Abstract
The source of circulating erythropoietin (EPO), the mediators and the mechanisms involved in the upregulation of EPO gene expression during acute-phase reaction are still poorly understood. Acute-phase reaction was induced by either intramuscular turpentine oil (TO) or intraperitoneal lipopolysaccharide (LPS) administration into wild-type and interleukin (IL)-6 knockout (KO) mice. Animals were killed at different time points and blood, liver and muscle tissue were collected. Serum levels of EPO were measured by enzyme-linked immunoadsorbent assay; liver and injured muscle samples were processed for RNA isolation and for protein analysis. EPO, hypoxia-inducible factors 1α and 2α (HIF-1α and HIF-2α) mRNA were analyzed by RT–PCR and the protein levels were analyzed by western blot and electrophoretic mobility shift assay. HIF-1α and HIF-2α localization was performed through immunofluorescence staining. EPO, HIF-1 and HIF-2 gene and protein expression levels were also analyzed in isolated mouse hepatocytes after stimulation with IL-6. In the wild-type animals, EPO serum levels increased dramatically at 12 h after the insults together with the hepatic gene expression. In TO-treated animals, the EPO gene expression reached an 8.2-fold increase at 12 h, and in LPS-treated mice a similar induction was recorded at 6 h (about 4.5-fold increase). In the IL-6KO strain, the upregulation after the inflammatory stimuli was much lower (only 2.0-fold increase). A progressive upregulation of HIF-1α and HIF-2α was detectable until 6 h after the insults, but only HIF-1α upregulation was reduced in IL-6KO mice. In isolated hepatocytes, stimulation with a single dose of IL-6 induced a nuclear accumulation of HIF-1α, in parallel with an increase of EPO mRNA. No effect on HIF-2α expression was found. IL-6 appears to be the main regulator of EPO gene expression and a major contributor for HIF-1α induction in hepatocytes and Kupffer cells during acute-phase response. The increase of HIF-2α, predominantly expressed in endothelial cells and fibroblast-like cells, seems not to be affected by the lack of IL-6.
Similar content being viewed by others
Main
In mammals, the response to pathogens and tissue damage has been recently pictured as a very well orchestrated process developing through distinct stages.1 The acute-phase response (APR) is a defensive program triggered by the production of proinflammatory cytokines released by inflammatory cells recruited in the injured areas and the major consequence of the action of these acute-phase cytokines on hepatocytes is the synthesis of acute-phase proteins. Cell damage in noninfectious tissue injury activates an ‘injury identification’ stage through the production of molecular markers released as damage-associated molecular pattern molecules.2 These actions aim to isolate and repress pathogens and the damage, but normal cells within the environment are also unavoidably damaged. The ambient tissue (redox state) and the balance between opposing proinflammatory mediator concentrations will determine whether inflammation or tissue protection dominates.
Erythropoietin (EPO) is a 34 kDa glycoprotein hormone mainly involved in the regulation of red blood cell production during physiological and hypoxic conditions.3 Over the past 15 years however, many studies have revealed novel nonhematopoietic functions involved in the acute and subacute biological responses to tissue damage. In fact, EPO has also been identified as a key molecular mediator able to attenuate the immune response triggered by injury and to mediate collateral effects related to the resolution of damage and recovery from injury.4 The concomitant presence in the serum of elevated EPO concentrations and of proinflammatory cytokines has been recently described in several clinical and experimental situations.5, 6 Although the circulating levels of EPO have been observed to increase during several pathophysiological conditions, the sites and the regulation of EPO gene expression during acute-phase reaction have not been investigated enough.
The role of hypoxia-inducible factors 1 and 2 (HIF-1α and HIF-2α) in the regulation of the EPO gene during the embryonic stages and during hypoxic conditions has been clearly described,7, 8 whereas hepatic EPO gene expression and the molecular pathways involved in its regulation during normoxic acute inflammation have been not studied so far. The activity of HIF members is mainly regulated by oxygen concentrations. When oxygen levels are normal, HIF-1α and HIF-2α undergo post-translational modifications by oxygen-dependent prolyl and asparaginyl hydroxylases that promote their degradation.9 When oxygen levels are low, oxygen-dependent hydroxylases are inactive and HIF-α signaling increases. Accumulation of HIF-2α is considered to be predominantly due to post-translational regulation as mRNA levels are not significantly induced under hypoxia.10 HIF-activated genes protect against damaging reactive oxygen molecules generated by mitochondria in response to hypoxia and other stresses,11 and also induce erythrocyte proliferation and blood vessel formation.12 Numerous growth factors and cytokines have been shown to increase HIF-α member stabilization and activity, and to induce HIF-1α gene expression,13 but the gene regulation and the protein stabilization during acute-phase reaction have not been considered yet. More importantly, the correlation between the HIF members and other transcriptional systems, like STAT-3 and NF-κB, has been shown to be essential for maximal and cell-type-specific upregulation of HIF target genes.14, 15 Recently, Dioum et al16 suggested an important role of the nicotinamide adenine dinucleotide (NAD)-dependent deacetylase, SiRT-1, in HIF-2α activation.
The components of the APR are individually regulated and not all the mediators involved in this process uniformly increase in all the patients with the same illness. This consideration, possibly explained by differences in the patterns of production of specific cytokines or their modulators in different pathophysiological states, prompted us to compare two experimental models of acute phase. With this clinical foundation, this study was performed on two murine models to evaluate the gene expression of EPO in the liver and the possible mechanisms involved in its regulation. Turpentine oil (TO) administration in the muscle induces a local sterile abscess with a consequent release of acute-phase cytokines (mainly interleukin (IL)-6) from the site of injury.17 These cytokines are considered to be responsible for the changes of gene expression in the hepatocytes. Intraperitoneal injection of lipopolysaccharide (LPS) simulates, at least in part, a Gram-negative sepsis whereby a massive upregulation of hepatic cytokines takes place through the activation of liver macrophages.18 Mice knocked out for the IL-6 (knockout, KO) gene and the respective wild-type strain were administered TO intramuscular injections or bacterial LPS intraperitoneal injections to investigate the relative importance of the different acute-phase cytokines in vivo. We analyzed the gene and protein expression of EPO, HIF-1α and HIF-2α in the livers of control and treated animals of both strains. We observed an increase in EPO and HIF-1α after the two experimental treatments in the wild-type animals, but the absence of IL-6 significantly reduced the gene upregulation in the KO strain. HIF-2α increase was not altered in the IL-6KO mice, although the LPS treatment did not induce an increase in gene expression. To evaluate the role of IL-6 in EPO gene regulation, we analyzed EPO, HIF-1α and HIF-2α gene expression in isolated liver cell populations. The results obtained indicate that IL-6 is an essential regulator of EPO gene expression and possibly of HIF-1α during acute-phase conditions mainly in hepatocytes, in spite of an increase of HIF-2α that turned out not to be affected by the loss of IL-6. Recent findings supporting antioxidant19 and protective functions20 of EPO seem to match with our observations, identifying EPO as one more weapon in the arsenal of the antioxidant and protective cellular mechanism that responds to injury and environmental stresses.
MATERIALS AND METHODS
Animals
Adult male B6.129S2-Il6tm1Kopf (IL-6 KO) mice and control wild-type adult male C57BL/6J mice (25–28 g) were purchased from Jackson Laboratory. The animals were kept under standard conditions with 12 h light/dark cycles and ad libitum access to fresh water and food pellets. All animals were treated according to the University's guidelines, the German convention for the protection of animals and NIH guidelines.
