Abstract
Stratification of recurrence risk is a cornerstone of early breast cancer diagnosis that informs a patient’s optimal treatment pathway. Several tools exist that combine clinicopathological and molecular information, including multigene assays, which can estimate risk of recurrence and quantify the potential benefit of different adjuvant treatment modalities. While the tools endorsed by treatment guidelines are supported by level I and II evidence and provide similar prognostic accuracy at the population level, they can yield discordant risk prediction at the individual patient level. This review examines the evidence for these tools in clinical practice and offers a perspective of potential future risk stratification strategies. Experience from clinical trials with cyclin D kinase 4/6 (CDK4/6) inhibitors in the setting of hormone receptor–positive (HR+)/human epidermal growth factor receptor 2-negative (HER2-) early breast cancer is provided as an illustrative example of risk stratification.
Similar content being viewed by others
Introduction
Overall, approximately 12–15% of people with stage I–III HR+ breast cancer will experience metastatic recurrence1. However, risk is not distributed evenly across clinical stage, and in addition to tumor size and nodal status, several other variables influence prognosis and several of these (e.g., histologic grade, the Oncotype DX® 21-gene recurrence score) are now incorporated into the 8th edition of the American Joint Committee on Cancer (AJCC) staging guidelines2. Accurate prediction of the absolute risk of local or distant recurrence that a patient faces after locoregional therapy is important for judging the risk-benefit ratio of systemic therapies. One of the challenges inherent with managing HR+ early breast cancer—and HR+/HER2- cancer in particular—is the persistent risk of recurrence that extends over decades, with as much as 50% of recurrences occurring more than 5 years after diagnosis3. Indeed, late recurrence (i.e., after 5 years of follow-up) risk prediction tools are emerging that are increasingly used to assist decision-making about extended adjuvant endocrine therapy (ET)4.
Breast tumors are highly heterogeneous with differences in morphology and molecular features, and many known and unknown factors influence the likelihood of response to treatment and risk of recurrence3,5. Multigene molecular tests capture some of these molecular features (most consistently proliferation and estrogen receptor [ER] signaling) and integrate them into a single risk score6,7,8,9,10. These assays can provide an estimate of the probability of recurrence as well as assign a risk category (low, high, intermediate); however, the most accurate risk prediction requires integration of tumor size, nodal status, grade, and patient age/menopausal status with the multigene risk scores11. Lymphovascular invasion is an additional prognostic factor that has significant negative impact on survival in N0 disease12. Since each multigene assay uses different sets of genes and weighs components differently, the individual patient level risk predictions can be discordant, particularly for patients who are in the intermediate-risk category3,13. In a direct comparison of several assays, including the Oncotype DX 21-gene recurrence score, MammaPrint, and PAM50 risk of recurrence score (Prosigna®), in the OPTIMA prelim trial, fewer than 40% of tumors were classified similarly by all tests13. Similarly, a review comparing risk classifications of the Oncotype DX 21-gene recurrence score, Breast Cancer Index, EndoPredict, MammaPrint, and Prosigna assays demonstrated distribution discrepancies among risk groups14.
This review examines the currently available clinical and transcriptomic tools for risk stratification, current evidence to support their use in different patient populations, and the extent to which they can inform treatment decisions. We will conclude by briefly discussing the future of risk stratification and generation of predictive tools to guide treatment decisions.
Results
Clinicopathologic risk assessment
Following diagnosis of breast cancer, histopathologic and molecular assessment have long been the cornerstones of risk stratification15. The AJCC guidelines recommend anatomic staging based on tumor size, and the existence of lymphadenopathy and distant metastases, histological tumor grade, and expression of ER, progesterone receptor (PR), HER2, and Ki-6716. Currently, PREDICT is one of the most widely available clinically validated prognostic risk assessment tools that uses information from routinely available clinical and pathologic variables (https://breast.predict.nhs.uk/tool)17,18. Clinical Treatment Score post-5 years (CTS5) is another commonly used tool; it was specifically developed to predict risk of recurrence between years 5 and 10 for women with ER+ breast cancer who are recurrence-free 5 years after ET. The CTS5 calculator is freely available online at https://www.cts5-calculator.com and combines information from tumor size, grade, age, and number of nodes involved19. Ki-67-related antigen is a clinicopathologic marker of cellular proliferation that can be detected using immunohistochemistry20. Its expression has been associated with breast cancer prognosis, including in early breast cancer20,21,22. Ki-67 is predictive of response to neoadjuvant ET23,24. Furthermore, suppression of Ki-67 expression in the setting of preoperative ET is prognostic for recurrence-free survival23,25. However, until recently, Ki-67 has not been included in routine clinical decision-making as its relevance to known targets has been unclear and hindered by concerns such as inter-laboratory variability and lack of cut-off consensus26,27. Another commonly used prognostic index is the preoperative endocrine prognostic index (PEPI) which utilizes pathological tumor size, node status, Ki-67 labeling index, and ER status following neoadjuvant therapy28. Unfortunately, classification based on clinicopathologic assessment alone may not sufficiently capture a patient’s prognosis, especially for cases where decisions are challenging3,29. More recently, gene expression profiling (including genomic subtypes luminal A, luminal B, luminal HER2, HER2-enriched, basal-like, and triple negative), as well as multigene panels have allowed for more nuanced prognostic profiling16.
Transcriptomic risk stratification tools
There are a number of commercially available and clinically validated transcriptomic risk stratification tools, each of which assesses a different suite of genes to generate a prognostic score (Table 1).
Oncotype DX
The most widely recommended genomic test is Oncotype DX Breast Recurrence Score® Test, often referred to as the 21-gene recurrence score assay. Oncotype DX uses gene expression data to calculate a recurrence score (RS) from 0 to 100 and provides a percent risk of distant recurrence over the next 9 years with ET alone and estimates the predicted benefit from adjuvant chemotherapy30,31. Estimates are adjusted for nodal status (positive vs. negative) and the company provides a free web tool (RSClin: https://online.genomichealth.com), which integrates RS with tumor size and grade to improve prognostic accuracy32. RSClin integrates the 21-gene RS with tumor grade, tumor size, and age. It was developed using data from a patient-specific meta-analysis of 10,004 women with HR + /HER2-, node-negative breast cancer. This database included 577 women from the NSABP B-14 study who received ET alone33, 4854 from TAILORx who received ET alone, and 4573 who also received chemotherapy34. Oncotype DX has been prospectively validated for pre- and postmenopausal patients with HR + /HER2- node-negative, and node-positive (1–3 positive nodes) disease35.
