen receptor (ER)-positive.2 A major challenge in the treatment planning for breast cancer is to identify those patients who are more likely to develop recurrence, so that the most appropriate therapeutic regimen can be provided. The decisions around systemic therapy in breast cancer have traditionally been based on combinations of clinical and histopathologic risk factors including measures of proliferation,3 tumor size,4 histologic grade,5 as well as lymph node staging.6 In addition, breast cancer biomarkers including ER, progesterone receptor (PR), and the human epidermal growth factor receptor-2 (HER-2), are routinely assessed to provide further prognostic information as well as to help identify subsets of patients who are appropriate for specific targeted therapies.7, 8, 9 These prognostic markers are very useful for identifying the higher risk triple negative or HER-2-positive cases; however, it remains challenging to accurately assess individual risk and the need for systemic chemotherapy for the lower risk subset of hormone receptor-positive patients on a case by case basis.
Over the last decade, molecular approaches, including multigene assays for predicting prognosis and treatment response, have entered into the clinical arena of breast cancer care.10, 11 Oncotype DX (Genomic Health, Redwood City, CA, USA) is a 21-gene commercial quantitative reverse transcription-polymerase chain reaction-based assay that quantifies the expression of 16 cancer-related genes. The remaining five genes are used to check RNA integrity and normalize expression levels.12 The Oncotype DX test has been shown to be prognostic12 and to be predictive of chemotherapy benefit13 in ER-positive lymph node-negative breast cancer patients. There is some evidence to suggest that the use of Oncotype DX testing can provide additional information in predicting recurrence in women with lymph node-positive breast cancer as well.14 Oncotype DX uses quantitative reverse transcription-polymerase chain reaction and an algorithm to calculate a recurrence score, giving the highest weight to proliferation (which includes Ki-67), followed by HER-2, ER, and PR. The Oncotype DX recurrence score is reported as a number that is divided into either low (<18), intermediate (18–30), or high (>30) recurrence risk categories.
Several studies have suggested that standard histopathologic variables can provide information similar to that provided by the Oncotype DX recurrence score.15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27 Four of the 16 genes (ER, PR, HER-2, and Ki-67) measured as parts of the Oncotype DX panel are routinely assessed at the protein level by immunohistochemistry28 in the routine diagnostic evaluation of breast cancer. Four linear regression analysis equations (Magee equations) have been published15, 16 using several histopathologic variables, and semiquantitative results from these four immunophenotypic markers (ER, PR, HER-2, and Ki-67). In these studies,15, 16 it was shown that standard histopathological variables in combination with semiquantitative ER, PR, HER-2, and Ki-67 results can be used in the Magee equations to calculate a recurrence score which correlated well with the Oncotype DX recurrence score, and provided information similar to that found in the Oncotype DX recurrence score.
The Magee equations use a semiquantitative scoring for ER and PR (the H-score) not used by all pathologists. In the current study, we have used a modification of the Magee equations in an institutional cohort of breast cancer cases that were sent for Oncotype DX from the University of Rochester Medical Center, Rochester, NY, USA. Our goal was to investigate whether or not these modified Magee equations, along with specific histologic and immunohistochemical criteria, might represent a cost-effective alternative method of identifying ER-positive breast cancer patients who might either safely benefit from, or safely avoid, systemic chemotherapy.
Materials and methods
Patients and Data Retrieval
A total of 299 cases with available Oncotype DX recurrence scores were identified from the pathology files at the University of Rochester Medical Center (2009–2013). Demographic information on age was extracted from the medical record. All tumor H&E slides and immunohistochemistry were reviewed by at least two board-certified breast pathologists, with manual interpretation of ER, PR, HER-2, and Ki-67 (FDA-approved test kits (DAKO) - ERα (clones ID5 and ER-2-123); PR (clone PgR1294) pharmDxTM; Rabbit anti-human HER-2 HercepTestTM; Monoclonal mouse anti-human Ki-67 antigen (clone MIB-1, code M7240)). Fluorescence in situ hybridization was performed (FDA-approved test kit (DAKO) - HER-2 IQFISH pharmDxTM) on all equivocal HER-2 immunohistochemistry results, and the fluorescence in situ hybridization results were used in lieu of the immunohistochemistry for these cases. The Nottingham score (NS) was calculated using the Nottingham modification of the Bloom-Richardson system.5 Information on tumor size was extracted from the pathology report. Sixteen cases were excluded because of lack of complete information on either NS, ER, PR, HER-2, or tumor size. A total of 283 cases (241 of these with Ki-67 results) were subsequently evaluated (244 invasive ductal carcinomas and 39 invasive lobular carcinomas).
Study Design
Flanagan et al15 published the original Magee equation (recurrence score=13.424+5.420 (nuclear grade)+5.538 (mitotic count) −0. 045 (ER H-score) −0.030 (PR H-score)+9.486 (0 for HER-2 negative/equivocal and 1 for positive)) as a model to predict the Oncotype DX recurrence score. In a subsequent paper, building on the original equation, Klein et al16 published three additional Magee equations (#1, #2, and #3) using different combinations of standard histopathologic variables (NS, ER, PR, HER-2, Ki-67, and tumor size). Using these most recent equations,16 we calculated a modified Magee recurrence score by modifying the H-score for ER and PR. The H-score used in the original Magee equations estimates the percentage (0–100) of cells that are positive for each particular level of intensity (grade 0–3), multiplies this percentage by that intensity, and then adds the total of the percentage multiplied by intensity for the three intensity grades. For example, a sample block consisting of 100 tumor cells with an intensity of grade 0 in 10 cells, grade 1 in 20 cells, grade 2 in 50 cells, and grade 3 in 20 cells would give an H-score of ((0 × 10)+(1 × 20)+(2 × 50)+(3 × 20))=180. We estimated the H-score by considering the average intensity of staining, which is essentially the H-score/100:

We used the predominant intensity grade as a surrogate for the average intensity of staining, and multiplied this number by the total percentage of cells which stained positive. In the example given above, the actual average intensity of staining would have been 1.8. The predominant stating pattern would have been estimated to be 2. Ninety out of 100 of the cells stained positive. The estimated H-score would be 2 × 90=180. We also used the average of the three modified Magee recurrence scores to generate an average modified Magee recurrence score. If the modified Magee recurrence scores #1 and #3 were not calculated owing to unavailability of Ki-67 results, the modified Magee recurrence score #2 (which does not require a Ki-67) was used as a surrogate for the average modified Magee recurrence score.