Experimental Models
A group of animals (n=3) for each strain was injected intramuscularly with 0.1 ml TO in both right and left hind limbs to induce an aseptic acute-phase reaction. A second group of animals (n=3) for each strain was injected intraperitoneally with 50 μg LPS from E. coli serum type to induce a nonsterile acute-phase reaction. Animals were killed 2, 4, 6, 12 and 24 h after the treatments under pentobarbital anesthesia. Liver, kidney and injured muscle tissues were excised and minced, rinsed with physiological sodium saline, snap frozen in liquid nitrogen and stored at −80°C till further use. Blood samples were collected from the inferior vena cava of the control and treated animals, allowed to clot overnight at 4°C and centrifuged for 20 min at 2000 g. Serum was removed and stored at −20°C.
Enzyme-Linked Immunoadsorbent Assay
For detection of EPO concentrations in serum, Quantikine Mouse/Rat ELISA kits from R&D Systems were used. Serum samples were processed according to the manufacturer's instructions.
RNA Isolation and Quantitative Real-Time PCR
Total RNA was isolated from hepatic tissue samples with TRIzol reagent according to the manufacturer's instructions and the RNA concentration was then quantified by measuring the absorbance at 260/280 nm. The cDNA was generated by reverse transcription of 3.0 μg of total RNA with 100 nM of dNTPs, 50 pM of primer oligo(dT)15, 200 U of Moloney murine leukemia virus reverse transcriptase, 16 U of protector RNase inhibitor, 1 × RT buffer and 2.5 ml of 0.1 M DTT for 1 h at 40°C. The primers used in this work are listed in Table 1. Gene expression was analyzed using Platinum SYBR Green qPCR mix UDG. β-Actin and ubiquitin c were used as housekeeping genes. Expression of IL-6, IL-1β, TNF-α, EPO, HIF-1α, HIF-2α, SiRT-1 and SOD-2 (manganese superoxide dismutase) was analyzed using Fast Taq SYBR Green. β-Actin and ubiquitin c were used as endogenous control. Primers sequences used are given in Table 1. The amplification was performed at 95–60°C for 45 cycles in an Applied Biosystems StepOne Plus sequence detection system. All samples were assayed in duplicate. The results were normalized to the endogenous control and fold change expression was calculated using Ct values, and comparisons to experimental controls.
Proteins Isolation and Western Blot Analysis
Total protein extraction was prepared from liver samples as previously described.21
Briefly, about 100 mg of frozen tissue was homogenized with an Ultra-Turrax TP 18/10 three times for 10 s each in 10 volumes of 50 mM Tris-HCl buffer (pH 7.4), containing 150 mM sodium chloride, 1 mM ethylenediaminetetraacetic acid (EDTA), 1% Triton X-100, 1 mM phenylmethanesulfonyl fluoride (PMSF), 1 mM benzamidine, 1 mg/ml leupeptin, 10 mM chymostatin, 1 mg/ml antipain and 1 mg/ml pepstatin A. Samples were then centrifuged twice for 15 min at 10 000 g and protein concentration was determined with Coomassie Blue Reagent (Pierce Biotechnology).
Total protein lysates (50 μg) were loaded in a 4–12% Nu-PAGE Bis-Tris (Invitrogen) gel and separated after 2 h electrophoresis at 100 V. After the transfer, the membranes were blocked in 5% milk and blotted with a rabbit anti-mouse/human/rat EPO (Santa Cruz Biotechnology) diluted 1:200, rabbit polyclonal anti-HIF-1α (Santa Cruz Biotechnology) diluted 1:200, polyclonal rabbit anti-HIF-2α (Santa Cruz Biotechnology) diluted 1:200 overnight at 4°C, monoclonal mouse anti-SiRT-1 (Sigma-Aldrich) diluted 1:400 and monoclonal mouse anti-β-actin (Sigma-Aldrich).
The secondary antibody was swine anti-rabbit immunoglobulins (Dako, Glostrup, Denmark) diluted at 1:1000. Membranes were developed with ECL Chemiluminescence Kit (Amersham).
A densitometric analysis of the western bands was performed using the software ImageJ 1.42q and the values were expressed as the ratio between protein band density and β-actin band density.
Immunohistochemistry and Immunocytochemistry
Immunohistochemical analyses were performed on 4 μm-thin cryostat sections fixed in methanol/acetone. After blocking nonspecific binding with PBS containing 1% bovine serum albumin (BSA; Serva, Heidelberg, Germany) and 10% goat serum (Dako) for 1 h at room temperature, the primary antibodies rabbit anti-HIF-1α (Novus Biologicals) and rabbit anti-EPAS-1 (Santa Cruz Biotechnology) were incubated overnight at 4°C on the sections. The rabbit polyclonal antibodies were detected with Alexa-555-conjugated goat-anti-rabbit and Alexa-488-conjugated goat-anti-mouse secondary antibodies (Molecular Probes, Leiden, the Netherlands). Sections were counterstained with DAPI (Molecular Probes) and observed with an epifluorescence microscope (Axiovert 200M; Zeiss, Jena, Germany). Negative control immunostainings were performed by omission of the primary antibody and use of isotype-matching control immunoglobulins. For HIF-1α and HIF-2α localization in macrophages, we used a mouse-specific macrophage marker F4/80 (AbDSerotec) at a dilution 1:100 in an antibody mixture with the previously mentioned antibodies.
After the treatment with IL-6, hepatocytes and Kupffer cells (KCs) were washed twice with cold PBS and fixed in methanol/acetone. For colocalization analysis, after the blocking for 1 h at room temperature, the sections were incubated overnight at 4°C with a mixture of primary antibody containing rabbit anti-EPAS-1 in combination with mouse anti-CK19 (Novocastra), or mouse anti-desmin (Sigma-Aldrich) or mouse anti-ED2 (Serotec). As mentioned above, the antibodies were detected with a mixture of Alexa-555-conjugated goat-anti-rabbit and Alexa-488-conjugated goat-anti-mouse secondary antibodies (Molecular Probes).
EMSA Assay and Supershift Analysis
Electrophoretic mobility shift assay (EMSA) was performed using the EPO promoter hypoxia response element (HRE) (Epo sense oligonucleotide 5′-GCCCTACGTGCTGTCTCACACAGC-3′ and antisense oligonucleotide 5′-GCTGTGTGAGACAGCACGTA-3′). The annealed oligonucleotides were labeled with γ-ATP using T4 Polynucleotide Kinase (Promega) and cleared in G-50 microcolumn (Amersham). The labeled oligonucleotides (20 000 c.p.m. per μl) were incubated with 30 μg of proteins for 20 min at room temperature in binding buffer, and the complex were separated in a 6% electrophoretic gel at 200 V for 2 h, as previously described.22 The supershift analysis was performed by incubating the protein extracts with 5 μg of anti-HIF-1α and of anti-HIF-2α (Novus Biologicals) 30 min before the reaction with binding buffer.
Isolation and Culture of Mouse Hepatocytes and Rat Kupffer Cells
Hepatocytes from C57BL/6J mouse livers were isolated by a two-step enzymatic dissociation as previously described,23 with some modifications. Briefly, the liver was perfused at a rate of 10 ml/min with a perfusion buffer for 5 min and then with a second buffer containing 0.01% collagenase type I for 5 min at a rate of 12 ml/min. Hepatocytes were then dispersed, filtered and centrifuged at 200 g. The isolated cells were cultured in Dulbecco's modified Eagle's medium containing 10% fetal calf serum (FCS), 1% penicillin/streptomycin, 1% L-glutamine, 10 nM dexamethasone and 10 nM insulin for 24 h before stimulation with cytokines. For the stimulation with IL-6 at different concentrations (1, 10, 100, 500, 1000 ng/ml) of the hepatocytes, a serum-free medium containing 0.2% BSA was used.