Mammaprint
MammaPrint is a similar transcriptomic assay that was also validated in a prospective trial and in multiple prospectively designed retrospective studies. It uses information from 70 genes to assign a MammaPrint low- or high-risk category10,36. The prognostic accuracy of MammaPrint is best established in node-negative patients due to the relatively small number of patients with positive nodes who were included in prospective trials with this assay10,29,36,37. The 70-gene signature can identify patients with an ultra-low risk of distant recurrence. Of the 6693 patients enrolled in the MINDACT trial, profiling revealed an ultra–low-risk 70-gene signature in 1000 patients. After a median follow-up of 8.7 years, 8-year distant metastasis-free interval in these patients was 97.0% vs. 94.5% for patients with low-risk signature and 89.2% for patients with high-risk signature38.
Prosigna and endopredict®
Two transcriptomic assays, Prosigna and EndoPredict®, incorporate clinical information in addition to molecular measurements in the algorithm for generating a prognostic risk score8. Prosigna is based on the PAM50 assay, incorporating tumor size and an estimate of molecular class (e.g., basal-like, HER2-enriched, luminal A, luminal B) to separate patients into low-, intermediate-, and high-risk groups based on a score8. EndoPredict combines transcriptomic and clinical risk factors (e.g., nodal status and tumor size) to categorize patients into high or low risk of recurrence groups39. EndoPredict is validated for use in postmenopausal patients with node-positive or node-negative disease, but validation is lacking for premenopausal patients39,40.
Breast cancer index
The Breast Cancer Index (BCI) risk of recurrence and extended endocrine benefit test is another multigene assay endorsed by guidelines for women with lymph node–negative or lymph node–positive disease29,41. The test provides a quantitative estimate of overall risk of recurrence over 10 years and a separate estimate for late distant recurrence (i.e., after 5 years)30,36. Uniquely, among all other transcriptomic assays, the BCI also provides a prediction of the likelihood of benefit from extended (greater than 5 years) adjuvant ET4. It has been validated in several prospectively designed retrospective studies, though not all validation studies have confirmed its predictive value for extended adjuvant ET benefit, due at least in part to a lack of statistical power4,42,43,44,45.
Role of risk stratification tools in informing treatment decisions for HR+/HER2- disease
RS group considerations
Some women with HR+/HER2- early breast cancer will gain substantial benefit from adjuvant (or neoadjuvant) chemotherapy, whereas many other patients can safely avoid chemotherapy. Over the past 15 years, important progress has been made in identifying the low-risk population who can safely forego adjuvant chemotherapy. Prior to the prospective analysis performed in the TAILORx study46, early work from the National Surgical Adjuvant Breast and Bowel Project (NSABP) B20 trial classified patients into low-, intermediate-, and high-risk groups based on Oncotype DX RS of <18, 18– < 31, and ≥ 31, respectively47. A retrospective analysis of the trial showed that patients with Oncotype DX RS of < 18 had excellent long-term outcomes and derived no apparent benefit from combination chemotherapy plus tamoxifen treatment vs. tamoxifen47. Similarly, patients with RS of 18–30 did not appear to receive substantial benefit from chemotherapy plus tamoxifen treatment vs. tamoxifen47. On the other hand, patients with RS ≥ 31 had a much higher absolute risk of recurrence and experienced a 27.6% decrease in absolute risk of distant recurrence with chemotherapy plus tamoxifen vs. tamoxifen47. Predictive potential has also been suggested for MammaPrint and for neoadjuvant ET for EndoPredict48,49. Additionally, a PEPI score of 0 after neoadjuvant ET is associated with a low risk of relapse without chemotherapy28. These findings, along with other smaller studies, led to treatment guidelines that do not recommend administration of chemotherapy for patients with very low-risk HR + /HER2- early breast cancer, and endorse use of adjuvant chemotherapy for the high-risk group29,41,50.
While the clinical benefits of chemotherapy have been established for patients with high risk of recurrence, until very recently it remained unclear whether those with intermediate-risk scores derive benefit from chemotherapy. Data from the TAILORx trial, consisting of 6907 node-negative patients who had an Oncotype DX RS of 11–25, showed that ET was noninferior to adjuvant chemotherapy plus ET for invasive disease-free survival (iDFS), freedom from local or distant recurrence, and overall survival (hazard ratio: 1.08, P = 0.26; hazard ratio: 1.11, P = 0.33; hazard ratio: 0.99, P = 0.89, respectively)7. An exploratory analysis of the TAILORx trial suggested that women younger than 50 years with an intermediate-risk score had higher risk of recurrence than older women and derived a significant survival benefit from chemotherapy. This effect was particularly apparent between RS 21 and 257. Whether this benefit is driven by the cytotoxic effect of the chemotherapy, or due to chemotherapy-induced amenorrhea, or both, remains unknown.
RS group and menopausal status considerations
While these results were generated from an unplanned exploratory analysis, they are nevertheless highly consistent with several other small and large studies that suggest higher risk and greater adjuvant chemotherapy benefit among younger HR+ patients51. For example, although underpowered, the exploratory analysis of the MINDACT study also indicated clinical benefit of chemotherapy for women aged less than 50 years at high clinical risk and low genomic risk52. The 8-year distant metastases-free survival (DMFS) with chemotherapy plus ET in women ≤ 50 years was 93.6% (95% CI: 89.3%–96.3%) compared with 88.6% (95% CI: 83.5%–92.3%) for ET alone52. Additionally, results from the RxPonder trial that included patients with 1–3 positive lymph nodes and RS ≤ 25 indicated no improvement of iDFS when adjuvant chemotherapy was added to ET for postmenopausal patients (hazard ratio: 0.97, P = 0.81)6. However, a substantial benefit was seen with the addition of adjuvant chemotherapy in premenopausal women (hazard ratio: 0.53, P < 0.001)6.
