Abstract
Fibroblasts act as important immune regulatory cells via their ability to cross-talk with T cells accumulating in lesions. Our previous study showed that fibroblasts produce several cytokines and chemokines by crosslinking HLA class II (HLA-II) molecules with monoclonal antibodies or by making T-cell receptor–peptide–HLA complexes. It is thus conceivable that the interaction of T cells and fibroblasts via HLA-II affects fibroblast responses to stimuli. This study used human gingival fibroblasts (HGF) to investigate possible effects of these fibroblast-derived soluble factors on the differentiation of naïve T cells and on the subsequent fibroblast responses. After mixed lymphocyte reaction culture between naïve T cells and allogeneic dendritic cells in the presence of culture supernatant from HGF stimulated via HLA-DQ molecules (DQ-sup), but not via DR, T cells exhibited a Th2-shifted phenotype, thereby producing quantitatively more IL-13 and IL-5 compared with interferon-γ. Astonishingly, analyses to identify possible factors affecting the Th2 polarization secreted from HLA-II-stimulated HGF, prostaglandin E2, was detected only in DQ-sup. The Th2 polarization of naïve T cells was blocked in the presence of supernatants from indomethacin-treated HGF with HLA-DQ stimulation. In addition, we found that the culture supernatants of Th cells activated following mixed lymphocyte reaction culture in the presence of DQ-sup had the potential to induce gene expression of type I and III collagens in HGF. These results suggested that fibroblasts stimulated via HLA-DQ molecules promote Th2 polarization in Th-cell responses and showed the counter activation of collagen synthesis, implicating orchestrated responses among these cells in the fibrosis of chronic inflammatory lesions.
Similar content being viewed by others
Main
Fibroblasts that accumulated at the site of tissue damage during chronic inflammation have a significant role in tissue repair by synthesizing extracellular matrix. In addition to this remodeling of connective tissues, recent reports also implicate an important and more direct role for fibroblasts in the immune system. Stimulated by invading microorganisms and/or other environmental factors, including inflammatory cytokines, fibroblasts produce various other cytokines, including IL-1, IL-6, IL-8, monocyte chemoattractant protein 1 (MCP-1; CCL-2), and prostaglandins.1, 2, 3, 4, 5, 6, 7 It is postulated that these fibroblast-derived products might help in conditioning the cytokine environment around inflammatory sites to promote the accumulation of hematopoietic cells, including neutrophils, monocyte/macrophages, dendritic cells (DCs), T cells, B cells, and plasma cells, which in turn act to regulate the immune response.
Many proteins expressed on the fibroblast surface are involved in regulating hematopoietic cells. Class II HLA (HLA-II) is one such molecule that signals to CD4+ helper T cells (Th cells) and whose expression is upregulated by interferon-γ (IFN-γ).8 In general, HLA-II molecules are expressed on antigen-presenting cells (APCs) to activate Th cells via the T-cell receptor(TCR)/antigenic peptide complex. Recent studies showed that HLA-II also acts as a receptor for signaling APCs to stimulate cytokine production.9, 10 We previously showed that fibroblasts secrete several cytokines, such as regulated upon activation, normal T cells expressed and secreted (RANTES), MCP-1, IL-8, and IL-6, when HLA-II molecules on the fibroblast surface are crosslinked with monoclonal antibodies (mAbs) or when a complex is formed comprising antigenic peptides, TCRs, and HLA-II molecules.11 As proliferative responses of T-cell clones were not observed in the co-culture system with antigen-presenting fibroblasts in that study, we proposed that HLA-II molecules expressed on the cell surface of fibroblasts act chiefly as receptor molecules to induce the cells to produce soluble factors, including cytokines and chemokines, rather than as antigen-presenting molecules to activate T cells. It is therefore likely that products from fibroblasts activated by HLA-II signaling would also regulate Th-cell activation and differentiation in response to antigenic peptides presented by APCs including DCs. These products might then in turn induce biological effects on fibroblasts. We hypothesized that such cellular responses to HLA-II signaling could influence the outcome of inflammatory responses stimulated at sites of injury.
DCs are the most potent APCs in terms of antigen-specific T-cell responses. DCs also contribute to the differentiation path of naïve T cells by developing themselves into functional DC phenotypes.12 This differentiation of DCs is regulated by a variety of extracellular factors, including cytokines, chemokines, and glycolipids,13, 14, 15 secreted from many kinds of cells located in the antigen-presenting environment. Products from fibroblasts activated by crosslinking HLA-II molecules are therefore possible factors affecting the development of DCs and the subsequent differentiation of naïve T cells.
This study examined the effects of products from human gingival fibroblasts (HGF) activated by crosslinking HLA-II molecules on Th-cell response and differentiation. To do this, we evaluated the Th-cell cytokine profile of culture supernatants using an in vitro model system following an allogeneic mixed lymphocyte reaction (MLR) between naïve T cells and DCs in the presence of products from HGF with or without HLA-II stimulus. We also assessed consecutive effects of differentiated Th cells after MLR culture in the presence of products of HLA-II-stimulated HGF.
MATERIALS AND METHODS
Antibodies
mAbs L243 (mouse anti-HLA-DR; Leinco Technologies, Ballwin, MO, USA) and 1a3 (anti-HLA-DQ; Leinco Technologies) were used to transduce signals into HGFs via HLA-DR and HLA-DQ, respectively. Isotype-matched control mouse IgG2a antibodies were obtained from Pharmingen (San Diego, CA, USA). Hit3a (mouse anti-human CD3; Pharmingen) and CD28.2 (mouse anti-human CD28; Pharmingen) were used as inducing mAbs for nonspecific T-cell activation.