A rat KC-enriched fraction was isolated by centrifugal elutriation according to the method of Knook et al24 as previously described.25 At more than 90% purity, KCs were cultured in M-199 supplemented with 10% FCS, kept in incubation at 37°C overnight and successively stimulated with IL-6 (100 ng/ml).
Biosynthetic Labeling, Immunoprecipitation and NuPAGE Analysis of Newly Synthesized Erythropoietin
Newly synthesized protein from primary cultured mouse hepatocytes were radiolabeled as previously described.26 Briefly, mouse hepatocytes were kept in culture 24 h and successively labeled in methionin-free RPMI medium supplemented with 35S-methionin (100 μCi/300 μl medium pro well) for 6 h. Part of the cells was further stimulated with murine IL-6 at a concentration of 100 ng/ml. After the labeling, cells were washed three times in PBS whereas the supernatants were collected and diluted in 50% lysis buffer containing 1% sodium dodecyl sulfate (SDS). Cells were submitted to cycles of freezing and thawing and scraped in lysis buffer supplemented with 1% PMSF but without SDS. Cell lysates were then collected and diluted to 50% with lysis buffer with SDS. The count of the total labeled proteins was taken after a trichloroacetic acid precipitation. For immunoprecipitation with anti-EPO (Santa Cruz Biotechnology) supernatants and cell lysates, the same numbers of total labeled proteins were used. Samples were precleared with protein A and incubated with the antibody overnight at 4°C. Immunocomplexes were precipitated by adding 50 μl of protein A and incubated for 1 h on ice, centrifuged and washed with lysis buffer containing SDS supplemented with 0.5% BSA. Samples were finally resuspended in loading buffer containing 5% β-mercaptoethanol. Immunoprecipitated EPO was analyzed in a 4–12% Nu-PAGE Bis-Tris gel, as described earlier, for 3 h at 80 V. Afterwards, gels were fixed overnight, incubated for 1 h in Amplify Fluorographic Reagent (GE Healthcare, Freiburg, Germany), covered with cellophane and then dried. Dried gels were analyzed by autoradiography.
Statistical Analysis
The results are shown as means±standard deviation. The significance within groups compared to the control was established according to Student's t-test and the intragroup analysis of variance (ANOVA) in the cell treatment was performed with a one-way ANOVA test. Significant difference was assessed at P<0.05.
RESULTS
Acute-Phase Response Cytokines Gene Expression after Intramuscular Turpentine Oil Injection
The APR induced by TO injection is characterized mainly by a massive release of IL-6 and IL-1β from the injured muscle. As illustrated in Figure 1a, the values of IL-6 and IL-1β progressively increased already from the second hour after the injection to peak at 6 h with an expression of 297±74- and 135±19-fold increase, respectively. The serum concentration of IL-6 gradually increased until 12 h after the injury with values of about 3 ng/ml (data not shown). The expression of TNF-α never reached values statistically different from the control group during the analyzed kinetic. In the IL-6 KO animals, the lack of IL-6 appeared to be compensated by a more strongly induced augment of IL-1β, which reaches a 450-fold increase at 12 h after the injection (Figure 1b). In this group also TNF-α gene was significantly upregulated with a maximum of expression up to 115±45-fold increase at 12 h.
Pattern of acute-phase cytokine expression in TO-injured muscles of wild-type (a) and IL-6KO mice (b). The relative expression was normalized using β-actin as housekeeping gene. IL-6 and IL-1β show a parallel kinetic of expression, with a significant upregulation already at 2 h after injection. They reach a peak of expression of 300- and 130-fold at 6 h after the administration followed by a progressive decline. No significant change in TNF-α gene expression is observed. In the IL-6KO strain the absence of IL-6 seems to be compensated by a stronger delayed upregulation of IL-1β increased up to 450-fold at 12 h after the injury with a similar increment of TNF-α up to a 110-fold increase. Results are expressed as mean±s.d. *Values significantly different compared with the control group (P<0.05, **P<0.01 analyzed by Student's t-test, N=3).
Acute-Phase Response Cytokines Gene Expression after Intraperitoneal LPS Administration
The APR induced by LPS administration is triggered mainly by KCs that come in contact with the bacterial component through the TLR4 receptor. The cytokine pattern that characterizes the acute response was more homogeneous, and IL-1β and TNF-α represent the main inflammatory mediators released by the liver (Figure 2). In the wild-type group, IL-1β reached a maximum peak at 4 h up to 108±26-fold, whereas TNF-α after a sudden and progressive upregulation peaked at 6 h up to 58±15-fold (Figure 2a). However, IL-6 showed a sudden augment at 2 h (53±6-fold increase) and remained constantly expressed until 6 h after which it progressively declined (Figure 2a). As shown in Figure 2b, the lack of IL-6 in this situation seems not to alter the cytokines expression except for an earlier upregulation of IL-1β and TNF-α. The mRNA levels of IL-6 were also detected in knockout mice to provide an appropriate control (Supplementary Figure 1).
Pattern of acute-phase cytokine expression in the liver of LPS-injected wild-type (a) and IL-6KO mice (b). The relative expression was normalized using β-actin as housekeeping gene. In this model, the induction of IL-1β expression (110-fold increase) overcomes the upregulation of IL-6 (55-fold increase). The expression of TNF-α in this case is also significantly induced until 6 h (up to 60-fold increase). In the IL-6KO strain no significant quantitative alteration are observed, other than a slight earlier upregulation of IL-1β and TNF-α with a peak of expression at 2 h. Results are expressed as mean±s.d. *Values significantly different compared with the control group (P<0.05, **P<0.01 analyzed by Student's t-test, N=3).
EPO Serum Concentrations after APR Induction
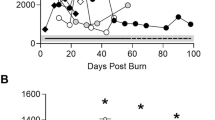
Erythropoietin serum concentration increased by about twofold compared with the control animals already 2 h after TO administration, then slightly declined to the control levels within 6 h. At 12 h we recorded a sudden increase that reached a 20-fold change to then gradually decline at 24 h after the insult (Figure 3a). In the IL6O strain, after a slight initial increase of about twofold, the levels of circulating EPO progressively declined over to 24 h (Figure 3a). The sudden increase at 2 h followed by a modest decline was also observed in the LPS-treated mice and a similar peak was registered at 12 h, but the increase was only 3.5-fold compared to the normal animals (Figure 3b). In the IL-6KO mice, the serum EPO concentration did not exceed a twofold increase in any of the time points analyzed (Figure 3b).
Serum EPO concentration in TO (a)- and LPS (b)-treated animals. The EPO concentration in serum samples was detected using an ELISA kit according to the manufacturer's instructions. The serum concentration of EPO in normal mice is around 110 pg/ml. After a sudden twofold increase, a progressive decrease up to the control levels is recorded until 6 h after the treatments in wild-type animals. At 12 h the circulating levels of EPO reach a concentration of about 2 ng/ml in the TO-administered group (a) and 350 pg/ml in the LPS-treated group (b). In the IL-6KO strain the concentration of EPO progressively declines after the muscular injury and does not increase more than twofold in the LPS-stimulated animals.
APR in Both Experimental Conditions Results in an Upregulation of EPO Gene Expression in the Livers of Wild-Type Mice, but a Significantly Lower Increase in the Livers of IL-6KO Mice
The hepatic values of EPO gene expression increased significantly in both models of APR in wild-type mice. Even if with different kinetics of expression, the values augment progressively to reach a peak of 8.2±2.2-fold at 12 h in the TO-administered animals (Figure 4a), whereas in the LPS-treated animals, the peak expression of 4.6±1.1-fold was recorded at 6 h followed by a progressive decline until 24 h (Figure 4b). In the IL-6KO animals the increase of EPO gene expression was dramatically reduced to 1.8±0.1-fold at 6 h in the TO model and a similar drastic decrease to 1.4-fold was observed in the LPS-treated animals at 6 h (Figure 4a and b). The western blot analysis (Figure 7a) showed a similar progressive increase of the EPO protein hepatic until 12 h after TO administration and until 4 h in the LPS-treated wild-type mice. Both the treatments induced a weaker protein increase in the livers of IL-6KO mice (Figure 8a). Of note, EPO is a glycoprotein hormone stored in the cell in very low amounts and the newly synthesized protein is supposed to be quickly secreted into the circulation. This could explain the low increase in the tissue protein content compared to the high mRNA induction.