Challenges: Discordant results
Where tests are readily accessible, and more than one transcriptomic assay is performed on the same tissue, discordance between test results poses a challenge for clinical practice. The OPTIMA preliminary study used five different clinically validated tools (Oncotype DX, MammaPrint, Prosigna, IHC4, and IHC4-AQUA) to compare risk stratification for women aged ≥ 40 years with HR + /HER2- stage II–III breast cancer13. The study found substantial patient-level disagreement between the tests: overall, 60.6% of tumors were given different risk categories by at least one assay13. However, comparisons across tests are challenging because different tests use different thresholds to define high risk. Additionally, some assays provide only two risk categories (high vs. low), while others provide three categories (low, intermediate, high)6,7,8,9,10. The tests also use different genes to calculate risk; for example, while MammaPrint and Prosigna quantify 70 and 50 genes, respectively, only three of these are common between the two tests13.
Based on currently available data, it is not possible to determine whether one test is overall superior to others, or if one test is more suited to a particular patient population. For this reason, guidelines discourage use of multiple transcriptomic tests, and clinicians should avoid redundant testing, as instead of improved precision, it leads to greater confusion37.
Use of tests in resource-constrained settings
Despite the cost-effectiveness and international guideline support for using transcriptomic tests29,41,50,53, testing is not routinely available for all patients in different parts of the world. The St. Gallen International Consensus Guidelines recognize that while the use of transcriptomic assays is preferable for patients with intermediate risk, integration of traditional clinical factors (tumor grade, ER, PR, and HER2 status, and proliferation by Ki-67 assessment) can also be used to identify patients at low risk of recurrence to inform adjuvant chemotherapy treatment decisions when the more accurate and standardized transcriptomic assays are not available50.
Risk stratification in clinical trials: Lessons from adjuvant studies of CDK4/6 inhibitors
Preliminary studies have found that CDK4/6 inhibitors abemaciclib, palbociclib, and ribociclib significantly lower Ki-67 expression54,55,56. As a result, this class of drugs may have a role in treatment of highly proliferative tumors in the early breast cancer setting. Indeed, these agents have demonstrated significantly improved progression-free survival and improved overall survival for some patients in metastatic HR + /HER2- breast cancer54,57,58,59,60,61.
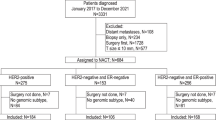
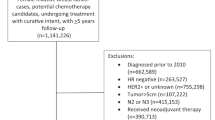
A number of phase 3 clinical trials investigating this class of drugs in the adjuvant setting have recently been completed or are ongoing (Table 2). Recent data from the monarchE, PALLAS, and PENELOPE-B trials show differing results for the use of CDK4/6 inhibitors for HR + /HER2- early breast cancer62,63,64. The monarchE trial was specifically designed to enroll a high-risk patient group based on number of positive lymph nodes, tumor size, grade, and Ki-67 expression64. In this trial (median follow-up of 27 months), abemaciclib in combination with ET demonstrated a statistically significant improvement in iDFS (2-year iDFS rate: 92.3%) in the intent-to-treat population compared to ET alone (2-year iDFS rate: 89.3%), with a 29% reduction in the risk of developing invasive disease (nominal P = 0.001)64. In patients with high Ki-67 of ≥ 20% (N = 2498), abemaciclib + ET demonstrated statistically significant improvement in iDFS at the primary outcome analysis (hazard ratio: 0.64, [95% CI: 0.48–0.87], P = 0.0042), and an absolute benefit of 7.1% in the 3-year iDFS rates (Fig. 1). Based on the efficacy results in cohort 1 patients with high Ki-67 scores at the additional follow-up analysis, the US Food and Drug Administration approved abemaciclib in combination with ET for patients with HR + /HER2-, node-positive, early breast cancer at high risk of recurrence and a Ki-67 score of ≥ 20%65; ASCO and NCCN have also updated their guidelines to include use of adjuvant abemaciclib plus ET in patients with ER + /HER2- early breast cancer and a Ki-67 score ≥ 20%32,64,66. In contrast, the PALLAS trial was stopped for futility at a pre-planned interim analysis, having shown no significant improvement in iDFS with adjuvant ET plus palbociclib vs. adjuvant ET alone67. At final analysis, the PENELOPE-B trial also showed no significant difference in iDFS for patients with residual disease who received adjuvant ET plus palbociclib compared with adjuvant ET alone at 4-year median follow-up; interestingly, the trial showed transient benefit in the initial 2–3 years, which was not seen with longer follow-up62. Notably the populations in PALLAS and PENELOPE-B did not use Ki-67 as an entry criterium as in the monarchE trial; indeed, only 25.5% of patients in the PALLAS trial had Ki-67 > 15%62. However, in a subgroup analysis, Ki-67 > 15% was not associated with an improved outcome relative to lower expression (Fig. 1)62. The use of the 15% threshold is further complicated by the fact that the clinical utility of Ki-67 at expression levels between 10 and 20% is limited in ER+/HER2- early breast cancer68.
The differences in outcome between the three trials is unexpected, as all CDK4/6 inhibitors in mBC have similar efficacy69. Potential explanations for the differences in outcome between the trials include different target populations, different baseline risk distribution (especially in terms of Ki-67 expression), different duration of treatment and follow-up, and potentially alleged differences in molecular mechanisms of action of the drugs (Table 2). Awaited data from the NATALEE trial are anticipated to provide more information on the potential adjuvant use of CDK4/6 inhibitors. Given that trial designs for monarchE, PALLAS, and PENELOPE-B pre-dated the era of transcriptome testing for risk stratification, the clinical utility of transcriptomic risk recurrence tools has not been clearly established with CDK4/6 inhibitors in early breast cancer with intermediate or high risk of recurrence; as such, focus directed toward ongoing trials of CDK4/6 inhibitors may shed light on the matter70,71,72.
Guideline recommendations
AJCC, the National Comprehensive Cancer Network (NCCN), American Society of Clinical Oncology (ASCO), European Society for Medical Oncology (ESMO), and St. Gallen treatment guidelines recommend the use of transcriptomic assays to provide additional information for anatomic, histologic, and molecular-based staging2,29,37,41,50. Some of these guidelines groups assign different levels of confidence to the specific tests they recommend (Table 3), noting that most of these tests were designed specifically for use in ER+ tumors.