Cells
Gingival fibroblasts
HGFs were isolated from three healthy volunteers’ gingival tissues (three males; age: 33.0±2.2 years), plated initially on 35-mm cell culture dishes pre-coated with type I collagen and fibronectin. Outgrown cells from tissue explants were expanded and maintained as described previously.16 Briefly, the cells were cultured in Dulbecco's modified Eagle's medium supplemented with 10% fetal bovine serum, 10 mg/ml gentamicin, 0.1 mM non-essential amino acids, vitamins, and 2 mM L-glutamine. Confluent cells were passaged with a split ratio of 1:4. All experiments were carried out while these cells were actively growing at passages 5–8.
Dendritic cells
Peripheral blood mononuclear cells (PBMC) were isolated from the buffy-coat fraction of anticoagulated blood samples by using the Ficoll-Paque (GE Healthcare Bio-Science Corp, Piscataway, NJ) gradient solution method. Four anonymized blood samples were kindly gifted from the Japanese Red Cross Society as redundant materials to blood transfusion. CD14+ cells were purified from PBMC using the MACS CD14 isolation kit (Miltenyi Biotec, Bergisch Gladbach, Germany). The CD14+ cells were cultured for 5 days in the presence of 50 ng/ml rGM-CSF (NCPC-GeneTech, Heibei, China) and 50 ng/ml rIL-4 (Osteogenetics Gmbh, Wuerzburg, Germany) to generate monocyte-derived immature DCs. To determine the effect of the HGF culture supernatants on DC maturation, immature DCs were re-stimulated with 50 ng/ml tumor necrosis factor-alpha (TNF-α) (PeproTech, London, UK) for 2 days as a maturation factor, in the presence or absence of the HGF culture supernatants.
Naïve CD4+ T cells
Naïve T cells were isolated from PBMC by negative selection using StemSep human naïve CD4+ T-cell enrichment kit (StemCell Technologies, Vancouver, BC, Canada) according to the manufacturer’s instructions after elimination of CD14+ cells. The naïve T-cell-enriched fraction contained >95% CD45RA-positive cells as determined by flow cytometry.
Informed consent was obtained from all donors, and the protocol was approved by the Human Ethics Committee of Hyogo College of Medicine.
Preparation of HGF Culture Supernatants Following the HLA-II Stimulus
Culture supernatants of HGF stimulated via HLA-DR (DR-sup) or -DQ molecules (DQ-sup) were collected following 16 h of HGF culture in the presence of L243 or 1a3 mAb, respectively. The control HGF cultures contained isotype-matched mouse control Ab. Before culturing with the anti-HLA mAbs, HGFs were cultured for 72 h with or without 500 U/ml IFN-γ (Genzyme, Cambridge, MA, USA), followed by serum-free medium for 24 h for serum starvation. The collected supernatants were then depleted of anti-HLA-II mAbs and mouse control Ab by incubation with sheep anti-mouse IgG Ab-conjugated magnetic beads and Dynabeads M-280 sheep anti-mouse IgG (Invitrogen, Carlsbad, CA, USA) for 3 h. Experiments in which indomethacin was used to block the synthesis of cyclooxygenase metabolites used 1 μM indomethacin (Sigma, St Louis, MO, USA).
Allogeneic MLR
Naïve T-cell differentiation was evaluated according to the Th-cell cytokine profiles following the allogeneic MLR. Briefly, DCs stimulated with or without the HGF culture supernatants in the presence of TNF-α were co-cultured with HLA-II-non-shared allogeneic naïve T cells to induce MLR, resulting in the activation of naïve T cells (DCs to T cells=1:10). After 7 days of culture in the presence or absence of DR-sup or DQ-sup, T cells were collected and re-stimulated with anti-CD3 and anti-CD28 agonistic mAbs to induce nonspecific T-cell activation. After an additional 16-h culture, supernatants were collected and assayed for selected cytokines.
Measurement of Cytokines and Prostaglandin E2
Specific solid-phase sandwich ELISA systems were used to measure IFN-γ and IL-13 titers with commercial pairs of capture and detection antibodies as follows: M700A and M701B for IFN-γ, or P130E and M130B for IL-13 (Pierce Biotechnology, Rockford, IL, USA). IL-5 titer was assayed using the IL-5 DuoSet ELISA Development kit (R&D Systems, Minneapolis, MN, USA) according to the manufacturer's instructions. Prostaglandin E2 (PGE2) production from HGF with or without the HLA-II stimulus was measured using Prostaglandin E2 enzyme immunoassay kits (Assay Designs, Ann Arbor, MI, USA). RANTES and MCP-1 productions from HGFs were measured by using the RANTES DuoSet ELISA Development kit (R&D Systems) and Quantikine human CCL2/MCP-1 immunoassay (R&D Systems). Supplementary Information available on Laboratory Investigation's website shows the amounts of cytokines used in the experiments.
Quantitative Real-Time Reverse Transcription-PCR Measurement of Gene Expression
The HGF lines in 398-well plates were evaluated for type I and III collagen synthesis by real-time PCR, using the ABI Prism 7900 Sequence Detection System (Applied Biosystems, Foster City, CA, USA) and according to the manufacturer's instructions. Two-step reverse transcription (RT)-PCR was performed using dilutions of first-strand cDNA in a final concentration of 1 × Assays-On-Demand and 1 × TaqMan Universal PCR Master Mix (Applied Biosystems). First-strand cDNA was synthesized with 1 μg of total RNA derived from HGF cultured with or without the supernatants of the MLR between T cells and DCs. Total cellular mRNA was extracted from HGF using TRIZOL Reagent (Invitrogen) according to the manufacturer's protocol. TaqMan probes and primers for COL1A1 (Hs01076777_m1), COL3A1 (Hs00164103_m1), IL13RA2 (Hs00152924_m1), TGFB1 (Hs00998133_m1), and GAPDH (4326317E) were provided in the Assay-on-Demand gene expression kit (Applied Biosystems). Triplicate RT-PCR reactions were prepared for each sample. The point at which the PCR product was first detected above a fixed threshold, termed the cycle threshold (Ct), was determined for each sample, and the average Ct of triplicate samples was calculated. The relative expression of type I and III collagens, IL-13RA2, and TGF-β mRNA was normalized to the amount of GAPDH in the same cDNA using the ΔCt method. The ΔCt value is determined by subtracting the average GAPDH Ct value from the average COL1A1, COL3A1, IL13RA2, and TGFB1 Ct values, respectively.