EPO mRNA hepatic expression of wild-type and IL-6KO after TO injection (a) and LPS (b) treatment. The relative expression was normalized using β-actin as housekeeping gene. EPO gene expression, after an initial decrease, was significantly upregulated at 12 h after TO administration in the wild-type strain (8.2±2.2-fold increase), whereas in the IL-6KO strain the increase reached 2.0±0.4-fold at 6 h and progressively declined to control level within 12 h (a). LPS treatment induced a lower increase between 6 and 12 h after the injection in the wild-type group (4.6±1.1- and 2.5±0.8-fold increase, respectively) (b). EPO gene expression remained almost unvaried in the IL-6KO mice treated with LPS. Results are expressed as mean±s.d. *Values significantly different compared with the control group (P<0.05, **P<0.01 analyzed by Student's t-test, N=3).
In mice, after TO administration the kidney showed a kinetic of expression similar to that observed for the liver (data not shown), but with a lower upregulation of up to 2.5-fold increase at 12 h in terms of mRNA expression. The LPS treatment induced a similar upregulation of EPO mRNA expression in both liver and kidney with a similar temporal pattern of induction. Lack of IL-6 almost totally reversed the renal EPO mRNA increase in both experimental models (data not shown).
APR Induced in Both the Experimental Conditions Results in an Upregulation of HIF-1α Gene and Protein Expression in the Livers of Wild-Type Mice, but in a Significantly Lower Increase in the Livers of IL-6KO Mice
The RT–PCR analysis revealed a parallel progressive upregulation of HIF-1α gene common to both the experimental models of APR (Figure 5). The degree of the augment in the number of transcripts was similar in TO- and LPS-treated wild-type mice (maximum 5.0±1.5- and 5.9±1.4-fold increase, respectively, at 6 h; Figure 5a and b). In the IL-6KO strain, no significant increase in the number of transcripts was observed after the TO administration, whereas in the LPS-treated group HIF-1α gene upregulation reached a peak of 3.7±1.5-fold at 6 h.
HIF-1α (a and b) mRNA hepatic expression of wild-type and IL-6KO mice after turpentine oil (TO) administration and LPS treatment. The relative expression was normalized using β-actin as housekeeping gene. HIF-1α gene expression follows a progressive increase up to 5.0-fold at 6 h after TO injection in the wild-type animals (a). Similarly, after LPS stimulation the hepatic changes of HIF-1α peak up to 5.9-fold at 6 h (b). The lack of IL-6 in vivo resulted in a dramatic inhibition of HIF-1α gene upregulation after TO injection (a), whereas the increase observed after LPS treatment was slightly reduced (b). Results are expressed as mean±s.d. *Values significantly different compared with the control group (P<0.05, **P<0.01 analyzed by Student's t-test, N=3).
The western blot analysis (Figure 7a) showed an augment of the signal already at 2 h, but was particularly evident at 12 h after TO treatment in wild-type mice, whereas in the LPS-treated animals, a stronger expression was registered within 6 h from the injection. In the IL-6KO animals (Figure 8a) the relative augment in the protein content was less prominent in both the acute-phase reaction models. The analysis of binding performed by EMSA revealed a progressive increase of HIF activity after TO administration with a particularly strong intensity of binding between 4 and 6 h (Figure 9a and b). A similar situation can be observed after LPS treatment, where the radiography showed an earlier increase of the signal at 4 h (Figure 9a and b). The supershift analysis indicates that a part of the binding protein is constituted by HIF-1α (Figure 9c).
HIF-2α Gene Expression Increases after TO Treatment in Both the Mice Strains, but LPS Injection Induces only an Augment of the Protein Levels without Affecting the Expression
The HIF-2α mRNA levels are particularly high in the normal liver, but liver protein content results in a minimal detectable concentration. Only after TO administration was there an upregulation of HIF-2α gene expression with a peak of 3.2±0.4-fold at 6 h for the wild-type and a peak of 2.5±0.2-fold at 12 h in the IL-6KO mice (Figure 6a and b). Interestingly, both of the acute-phase models were able to induce a stabilization of the protein in wild-type and IL-6KO mice, as reported in the western blot analysis (Figures 7a and 8a). This result clearly indicates that, for HIF-2α, the gene expression and the protein stabilization are independently regulated. Moreover the radiography obtained after supershift analysis in Figure 9c showed an almost complete disappearance of the signal after incubation with HIF-2α antibody, indicating a further involvement of this member in the transcription complex.
HIF-2α (a and b) mRNA hepatic expression of wild-type and IL-6KO mice after TO injection and LPS treatment. The relative expression was normalized using β-actin as housekeeping gene. HIF-2α gene expression was significantly augmented after TO injection in the wild-type group, with a delay in the kinetic in the IL-6KO strain (3.2±0.4- and 2.5±0.1-fold increase, respectively) (a). No significant variations of HIF-2α were detected (b). Results are expressed as mean±s.d. *Values significantly different compared with the control group (P<0.05, **P<0.01 analyzed by Student's t-test, N=3).
Western blot analysis of EPO, HIF-1α and HIF-2α in liver of wild-type mice during two models of acute-phase reaction. EPO protein tissue levels slightly increased in the liver between 4 and 12 h. The sudden release of the protein into the circulation and very low amounts of stored protein in the cells could explain the low augment of signal detected by western blot analysis. The HIF-1α band slightly increased at 6 h after turpentine oil (TO) injection and was strongly expressed at 2 and 4 h after LPS treatment in wild-type animals (a). The densitometric analysis normalized to β-actin expression revealed a parallel increase of EPO and HIF-2α protein levels up to 12 h after TO injection, whereas HIF-1α protein augment peaked at 6 h after the treatment (b). In the LPS-treated group, the increase in EPO and HIF-1α tissue levels were quite modest compared to a stronger HIF-2α protein expression (c).
Western blot analysis of EPO, HIF-1α and HIF-2α in livers of IL-6KO mice during two models of acute-phase reaction. EPO protein tissue levels seem not be altered in this strain as also HIF-1α levels showed to be after turpentine oil injection. LPS treatment resulted in any case in an increase of HIF-1α protein levels, whereas HIF-2α expression seems not to be affected by the lack of IL-6 (a). The densitometric analysis normalized to β-actin supports the images obtained using western blotting, in which for both models HIF-2α protein expression increased in the IL-6KO strains as well (b and c).
EMSA analysis of DNA-binding activity. The signal of binding progressively increases up to 6 h in both acute-phase models in the wild-type strain, whereas a maximum of signal expression is recordable at 4 h in the IL-6KO strain (a and b). The supershift analysis confirms the involvement of both HIF members in the HRE binding region during acute-phase reaction (c). (c: TO-treated animals at 4 and 6 h, lanes 1 and 2; competition with 100 × , 200 × and 400 × cold probe, lanes 3–5; anti-HIF-1α 4 and 6 h after TO and LPS treatment, lanes 6–9; anti-HIF-2α 4 h and 6 h after TO and LPS treatment, lanes 10–13).