The NCCN guidelines recommend considering transcriptomic testing for all patients with invasive ductal or lobular tumors greater than 0.5 cm in diameter and no lymph node involvement, and for patients with 1–3-node-positive disease who are candidates for adjuvant chemotherapy37. The St. Gallen International Consensus Guidelines also endorse the value of transcriptomic assays for determining whether to recommend chemotherapy in T1/T2 N0 tumors, T3 N0 tumors, and TxN1 (1–3 positive lymph nodes)50. ASCO and ESMO also make specific recommendations (Table 3).
Overall, the Oncotype DX RS has the largest body of evidence from prospective clinical trials to guide its use in the clinic and is the preferred assay according to the NCCN guidelines and AJCC staging (Table 3)37. NCCN gives the most detailed recommendations for translating Oncotype DX RS and other risk scores to clinical action. For node-negative premenopausal HR + /HER2- patients, NCCN guidelines indicate that there is no additional benefit to be gained from initiating chemotherapy with an Oncotype DX RS < 15, but recommend considering chemotherapy before ET, or ovarian suppression, for RS of 16–25, and addition of chemotherapy for RS ≥ 26. For patients with 1–3 positive lymph nodes, NCCN recommends addition of chemotherapy with a RS ≥ 26. For RS < 26, the recommendation to add chemotherapy depends on the menopausal status of the patient. ASCO has provided similar recommendations based on the results of TAILORx4,5,6,41.
Dicussion
The future of risk stratification
There are several emerging technologies that could potentially have a major impact on risk stratification in the not-too-distant future. Systemic recurrence in the absence of any detectable disease after surgical resection of the primary tumor by definition implies that a very small number of disseminated cancer cells survived adjuvant treatment and give rise to recurrence years later. Several methods have been developed to detect minimal residual disease (MRD). The presence of circulating tumor cells (CTCs) in blood in early breast cancer have been detected after surgery but before adjuvant chemotherapy in 21.5% of patients, but this was only associated with a modest reduction in DFS (hazard ratio: 2.1). Although a greater reduction in DFS was seen with patients who had > 5 CTCs detected (hazard ratio: 4.5), the population was small, accounting for only 3% of patients in the study. A stronger association was observed between presence of CTCs and risk of recurrence for patients with high-risk, HR+ disease at 5 years after diagnosis (hazard ratio: 13.1). However, CTC assays have low sensitivity and a risk of false-positive results and are not widely used in clinical practice73.
The major technological advance was the development of highly sensitive and specific circulating tumor DNA (ctDNA) assays, which can detect and quantify free tumor-derived DNA in plasma (see Coakley et al.73 for an in-depth discussion). The presence of ctDNA after completing treatment is associated with a very high risk of future relapse compared with absence of ctDNA (hazard ratio: 3.1–43.4 across a range of tumor types)73. In breast cancer, the presence of ctDNA after neoadjuvant therapy has been shown to be a good predictive marker of future relapse74,75,76. Regular ctDNA monitoring can also detect molecular relapse 8–11 months before clinical or radiological relapse is detectable73. In the metastatic setting, ctDNA has been shown to be more sensitive than CTC analysis to detect early progression and shows concordance with protein biomarkers such as CA27.2977,78. Results from metastatic breast cancer have found that ctDNA detection of variants of ESR1, TP53, and PIK3CA were predictive of poor overall survival, and may help to identify which patients may benefit from certain treatments79. For example, patients with PIK3CA mutations may benefit from treatment with PI3K inhibitors such as alpelisib79. Other potential roles of ctDNA may include monitoring treatment response and early detection of disease progression, detection of minimal residual disease, and obtaining information on the tumor when a biopsy is not feasible80,81.
These studies demonstrated technical robustness and clinical validity of ctDNA testing, but none of them have addressed its clinical utility, whether or not patient outcome improves because of ctDNA testing, or if ctDNA testing can help to optimize therapy. Several other important questions also remain unanswered, including the true prevalence of ctDNA positivity in different prognostic risk groups, the dynamics of ctDNA during follow-up in the absence of intervention, the proportion of patients who already have asymptomatic but detectable metastatic disease at the time of detecting ctDNA positivity, and most importantly, whether or not early therapeutic intervention at a molecular relapse state can improve clinical outcome (particularly overall survival). In addition, sampling time points and techniques have varied across studies conducted to date, indicating that standardization is required to inform routine clinical use of ctDNA sampling64.
Another new technological advance is the detection of mRNA. This approach has the potential to replace immunohistochemistry and in situ hybridization for evaluation of key biomarkers, including ER, PR, HER2, and Ki-6768. The recently developed STRAT4 assay is able to simultaneously detect expression of ESR1, PGR, ERBB2, and MKi67. This automated assay has the potential to eliminate the intra- and inter-observer variability inherent to immunohistochemistry and in situ hybridization.
