Abstract
The role of the mitochondrial permeability transition pore (MPTP) in apoptosis of nucleated cells is well documented. In contrast, the role of MPTP in apoptosis of anucleated platelets is largely unknown. The aim of this study was to elucidate the contribution of MPTP in the control of different manifestations of platelet apoptosis by analyzing the effect of cyclosporin A (CsA), a potent inhibitor of MPTP formation. Using flow cytometry, we studied the effect of pretreatment of platelets with CsA on apoptotic responses in human platelets stimulated with calcium ionophore A23187. We found that CsA inhibited A23187-stimulated platelet apoptosis, completely preventing (i) depolarization of mitochondrial inner membrane potential (ΔΨm), (ii) activation of cytosolic apoptosis executioner caspase-3, (iii) platelet shrinkage, and (iv) fragmentation of platelets to microparticles, but (v) only partially (≈25%), inhibiting phosphatidylserine (PS) exposure on the platelet surface. This study shows that MPTP formation is upstream of ΔΨm depolarization, caspase-3 activation, platelet shrinkage and microparticle formation, and stringently controls these apoptotic events in A23187-stimulated platelets but is less involved in PS externalization. These data also indicate that CsA may rescue platelets from apoptosis, preventing caspase-3 activation and inhibiting the terminal cellular manifestations of platelet apoptosis, such as platelet shrinkage and degradation to microparticles. Furthermore, the results suggest a novel potentially useful application of CsA as an inhibitor of platelet demise through apoptosis in thrombocytopenias associated with enhanced platelet apoptosis.
Similar content being viewed by others
Main
Mitochondria are known as the ‘power factories’ of the cell, which supply energy required for cell life. However, another, quite unexpected, function of mitochondria has been documented providing strong evidence that they also play a key role in the control of cell apoptosis.1, 2, 3, 4, 5 Apoptosis, or programmed cell death, is the physiological mechanism that serves for controlled deletion of unwanted cells.3, 6 Since its discovery,7 apoptosis was long attributed exclusively to nucleated cells, in which it was shown that the formation of mitochondrial permeability transition pore (MPTP) is a critical event in mitochondrial control of apoptosis, responsible for depolarization of mitochondrial inner transmembrane potential (ΔΨm), permeabilization of inner and outer mitochondrial membrane, and subsequent release of proapoptotic proteins (such as cytochrome c and apoptosis-inducing factor) from mitochondria to cytosol.1, 2, 3, 4, 5, 8 MPTP is a channel which spans the inner and outer mitochondrial membranes and consists of multiple proteins, including the protein from the inner mitochondrial membrane (adenine nucleotide translocator, ANT), and the ANT-interacting mitochondrial matrix protein cyclophilin D (CypD), an essential regulator of MPTP formation.2, 9, 10 Although the role of ANT is debated,11, 12, 13 the role of CypD in the MPTP opening beyond doubt.2, 9, 10, 12, 13 Cyclosporin A (CsA), that interacts with CypD, is a well-known potent inhibitor of MPTP formation in isolated mitochondria and intact nucleated cells.2, 5, 8, 13
Over the past decade it has been recognized that apoptosis also occurs in anucleated cytoplasts14, 15, 16 and platelets.17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31 In contrast to nucleated cells, where the pivotal role of the mitochondrion in the control of apoptosis is well documented, the role of mitochondrial control of apoptosis in platelets is largely unknown. Although platelets lack a nucleus and nuclear DNA, they do contain mitochondria and mitochondrial DNA32, 33, 34 and metabolically stable mRNA and are capable of protein synthesis.35, 36, 37 Mitochondria contribute significantly to the energy metabolism of platelets.32
We have shown that diverse stimuli induce ΔΨm depolarization in platelets, including the soluble platelet agonists thrombin26, 28 and calcium ionophore A23187,24, 26 anti-glycoprotein (GP) IIb antibody,27 pathologically high shear stresses24 and long-term incubation of platelets under blood banking conditions.26, 31 Others, using rabbit and dog models, have shown the decrease of ΔΨm in circulating platelets during aging of platelets in vivo.25, 38 Mitochondria-associated apoptotic markers, caspase-9 and proapoptotic members of Bcl-2 family, as well as activation of executioner caspase-3 have also been shown to be induced in human and mouse platelets both in vitro and in vivo under an appropriate stimulation.17, 18, 19, 20, 21, 22, 24, 26, 27, 28, 29, 30, 31