Western Blot Analysis
HGFs were cultured for 18 h with the supernatants of Th cells activated after MLR culture in the presence of DR-sup, DQ-sup, or Cont-sup. The HGF culture supernatants were then harvested and analyzed by western blotting to assess the protein synthesis of type I and type III collagens. Briefly, the culture supernatants of HGFs were centrifuged at 13 000 g for 10 min, and the amounts of total protein were quantitated using the Bradford protein assay (Bio-Rad Laboratories, Richmond, CA, USA). Equal protein amounts (7.5 μg) were subjected to SDS-PAGE under reducing conditions, followed by electrophoretic transfer to nitrocellulose membrane for immunoblotting. Membranes were blocked with 5% non-fat dry milk in PBS containing 0.1% Tween-20 overnight, and then incubated with antibody against human type I collagen (COL1A1 (H-197); Santa Cruz Biotechnology, Santa Cruz, CA, USA) or type III collagen (Rockland Immunochemicals, Gilbertsville, PA, USA). The membranes were then incubated with horseradish peroxidase-linked secondary antibody (Santa Cruz Biotechnology) and antibody binding was subsequently visualized by chemiluminescence (ECL reagent; Amersham Biosciences, Tokyo, Japan) according to the manufacturer's recommendations.
Statistical Analysis
The multiple comparison procedure following a significant F-test of ANOVA was used to determine significant difference among the multigroup data. Student's t-test was used for comparing data between groups. P-values <0.05 were considered as significant.
RESULTS
The Expression of HLA II Molecules on HGF
We first estimated the expression levels of HLA-DR and -DQ in HGF cell lines established from three different donors by flow cytometry, and found no significant difference among them. The comparison of DR and DQ expression levels revealed that DR molecules were more highly expressed than DQ molecules. As reported previously,8, 17 HLA-DR was upregulated on HGF in the presence of IFN-γ. In contrast, DQ expression on HGF remained constant regardless of the pretreatment with IFN-γ (Figure 1)
Expression of HLA-DR and HLA-DQ molecules on HGF stimulated with or without IFN-γ. Cell surface expression of HLA-DR and HLA-DQ molecules (open histograms) by HGF were analyzed by immunostaining followed by flow cytometry analysis. HGFs were treated with (solid lines) or without (dotted lines) IFN-γ at 200 U/ml for 72 h. Basal fluorescence levels are indicated by shaded area when cells were stained with isotype-matched nonspecific IgG antibody. Representative data of two independent experiments from three donors are shown.
The Effect of Culture Supernatants of HGF Stimulated via HLA-II on Th-cell Polarization
The effect of incubating culture supernatants from HLA-II-stimulated HGF on the differentiation of naïve T cells was then tested. Cytokine profiles of activated T cells were analyzed after co-culturing with HLA-II-non-shared allogeneic DCs, namely the MLR cultures, in the presence of culture supernatants of HGF stimulated with anti-HLA-DR mAb (DR-sup), anti-DQ mAb (DQ-sup), or isozyme-matched control antibody (Cont-sup).
Before the MLR study, culture supernatants of HGF cell lines from three donors with or without HLA-II stimulus were assayed for the cytokines secreted from HLA-DR-stimulated periodontal ligament fibroblasts as reported in our previous study.11 RANTES, MCP-1, IL-8, and IL-6 were detected in both DR-sup and DQ-sup as shown previously, and each cytokine or chemokine concentrations was similar to our previous data11 (data not shown). There was little difference in the total amounts of these cytokines between DR-sup and DQ-sup in each HGF donor cell line tested in this study. However, no difference was detected in the profile of cytokines secreted by HGF stimulated via HLA-DR or -DQ molecules according to our commercially supplied cytokine array (Raibiotech, Norcross, GA, USA)18 (data not shown).
Naïve T cells co-cultured with allogeneic DCs in the presence of HGF culture supernatant from DQ-sup-stimulated, but not DR-sup-stimulated cells differentiated into cells able to produce high amounts of Th2-type cytokines, including IL-5 and IL-13, as compared with the Th1 cytokine, IFN-γ (Figure 2a). The ratios of IL-13 and IL-5 to IFN-γ tended to parallel the change in titers of the culture supernatants of HGF stimulated via HLA-II and contained in the MLR culture medium.
Cytokine production of activated Th cells following MLR culture with allogeneic DCs in the presence of soluble factors produced by HLA-II-stimulated HGFs. Naïve Th cells were cultured with allogeneic DCs (T cells/DC ratio 10:1) for 7 days. After the cellular expansion by MLR culture, Th cells were collected and re-stimulated with anti-CD3/CD28 mAbs for 2 days, and culture supernatants were harvested to determine IFN-γ, IL-5, and IL-13 concentrations by ELISA. The ratios of IL-13/IFN-γ and IL-5/IFN-γ were calculated and were indicated by the mean value±s.d. of triplicate cultures of one set of T-cell-DC-HGF. Soluble factors produced from HGF stimulated with HLA-II mAbs, including anti-DR (L243; shaded columns) and anti-DQ mAbs (1a3; closed column), or with isozyme-matched control antibodies (open columns) were diluted (final concentration: 1/2, 1/4, 1/8) and added into the MLR culture between DCs and Th cells (a) or the culture of DCs to induce maturation (b). Representative data of six independent experiments are shown (*P<0.05).