HIF-1α and HIF-2α Tissue Localization during APR
The immunofluorescence staining with anti-HIF-1α resulted in a weak positivity diffused in all the hepatic parenchyma (Figure 10a), suggesting the presence of small amounts of the protein mainly in the cytosolic compartment of the hepatocytes. In can be seen in Figure 10b, it is possible to observe how after the turpentine injection HIF-1α positivity slightly increases and is located mainly in the nuclei of the hepatocyte, although some nonparenchymal cells (reasonably KCs) show an evident positivity too. Conversely, the LPS represents a phenomenon mainly promoted by the macrophage compartment that directly interacts through the TLR4 receptor. In this case, KCs evidently showed a strong positivity for HIF-1α, justifying an increase of the protein observed by western blot, although also hepatocyte clearly expresses a nuclear positivity (Figure 10c and d).
Immunolocalization of HIF-1α in the livers of wild-type mice during acute-phase reaction. Immunostaining analysis reveals a weak cytoplasmic positivity involving all the hepatic parenchyma of control animals (a). In TO-treated animals the positivity is particularly evident in the nuclei of hepatocytes (b, arrows) with the presence of extraparenchymal positivity (arrowheads). The LPS treatment induces an increase of the protein levels also in the nuclei of the extraparenchymal cell population (reasonably Kupffer cells) (c, arrowheads), whereas hepatocytes clearly express a nuclear signal (c, arrows). The double stain with F4/80 antibody better identifies a colocalization of HIF-1α-positive macrophages in green (d).
In the liver the protein levels of HIF-2α were detectable mainly in proximity with the sinusoidal spaces (Figure 11a), indicating a stronger expression reasonably in endothelial cells and interstitial cell populations as previously suggested, like fibroblasts or activated KCs. Under normal physiologic conditions, hepatocytes revealed a weak presence of HIF-2α protein, and even after TO administration and LPS treatment the clearest positivity was detected in nonparenchymal cells (Figure 11b and c). Interestingly, nonparenchymal F4/80-negative cells located near the sinusoidal spaces also showed a strong positivity for HIF-2α, indicating probable infiltrating inflammatory cell populations (Figure 11d).
Immunolocalization of HIF-1α in the livers of wild-type mice during acute-phase reaction. HIF-2α immunostaining reveals a clear positivity of nonparenchymal cells, probably sinusoidal or macrophage compartment, with a weak positivity in the hepatocytes nuclei (a). The signal increases after TO treatment in the same nonparenchymal district (macrophage-like cells) (b and c) but also in some hepatocytes nucleus. The double stain with F4/80 antibody indicates the presence of HIF-2α -F4/80-positive cells (arrowheads), although a population of F4/80-positive cells was negative for HIF-2α (arrows) (d).
A similar pattern of cellular expression has also been confirmed by immunostaining in different liver cell populations, where hepatocytes presented a clear induction of HIF-1α protein in the nuclei, whereas HIF-2α was mainly expressed in colocalization with desmin-positive cells (Figures 12 and 13).
Immunolocalization of HIF-1α and HIF-2α in mouse hepatocytes after IL-6 stimulation in normoxic conditions. Although sporadic mouse hepatocytes present a weak positivity for HIF-1α, after the treatment with 100 ng/ml of IL-6 the number and the signal of positive cells clearly augment (arrowheads). No changes or nuclear increase in HIF-2α positivity are detectable after IL-6 stimulation (original magnification, × 200).
Immunolocalization of HIF-1α and HIF-2α (a and b) in nonparenchymal liver cells. The isolation of a nonparenchymal cell fraction allowed the characterization of a macrophage-enriched cell population, with a residual contamination of about 5–10% composed mainly of fibroblasts and a few endothelial cells and cholangiocytes (a). The stimulation with IL-6 (100 ng/ml culture medium) seems not to influence significantly the levels of HIF-1α and HIF-2α protein, expressed in modest cytosolic and nuclear amounts in the control cells. Interestingly, it is possible to recognize small isolated round cells (arrowheads) or cells organized in clusters that present a particularly strong positivity for HIF-2α (original magnification, × 200). The merge in the double-stain analysis revealed a main double positivity for HIF-2α and desmin (arrowheads), indicating a probable identification of those cells as fibroblasts or endothelial cells organized in clusters, as also previously suggested although rare CK-19-positive cells also express a marked positivity for HIF-2α (b).
Hepatocytes Stimulation with IL-6 Upregulates EPO and HIF-1α Gene Expression
The stimulation of mouse hepatocytes with increasing concentrations of IL-6 modestly induced a significant upregulation of EPO gene at a concentration between 10 and 100 ng/ml of 2.5- and 1.5-fold, respectively, compared to the control group after 6 h of treatment (Figure 14a). Interestingly, we observed a dose-dependent induction of HIF-1α showing an up to 2.3-fold increase but no significant effects were observed on HIF-2α gene (Figure 14b and c). In parallel, a proportional increase of the HIF-1α protein levels was also detected after IL-6 stimulation, but no evident protein increase was reported for HIF-2α (Figure 14d). The protein detection was supported by densitometric analysis shown in Figure 15. Moreover, the biosynthetic analysis in primary cultured mouse hepatocytes showed an increase in the protein synthesis after stimulation with IL-6 (single dose 100 ng/ml culture medium) with an augmented signal for the supernatants, too, to indicate an active release of EPO in the culture medium (Figure 14e). The immunostaining analysis also showed a nuclear accumulation of HIF-1α (Figure 12, upper panels) in the nuclei of hepatocytes treated with IL-6 (100 ng/ml culture medium), but no clear effects on HIF-2α protein (Figure 12, lower panels).
Mouse hepatocytes stimulation with IL-6 in normoxic conditions. The stimulation with different IL-6 concentrations at 6 h induces an upregulation of EPO genes particularly at a concentration between 10 and 100 ng/ml and a dose-dependent increase of HIF-1α gene expression (a and b), but an apparent downregulation of HIF-2α gene (c). The expression of HIF-1α and HIF-2α reflects in parallel an increase and a decrease of the relative protein levels, respectively (d). Interestingly, the biosynthetic labeling reveals an increase of newly synthesized EPO in hepatocytes stimulated by 100 ng/ml IL-6 for 6 h, and an increase of the extracellular protein content indicating an active secretion from the hepatocytes (e). Results are expressed as mean±s.d. *Values significantly different compared with the control group (P<0.05, **P<0.01 analyzed by Student's t-test, N=3).
Densitometric analysis of HIF-1α (a) and HIF-2α (b) western blot from mouse hepatocytes stimulated with IL-6 in normoxic conditions. The densitometric analysis revealed a progressive increase of HIF-1α protein levels that present a 2-fold increase with an IL-6 concentration between 100 and 500 ng/ml (a). HIF-2α protein slightly increased (1.3-fold increase) only at the highest IL-6 concentration 1000 ng/ml (b).
SiRT-1 Gene Expression Resulted in Increases after TO Treatment That are not Induced in the IL-6KO Strain
The activity of HIF-2α has been shown to be regulated by deacetylation other than phosphorylation (Figure 16). The deacetylation of this protein seems to be fundamental for its transcriptional activity and it directly contributes to Epo regulation in mice. Interestingly, although both strains showed increased levels of HIF-2α protein, a significant change of the mRNA transcripts of up to 2.1±0.1-fold increase within 2 and 4 h after TO administration in the wild-type animals was observed, whereas no increase was detected in the IL-6KO mice (Figure 16a). The LPS treatment resulted in a lower increase of SiRT-1 gene expression of up to 1.4-fold that was not altered by the absence of IL-6 (Figure 16b). The protein analysis revealed an augment of the protein levels particularly evident at 6 h in both models for the wild-type animals (Figure 17a). In the IL-6 KO strain, no clear increase of the protein content was detectable through western blot analysis (Figure 17b).