Statistical Analysis
Available clinical and pathologic data were summarized using percentages, descriptive statistics (mean, range, frequencies) and inferential statistics (t-test). The risk categories used by the Oncotype DX recurrence score (low (<18), intermediate (18–30), or high (>30)) were applied to the modified Magee recurrence score, and the modified Magee recurrence scores were compared with their paired Oncotype DX recurrence scores for correlation (Pearson correlation) and concordance. We compared the average modified Magee recurrence score, ER, PR, and Ki-67 values at several cutoff points to determine how they stratified into the high and low Oncotype DX recurrence score risk stratification groups. The various cutoff points were then examined to determine which types of cases had the greatest likelihood of stratifying into either a high or low Oncotype DX risk stratification group, with the lowest likelihood of discordance. On the basis of these cutoff points, an algorithm was then created for which cases to consider sending for Oncotype DX testing. All data analyses were performed using the statistical Analysis ToolPak (Microsoft Excel Office 2010 version 14.0.7015.100) except for the likelihood ratios, which were performed using JavaStat 2-way Contingency Table Analysis (revised version 7/23/2013 http://statpages.org/ctab2x2.html). For all results, a P-value of<0.05 was considered significant.
Results
A summary of clinicopathologic features in the patient population is detailed in Table 1.
Correlation and Concordance between Modified Magee Recurrence Score and Oncotype DX Recurrence Score
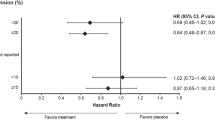
There was an overall 68% (n=241), 68% (n=283), 70% (n=241), and 70% (n=283) agreement between the modified Magee recurrence score (equations #1, #2, #3 and the average modified Magee recurrence score, respectively) and the Oncotype DX recurrence score. The correlation between recurrence score and NS, ER, PR, HER-2, Ki-67, and tumor size was similar in both the modified Magee recurrence scores and the Oncotype DX recurrence score (Table 1), with a pattern of increasing recurrence score with increasing NS, HER-2, Ki-67, and tumor size, and a pattern of increasing recurrence score with decreasing ER and PR. The average recurrence score, NS, ER, PR, Ki-67, HER-2, and tumor size for modified Magee recurrence score equations #1, #2, and #3 were not statistically different from the average recurrence score, NS, ER, PR, Ki-67, Her-2, and tumor size for the average modified Magee recurrence score (P>0.1). The Pearson correlation coefficient (r) for the average modified Magee recurrence score and Oncotype DX recurrence score was 0.6644 (n=283; P<0.0001) with an average coefficient of determination (r2) of 0.4414 (Figure 1). Following the criteria set by the Oncotype DX recurrence score for low, intermediate, and high risk categories, there was no ‘two-step’ discordance (discordant high and low recurrence scores) between any modified Magee recurrence score and their paired Oncotype DX recurrence score (Table 2, and Supplementary Appendix—Supplementary Tables 1, 2, and 3).
Oncotype DX Recurrence Score, Average Modified Magee Recurrence Score, and General Histologic Characteristics
There were consistently significant differences (P<0.05) between the Oncotype DX risk stratification categories (low, intermediate, and high) for NS, ER, PR, and Ki-67, but not for HER-2 and tumor size (P>0.05). The NS, PR, and Ki-67 values consistently showed greater statistical significance between risk stratification categories than the ER values. The histologic grades risk stratified by Oncotype DX recurrence score, with concurrent mean Oncotype DX recurrence score, average modified Magee recurrence score, ER, PR, and Ki-67 values are shown in Table 3 (Supplementary Appendix).
100% (n=222) of cases with an average modified Magee recurrence score<21.5 had an Oncotype DX recurrence score<30 (range 0–28). 68% of these cases (151/222) had an Oncotype DX recurrence score<18 (LR= 1.61, P<0.005). The average of the average modified Magee recurrence score, NS, ER, PR, and Ki-67 values for the 151 cases with an Oncotype DX recurrence score<18 (127 with an available Ki-67) was 14.4, 5.1, 256.2, 219.4, and 10.5, respectively. The average of the average modified Magee recurrence score, NS, ER, PR, and Ki-67 values for the 71 cases with an Oncotype DX recurrence score≥18 (61 with an available Ki-67) was 16.5, 5.6, 259.6, 173.1, and 13.5, respectively.
100% (n=141) of low grade tumor (NS<6) had an Oncotype DX recurrence score<30 (range 0–28). 1% (1/71) of cases with a NS of 6 had an Oncotype DX recurrence score>30 (range 2–49). 7% (2/29) of cases with a NS of 7 had an Oncotype DX recurrence score>30 (range 9–32). 21% (6/29) of cases with a NS of 8 had an Oncotype DX recurrence score>30 (range 0–78). 54% (7/13) of cases with a NS of 9 had an Oncotype DX recurrence score>30 (range 12–44).