DCs have the unique ability to induce a primary immune response through activation and polarization of naïve T cells.19, 20, 21 It is therefore possible that the products of HLA-II-stimulated HGF might affect the development of DCs, with consequential implications for the differentiation of naïve T cells. Thus, we also examined cytokine levels in activated Th cells co-cultured with HLA-II-non-shared allogeneic DCs that were previously cultured with HGF supernatants during their maturation process. Naïve T cells co-cultured with allogeneic DCs matured in the presence of DQ-sup showed marked Th2 polarization relative to those co-cultured with DCs matured in the presence of DR-sup or Cont-sup (Figure 2b), which was similar to the results with co-cultured naïve T cells with DCs in the presence of HGF culture supernatants as shown in Figure 2a. These results suggested that products from HGF stimulated via HLA-DQ molecules act mainly on DC activation, thus skewing T cells toward the Th2 phenotype in a primary allogeneic response.
Identification of the Possible Factors Regulating T Cells and DCs Differentiation by HGF Stimulated via HLA-DQ Molecules
Although there was quite a difference between DR-sup and DQ-sup in the ability to induce Th2 polarization in Th cells after MLR culture, the cytokine profiles of these two supernatants were similar as we described previously.18 As PGE2 was recently implicated in promoting Th2 polarization in Th cells,22, 23 we next compared PGE2 production between HGF stimulated via HLA-DR and -DQ. Surprisingly, PGE2 was detected only in DQ-sup, but neither in DR-sup nor in the culture supernatant of HGF without stimulus, whereas the levels of secreted RANTES and MCP-1 did not differ between stimuli (Figure 3). PGE2 production from HGF stimulated via HLA-DQ was inhibited by the cyclooxygenase inhibitor indomethacin, whereas again, RANTES and MCP-1 production was similar between indomethacin-treated and -untreated HGF (Figure 3).
PGE2 and chemokine production by HLA-II-stimulated HGF. Fibroblasts were cultured in the presence (closed columns) or absence (shaded columns) of indomethacin and stimulated with anti-DR mAb (Indo-DR-sup and DR-sup), anti-DQ mAb (Indo-DQ-sup and DQ-sup), or isozyme-matched control Ab (Indo-Cont-sup and Cont-sup). The supernatants were collected following 16 h of culture after the stimulation to assay PGE2, RANTES, and MCP-1 by ELISA. Values are expressed as mean±s.d. from six HGF cultures established from three independent donors (*P<0.05).
We next examined the differentiation of naïve T cells co-cultured with allogeneic DCs in the presence of culture supernatants of indomethacin-treated HGF stimulated via HLA-DR (Indo-DR-sup) or HLA-DQ (Indo-DQ-sup). Th-cell polarization was also compared between culture supernatants of indomethacin-treated and -untreated HGF. As shown in Figure 4a, Th2 skewing was abrogated when DQ-sup was changed to Indo-DQ-sup. T-cell differentiation after MLR culture was similar between DR-sup and Indo-DR-sup. We also assessed the effects of these indomethacin-treated HGF supernatants on the activation of DCs during their maturation process from immature DC to mature DC. Naïve T cells co-cultured with DCs matured in the presence of Indo-DR-sup or Indo-DQ-sup showed similar Th2 polarization to that observed in co-cultures of Th cells with allogeneic DCs in the presence of Indo-DR-sup or Indo-DQ-sup (Figure 4b). Moreover, when PGE2 was added to Indo-DQ-sup, naïve T cells showed similar Th2 polarization to that observed in co-cultures of Th cells with allogeneic DCs in the presence of DQ-sup (Figure 4b).
Cytokine production of activated Th cells following MLR culture in the presence of soluble factors secreted from indomethacin-treated HGF. Naïve Th cells were cultured with allogeneic DCs (T cells/DC ratio 10:1) for 7 days. After the cellular expansion by MLR culture, Th cells were collected and re-stimulated with anti-CD3/CD28 mAbs for 2 days, and culture supernatants were harvested to determine IFN-γ, IL-5, and IL-13 concentrations by ELISA. The ratios of IL-13/IFN-γ and IL-5/IFN-γ were calculated and were indicated by the mean value±s.d. of triplicate cultures of one set of T-cell-DC-HGF. Soluble factors from indomethacin-treated (closed column) or -untreated (shaded column) HGFs, which were stimulated with anti-DR mAbs (Indo-DR-sup and DR-sup), anti-DQ mAb (Indo-DQ-sup and DQ-sup), or isozyme-matched control antibodies (Indo-Cont-sup and Cont-sup), were added into the MLR culture between DCs and Th cells (a) or the culture of DCs for the maturation process (b). Indo-DQ-sup supplemented with PGE2 (open column) was also added into both MLR culture systems (a, b). Final concentration of the supernatants in the culture medium was 1/2 in both experiments. Representative data of six independent experiments were shown (*P<0.05).
Thus, the regulation of Th2 polarization in Th cells could be partially attributed to the activation of DCs being affected by PGE2 produced from HGF stimulated via HLA-DQ.