SiRT-1 mRNA hepatic expression in wild-type and IL-6KO mice after TO injection (a) and LPS treatment (b). The relative expression was normalized using β-actin as housekeeping gene. After TO administration, the number of transcripts significantly already increased at 2 h (2.1±0.1-fold increase) and remained constantly elevated until 12 h followed by a progressive decline. No significant changes were detectable after treatment in the IL-6KO strain (a). In the LPS-treated group the lack of IL-6 seems not to influence SiRT-1 gene expression, and after a slight initial increase, the values declined progressively over 24 h (b). Results are expressed as mean±s.d. *Values significantly different compared with the control group (P<0.05, **P<0.01 analyzed by Student's t-test, N=3).
SiRT-1 protein expression in liver during acute-phase reaction. SiRT-1 protein expression was quite modest in normal control animals and a slight increase was detectable at 6 h after both treatments (a). No evident changes in SiRT-1 protein expression were detectable in IL-6KO animals subjected to both models (c). The densitometric analysis normalized to β-actin confirmed the western blot images with a relative increase of 1.5- and 1.4-fold changes in TO- and LPS-treated animals, respectively (c–d).
Expression of SOD-2, a Gene known to be Regulated by HIF-2α, Increases during APR Particularly after TO Treatment and Its Increase was Totally Reversed in the IL-6KO Strain
The mitochondrial SOD-2, together with EPO, has recently been identified as being one of the HIF-2α target genes. We observed a significant upregulation of SOD-2 gene with a peak of 3.4±0.5-fold at 12 h after TO treatment in the wild-type animals (Figure 18a). No significant changes were observed in the IL-6KO group. The LPS-treated mice showed a lower augment in SOD-2 transcript number and the peak of 2.5-fold registered in the wild-type group at 4 h preceded the one described for the IL-6KO group at 6 h without significant changes of expression (Figure 18b).
SOD-2 mRNA hepatic expression in wild-type and IL-6KO mice after TO administration (a) and LPS treatment (b). The relative expression was normalized using β-actin as housekeeping gene. Similar to the EPO gene kinetics in the TO model, the expression of SOD-2 gene was significantly upregulated at 6 h after the injury to reach a peak of 3.4±0.5-fold in the wild-type animals, whereas no significant changes are detectable (a). A different cellular and molecular pattern triggered by LPS administration reflects a different kinetic of expression with an increment of RNA transcripts up to 2.5±0.5-fold increase at 4 h in the wild-type group and up to 2.3±0.1-fold increase at 6 h in the IL-6KO group (b). Results are expressed as mean±s.d. *Values significantly different compared with the control group (P<0.05, **P<0.01 analyzed by Student's t-test, N=3).
DISCUSSION
We recently reported that during acute-phase reaction the hematic EPO concentration increases in parallel to an upregulation of the hepatic mRNA EPO gene expression.27 In this work our aim was to investigate the mechanisms regulating EPO gene expression in the same normoxic conditions through a comparison of two models of acute-phase reaction. In addition, we analyze the acute-phase effects on EPO gene expression in the absence of IL-6, a critical regulatory acute-phase cytokine. The EPO mRNA increases in the liver during APR with results detectable between 6 and 12 h after the injections in parallel to an augmented activity of the two main transcription factors involved in EPO gene induction, HIF-1α and HIF-2α. Interestingly, the lack of IL-6 did not influence HIF-2α protein expression but HIF-1α mRNA expression was strongly reduced and the hepatic gene expression and serum concentration of EPO dramatically declined in the IL-6KO mice after the insults. The stimulation of isolated mouse hepatocytes with several concentrations of IL-6 revealed an upregulation of EPO gene expression and an induction of protein synthesis and release, showing a direct regulative function of this important acute-phase cytokine.
Although the persistence of a proinflammatory environment has been shown to be often associated with the development of anemic conditions,28 a growing body of clinical and experimental studies supports a possible direct correlation between IL-6 and EPO plasma levels. In a clinical study, Elliot et al6 reported a significant correlation between a sudden increase of EPO levels and IL-6 serum concentrations in patients affected by inflammatory diseases with or without acute renal failure. Subsequently, a similar analysis was performed by Ferrucci et al29 who described a ‘preanemic’ state characterized by a compensatory increment of EPO to maintain normal hemoglobin levels in patients undergoing proinflammatory states. Furthermore, in a previous work by Abel et al,5 the pattern of serum EPO levels was recorded in parallel to that of acute-phase proteins, IL-6 above all, in patients with sepsis.
The hepatic contribution up to a 40% of the total EPO has also been clearly shown in rats whereas in mice and sheep the hepatic contribution of the total body EPO production has been shown to reach only 15–20% in hypoxic conditions.30 This species-specific difference could explain a delay in the hepatic EPO mRNA increase observed among rats and mice after an acute-phase stimulus. Clinically and biologically, every single patient and every individual develops quantitatively and qualitatively different responses depending on the clinical setting that characterizes their physiopathological condition. The use of two models of acute-phase reaction, TO injection (aseptic) and LPS administration (septic), allowed us not only to monitor the circulating levels of EPO as a simulation of two clinical conditions, but also to analyze in vivo the possible mechanisms involved in gene regulation under these specific conditions. To the best of our knowledge, most of the studies concerning EPO synthesis and regulation have been focused on hypoxic experimental conditions and within the kidney compartment. Although the central role of the liver in the regulation of acute-phase mediators and in the reorganization of the iron storage after injury has been deeply investigated,31, 32 however the EPO synthesis and production during acute-phase reaction and its regulatory mechanisms are still poorly understood.
Proinflammatory cytokines, like IL-1β and TNF-α, have been shown to inhibit EPO expression in vitro and in some experimental animal models, as widely reviewed by Jelkmann.33 Interestingly, these proinflammatory cytokines were capable of inducing HIF-1α, discrediting the hypothesis that impaired hypoxic signaling is responsible for the repression of EPO gene activity. Most of the in vivo studies performed till today focused mainly on the inhibitory effects of these cytokines on kidney EPO expression under hypoxic conditions.34, 35 The analysis of two models characterized by the activation of several hepatic cell populations and the distinct pattern of acute-phase mediators, and the use of an IL-6KO mice strain offered us the possibility to better investigate mechanisms involved in the regulation of EPO in an in vivo situation under physiologic oxygen concentrations. This analysis could suggest reasonable explanations according to which several inflammatory mediators, such as nitric oxide, have been shown to inhibit or induce EPO gene expression under hypoxic and normoxic conditions, respectively.36
The regulation of EPO gene expression during hypoxia has been widely explained,37 but several points concerning the tissue-specific EPO gene expression and the after-birth switch between the fetal hepatic production and the adult kidney counterpart still need further clarifications. The HIF transcription factor family has been initially identified as the most important regulator of EPO genes under hypoxia and in the adult kidney,38 but the specific involvement of the single members of this transcription family in direct gene regulation is still an opened question.39 HIF activation influences genes that are fundamental in iron metabolism and other pathways that facilitate an efficient erythropoiesis.40 Indeed, as recently reviewed by Semenza,41 HIF-1α controls the absorption and delivery of iron to the bone marrow, a process mediated through the regulation of at least five gene products (EPO, EPOR, hepcidin, transferrin and transferrin receptor) and involving five organs (kidney, liver, intestine, blood and bone marrow).