Treatment guidelines recommend the use of gene expression tools to inform adjuvant chemotherapy selection for patients with early-stage HR+/HER2- breast cancers, with intermediate risk defined using clinical and histopathologic methods29,37,41,82,83,84. For individual patients, the classification of risk may vary between transcriptomic tools, thus necessitating a greater understanding of factors influencing discordance between assays13. Efforts are also underway to assess risk with greater granularity—such as improved detection of MRD. The implication of RS < 26 for pre- and postmenopausal women was clearly described in the RxPonder trial6. With a median follow-up of 5.3 years, and when adjusted for menopausal status, continuous recurrence score, and treatment group, the interaction between the continuous recurrence score and treatment group was not significant (P = 0.35). Hence, in women with N1 breast cancer and a recurrence score value of 0 to 25, the recurrence score did not significantly predict any relative improvement to iDFS as a result of chemotherapy treatment. In the overall trial population, patients who received chemoendocrine therapy had a significantly longer period of iDFS versus those who received endocrine therapy alone. iDFS for all participants at 5 years was 91.6%; specifically, 92.2% for the chemoendocrine group compared to 91.0% for the endocrine-only group (P = 0.10 by the log-rank test). There was no significant difference in iDFS between treatment groups for postmenopausal women, with iDFS at 5 years estimated at 91.3% in the chemoendocrine group and 91.9% in the endocrine-only group (hazard ratio for invasive disease recurrence, new primary cancer [breast cancer or another type], or death, 1.02; 95% CI, 0.82 to 1.26; P = 0.89)6. In premenopausal women, the rate of iDFS at 5 years for the chemoendocrine group was 93.9% versus 89.0% for the endocrine-only group (absolute difference, 4.9 percentage points), with a significant benefit from the addition of chemotherapy to ET (hazard ratio for invasive disease recurrence, new primary cancer [breast cancer or another type], or death, 0.60; 95% CI, 0.43–0.83; P = 0.002). All subgroups had a greater iDFS benefit with chemoendocrine therapy compared to endocrine therapy only. The hazard ratios were similar regardless of the type of nodal sampling, number of positive nodes, and recurrence score (0–13 or 14–25)6. Several clinical trials are now prospectively testing the clinical utility of MRD monitoring and early intervention in HR+ (DARE; NCT04567420) and triple-negative (C-TRAK; NCT03145961) early-stage breast cancers. Despite these efforts, many questions on risk stratification in the early breast cancer setting remain to be answered. While multiparametric scores, including both clinicopathological and genomic variables, retain the highest prognostication validity, and testing tools have all been shown to accurately predict both relapse of disease and overall survival, it is unknown which one should be preferred. We need to routinely assess features of the disease as stage, biology and genomic profile to better quantify the risk of HR+/HER2- early-stage breast cancer recurrence. This assessment, may in the feature with the help of artificial intelligence tools or algorithms, we help us to identify those patients candidate to endocrine therapy or to chemotherapy followed by adjuvant CDK 4–6 inhibitors. Potential new technologies, such as liquid biopsy, need to be studied to assess their clinical utility and clinical validity for assessing the risk of relapse or to identify molecular residual disease (MRD) after surgery systemic therapy. We need also to better quantify the magnitude of clinical benefit derived from escalation with CDK 4/6 inhibitors in the context of the world setting and using patient-reported outcomes tools.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
Source data for all figures and tables are provided in the paper. No new data sets have been generated or analyzed for this article.
References
Malmgren, J., Hurlbert, M., Atwood, M. & Kaplan, H. G. Examination of a paradox: Recurrent metastatic breast cancer incidence decline without improved distant disease survival: 1990–2011. Breast Cancer Res. Treat. 174, 505–514 (2019).
Giuliano, A. E., Edge, S. B. & Hortobagyi, G. N. Eighth Edition of the AJCC Cancer Staging Manual: Breast Cancer. Ann. Surg. Oncol. 25, 1783–1785 (2018).
Sestak, I. Risk stratification in early breast cancer in premenopausal and postmenopausal women: integrating genomic assays with clinicopathological features. Curr. Opin. Oncol. 31, 29–34 (2019).
Noordhoek, I. et al. Breast Cancer Index Predicts Extended Endocrine Benefit to Individualize Selection of Patients with HR(+) Early-stage Breast Cancer for 10 Years of Endocrine Therapy. Clin. Cancer Res. 27, 311–319 (2021).
Dieci, M. V., Orvieto, E., Dominici, M., Conte, P. & Guarneri, V. Rare breast cancer subtypes: histological, molecular, and clinical peculiarities. Oncologist 19, 805–813 (2014).
Kalinsky, K. et al. 21-Gene Assay to Inform Chemotherapy Benefit in Node-Positive Breast Cancer. N. Engl. J. Med. 385, 2336–2347 (2021).
Sparano, J. A. et al. Adjuvant Chemotherapy Guided by a 21-Gene Expression Assay in Breast Cancer. N. Engl. J. Med. 379, 111–121 (2018).
Wallden, B. et al. Development and verification of the PAM50-based Prosigna breast cancer gene signature assay. BMC Med Genomics 8, 54 (2015).
Brandao, M., Ponde, N. & Piccart-Gebhart, M. Mammaprint: a comprehensive review. Future Oncol. 15, 207–224 (2019).
Cardoso, F. et al. 70-Gene Signature as an Aid to Treatment Decisions in Early-Stage Breast Cancer. N. Engl. J. Med. 375, 717–729 (2016).
Ovcaricek, T., Takac, I. & Matos, E. Multigene expression signatures in early hormone receptor positive HER 2 negative breast cancer. Radio. Oncol. 53, 285–292 (2019).
Houvenaeghel, G. et al. Lymphovascular invasion has a significant prognostic impact in patients with early breast cancer, results from a large, national, multicenter, retrospective cohort study. ESMO Open 6, 100316 (2021).
Bartlett, J. M. et al. Comparing Breast Cancer Multiparameter Tests in the OPTIMA Prelim Trial: No Test Is More Equal Than the Others. J. Natl. Cancer Inst. 108, djw050 (2016).
Varga, Z., Sinn, P. & Seidman, A. D. Summary of head-to-head comparisons of patient risk classifications by the 21-gene Recurrence Score® (RS) assay and other genomic assays for early breast cancer. Int. J. Cancer 145, 882–893 (2019).
Regan, M. M. Risk stratification according to stage and pathology. Breast 48, S23–S25 (2019).
Kalli, S. et al. American Joint Committee on Cancer’s Staging System for Breast Cancer, Eighth Edition: What the Radiologist Needs to Know. Radiographics 38, 1921–1933 (2018).
Wishart, G. C. et al. PREDICT: a new UK prognostic model that predicts survival following surgery for invasive breast cancer. Breast Cancer Res. 12, R1 (2010).
NHS Predict. https://breast.predict.nhs.uk/tool. Accessed November 2020.
CTS5 Calculator. https://www.cts5-calculator.com/. Accessed November 2020.
Trihia, H. et al. Ki-67 expression in breast carcinoma: its association with grading systems, clinical parameters, and other prognostic factors–a surrogate marker? Cancer 97, 1321–1331 (2003).
Domagala, W., Markiewski, M., Harezga, B., Dukowicz, A. & Osborn, M. Prognostic significance of tumor cell proliferation rate as determined by the MIB-1 antibody in breast carcinoma: its relationship with vimentin and p53 protein. Clin. Cancer Res. 2, 147–154 (1996).
de Azambuja, E. et al. Ki-67 as prognostic marker in early breast cancer: a meta-analysis of published studies involving 12,155 patients. Br. J. Cancer 96, 1504–1513 (2007).
Dowsett, M. et al. Prognostic value of Ki67 expression after short-term presurgical endocrine therapy for primary breast cancer. J. Natl. Cancer Inst. 99, 167–170 (2007).
Ellis, M. J. et al. Letrozole inhibits tumor proliferation more effectively than tamoxifen independent of HER1/2 expression status. Cancer Res. 63, 6523–6531 (2003).