For cases with an available Ki-67 (n=241), 100% of cases that had a Ki-67<10% (n=94) also had an Oncotype DX recurrence score<30 (range 0–28). 73% of these cases (69/94) had an Oncotype DX recurrence score<18 (LR=2.17, P<0.005). The average of the average modified Magee recurrence score, NS, ER, PR, and Ki-67 values for these 69 cases with an Oncotype DX recurrence score<18 was 13.9, 4.8, 256.6, 201.8, and 5.2, respectively. The average of the average modified Magee recurrence score, NS, ER, PR, and Ki-67 values for the 25 cases with an Oncotype DX recurrence score≥18 was 16.3, 5.2, 253.3, 134.2, and 4.2, respectively.
100% (n=38) of low grade tumors with an ER and PR≥150, and a Ki-67<10%, had an Oncotype DX recurrence score≤25 (range 0–25). Eighty-nine percent of these cases (34/38) had an Oncotype DX recurrence score<18 (LR=2.13 (when compared with tumors with a NS≥6 with similar histologic characteristics), P=0.02). Three of the four cases with an Oncotype DX recurrence score≥18 are represented in Table 3. The fourth case had an Oncotype DX recurrence score of 18.
100% (n=5) of tumors with an ER≤180, PR≤15, and Ki-67≥45% had an Oncotype DX recurrence score>30, and all were high grade (NS≥8).
Cases with an Average Modified Magee Recurrence Score<18
100% of cases with an average modified Magee recurrence score<18 (n=173) had an Oncotype DX recurrence score<30 (range 0–28). 75% (129/173) of these cases had an Oncotype DX recurrence score<18 (LR=2.22, P<0.005). The average of the average modified Magee recurrence score, NS, ER, PR, and Ki-67 values for these 129 cases (108 with available Ki-67) was 13.5, 5.0, 258.8, 236.4, and 9.5, respectively. The average of the average modified Magee recurrence score, NS, ER, PR, and Ki-67 values for the 44 cases with an Oncotype DX recurrence score≥18 (35 with an available Ki-67) was 14.5, 5.4, 266.0, 214.2, and 11.4, respectively.
For cases with an available Ki-67, 100% (n=5) of cases with an average modified Magee recurrence score<9 had an Oncotype DX recurrence score<18 (P=0.05). All of these cases had Ki-67 values<10%. Eighteen cases had at least one modified Magee recurrence score<9. 89% (16/18) of these cases had an Oncotype DX recurrence score<18 (LR=6.06, P< 0.005). 86% (38/44) of cases with an average modified Magee recurrence score≤12 had an Oncotype DX recurrence score<18 (LR=4.80, P< 0.005). The six cases with an average modified Magee recurrence score≤12 and an Oncotype DX recurrence score≥18 are detailed in Table 3. Of the cases with an average modified Magee recurrence score≤12 and an available Ki-67 (n=35), all had Ki-67 values≤15%.
Cases with an Average Modified Magee Recurrence Score>30
100% (n=8) of cases that had an average modified Magee recurrence score>30 had an Oncotype DX recurrence score>30. The histologic characteristics of these eight cases are detailed in the Supplementary Appendix (Supplementary Table 5). Eleven cases had at least one modified Magee recurrence score>30. 82% (9/11) of these cases had an Oncotype DX recurrence score>30 (LR=129.7 P<0.0001). The two outlier cases had Oncotype DX recurrence scores of 29 and 22. Eight cases had an average modified Magee recurrence score≤30 with an Oncotype DX recurrence score>30 (Supplementary Appendix, Supplementary Table 6).
Cost Analysis
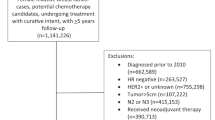
The estimated cost of sending our 283 cases out for Oncotype DX testing, based on the current list price of $4,350.00, would be $1,231,050.00. 100% of cases with an average modified Magee recurrence score>30 (n=8), and 100% of cases with an average modified Magee recurrence score<9 and an available Ki-67 (n=5), would have been correctly predicted to have a high (>30) or low (<18) Oncotype DX recurrence score, respectively. These 13 cases would represent a more conservative approach (100% concordance in our population) in eliminating high and low risk cases from Oncotype DX testing. 86% of cases with an average modified Magee recurrence score≤12 (38/44) would have been correctly predicted to have a low Oncotype DX recurrence score. The six outlier cases have been previously discussed (Table 3). 89% (34/38) of tumors with a NS<6, an ER and PR≥150, and a Ki-67<10% would have been correctly predicted to have a low Oncotype DX recurrence score. The four outlier cases have been previously discussed (Table 3, fourth outlier case Oncotype DX recurrence score of 18). Twenty-five of these 38 cases had an average modified Magee recurrence score≤12. 92% (12/13) of cases with an NS<6, an ER and PR≥150, and a Ki-67<10%, but with an average modified Magee recurrence score>12, would have been correctly predicted to have a low Oncotype DX recurrence score. The single outlier case has been previously discussed (Oncotype DX recurrence score of 18). The 8 cases with an average modified Magee recurrence score>30, the 44 cases with an average modified Magee recurrence score≤12, and the 13 cases with an average modified Magee recurrence score>12, a NS<6, ER and PR≥150, and a Ki-67<10% (total n=65) would represent a less conservative approach (89% (58/65) concordance in our population) in eliminating high and low risk cases from Oncotype DX testing. Table 4 details the specificity, sensitivity, positive predictive value, and negative predictive value for cases with either (1) an average modified Magee recurrence score<9, (2) an average modified Magee recurrence score≤12, (3) an ER and PR≥150 with a Ki-67<10%, or (4) an average modified Magee recurrence score>30. Figure 2 illustrates an algorithmic approach for sending these cases for Oncotype DX testing. Using the more and less conservative approaches to eliminate high and low risk cases from Oncotype DX testing, between 5% (13/283) and 23% (65/283) of cases would potentially not have been sent out by our institution for Oncotype DX testing, creating a potential cost savings between $56,550.00 and $282,750.00, respectively.