Recently, Rankin et al,42 with the use of conditional gene inactivation and von Hippel–Lindau tumor-suppressor-deficient mice, showed that HIF-2α seems to have a crucial role in the induction of the hepatic EPO in anemic mice. Moreover, their work showed that HIF-1α and HIF-2α can activate simultaneously distinct target genes with different functions regarding the regulation of hypoxia-related genes. In our two models of acute-phase reaction, we also observed a hepatic increase of both members' protein levels as shown with western blot and histological analyses, although only HIF-1α mRNA was upregulated. In addition, the supershift analysis revealed a possible involvement of both transcription factor members, suggesting a contemporary activation in the same pathologic conditions. The identification with immunofluorescence revealed a dominant positivity for HIF-1 in hepatocytes and isolated clusters of KCs, whereas HIF-2α was dominantly expressed in endothelial cells and possibly fibroblast-like cells, with a weaker nuclear induction of protein levels in hepatocytes during inflammation. Interestingly, Rankin et al performed their study in PEPCK-Cre transgenic mice, a gene that is also expressed in extraparenchymal cell populations such as KCs (data not shown). These observations support two concepts that invite future investigation: the possible involvement of the macrophage compartment in the production of EPO and a cell-specific balance between transcription factors that, according to the cellular microenvironment, might induce or silence the expression of the same gene. Further studies will aim to establish an effective role of the single hepatic extraparenchymal populations in the contribution of EPO production on stimulation with acute-phase cytokines. A significant correlation is emerging between HIF members and transcription factors involved in the initiation of the innate immunity. On the basis of the work by Rius et al43 and Bracken et al,44 introducing an essential association between HIF-1α and HIF-2α with the transcription factors family NF-κB, Taylor elegantly reviewed an interconnection between these transcription factors in a multifactorial complex mechanism.45 HIF-1α has also been shown to become activated in macrophages after LPS challenge in a TLR4-dependent manner and to participate in the promotion of the production of proinflammatory cytokines in the early stages of sepsis.46 Notably, the hepatocyte nuclear factor (HNF)-4 has been shown to be crucial for the tissue specificity of EPO gene expression, particularly in the liver where a there is a binding sequence flanking the hypoxia-responsive element in the EPO gene promoter.47 Recently, HNF-4 has been described as an important regulator of the APR acting as an activator of CrebH.48
From the results obtained in our work there emerged a crucial role for IL-6 in the production of EPO in hepatocytes during APR and in hepatic HIF-1α mRNA upregulation. Although HIF-2α increased in both models, no evident correlation with IL-6 was observed. As NF-κB has been presented as a tight regulator of HIF-2α,49 the cell-specific localization and the potential role of this transcription factor as a redox-sensible protein might indicate an activation of HIF-2α on reactive oxygen-mediated signaling. Under hypoxic conditions, characterized by dramatic alteration of the mitochondrial respiration and a massive release of oxygen-reactive species, the transcription factor balance might decline in favor of HIF-2α-dependent gene regulation. Curiously, a deeper insight into the mechanisms of HIF-2α transcription regulation described by Dioum et al16 indicates a deacetylation process operated by the NAD+-dependent deacetylase sirtuin1 (SIRT-1) as a crucial step in the enhancement of its transcription activity. Congenital Sirt1 deficiency affects fetal and adult EPO gene expression in mice50 and RNA interference of endogenous SIRT-1 reduced the expression of the liver EPO gene, whereas the overexpression of both SIRT-1 and HIF-2α further augments hepatic EPO gene expression even in normoxic condition. In this work we recorded an increase of SIRT-1 expression related to HIF-2α, particularly evident in the TO-treated animals, in which EPO gene expression was higher compared to the LPS-treated animals. Interestingly, in the IL-6KO mice, SIRT-1 expression did not change in spite of an HIF-2α augment not unlike the wild-type strain. Indeed, SOD-2, another gene supposed to be regulated also through HIF-2α and upregulated in parallel to EPO in the wild-type groups, showed no induction in the IL-6KO mice after TO administration. In vitro SiRT-1 has been shown to be activated in response to growth factor deprivation and increased oxidative stress.51 Moreover, SIRT-1 has been described as protecting against metabolic, genotoxic and heat stress by deacetylating key transcription factors responding to these stressors.52 Considering the actual rediscovered biological properties of EPO beyond the erythroid lineage-induced proliferation, like prosurvival and antioxidant protective effects,53 it could be interesting to speculate on a functional protective correlation between SIRT-1 expression and EPO in response to stressful conditions, such as acute-phase reaction.
In summary, the results of our study indicate an increase of EPO circulating levels in two models of APR, although with different kinetic and levels of expression. Importantly, IL-6KO mice subjected to the same experimental models showed a dramatically reduced gene expression and lower EPO serum concentrations compared to the wild-type groups, regardless of the activation of the HIF transcription factor members. The comparison between two models of acute response triggering with different pathways of signaling also showed a possible cell-specific EPO gene regulation in distinct physiopathological settings. A detailed analysis of the protein regulating EPO production suggested that the pattern of mediators released during APR and during different oxygen concentration environments might influence the balance of the transcription involved in EPO gene regulation within the heterogenic cell population of the liver. Hepatocytes, the main cell population orchestrating the acute-phase reaction, may represent the major producers of EPO through a direct IL-6 regulation. A contribution from other cell populations might come following a disruption of the cellular redox balance characterizing the inflammatory process and acting on other transcription factors, such as HIF-2α. The identification of a key role for IL-6 in the regulation of EPO gene expression during acute-phase reaction might contribute further to the understanding of the hypoxia-related immune response.
References
Ramadori G, Christ B . Cytokines and the hepatic acute-phase response. Semin Liver Dis 1999;19:141–155.
Lotze MT, Zeh HJ, Rubartelli A, et al. The grateful dead: damage-associated molecular pattern molecules and reduction/oxidation regulate immunity. Immunol Rev 2007;220:60–81.
Jelkmann W . Erythropoietin after a century of research: younger than ever. Eur J Haematol 2007;78:183–205.
Brines M, Cerami A . Erythropoietin-mediated tissue protection: reducing collateral damage from the primary injury response. J Intern Med 2008;264:405–432.
Abel J, Spannbrucker N, Fandrey J, et al. Serum erythropoietin levels in patients with sepsis and septic shock. Eur J Haematol 1996;57:359–363.
Elliot JM, Virankabutra T, Jones S, et al. Erythropoietin mimics the acute phase response in critical illness. Crit Care 2003;7:R35–R40.
Semenza GL, Agani F, Iyer N, et al. Regulation of cardiovascular development and physiology by hypoxia-inducible factor 1a. Ann NY Acad Sci 1999;874:262–268.
Semenza GL, Wang GL . A nuclear factor induced by hypoxia via de novo protein synthesis binds to the human erythropoietin gene enhancer at a site required for transcriptional activation. Mol Cell Biol 1992;12:5447–5454.
Ivan M, Kondo K, Yang H, et al. HIFα targeted for VHL-mediated destruction by proline hydroxylation: implications for O2 sensing. Science 2001;292:464–468.
Wiesener MS, Jurgensen JS, Rosenberger C, et al. Widespread hypoxia-inducible expression of HIF-2α in distinct cell population of different organs. FASEB J 2003;17:271–273.
Semenza GL . Hypoxia-inducible factor 1: oxygen homeostasis and disease pathophysiology. Trends Mol Med 2001;7:345–350.
Ryan HE, Lo J, Johnson RS . HIF-1alpha is required for solid tumor formation and embryonic vascularisation. EMBO J 1998;17:3005–3015.
Zhou J, Brune B . Cytokines and hormones in the regulation of hypoxia-inducible factor-1alpha (HIF-1alpha). Cardiovasc Hematol Agents Med Chem 2006;4:189–197.
Jung JE, Kim HS, Lee CS, et al. STAT3 inhibits the degradation of HIF-1alpha by pVHL-mediated ubiquitination. Exp Mol Med 2008;40:479–485.