Smith, I. et al. Long-term outcome and prognostic value of Ki67 after perioperative endocrine therapy in postmenopausal women with hormone-sensitive early breast cancer (POETIC): an open-label, multicentre, parallel-group, randomised, phase 3 trial. Lancet Oncol. 21, 1443–1454 (2020).
Cheang, M. C. et al. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J. Natl. Cancer Inst. 101, 736–750 (2009).
Acs, B. et al. Systematically higher Ki67 scores on core biopsy samples compared to corresponding resection specimen in breast cancer: a multi-operator and multi-institutional study. Mod. Pathol. 35, 1362–1369 (2022).
Ellis, M. J. et al. Outcome prediction for estrogen receptor-positive breast cancer based on postneoadjuvant endocrine therapy tumor characteristics. J. Natl. Cancer Inst. 100, 1380–1388 (2008).
Cardoso, F. et al. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. dagger Ann. Oncol. 30, 1194–1220 (2019).
Paik, S. et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N. Engl. J. Med. 351, 2817–2826 (2004).
Precision Oncology. Oncotype DX Breast Recurrence Score® Test Interactive Report Guide. https://precisiononcology.exactsciences.com/healthcare-providers/treatment-determination/breast-cancer/oncotype-dx-breast-recurrence-score/interpret-the-results. Accessed September 28, 2022.
Sparano, J. A. et al. Development and Validation of a Tool Integrating the 21-Gene Recurrence Score and Clinical-Pathological Features to Individualize Prognosis and Prediction of Chemotherapy Benefit in Early Breast Cancer. J. Clin. Oncol. 39, 557–564 (2021).
Fisher, B. et al. A randomized clinical trial evaluating tamoxifen in the treatment of patients with node-negative breast cancer who have estrogen-receptor-positive tumors. N. Engl. J. Med. 320, 479–484 (1989).
Sparano, J. A. et al. Clinical and genomic risk to guide the use of adjuvant therapy for breast cancer. N. Engl. J. Med. 380, 2395–2405 (2019).
Buus, R. et al. Development and validation for research assessment of Oncotype DX® Breast Recurrence Score, EndoPredict® and Prosigna®. NPJ Breast Cancer 7, 15 (2021).
Zhang, Y. et al. A Novel Breast Cancer Index for Prediction of Distant Recurrence in HR(+) Early-Stage Breast Cancer with One to Three Positive Nodes. Clin. Cancer Res. 23, 7217–7224 (2017).
Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Breast Cancer V.4.2022. © National Comprehensive Cancer Network, Inc. 2022. All rights reserved. Accessed September 28, 2022. To view the most recent and complete version of the guidelines, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use, or application and disclaims any responsibility for their application or use in any way.
Lopes Cardozo, J. M. N. et al. Outcome of Patients With an Ultralow-Risk 70-Gene Signature in the MINDACT Trial. J. Clin. Oncol. JCO2102019, https://doi.org/10.1200/JCO.21.02019 (2022).
Dubsky, P. et al. The EndoPredict score provides prognostic information on late distant metastases in ER+/HER2- breast cancer patients. Br. J. Cancer 109, 2959–2964 (2013).
Filipits, M. et al. Prediction of distant recurrence using endopredict among women with ER(+), HER2(-) Node-Positive and Node-Negative breast cancer treated with endocrine therapy only. Clin. Cancer Res. 25, 3865–3872 (2019).
Andre, F. et al. Biomarkers for Adjuvant Endocrine and Chemotherapy in Early-Stage Breast Cancer: ASCO Guideline Update. J. Clin. Oncol. 40, 1816–1837 (2022).
Sgroi, D. C. et al. Prediction of late disease recurrence and extended adjuvant letrozole benefit by the HOXB13/IL17BR biomarker. J. Natl. Cancer Inst. 105, 1036–1042 (2013).
Bartlett, J. M. S. et al. Breast Cancer Index and prediction of benefit from extended endocrine therapy in breast cancer patients treated in the Adjuvant Tamoxifen-To Offer More? (aTTom) trial. Ann. Oncol. 30, 1776–1783 (2019).
Jerevall, P. L. et al. Prognostic utility of HOXB13:IL17BR and molecular grade index in early-stage breast cancer patients from the Stockholm trial. Br. J. Cancer 104, 1762–1769 (2011).
Mamounas EP, B. H. et al. Breast Cancer Index (BCI) and prediction of benefit from extended aromatase inhibitor (AI) therapy (tx) in HR+ breast cancer: NRG oncology/NSABP B-42. J. Clin. Oncol. 39, 501 (2021).
Sparano, J. A. et al. Prospective Validation of a 21-Gene expression assay in breast cancer. N. Engl. J. Med. 373, 2005–2014 (2015).
Paik, S. et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J. Clin. Oncol. 24, 3726–3734 (2006).
Knauer, M. et al. The predictive value of the 70-gene signature for adjuvant chemotherapy in early breast cancer. Breast Cancer Res. Treat. 120, 655–661 (2010).
Dubsky, P. C. et al. The EndoPredict score predicts response to neoadjuvant chemotherapy and neoendocrine therapy in hormone receptor-positive, human epidermal growth factor receptor 2-negative breast cancer patients from the ABCSG-34 trial. Eur. J. Cancer 134, 99–106 (2020).
Burstein, H. J. et al. Customizing local and systemic therapies for women with early breast cancer: the St. Gallen International Consensus Guidelines for treatment of early breast cancer 2021. Ann. Oncol. 32, 1216–1235 (2021).
Dowsett, M. & Turner, N. Estimating Risk of Recurrence for Early Breast Cancer: Integrating Clinical and Genomic Risk. J. Clin. Oncol. 37, 689–692 (2019).
Piccart, M. et al. 70-gene signature as an aid for treatment decisions in early breast cancer: updated results of the phase 3 randomised MINDACT trial with an exploratory analysis by age. Lancet Oncol. 22, 476–488 (2021).
Jahn, B. et al. Personalized treatment of women with early breast cancer: a risk-group specific cost-effectiveness analysis of adjuvant chemotherapy accounting for companion prognostic tests OncotypeDX and Adjuvant!Online. BMC Cancer 17, 685 (2017).