Discussion
Although the Oncotype DX test has gained widespread acceptance, cost has been an impediment to its adoption in many centers throughout the United States, and internationally. Clark et al,17 Zbytek et al,18 Kraus et al,19 Cuzick et al,20 and Biroschak et al21 all reported that the Oncotype DX recurrence score relies heavily on parameters already available from routine pathologic examination. Lee and Shen22 reported that patients with strongly ER-positive tumors will have a low or intermediate recurrence score, and that the clinical utility of the Oncotype DX assay in these patients is limited. Williams et al23 reported that the expression of Ki-67 by immunohistochemistry is significantly correlated with recurrence score, and Sahebjam et al24 found that the likelihood of a tumor with a Ki-67≥25% having a high or intermediate Oncotype DX recurrence score is >90%. Auerbach and colleagues25 reported that a mitotic count greater than 1 combined with a negative PR result could serve as a marker for an intermediate or high Oncotype DX recurrence score. Allison et al26 reported that high grade breast cancers with low to absent PR expression (Allred<5) and a Ki-67>10% were more likely to have a high recurrence score, and that grade 1 breast cancers with strong PR expression (Allred score≥5) and a Ki-67≤10% were more likely to have a low recurrence score. Tang et al27 concluded that PR negativity, luminal B subtype, tubal formation, and mitosis are strongly correlated with a higher recurrence score, and published a linear regression equation using these histopathologic variables to predict the Oncotype DX recurrence score. Flanagan et al15 also used linear regression analysis to propose a model equation (the original Magee equation) which showed that nuclear grade and mitotic count, in combination with semiquantitative ER, PR, and HER-2, can provide information that is remarkably similar to that found in the Oncotype DX recurrence score. Building from the Flanagan et al15 study, Klein et al16 again used linear regression analyses to create three new model equations, each using different combinations of either the NS, Ki-67, or tumor size, in addition to semiquantitative ER, PR, and HER-2. These equations, labeled as the ‘new Magee equations’, were reported to predict the actual Oncotype DX recurrence score for a given patient with a high degree of accuracy, particularly for patients with a low or high risk recurrence score.
Our findings support that the use of these new Magee equations, with a modification of the H-score (the modified Magee equations), in combination with standard histopathologic and immunohistochemical variables, may constitute a less expensive alternative to Oncotype DX testing, particularly for women found to have a predicted high or low risk Oncotype DX recurrence score. Cases with higher Oncotype DX recurrence scores typically had a higher average modified Magee recurrence score, NS, and Ki-67, with lower ER and PR. Cases with lower Oncotype DX recurrence scores typically had a lower average modified Magee recurrence score, NS, and Ki-67, with higher ER and PR. In our population, there were consistent significant differences (P<0.05) for NS, ER, PR, and Ki-67, between the Oncotype DX risk stratification categories (low, intermediate, and high), but not for HER-2 and tumor size. This suggests that a negative or equivocal HER-2 and tumor size may have less importance in risk stratification with Oncotype DX testing than NS, ER, PR, or Ki-67. The value of HER-2 with Oncotype DX testing has been questioned previously.29 The NS, PR, and Ki-67 values consistently showed greater statistical significance between risk stratification categories than the ER values, suggesting that these three values may have more importance in risk stratification than ER. These findings are supported in previous studies.22, 23, 24, 25, 26, 27 100% (n=8) of cases with an average modified Magee recurrence score>30 had an Oncotype DX recurrence score of>30. 100% (n=5) of cases with an average modified Magee recurrence score<9 and an available Ki-67 had an Oncotype DX recurrence score<18. All cases with an average modified Magee recurrence score<9 had a Ki-67<10%. 86% (38/44) of cases with an average modified Magee recurrence score≤12 had an Oncotype DX recurrence score of<18. All cases with an average modified Magee recurrence score≤12 were low grade with a Ki-67≤15%. The six cases with an average modified Magee recurrence score≤12 and an Oncotype DX recurrence score≥18 are all listed in Table 3. As the reader can see, these six cases generally have low to intermediate Oncotype DX recurrence scores, most of them 18–20, with relatively lower NS and Ki-67 values, and relatively higher ER and PR values. All have an Oncotype DX recurrence score≤25. 89% (34/38) of low grade tumors with an ER and PR≥150 and a Ki-67<10% had an Oncotype DX recurrence score of<18, and typically had an average modified Magee recurrence score≤12. Three of the four cases with an Oncotype DX recurrence score≥18 are also listed in Table 3. A fourth case had an Oncotype DX recurrence score of 18.
Joh et al30 concluded that breast oncology specialists tended to overestimate the risk of tumor recurrence compared with the Oncotype DX recurrence score; however, their study methods reflect most other studies that examine the correlation of histopathologic variables with the Oncotype DX recurrence score, in that specific quantitative criteria were not used. This was in part addressed by Allison et al,26 who have proposed an algorithm stratifying low grade and high grade cancers based on levels of PR expression and a Ki-67≤10% or>10%, respectively. Our data support the Allison et al study, and we propose more specific criteria with which ER-positive patients might be more likely to have a low or high Oncotype DX recurrence score. The algorithm in Figure 2 offers a stepwise approach using the average modified Magee recurrence score, along with histologic and immunohistochemical criteria, to consider cases which might possibly be excluded from Oncotype DX testing.