Van Uden P, Kenneth NS, Rocha S . Regulation of hypoxia-inducible factor-1α by NF-κB. Biochem J 2008;412:477–484.
Dioum EM, Chen R, Alexander MS, et al. Regulation of hypoxia-inducible factor 2α signalling by the stress-responsive deacetylase sirtuin-1. Science 2009;324:1289–1293.
Sheikh N, Dudas J, Ramadori G . Changes of gene expression of iron regulatory proteins during turpentine oil-induced acute-phase response in the rat. Lab Invest 2007;87:713–725.
Fantuzzi G, Zheng H, Faggioni R, et al. Effect of endotoxin in IL-1 beta-deficient mice. J Immunol 1996;157:291–296.
Mihov D, Vogel J, Gassmann M, et al. Erythropoietin activates nitric oxide synthase in murine erythrocytes. Am J Physiol Cell Physiol 2009;297:C378–C388.
Pregi N, Wenker S, Vittori D, et al. TNF-alpha-induced apoptosis is prevented by erythropoietin treatment on SH-SY5Y cells. Exp Cell Res 2009;315:419–431.
Tron K, Samoylenko A, Musikowski G, et al. Regulation of rat heme oxygenase-1 expression by interleukin-6 via the Jak/STAT pathway in hepatocytes. J Hepatol 2006;45:72–80.
Rankin EB, Higgins DF, Walisser JA, et al. Inactivation of the arylhydrocarbon receptor nuclear translocator (Arnt) suppresses von Hippel–Lindau disease-associated vascular tumors in mice. Mol Cell Biol 2005;25:3163–3172.
Chua ACG, Olynyk JK, Leedman PJ, et al. Nontransferrin-bound iron uptake by hepatocytes is increased in the Hfe knockout mouse model of hereditary hemochromatosis. Blood 2004;104:1519–1525.
Knook DL, Blansjaar N, Sleyster EC . Isolation and characterization of Kupffer and endothelial cells from the rat liver. Exp Cell Res 1977;109:317–329.
Armbrust T, Nordmann B, Kreissig M, et al. C1q-synthesis by tissue mononuclear phagocytes from normal and from damaged rat livers: upregulation by dexamethasone and downregulation by interferon gamma and lipopolysaccharide. Hepatology 1997;26:98–106.
Elmaouhoub A, Dudas J, Ramadori G . Kinetics of albumin- and alpha-fetoprotein-production during rat liver development. Histochem Cell Biol 2007;128:431–443.
Ramadori P, Sheikh N, Ahmad G, et al. Hepatic changes of erythropoietin gene expression in a rat model of acute-phase response. Liv Int 2010;30:55.
Adamson JW . The anemia of inflammation/malignancy: mechanisms and management. Hematology Am Soc Hematol Educ Program Book. Jan 2008; 2008:159–165.
Ferrucci L, Guralnik JM, Woodman RC, et al. Proinflammatory state and circulating erythropoietin in persons with and without anemia. Am J Med 2005;118:1288.e11–1288.e19.
Weidemann A, Johnson RS . Nonrenal regulation of EPO synthesis. Kid Int 2009;75:682–688.
Ramadori G, Armbrust T . Cytokines in the liver. Eur J Gastroenterol Hepatol 2001;13:777–784.
Verga Falzacappa MV, Vujic Spasic M, Kessler R, et al. STAT3 mediates hepatic hepcidin expression and its inflammatory stimulation. Blood 2007;109:353–358.
Jelkmann W . Proinflammatory cytokines lowering erythropoietin production. J Interferon Cytokine Res 1998;18:555–559.
Frede S, Fandrey J, Pagel H, et al. Erythropoietin gene expression is suppressed after lipopolysaccharide or IL-1β injections in rats. Am J Physiol 1997;273:R1067–R1071.
Faquin WC, Schneider TJ, Goldberg MA . Effect of inflammatory cytokines on hypoxia-induced erythropoietin production. Blood 1992;8:1987–1994.
Brüne B, Zhou J . Nitric oxide and superoxide: interference with hypoxic signalling. Cardiovasc Res 2007;75:275–282.
Ebert BL, Bunn HF . Regulation of the erythropoietin gene. Blood 1999;94:1864–1877.
Bracken CP, Whitelaw ML, Peet DJ . The hypoxia-inducible factors: key transcriptional regulators of hypoxic responses. Cell Mol Life Sci 2003;60:1376–1393.
Ratcliffe PJ . HIF-1 and HIF-2: working alone or together in hypoxia? J Clin Invest 2007;117:862–865.
Semenza GL . Expression of hypoxia-inducible factor 1: mechanisms and consequences. Biochem Pharmacol 2000;59:47–53.
Semenza GL . Involvement of oxygen-sensing pathways in physiologic and pathologic erythropoiesis. Blood 2009;114:2015–2019.
Rankin EB, Biju MP, Liu Q, et al. Hypoxia-inducible factor-2 (HIF-2) regulates hepatic erythropoietin in vivo. J Clin Invest 2007;117:1068–1077.
Rius J, Guma M, Schachtrup C, et al. NF-kappaB links innate immunity to the hypoxic response through transcriptional regulation of HIF-1alpha. Nature 2008;453:807–811.
Bracken CP, Whitelaw ML, Peet DJ . Activity of hypoxia-inducible factor 2alpha is regulated by association with the NF-kappaB essential modulator. J Biochem Chem 2005;280:14240–14251.
Taylor CT . Interdependent roles for hypoxia inducible factor and nuclear factor-kappaB in hypoxic inflammation. J Physiol 2008;586 (Part 17):4055–4059.
Peyssonnaux C, Cejudo-Martin P, Doedens A, et al. Cutting edge: essential role of hypoxia inducible factor-1alpha in development of lipopolysaccharide-induced sepsis. J Immunol 2007;178:7516–7519.
Galson DL, Tsuchiya T, Tendler DS, et al. The orphan receptor hepatic nuclear factor functions as a transcriptional activator for tissue-specific and hypoxia specific erythropoietin gene expression and is antagonized by EAR3/COUP-TF1. Mol Cell Biol 1995;15:2135–2140.
Luebke-Wheeler J, Zhang K, Battle M, et al. HNF-4α is implicated in ER stress induced acute phase response by regulating expression of CrebH. Hepatology 2008;48:1242–1250.
Bracken CP, Whitelaw ML, Peet DJ . Activity of hypoxia-inducible factor 2α is regulated by association with the NF-kappaB essential modulator. J Biol Chem 2005;280:14240–14251.
Denu JM . Linking chromatin function with metabolic networks: Sir2 family of NAD(+)-dependent deacetylases. Trends Biochem Sci 2003;28:41–48.
Luo J, Nikolaev AY, Imai S, et al. Negative control of p53 by Sir2alpha promotes cell survival under stress. Cell 2001;107:137–148.
Gorospe M, de Cabo R . AsSIRTing the DNA damage response. Trends Cell Biol 2008;18:77–83.
Maiese K, Hou J, Chong ZZ, et al. Erythropoietin, forkhead proteins, and oxidative injury: biomarkers and biology. ScientificWorldJournal 2009;9:1072–1104.
Acknowledgements
We thank Mrs Sandra Georgi, Anke Herbst and Elke Neumann for their kind and skillful technical assistance. This work was supported by grants from the Deutsche Forschungsgemeinschaft SFB 402 TP C6, C7, D3 and GRK 335.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Laboratory Investigation website
Supplementary information
Rights and permissions
About this article
Cite this article
Ramadori, P., Ahmad, G. & Ramadori, G. Cellular and molecular mechanisms regulating the hepatic erythropoietin expression during acute-phase response: a role for IL-6. Lab Invest 90, 1306–1324 (2010). https://doi.org/10.1038/labinvest.2010.85
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.2010.85