The Effects of the Culture Supernatants of Th cells Activated by MLR in the Presence of DR- and DQ-Sup on HGF Activities in Collagen Synthesis
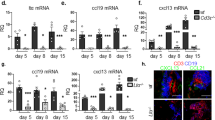
Recent studies showed that several cytokines produced by Th cells regulate extracellular matrix deposition by fibroblasts. Indeed, Th2-type cytokines such as IL-13 enhance collagen synthesis in fibroblasts, whereas Th1-type cytokines, especially IFN-γ, show the opposite effect.24, 25, 26 We therefore hypothesized that collagen synthesis in the HGF lines would be enhanced by the soluble products from Th cells activated in the presence of the HLA-II-stimulated HGF culture supernatant. To test this issue, we compared mRNA expressions of COL1A1 and COL3A1 among HGF lines cultured with several Th-cell culture supernatants after MLR with DR-, DQ-sup, or Cont-sup. After a 6-h culture, the expressions of COL1A1 and COL3A1 were significantly higher in HGF cultured with the Th-cell culture supernatants after MLR in the presence of the supernatants of HGF stimulated via HLA-II compared with Cont-sup (Figure 5a). In addition, Th-cell culture supernatants after MLR in the presence of DQ-sup induced higher mRNA expression of both COL1A1 and COL3A1 in HGF than in the presence of DR-sup. The evaluation of protein synthesis of type I and type III collagens in 18-h cultures of HGFs revealed results similar to the mRNA expression analysis of COL1A1 and COL3A1, respectively, in comparison with the effects of Th-cell culture supernatants after MLR in the presence of DR-, DQ-sup, or Cont-sup (Figure 5b).
Gene expression of HGF in the culture supernatants of activated Th cells following MLR culture in the presence of HLA-II-stimulated HGF. Cells were cultured with the supernatants of Th cells activated after MLR culture with allogeneic DCs in the presence of DR-sup, DQ-sup, or Cont-sup. After 6 h of culture, the gene expression levels of COL1A1 and COL3A1 (a), IL13RA2 (c), and TGFB1 (d) were evaluated by real-time RT-PCR. The results were expressed as relative gene expression values (*P<0.05). The protein synthesis of type I and type III collagens (b) was also evaluated by western blotting of the culture supernatants from HGFs incubated with Th-cell culture supernatants after MLR in the presence of DR-, DQ-, and Cont-sups for 18 h.
Moreover, the gene expressions of IL-13α2 receptor (IL13RA2) and TGF-β1 (TGFB1) were evaluated in HGF cultured with the supernatants of activated Th cells in the presence of DQ-sup compared with the supernatants of activated Th cells in the presence of DR-sup (Figure 5c), showing an elevation of IL13RA2 expression. However, we could not resolve the effects on the gene expression of TGFB1 (Figure 5d). Hence, these results suggested that the products from Th cells activated in the presence of the products from HLA-DQ-stimulated HGF are likely to induce collagen synthesis in HGF regardless of changes in the gene expression of TGFB1.
DISCUSSION
Many kinds of mesenchymal or epithelial bystander cells around immunological cells regulate the development of T cells27, 28, 29, 30, 31 and DCs32, 33, 34, 35, 36 via signals mediated by the soluble factors, and/or direct cell–cell contact resulting in cell ligations such as CD40-CD40L and ICAM-1-LFA-1. Previously, we reported that fibroblasts produce several cytokines such as RANTES, MCP-1, IL-6, IL-8, and the growth-related gene product following HLA-II stimulation.11, 18 These results suggested that fibroblasts stimulated thus might act in the recruitment of immunological cells and angiogenesis at sites of inflammatory lesions. Accordingly, this study estimated the effects of soluble factors from HLA-II-stimulated fibroblasts on the immunological responses mediated by Th cells. The findings revealed that some of these factors, especially from those cells stimulated via HLA-DQ signaling, skew Th cells toward the Th2 immune response. These results implicate fibroblasts stimulated via HLA-II molecules as potential regulators of Th-cell responses evoked in inflammatory lesions around fibrous tissues.
In this study, we focused on the soluble factor-mediated immunomodulatory effects of HLA-II-stimulated fibroblasts on the differentiation of naïve T cells during interactions between T cells and antigen-presenting DCs. Such factors, and DQ in particular, showed the potential to skew Th cells toward the Th2 immune response. Meanwhile, it is likely that naïve T-cell differentiations are also directly regulated via signaling induced by the ‘cell-to-cell’ contact between T cells and fibroblasts. However, since our previous studies showed no proliferative responses of T-cell clones in co-cultures with antigen-presenting fibroblasts, the T-cell differentiation seems to be chiefly affected by environmental changes mediated by soluble factors, such as cytokines and eicosanoids, and not via the ‘cell-to-cell’ contact of T cells with HLA-II-stimulated fibroblasts. Further studies are needed to confirm this hypothesis, including co-culture experiments among T cells, DCs, and fibroblasts by gathering the donors of these cells in a various matched and/or unmatched combination of HLA-II haplotypes. These additional experiments might also explain the significance of the HLA-II stimulus induced by several different molecules expressed on fibroblasts and involved in the cross-talk between T cells and fibroblasts.
DCs have a central role in inducing Th2-type responses in T cells. Several factors are likely to be involved in this process to enhance the Th2 response in an antigen nonspecific manner, the so-called Th2 adjuvant. For instance, PGE2 and PGE1 are reportedly powerful Th2 adjuvants.37 A possible mechanism by which PGE2 acts in this way lies in its ability to induce IL-12p40 subunit production in DCs, resulting in the production of monomeric and/or homodimeric p40 components to function as an antagonist against IL-12p70 activity.23 It has also been reported that PGE2 acts on CD4+ T cells directly to induce Th2 cytokines, such as IL-4 and IL-5, by inhibiting the production of Th1 cytokines, such as IFN-γ and IL-2.38, 39, 40 In this study, Th2 skewing of naïve T cells was observed in the co-cultures with allogeneic DCs in the presence of culture supernatants of HGFs stimulated via HLA-DQ molecules (DQ-sup). Similar results were also obtained when naïve T cells were co-cultured with allogeneic DCs cultured with DQ-sup during their TNF-α-dependent maturation process. From these results, we proposed that PGE2 included in the DQ-sup affected DCs rather than affecting T cells directly, thus inducing Th2 polarization of naïve T cells after co-culturing with allogeneic DCs. Recent studies have revealed that PGE2 also act on DCs to produce IL-23 and on T cells directly to induce Th17 differentiation of T cells.41, 42, 43, 44, 45 It is therefore likely that DQ-sup would also be implicated in the Th17 differentiation of T cells. Further studies would be needed to clarify these issues.