Several limitations in our study exist. The study set consisted of relatively recent archival cases, and there has not been sufficient time for clinical follow-up. Also, these cases were selected for Oncotype DX testing based on the clinical judgment of the medical oncologist, who would likely be biased toward patients with an indeterminate clinical risk assessment. Supporting this view is the low number of cases with a high recurrence score, which likely reflects the fact that patients who were judged to be at high recurrence risk based on standard histopathologic and clinical criterion were recommended for treatment with chemotherapy, and an Oncotype DX was not requested. As such, our study population might not be considered representative of the general breast cancer population. Nevertheless, our study is in agreement with Klein et al,16 in that the use of the Magee equations can help to accurately stratify breast cancer patients into subgroups where the calculated recurrence score would be likely concordant with its paired Oncotype DX recurrence score. Study of the prognostic significance of the calculated recurrence score in the general breast cancer population, with clinical follow-up, is needed and is currently ongoing in our institution.
A second limitation is that we had a number of cases that did not have an available Ki-67 (n=42), and we used the modified Magee recurrence score #2 (which does not require a Ki-67) as a surrogate for the average modified Magee recurrence score in these cases. Knowledge of the Ki-67 may have decreased the specificity of an algorithm which considered the average modified Magee recurrence score alone. Assuming theoretical Ki-67 values of≥90% (an unlikely scenario) in the 42 cases without an available Ki-67, five cases with a modified Magee recurrence score #2<30, would have had an actual (not surrogate) average modified Magee recurrence score>30. Only one of these five cases had an Oncotype DX recurrence score that was >30. The other four cases might have been recommended for exclusion from Oncotype DX testing (and possibly considered for treatment), based on the average modified Magee recurrence score alone. For cases with an available Ki-67, there was one case with a modified Magee recurrence score #2>30 and an Oncotype DX recurrence score <30. This case might have been recommended for exclusion from Oncotype DX testing (and possibly considered for treatment), based on the average modified Magee recurrence score alone, if there had been no Ki-67 available (i.e., using a surrogate average modified Magee recurrence score). There were 4/42 cases without an available Ki-67 that had a modified Magee recurrence score #2<9. Three of these cases had an Oncotype DX recurrence score of <18, and would have supported an algorithm considering the average modified Magee recurrence score alone, given any Ki-67 value; however, assuming a theoretical Ki-67 value of ≤8%, the fourth case, which had an intermediate Oncotype DX recurrence score of 20, might have been recommended for exclusion from Oncotype DX testing (and possibly not considered for treatment), based on the average modified Magee recurrence score alone. For cases with an available Ki-67, there was one case with a modified Magee recurrence score #2<9 and an intermediate Oncotype DX recurrence score (19), which might have been recommended for exclusion from Oncotype DX testing (and possibly not considered for treatment), based on the average modified Magee recurrence score alone, if there had been no Ki-67 available (i.e., using a surrogate average modified Magee recurrence score).
All of our cases with an available Ki-67 that had an average modified Magee recurrence score<9 (n=5) also had a modified Magee recurrence score #1<9, a modified Magee recurrence score #2<7.0, and a Ki-67 value<10%. Of note, no case had a modified Magee recurrence score #3<9. All of our cases that had an average modified Magee recurrence score >30 (n=8), also had at least two other modified Magee recurrence scores >30, and/or a modified Magee recurrence score #2 that was >30. We recommend that in addition to the average modified Magee recurrence score, the Ki-67 be should be available, and at least two other modified Magee recurrence scores should be considered, with one being a modified Magee recurrence score #2, when considering excluding cases from Oncotype DX testing (Figure 2).
Another potential concern is the lack of reproducibility and reliability in the use of immunohistochemistry for applications. Differences in immunohistochemistry values may occur as a result of variability in a variety of factors including tissue handling,31, 32 tissue fixation, reagents protocols, staining protocols, and pathologist interpretation.32 In light of these concerns, several quality assurance programs have been created including ad hoc consensus conference recommendations,33, 34 and the guideline recommendations from the American Society of Clinical Oncology/College of American Pathologist for HER-2, ER, and PR testing,35, 36 which includes mandatory proficiency testing. These national efforts have led to marked improvements in the quality, reliability, and inter-laboratory agreement for these breast cancer assays,37, 38, 39, 40, 41 and have made the use of semiquantitative immunohistochemistry results more feasible for estimating risk. These efforts in improving quality may be most helpful in reconsidering the role of Ki-67 as part of the routine panel for testing of breast cancers. Routine testing of breast cancers for Ki-67 expression is not currently recommended by either the American Society of Clinical Oncology or the National Comprehensive Cancer Network.42, 43 Our data support other studies22, 23, 24, 26, 27 which suggest that Ki-67 is critical in the assessment of risk stratification for patients with ER-positive breast cancer patients who are being considered for systemic chemotherapy.