Johnston, S. et al. Randomized Phase II Study Evaluating Palbociclib in Addition to Letrozole as Neoadjuvant Therapy in Estrogen Receptor-Positive Early Breast Cancer: PALLET Trial. J. Clin. Oncol. 37, 178–189 (2019).
Hurvitz, S. A. et al. Potent Cell-Cycle Inhibition and Upregulation of Immune Response with Abemaciclib and Anastrozole in neoMONARCH, Phase II Neoadjuvant Study in HR(+)/HER2(-) Breast Cancer. Clin. Cancer Res. 26, 566–580 (2020).
Curigliano, G. et al. Ribociclib plus letrozole in early breast cancer: A presurgical, window-of-opportunity study. Breast 28, 191–198 (2016).
Finn, R. S. et al. Palbociclib and Letrozole in Advanced Breast Cancer. N. Engl. J. Med. 375, 1925–1936 (2016).
Hortobagyi, G. N. et al. Ribociclib as First-Line Therapy for HR-Positive, Advanced Breast Cancer. N. Engl. J. Med. 375, 1738–1748 (2016).
Turner, N. C. et al. Overall Survival with Palbociclib and Fulvestrant in Advanced Breast Cancer. N. Engl. J. Med. 379, 1926–1936 (2018).
Slamon, D. J. et al. Overall Survival with Ribociclib plus Fulvestrant in Advanced Breast Cancer. N. Engl. J. Med. 382, 514–524 (2020).
Sledge, G. W. Jr. et al. MONARCH 2: Abemaciclib in Combination With Fulvestrant in Women With HR+/HER2- Advanced Breast Cancer Who Had Progressed While Receiving Endocrine Therapy. J. Clin. Oncol. 35, 2875–2884 (2017).
Loibl, S. et al. Palbociclib for Residual High-Risk Invasive HR-Positive and HER2-Negative Early Breast Cancer-The Penelope-B Trial. J. Clin. Oncol. 39, 1518–1530 (2021).
Gnant, M. et al. Djuvant Palbociclib for Early Breast Cancer: The PALLAS Trial Results (ABCSG-42/AFT-05/BIG-14-03. J.Clin. Oncol. 40, 282–293 (2022).
Harbeck, N. et al. Adjuvant abemaciclib combined with endocrine therapy for high-risk early breast cancer: updated efficacy and Ki-67 analysis from the monarchE study. Ann. Oncol. 32, 1571–1581 (2021).
US Food and Drug Administration. FDA approves abemaciclib with endocrine therapy for early breast cancer. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-abemaciclib-endocrine-therapy-early-breast-cancer. Accessed February 22, 2022.
Giordano, S. H., Freedman, R. A. & Somerfield, M. R. Optimal Adjuvant, C. & Targeted Therapy Guideline Expert, P. Abemaciclib With Endocrine Therapy in the Treatment of High-Risk Early Breast Cancer: ASCO Optimal Adjuvant Chemotherapy and Targeted Therapy Guideline Rapid Recommendation Update. J. Clin. Oncol. 40, 307–309 (2022).
Mayer, E. L. et al. Palbociclib with adjuvant endocrine therapy in early breast cancer (PALLAS): interim analysis of a multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 22, 212–222 (2021).
Filipits, M. et al. ESR1, PGR, ERBB2, and MKi67 mRNA expression in postmenopausal women with hormone receptor-positive early breast cancer: results from ABCSG Trial 6. ESMO Open 6, 100228 (2021).
Piezzo, M. et al. Targeting Cell Cycle in Breast Cancer: CDK4/6 Inhibitors. Int. J. Mol. Sci. 21, 6479 (2020).
ClinicalTrials.gov. Adj. Marker-adjusted Personalized Therapy Comparing ET+Ribociclib vs Chemotherapy in Intermediate Risk, HR+/HER2- EBC (ADAPTcycle). https://clinicaltrials.gov/ct2/show/NCT04055493. Accessed March 2, 2022.
ClinicalTrials.gov. Adj. Dyn. Marker-adjusted Personalized Therapy Comparing Abemaciclib + SOC ET vs. SOC ET in Clinical or Genomic High Risk, HR+/HER2- EBC (ADAPTlate). https://clinicaltrials.gov/ct2/show/NCT04565054. Accessed March 2, 2022.
ClinicalTrials.gov. High Risk ER+HER2- T1-2N0-1 Early Breast Cancer With Palbociclib Plus Endocrine Therapy(HIPEx). https://clinicaltrials.gov/ct2/show/NCT04247633. Accessed March 2, 2022.
Coakley, M., Garcia-Murillas, I. & Turner, N. C. Molecular Residual Disease and Adjuvant Trial Design in Solid Tumors. Clin. Cancer Res. 25, 6026–6034 (2019).
Lin, P. H. et al. Circulating Tumor DNA as a Predictive Marker of Recurrence for Patients With Stage II-III Breast Cancer Treated With Neoadjuvant Therapy. Front. Oncol. 11, 736769 (2021).
Magbanua, M. J. M. et al. Circulating tumor DNA in neoadjuvant-treated breast cancer reflects response and survival. Ann. Oncol. 32, 229–239 (2021).
Magbanua, M. J. M. et al. Circulating tumor DNA and magnetic resonance imaging to predict neoadjuvant chemotherapy response and recurrence risk. NPJ Breast Cancer 7, 32 (2021).
Coombes, R. C. et al. Personalized Detection of Circulating Tumor DNA Antedates Breast Cancer Metastatic Recurrence. Clin. Cancer Res. 25, 4255–4263 (2019).
Patel, A. et al. Abstract P1-02-06: Serial monitoring of circulating tumor DNA in patients with metastatic breast cancer. Cancer Res. 77, P1-02-06 (2017).
Page, K. et al. Circulating Tumor DNA Profiling From Breast Cancer Screening Through to Metastatic Disease. JCO Precis. Oncol. 5, https://doi.org/10.1200/PO.20.00522 (2021).
Sant, M., Bernat-Peguera, A., Felip, E. & Margeli, M. Role of ctDNA in Breast Cancer. Cancers (Basel) 14, https://doi.org/10.3390/cancers14020310 (2022).
Shoukry, M., Broccard, S., Kaplan, J. & Gabriel, E. The Emerging Role of Circulating Tumor DNA in the Management of Breast Cancer. Cancers (Basel). 13, https://doi.org/10.3390/cancers13153813 (2021).