Soluble factors produced from HGF stimulated via HLA-DQ skewed naïve T cells toward Th2 immune responses. As the products from indomethacin-treated HGF stimulated via DQ showed no potential for Th2 skewing, we proposed PGE2 as the most likely factor involved in the Th2 polarization of Th cells. Other cytokines and chemokines produced by mesenchymal and/or epithelial cells have also been implicated in the immune response involving DCs and Th cells, one of which is thymic stromal lymphoprotein (TSLP).36 TSLP is a novel epithelial cell-derived cytokine with the reported potential to activate myeloid DCs, resulting in the polarization of naïve T cells toward Th2 cells.46, 47 As TSLP is also produced by activated synovial fibroblasts derived from patients with rheumatoid arthritis and osteoarthritis,48 it is likely that TSLP is partially involved in Th2 polarization of T cells mediated by products from HLA-DQ-stimulated HGF. In this study however, TSPL gene expression was not enhanced by supernatants from HLA-II-stimulated HGF (data not shown). As IFN-γ-treated HGFs were used in this study to increase HLA-II expression and because IFN-γ was reported to inhibit the TNF-α upregulation of TSLP expression in rheumatoid arthritis- and osteoarthritis-derived synovial fibroblasts,48 further studies will be needed to reveal the implications of TSLP in this issue, including experiments using IFN-γ-untreated HGF.
In this study, we showed that naïve T cells showed skewing toward Th2 following MLR culture with allogeneic DCs in the presence of DQ-sup, but not with DR-sup. A previous study revealed that T-cell lines showing proliferative responses in the context of HLA-DQ and -DP molecules exhibited Th2-shifted phenotypes compared with DR-restricted T-cell lines according to the distinct monokine profiles of monocytes activated via HLA-DR, -DQ, and -DP molecules.10 Intrinsically, HLA-DQ molecules are gene products of immune-suppression (Is) genes based on their role in immune suppression via antigen-specific immune responses at the cellular level.49 From this viewpoint, our results agreed with these previous findings and indicated that fibroblasts activated via HLA-DQ stimulus cooperate with monocytes to regulate antigen-specific Th-cell responses.
HGF cultured with the supernatants of activated Th cells following MLR culture with DR- or DQ-sup, especially DQ-sup, showed higher gene expression of COL1A1 and COL3A1. It is widely accepted that TGF-β1, IL-4, and IL-13 may act in the profibrotic mechanism. This idea was proposed by several experimental results in many disease models, such as hepatic fibrosis and pulmonary fibrosis.50, 51, 52, 53, 54 IL-4 and IL-13 exploit the same IL-4Ra/Stat6 signaling pathways55 to induce the incremental transcriptional activity of COL1A2 gene expression and type I collagen protein synthesis.56 In this study, as IL-4 was not detected in the supernatants of activated Th cells following MLR culture with DQ-sup (data not shown), IL-13 is found to be the most probable facilitator of collagen synthesis in fibroblasts. TGF-β1 is also a key cytokine in the mechanisms of fibrosis, whereby TGF-β1 production is induced by IL-13 stimulation via IL-13Rα2 in fibroblasts.57 In this study, HGF showed the incremental elevation of IL13RA2 gene expression in cells cultured with the supernatants of activated Th cells following MLR culture with DQ-sup; however, gene expression of TGFB1 was not elevated (Figure 5d). A previous study revealed the upregulation of TGFB1 transcriptional activity by IL-13 signaling via IL-13Rα2 only in the presence of TNF-α stimulation,57 suggesting that collagen synthesis might further progress in the presence of TNF-α, such as in the environment surrounding inflammatory lesions.
In conclusion, we have provided in vitro evidence of a reciprocal response between Th cells and fibroblasts via HLA-II signaling. This study showed that ligation of HLA-II molecules on HGF induced them to secrete chemoattractant factors against immune cells as well as Th2 polarization-promoting factors. Of all products produced from HGF, PGE2 could be a key player in the HLA-DQ-induced Th2 polarization. In addition, Th cells activated in the presence of products from HGF stimulated via HLA-DQ produce soluble factors to facilitate collagen synthesis. These observations might provide a basis for future therapeutic approaches in the management of diseases involving both Th cells and fibroblasts, such as rheumatoid arthritis, periodontitis, pulmonary inflammation, tuberculosis, and hepatic fibrosis.
References
Strieter RM, Phan SH, Showell HJ, et al. Monokine-induced neutrophil chemotactic factor gene expression in human fibroblasts. J Biol Chem 1989;264:10621–10626.
Larsen CG, Anderson AO, Oppenheim JJ, et al. Production of interleukin-8 by human dermal fibroblasts and keratinocytes in response to interleukin-1 or tumour necrosis factor. Immunology 1989;68:31–36.
Xing Z, Jordana M, Braciak T, et al. Lipopolysaccharide induces expression of granulocyte/macrophage colony-stimulating factor, interleukin-8, and interleukin-6 in human nasal, but not lung, fibroblasts: evidence for heterogeneity within the respiratory tract. Am J Respir Cell Mol Biol 1993;9:255–263.
Tamura M, Tokuda M, Nagaoka S, et al. Lipopolysaccharides of Bacteroides intermedius (Prevotella intermedia) and Bacteroides (Porphyromonas) gingivalis induce interleukin-8 gene expression in human gingival fibroblast cultures. Infect Immun 1992;60:4932–4937.