The cost of the Oncotype DX test has been quoted anywhere from $3,460.00 to $4,400.00, with the current list price recently increased from $4,175.00 to $4,350.00.44 Consideration of a cost-effective approach in deciding which patients should be sent for Oncotype DX testing cannot be overlooked in this era of cost-conscious health care. In the Genomic Health 2012 Annual Report,44 the Letter to Stockholders reported a ‘12% increase compared to 2011’, with ‘total revenue increased by 14%, rising to $235,000,000 compared with the previous year.’ In that same report, ‘for the year ended December 31, 2012, more than 74,520 Oncotype DX test reports were delivered for use for treatment planning,’ and approximately 85% of revenue from Oncotype DX testing was reported to come from invasive breast carcinoma testing. If we considered that approximately 85% of the 74,520 reported 2012 Oncotype DX test reports were invasive breast cancer cases, then 63,342 Oncotype DX test reports were generated for invasive breast cancer cases. The Oncotype DX risk stratification of these cases is unknown; however, we might envision a reasonable cost-containment scenario. Depending on the pathologist in the Paik et al12 study, between 107 (16%) and 224 (34%) of cases were considered ‘low grade’ tumors. In our study, we had 141 (50%) low grade tumors. Considering only low grade tumors, 6/141 (5%) in our population had an average modified Magee recurrence score <9 which would have satisfied our algorithmic criteria for exclusion from Oncotype DX testing. If we considered the most conservative scenario in which approximately 16% (based on the Paik et al12 study) of the suspected 63,342 invasive breast tumors sent to Genomic Health for Oncotype DX testing in 2012 were low grade (n=10,135), and that 5% (based on our data) of these tumors (n=460) had an average modified Magee recurrence score <9 which satisfied the algorithmic criteria, the estimated cost savings to the health-care system from not sending these tumors for Oncotype DX testing (based on the current list price) would be approximately $2,001,000.00. If we also were able to exclude subsets of cases satisfying our algorithmic criteria that either had an average modified Magee recurrence score >30, an average modified Magee recurrence score ≤12, and/or a NS<6 with an ER/PR≥150 and a Ki-67<10%, the cost savings would undoubtedly be substantially higher.
Analysis of the data from the B20 clinical trial13 and Oncotype DX results suggested that the benefit from the addition of chemotherapy was only significant for the group of patients with a recurrence score of >25, whereas the confidence intervals for the risk of relapse showed complete overlap in the 11–25 recurrence score range.45 In the Trial Assigning Individualized Option for Treatment (TAILORx), the recurrence score ranges used for enrollment were changed from the original definitions, such that patients with a recurrence score of >25 were to receive chemotherapy, and those in the 11–25 range would be randomized, in an attempt to minimize the potential for under treatment in both the high risk group and the randomized group.45 The results of this study have not been published yet. In our population, 100% of tumors with an average modified Magee recurrence score ≤12 (n=44) or a NS<6 with an ER of≥150, PR≥60, and Ki-67<20% (n=75) had an Oncotype DX recurrence score of ≤25. 98% (113/115) of all cases with an ER of≥150, PR≥150, and Ki-67<25% had an Oncotype DX recurrence score of ≤25. 99% (134/136) of all cases with an ER and PR≥30, and a Ki-67<20% had an Oncotype DX recurrence score ≤25. The two outlier cases were the same in both groups, with Oncotype DX recurrence scores of 26 and 28, and an average modified Magee recurrence score, NS, ER, PR, Ki-67, Her-2, and tumor size of 14.6, 7, 285, 240, 5, 0, and 1.5 and 12.5, 6, 285, 270, 5, 1, and 1.5, respectively. We look forward to the results of the TAILORx study.
Examination of the available data provided in the Paik et al12 study shows that there were several patients in the low to intermediate histologic grade category with higher Oncotype DX recurrence scores, similar to our two outlier cases above. Although it is reasonable to consider that higher Oncotype DX recurrence scores in the patients with low to intermediate histologic grade tumors in the Paik et al study were at least in part due to lower ER and/or PR values, or a mitotically active tumor, the possibility that the tumor microenvironment contributed to a higher Oncotype DX recurrence score should also be considered. Acs et al and others26, 46 have suggested that a mitotically active cellular stroma, or tumor-associated inflammatory cells, may contribute to a higher Oncotype DX recurrence score. We are currently investigating this concept of the tumor microenvironment and its influence on the Oncotype DX recurrence score in our own data, and we plan to report our results in a future publication.
Oncotype DX testing is supported by both the American Society of Clinical Oncology and the National Comprehensive Cancer Network for guiding management in breast cancer patients with node-negative, ER-positive disease,42, 43 and is clearly recognized as a valuable test in the literature.30, 47, 48, 49 However, the widespread use of this test has come into question recently, as the literature has suggested that certain cases might be risk stratified more cost-effectively using histopathologic variables.50, 51, 52, 53, 54 Our data support this. The Magee equations, along with histologic and immunohistochemical criteria, may be a more cost-effective alternative in identifying cases that would likely stratify into a high or low Oncotype DX risk-stratification category. The information needed is already generated by many pathology laboratories during the initial assessment of primary breast cancer. The equations are user-friendly and publicly available free of any cost. All three equations can be accessed on the University of Pittsburgh Medical Center Department of Pathology website: (http://path.upmc.edu/onlineTools/mageeEquations.html). The modified Magee equations provide an alternative to the original Magee equations for pathology laboratories that do not use the H-score to determine ER and PR intensity.
It is important to emphasize that the use of these equations is heavily dependent on accurate histology grading and high quality ER, PR, HER-2, and Ki-67 immunohistochemical results. In cases where Oncotype DX testing is done, the Magee recurrence score should not be dramatically different from the Oncotype DX recurrence score. If there is a significant difference, this should be thoroughly investigated before decisions on adjuvant therapy are made. Additional studies to further validate the suggested algorithm are needed.
References
Siegel R, Ma J, Zou Z et al. Cancer Statistics, 2014. CA Cancer J Clin 2014;64:9–29.
Hassett MJ, Hughes ME, Niland JC et al. Chemotherapy use for hormone receptor-positive, lymph node-negative breast cancer. J Clin Oncol 2008;26:5553–5560.
Jan P, Baak A, Gudlaugsson E et al. Proliferation is the strongest prognosticator in node-negative breast cancer: significance, error sources, alternative and comparison with molecular prognostic markers. Breast Cancer Res Treat 2009;115:241–254.
Koscielny S, Tubiana M, Le MG et al. Breast cancer: relationship between the size of the primary tumour and the probability of metastatic dissemination. Br J Cancer 1984;49:709–715.