Burstein, H. J. et al. Estimating the benefits of therapy for early-stage breast cancer: The St. Gallen International Consensus Guidelines for the primary therapy of early breast cancer 2019. Ann. Oncol. 30, 1541–1557 (2019).
Albain, K. S. et al. Prognostic and predictive value of the 21-gene recurrence score assay in postmenopausal women with node-positive, oestrogen-receptor-positive breast cancer on chemotherapy: a retrospective analysis of a randomised trial. Lancet Oncol. 11, 55–65 (2010).
Stemmer, S. M. et al. Clinical outcomes in ER+ HER2 -node-positive breast cancer patients who were treated according to the Recurrence Score results: evidence from a large prospectively designed registry. NPJ Breast Cancer 3, 32 (2017).
ClinicalTrials.gov. PALbociclib CoLlaborative Adjuvant Study (PALLAS). https://clinicaltrials.gov/ct2/show/NCT02513394. Accessed March 2, 2022.
ClinicalTrials.gov. A Study of Palbociclib in Addition to Standard Endocrine Treatment in Hormone Receptor Positive Her2 Normal Patients With Residual Disease After Neoadjuvant Chemotherapy and Surgery (PENELOPE-B). https://clinicaltrials.gov/ct2/show/NCT01864746. Accessed March 2, 2022.
ClinicalTrials.gov. Endocrine Therapy With or Without Abemaciclib (LY2835219) Following Surgery in Participants With Breast Cancer (monarchE). https://clinicaltrials.gov/ct2/show/NCT03155997?term=monarchE&draw=2&rank=1. Accessed March 2, 2022.
ClinicalTrials.gov. A Trial to Evaluate Efficacy and Safety of Ribociclib With Endocrine Therapy as Adjuvant Treatment in Patients With HR+/HER2- Early Breast Cancer (NATALEE). https://clinicaltrials.gov/ct2/show/NCT03701334. Accessed March 2, 2022.
Jeruss, J. S. et al. Staging of breast cancer in the neoadjuvant setting. Cancer Res. 68, 6477–6481 (2008).
Acknowledgements
We thank the many investigators and patients involved in clinical trials without whose commitment to research the advances reviewed in this paper would not have been possible. Editorial/medical writing support was provided by International Meetings and Science (IMsci) and was funded by Pfizer. No other funding was granted for the study.
Author information
Authors and Affiliations
Contributions
All authors (C.G., R.B., A.L.C., M.P., L.P., N.T., and G.V.) made a substantial contribution to the conception of the article. All authors (C.G., R.B., A.L.C., M.P., L.P., N.T., and G.V.) participated either in the drafting or revising of the article. All authors (C.G., R.B., A.L.C., M.P., L.P., N.T., and G.V.) have approved the final version of the article and assume accountability for all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
G.C. declares no Competing Non-Financial Interests but the following Competing Financial Interests: The author has received institutional financial support and served as an advisor for clinical trials from Bristol-Myers Squibb, Roche, Novartis, Eli Lilly, Pfizer, Daiichi Sankyo, Celcuity, Veracyte, Seagen, AstraZeneca, and Ellipses Pharma. R.D. declares no Competing Non-Financial Interests but the following Competing Financial Interests: The author has served as an advisory consultant for AstraZeneca, Eisai, Merck Sharp & Dohme, Novartis, Pfizer, and Roche; has received fees for expenses from Eisai, Merck Sharp & Dohme, Pfizer, and Roche. A.L-C. declares no Competing Non-Financial Interests but the following Competing Financial Interests: The author has patents and intellectual property with MEDSIR and owns stock in MEDSIR; has served in a leadership role for Eisai, Celgene-BMS, Eli Lilly, Pfizer, Roche, Novartis, Merck Sharp & Dohme, and TESARO-GSK; has been a consultant/advisory board member for Eli Lilly, Roche, Pfizer, Novartis, Pierre Fabre, Genomic Health, and TESARO-GSK; has received speakers bureau honoraria from Eli Lilly, AstraZeneca, Merck Sharp & Dohme, Pfizer, and Roche; has received institutional research funding from Roche, Foundation Medicine, Pierre Fabre, and Agendia; has received fees for expenses, travel, and accommodations (paid or reimbursed) by Roche, Eli Lilly, Novartis, Pfizer, and AstraZeneca. M.P. declares no Competing Non-Financial Interests but the following Competing Financial Interests: The author has received consultation fees from Roche/Genentech, Pfizer, Seagen, and Eli Lilly. L.P. declares no Competing Non-Financial Interests but the following Competing Financial Interests: The author has received consultation fees and honoraria from Seagen, Pfizer, AstraZeneca, Merck, Novartis, Bristol-Myers Squibb, Genentech, Eisai, Pieris Pharmaceuticals, Immunomedics, Clovis Oncology, Syndax, H3 Biomedicine, Radius Health, Personalis, Daiichi Sankyo, Natera; has received institutional research funding from Seagen, AstraZeneca, Merck, Pfizer, and Bristol-Myers Squibb. N.T. declares no Competing Non-Financial Interests but the following Competing Financial Interests: The author has received advisory board honoraria from AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Merck Sharp & Dohme, Novartis, Pfizer, Roche/Genentech, GlaxoSmithKline, Zentalis Pharmaceuticals, Repare Therapeutics, Arvinas; has received research funding from AstraZeneca, BioRad, Pfizer, Roche/Genentech, Merck Sharp & Dohme, Guardant Health, Invitae, Inivata, Personalis, and Natera. G.V. declares no Competing Non-Financial Interests but the following Competing Financial Interests: The author has received consultation fees from Dako/Agilent, Roche, MSD Oncology, AstraZeneca, Daiichi Sankyo, Pfizer, and Eli Lilly.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Curigliano, G., Dent, R., Llombart-Cussac, A. et al. Incorporating clinicopathological and molecular risk prediction tools to improve outcomes in early HR+/HER2– breast cancer. npj Breast Cancer 9, 56 (2023). https://doi.org/10.1038/s41523-023-00560-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41523-023-00560-z
This article is cited by
-
Clinical evaluation of deep learning-based risk profiling in breast cancer histopathology and comparison to an established multigene assay
Breast Cancer Research and Treatment (2024)