Tran CN, Lundy SK, White PT, et al. Molecular interactions between T cells and fibroblast-like synoviocytes: role of membrane tumor necrosis factor-alpha on cytokine-activated T cells. Am J Pathol 2007;171:1588–1598.
Ohta K, Shigeishi H, Taki M, et al. Regulation of CXCL9/10/11 in oral keratinocytes and fibroblasts. J Dent Res 2008;87:1160–1165.
Zhang Y, Cao HJ, Graf B, et al. CD40 engagement up-regulates cyclooxygenase-2 expression and prostaglandin E2 production in human lung fibroblasts. J Immunol 1998;160:1053–1057.
Pober JS, Collins T, Gimbrone Jr MA, et al. Lymphocytes recognize human vascular endothelial and dermal fibroblast Ia antigens induced by recombinant immune interferon. Nature 1983;305:726–729.
Matsuoka T, Kohrogi H, Ando M, et al. Altered TCR ligands affect antigen-presenting cell responses: up-regulation of IL-12 by an analogue peptide. J Immunol 1996;157:4837–4843.
Matsuoka T, Tabata H, Matsushita S . Monocytes are differentially activated through HLA-DR, -DQ, and -DP molecules via mitogen-activated protein kinases. J Immunol 2001;166:2202–2208.
Ohyama H, Nishimura F, Meguro M, et al. Counter-antigen presentation: fibroblasts produce cytokines by signalling through HLA class II molecules without inducing T-cell proliferation. Cytokine 2002;17:175–181.
Banchereau J, Steinman RM . Dendritic cells and the control of immunity. Nature 1998;19:392:245–392:252.
Luft T, Jefford M, Luetjens P, et al. Functionally distinct dendritic cell (DC) populations induced by physiologic stimuli: prostaglandin E(2) regulates the migratory capacity of specific DC subsets. Blood 2002;100:1362–1372.
Lee JJ, Takei M, Hori S, et al. The role of PGE(2) in the differentiation of dendritic cells: how do dendritic cells influence T-cell polarization and chemokine receptor expression? Stem Cells 2002;20:448–459.
de Jong EC, Vieira PL, Kalinski P, et al. Microbial compounds selectively induce Th1 cell-promoting or Th2 cell-promoting dendritic cells in vitro with diverse Th cell-polarizing signals. J Immunol 2002;168:1704–1709.
Nishimura F, Terranova VP . Comparative study of the chemotactic responses of periodontal ligament cells and gingival fibroblasts to polypeptide growth factors. J Dent Res 1996;75:986–992.
Maurer DH, Hanke JH, Mickelson E, et al. Differential presentation of HLA-DR, DQ, and DP restriction elements by interferon-gamma-treated dermal fibroblasts. J Immunol 1987;139:715–723.
Okada Y, Meguro M, Ohyama H, et al. Human leukocyte histocompatibility antigen class II-induced cytokines from human gingival fibroblasts promote proliferation of human umbilical vein endothelial cells: potential association with enhanced angiogenesis in chronic periodontal inflammation. J Periodontal Res 2009;44:103–109.
Kapsenberg ML . Dendritic-cell control of pathogen-driven T-cell polarization. Nat Rev Immunol 2003;3:984–993.
Moser M, Murphy KM . Dendritic cell regulation of TH1–TH2 development. Nat Immunol 2000;1:199–205.
Feili-Hariri M, Falkner DH, Morel PA . Polarization of naive T cells into Th1 or Th2 by distinct cytokine-driven murine dendritic cell populations: implications for immunotherapy. J Leukoc Biol 2005;78:656–664.
Harris SG, Padilla J, Koumas L, et al. Prostaglandins as modulators of immunity. Trends Immunol 2002;23:144–150.
Kaliński P, Vieira PL, Schuitemaker JH, et al. Prostaglandin E(2) is a selective inducer of interleukin-12 p40 (IL-12p40) production and an inhibitor of bioactive IL-12p70 heterodimer. Blood 2001;97:3466–3469.
Sempowski GD, Derdak S, Phipps RP . Interleukin-4 and interferon-gamma discordantly regulate collagen biosynthesis by functionally distinct lung fibroblast subsets. J Cell Physiol 1996;167:290–296.
Liu X, Kohyama T, Wang H, et al. Th2 cytokine regulation of type I collagen gel contraction mediated by human lung mesenchymal cells. Am J Physiol Lung Cell Mol Physiol 2002;282:L1049–L1056.
Kimura T, Ishii Y, Yoh K, et al. Overexpression of the transcription factor GATA-3 enhances the development of pulmonary fibrosis. Am J Pathol 2006;169:96–104.
Clark RA, Yamanaka K, Bai M, et al. Human skin cells support thymus-independent T cell development. J Clin Invest 2005;115:3239–3249.
Clark RA, Kupper TS . IL-15 and dermal fibroblasts induce proliferation of natural regulatory T cells isolated from human skin. Blood 2007;109:194–202.
Aschenbrenner K, D’Cruz LM, Vollmann EH, et al. Selection of Foxp3+ regulatory T cells specific for self antigen expressed and presented by Aire+ medullary thymic epithelial cells. Nat Immunol 2007;8:351–358.
Black AP, Ardern-Jones MR, Kasprowicz V, et al. Human keratinocyte induction of rapid effector function in antigen-specific memory CD4+ and CD8+ T cells. Eur J Immunol 2007;37:1485–1493.
Ardern-Jones MR, Black AP, Bateman EA, et al. Bacterial superantigen facilitates epithelial presentation of allergen to T helper 2 cells. Proc Natl Acad Sci USA 2007;104:5557–5562.
Saalbach A, Klein C, Sleeman J, et al. Dermal fibroblasts induce maturation of dendritic cells. J Immunol 2007;178:4966–4974.