Elston CW, Ellis IO . Pathological prognostic factors in breast cancer. I, the value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 1991;19:403–410.
Fisher B, Bauer M, Wickerham DL et al. Relation of the number of positive axillary nodes to the prognosis of patients with primary breast cancer. An NSABP update. Cancer 1983;52:1551–1557.
Colditz GA, Rosner BA, Chen WY et al. Risk factors for breast cancer according to estrogen and progesterone receptor status. J Natl Cancer Inst 2004;96:218–228.
Hicks DG, Kulkarni S . Trastuzumab as adjuvant therapy for early breast cancer: the importance of accurate human epidermal growth factor receptor 2 testing. Arch Pathol Lab Med 2008;132:1008–1015.
Viale G . Pathologic work up of the primary tumor: getting the proper information out of it. The Breast 2011;20:S82–S86.
Allison KH . Molecular pathology of breast cancer: what a pathologist needs to know. Am J Clin Pathol 2012;138:770–780.
Simpson PT, Reis-Filho JS, Gale T et al. Molecular evolution of breast cancer. J Pathol 2005;205:248–254.
Paik S, Shak S, Tang G et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. New Engl J Med 2004;351:2817–2826.
Paik S, Tang G, Shak S et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Onc 2006;24:3726–3734.
Ishibe N, Schully S, Freedman A et al. Use of Oncotype DX in Women with node-positive breast cancer. PLoS Curr 2011;3:RRN1249.
Flanagan MB, Dabbs DJ, Brufsky AM et al. Histopathologic variables predict Oncotype DX recurrence score. Mod Pathol 2008;21:1255–1261.
Klein ME, Dabbs DJ, Shuai Y et al. Prediction of the Oncotype DX recurrence score: use of pathology-generated equations derived by linear regression analysis. Mod Pathol 2013;26:658–664.
Clark BZ, Dabbs DJ, Cooper KL et al. Impact of progesterone receptor semiquantitative immunohistochemical result on Oncotype DX recurrence score: A quality assurance study of 1074 cases. Appl Immunohistochem Mol Morphol 2013;21:287–291.
Zbytek B, Cohen C, Wang J et al. Nottingham-defined mitotic score: comparison with visual and image cytometric phosphohistone H3 labeling indices and correlation with Oncotype DX recurrence score. Appl Immunohistochem Mol Morphol 2013;21:48–53.
Kraus JA, Dabbs DJ, Beriwal S et al. Semi-quantitative immunohistochemical assay versus Oncotype DX qRT-PCR assay for estrogen and progesterone receptors: an independent quality assurance study. Mod Pathol 2012;25:869–876.
Cuzick J, Dowsett M, Pineda S et al. Prognostic value of a combined estrogen receptor, progesterone receptor, Ki-67, and human epidermal growth factor receptor 2 immunohistochemical score and comparison with the Genomic Health recurrence score in early breast cancer. J Clin Oncol 2011;29:4273–4278.
Biroschak JR, Schwartz GF, Palazzo JP et al. Impact of Oncotype DX on treatment decisions in ER-positive, node-negative breast cancer with histologic correlation. Breast J 2013;19:269–275.
Lee JJ, Shen J . Is the Oncotype DX assay necessary in strongly estrogen receptor-positive breast cancers? Am Surg 2011;77:1364–1367.
Williams DJ, Cohen C, Darrow M et al. Proliferation (Ki-67 and phosphohistone H3) and Oncotype DX recurrence score in estrogen receptor-positive breast cancer. Appl Immunohistochem Mol Morphol 2011;19:431–436.
Sahebjam S, Aloyz R, Pilavdzic D et al. Ki 67 is a major, but not the sole determinant of Oncotype DX recurrence score. Br J Cancer 2011;105:1342–1345.
Auerbach J, Kim M, Fineberg S . Can features evaluated in the routine pathologic assessment of lymph node-negative estrogen receptor-positive stage I or II invasive breast cancer be used to predict the Oncotype DX recurrence score? Arch Pathol Lab Med 2010;134:1697–1701.
Allison KH, Kandalaft PL, Sitlani CM et al. Routine pathologic parameters can predict Oncotype DX recurrence scores in subsets of ER positive patients: who does not always need testing? Breast Cancer Res Treat 2012;131:413–424.
Tang P, Wang J, Hicks DG et al. A lower Allred score for progesterone receptor is strongly associated with a higher recurrence score of 21-gene assay in breast cancer. Cancer Invest 2010;28:978–982.
Cronin M, Sangli C, Liu ML et al. Analytical validation of the Oncotype DX genomic diagnostic test for recurrence prognosis and therapeutic response prediction in node-negative, estrogen receptor-positive breast cancer. Clin Chem 2007;53:1084–1091.
Dabbs DJ, Klein ME, Mohsin SK et al. High false-negative rate of HER2 quantitative reverse transcription polymerase chain reaction of the Oncotype DX test: An independent quality assurance study. J Clin Oncol 2011;29:4279–4285.
Joh JE, Esposito NN, Kiluk JV et al. The effect of Oncotype DX recurrence score on treatment recommendations for patients with estrogen receptor-positive early stage breast cancer and correlation with estimation of recurrence risk by breast cancer specialists. The Oncologist 2011;16:1520–1526.
Hicks DG, Boyce BF . The challenge and importance of standardizing pre-analytical variables in surgical pathology specimens for clinical care and translational research. Biotech Histochem 2012;87:14–17.
Neumeister VM, Anagnostou V, Siddiqui S et al. Quantitative assessment of effect of preanalytic cold ischemic time on protein expression in breast cancer tissues. J Natl Cancer Inst 2012;104:1815–1824.
Goldstein NS, Hewitt SM, Taylor CR et al. Recommendations for improved standardization of immunohistochemistry. Appl Immunohistochem Mol Morphol 2007;15:124–133.
Yaziji H, Taylor CR, Goldstein NS et al. Consensus recommendations on estrogen receptor testing in breast cancer by immunohistochemistry. Appl Immunohistochem Mol Morphol 2008;16:513–520.
Hammond ME, Hayes DF, Dowsett M et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer (unabridged version). Arch Pathol Lab Med 2010;134:e48–e72.
Wolff AC, Hammond ME, Schwartz JN et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. Arch Pathol Lab Med 2007;131:18–43.
Cohen DA, Dabbs DJ, Cooper KL et al. Interobserver agreement among pathologists for semiquantitative hormone receptor scoring in breast carcinoma. Am J Clin Pathol 2012;138:796–802.
Vergara-Lluri ME, Moatamed NA, Hong E et al. High concordance between HercepTest immunohistochemistry and ERBB2 fluorescence in situ hybridization before and after implementation of American Society of Clinical Oncology/College of American Pathology 2007 guidelines. Mod Pathol 2012;25:1326–1332.
Yildiz-Aktas IZ, Dabbs DJ, Bhargava R . The effect of cold ischemic time on the immunohistochemical evaluation of estrogen receptor, progesterone receptor, and HER2 expression in invasive breast carcinoma. Mod Pathol 2012;25:1098–1105.
Middleton LP, Price KM, Puig P et al. Implementation of American Society of Clinical Oncology/College of American Pathologists HER2 Guideline Recommendations in a tertiary care facility increases HER2 immunohistochemistry and fluorescence in situ hybridization concordance and decreases the number of inconclusive cases. Arch Pathol Lab Med 2009;133:775–780.
Brunelli M, Manfrin E, Martignoni G et al. HER-2/neu assessment in breast cancer using the original FDA and new ASCO/CAP guideline recommendations: impact on selecting patients for herceptin therapy. Am J Clin Pathol 2008;129:907–911.
Fitzgibbons PL, Dillon DA, Alsabeh R et al. Template for reporting results of biomarker testing specimens from patients with carcinoma of the breast. version: Breast Biomarkers 1.1.0.0. College of American Pathologists, 2014. Available from http://www.cap.org/cancerprotocols. (Accessed 6 April 2014).
Harris L, Fritsche H, Mennel R et al. American Society of Clinical Oncology 2007 update of recommendations for the use of tumor markers in breast cancer. J Clin Oncol 2007;25:5287–5312.
Genomic Health Annual Report 2012.
Sparano JA, Paik S . Development of the 21-gene assay and its application in clinical practice and clinical trials. J Clin Oncol 2008;26:721–728.
Acs G, Esposito NN, Kiluk J et al. A mitotically active, cellular tumor stroma and/or inflammatory cells associated with tumor cells may contribute to intermediate or high Oncotype DX recurrence score in low-grade invasive breast carcinomas. Mod Pathol 2012;25:556–566.
Rouzier R, Pronzato P, Chéreau E et al. Multigene assays and molecular markers in breast cancer: systematic review of health economic analyses. Breast Cancer Res Treat 2013;139:621–637.
Vataire AL, Laas E, Aballéa S et al. Cost-effetiveness of a chemotherapy predictive test. Bull Cancer 2012;99:907–914.
Blohmer JU, Rezai M, Kümmel S et al. Using the 21-gene assay to guide adjuvant chemotherapy decision-making in early-stage breast cancer: a cost-effectiveness evaluation in the German setting. J Med Econ 2013;16:30–40.
Carlson JJ, Roth JA . The impact of the Oncotype DX breast cancer assay in clinical practice: a systematic review and meta-analysis. Breast Cancer Res Treat 2013;141:13–22.
Kelly CM, Krishnamurthy S, Bianchni G et al. Utility of Oncotype DX risk estimates in clinically intermediate risk hormone receptor-positive, Her-2-normal, grade II, lymph node-negative breast cancers. Cancer 2010;116:5161–5167.
Brufsky A . Precision Oncology in breast cancer: better than ever, or less than before. Breast J 2013;19:355–356.
Milburn M, Rosman M, Mylander C et al. Is Oncotype DX recurrence score (RS) of prognostic value once Her2-positive and low-ER expression patients are removed? Breast J 2013;19:357–364.
Schmidt M, Untch M . Prediction of benefit from chemotherapy in ER-positive/Her-2 negative breast cancer- a problem still to be solved. Ann Oncol 2014;25:754.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Modern Pathology website
Rights and permissions
About this article
Cite this article
Turner, B., Skinner, K., Tang, P. et al. Use of modified Magee equations and histologic criteria to predict the Oncotype DX recurrence score. Mod Pathol 28, 921–931 (2015). https://doi.org/10.1038/modpathol.2015.50
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2015.50
This article is cited by
-
Adjuvant chemotherapy for pT1-3N0-1 breast cancer patients with HR+, HER2− subtype: a propensity-score matched study with competing risk analysis
Journal of Cancer Research and Clinical Oncology (2023)
-
Differential distribution of actual and surrogate oncotype DX recurrence scores in breast cancer patients by age, menopausal status, race, and body mass index
Breast Cancer Research and Treatment (2023)
-
Use of a supervised machine learning model to predict Oncotype DX risk category in node-positive patients older than 50 years of age
Breast Cancer Research and Treatment (2022)
-
Concordance between results of inexpensive statistical models and multigene signatures in patients with ER+/HER2− early breast cancer
Modern Pathology (2021)
-
Prediction of Oncotype DX recurrence score using deep multi-layer perceptrons in estrogen receptor-positive, HER2-negative breast cancer
Breast Cancer (2020)