Svensson M, Maroof A, Ato M, et al. Stromal cells direct local differentiation of regulatory dendritic cells. Immunity 2004;21:805–816.
Zhang M, Tang H, Guo Z, et al. Splenic stroma drives mature dendritic cells to differentiate into regulatory dendritic cells. Nat Immunol 2004;5:1124–1133.
Mollah ZU, Aiba S, Manome H, et al. Cord blood CD34+ cells differentiate into dermal dendritic cells in co-culture with cutaneous fibroblasts or stromal cells. J Invest Dermatol 2002;118:450–460.
Liu YJ, Soumelis V, Watanabe N, et al. TSLP: an epithelial cell cytokine that regulates T cell differentiation by conditioning dendritic cell maturation. Annu Rev Immunol 2007;25:193–219.
Gold KN, Weyand CM, Goronzy JJ . Modulation of helper T cell function by prostaglandins. Arthritis Rheum 1994;37:925–933.
Minakuchi R, Wacholtz MC, Davis LS, et al. Delineation of the mechanism of inhibition of human T cell activation by PGE2 . J Immunol 1990;145:2616–2625.
Demeure CE, Yang LP, Desjardins C, et al. Prostaglandin E2 primes naive T cells for the production of anti-inflammatory cytokines. Eur J Immunol 1997;27:3526–3531.
Kubo S, Takahashi HK, Takei M, et al. E-prostanoid (EP)2/EP4 receptor-dependent maturation of human monocyte-derived dendritic cells and induction of helper T2 polarization. J Pharmacol Exp Ther 2004;309:1213–1220.
Sheibanie AF, Tadmori I, Jing H, et al. Prostaglandin E2 induces IL-23 production in bone marrow-derived dendritic cells. FASEB J 2004;18:1318–1320.
Khayrullina T, Yen JH, Jing H, et al. In vitro differentiation of dendritic cells in the presence of prostaglandin E2 alters the IL-12/IL-23 balance and promotes differentiation of Th17 cells. J Immunol 2008;181:721–735.
Chizzolini C, Chicheportiche R, Alvarez M, et al. Prostaglandin E2 synergistically with interleukin-23 favors human Th17 expansion. Blood 2008;112:3696–3703.
Boniface K, Bak-Jensen KS, Li Y, et al. Prostaglandin E2 regulates Th17 cell differentiation and function through cyclic AMP and EP2/EP4 receptor signaling. J Exp Med 2009;206:535–548.
Napolitani G, Acosta-Rodriguez EV, Lanzavecchia A, et al. Prostaglandin E2 enhances Th17 responses via modulation of IL-17 and IFN-gamma production by memory CD4+ T cells. Eur J Immunol 2009;39:1301–1312.
Soumelis V, Reche PA, Kanzler H, et al. Human epithelial cells trigger dendritic cell mediated allergic inflammation by producing TSLP. Nat Immunol 2002;3:673–680.
Wang YH, Ito T, Wang YH, et al. Maintenance and polarization of human TH2 central memory T cells by thymic stromal lymphopoietin-activated dendritic cells. Immunity 2006;24:827–838.
Koyama K, Ozawa T, Hatsushika K, et al. A possible role for TSLP in inflammatory arthritis. Biochem Biophys Res Commun 2007;357:99–104.
Hirayama K, Matsushita S, Kikuchi I, et al. HLA-DQ is epistatic to HLA-DR in controlling the immune response to schistosomal antigen in humans. Nature 1987;327:426–430.
Wynn TA . Fibrotic disease and the T(H)1/T(H)2 paradigm. Nat Rev Immunol 2004;4:583–594.
Chiaramonte MG, Donaldson DD, Cheever AW, et al. An IL-13 inhibitor blocks the development of hepatic fibrosis during a T-helper type 2-dominated inflammatory response. J Clin Invest 1999;104:777–785.
Bataller R, Brenner DA . Liver fibrosis. J Clin Invest 2005;115:209–218.
Zhu Z, Homer RJ, Wang Z, et al. Pulmonary expression of interleukin-13 causes inflammation, mucus hypersecretion, subepithelial fibrosis, physiologic abnormalities, and eotaxin production. J Clin Invest 1999;103:779–788.
Jakubzick C, Choi ES, Joshi BH, et al. Therapeutic attenuation of pulmonary fibrosis via targeting of IL-4- and IL-13-responsive cells. J Immunol 2003;171:2684–2693.
Zurawski SM, Vega Jr F, Huyghe B, et al. Receptors for interleukin-13 and interleukin-4 are complex and share a novel component that functions in signal transduction. EMBO J 1993;12:2663–2670.
Jinnin M, Ihn H, Yamane K, et al. Interleukin-13 stimulates the transcription of the human alpha2 (I) collagen gene in human dermal fibroblasts. J Biol Chem 2004;279:41783–41791.
Fichtner-Feigl S, Strober W, Kawakami K, et al. IL-13 signaling through the IL-13alpha2 receptor is involved in induction of TGF-beta1 production and fibrosis. Nat Med 2006;12:99–106.
Acknowledgements
This study was supported, in part, by a Grant-in-Aid for Scientific Research (C) (Nos. 20592443 and 20599020) from the Japan Society for the Promotion of Science.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Laboratory Investigation website
Supplementary information
Rights and permissions
About this article
Cite this article
Kato-Kogoe, N., Ohyama, H., Nishimura, F. et al. Fibroblasts stimulated via HLA-II molecules produce prostaglandin E2 and regulate cytokine production from helper T cells. Lab Invest 90, 1747–1756 (2010). https://doi.org/10.1038/labinvest.2010.128
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.2010.128
Keywords
This article is cited by
-
Role of fibroblast plasticity and heterogeneity in modulating angiogenesis and healing in the diabetic foot ulcer
Molecular Biology Reports (2023)