Recently, the role of MPTP in the formation of a human platelet sub-population corresponding to ‘coated-platelets’ (platelets costimulated with collagen mimetic and GPVI agonist convulxin+thrombin) has been shown, as measured by the effect of CsA on coated-platelet markers—fibrinogen retention, calcein release and phosphatidylserine (PS) exposure.39 A key role for CypD was also shown in murine-coated platelets, using CypD-deficient (CypD−/−) and CypD-positive (CypD+/+) control mice: CypD−/− platelets exhibited reduced ΔΨm depolarization and PS exposure, and decreased surface retention of high-level fibrinogen.40
Although MPTP formation and ΔΨm depolarization were defined as early manifestations of apoptosis in nucleated cells,1, 2, 4, 8 the terminal ‘degradation phase’ of apoptosis is characterized by PS externalization on the plasma membrane surface and morphological alterations at the whole-cell level, such as cell shrinkage and shedding of membrane-enclosed vesicles, apoptotic bodies.5 These terminal manifestations of apoptosis were also shown in platelets after exposure to very high pathological shear stresses.24
The aim of this study was to elucidate the role of MPTP in the terminal manifestations of platelet apoptosis by analyzing the effect of CsA on PS exposure, platelet shrinkage and shedding of platelet microparticles in platelets stimulated with A23187, which is a known strong inducer of these platelet responses.23, 26, 41 Quantitative comparison of the CsA effect on mitochondrial (ΔΨm depolarization), cytoplasmic (caspase-3 activation), plasma membrane (PS exposure) and cellular (platelet shrinkage and microparticle formation) apoptotic events was also performed to evaluate, using ‘CsA-dependency test,’ the relative contribution of MPTP in the control of mitochondrial, executioner and terminal phases of platelet apoptosis.
MATERIALS AND METHODS
Reagents and Solutions
Bovine serum albumin (BSA), dimethylsulfoxide (DMSO) and 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES) and CsA were purchased from Sigma (St Louis, MO, USA), paraformaldehyde was purchased from Polysciences (Warrington, PA, USA), A23187 was purchased from Calbiochem (San Diego, CA, USA) and calpeptin (N-benzyloxycarbonyl-L-leucylnorleucinal) was purchased from Tocris Bioscience (Ellisville, MO, USA). Fluorescein isothiocyanate (FITC)-conjugated anti-GPIIbIIIa antibody (anti-CD41-FITC, clone P2) was purchased from Beckman-Coulter (Westbrook, ME, USA) and phycoerythrin (PE)-conjugated annexin V was purchased from BD Biosciences (San Jose, CA, USA). JC-1 (5,5′,6,6′-tetrachloro-1,1′,3,3′-tetraethylbenzimidazolyl-carbocyanine iodide) was purchased from Invitrogen (Carlsbad, CA, USA) and FAM-DEVD-FMK (carboxyfluorescein-carbonyl-aspartyl-glutamyl-valyl-aspartic acid fluoromethyl ketone) was purchased from Chemicon International (Temecula, CA, USA). Buffer A was composed of phosphate-buffered saline (Invitrogen) supplemented with 1 mM MgCl2, 5.6 mM glucose, 0.1% BSA and 10 mM HEPES, pH 7.4. Buffer B was composed of buffer A containing 0.5% DMSO. Stock solutions of CsA (10 mM) and A23187 (12 mM) were dissolved in DMSO, aliquots were stored at −80°C and after thawing just before use, working solutions were prepared by 1:200 dilution of stock solutions with buffer A to obtain required concentrations of CsA (50 μM) and A23187 (60 μM) in buffer A containing 0.5% DMSO.
Preparation and Treatment of Platelets with CsA and A23187
Venous blood from healthy volunteers was anticoagulated with 0.32% sodium citrate. Platelet-rich plasma (PRP) was obtained by centrifugation at 180 g for 15 min at room temperature (RT), and platelet count was determined by a Coulter LH750 Analyzer (Beckman-Coulter, Miami, FL, USA).
Platelet-rich plasma was diluted 1:10 with buffer A (for ΔΨm, caspase-3, platelet shrinkage and microparticle assays) and 1:60 with buffer A (for PS assay), and apoptotic events were determined in four groups of platelet samples: (i) buffer B-treated platelets, (ii) CsA- plus buffer B-treated platelets, (iii) A23187-treated platelets and (iv) CsA- plus A23187-treated platelets. All platelet treatment procedures were performed in a total volume of 30 μl. For buffer B-treated platelets (used as the DMSO-diluent control for CsA and A23187 treatments), 20 μl of diluted PRP aliquots were incubated with 10 μl buffer B for 45 min at RT. For CsA- plus buffer B-treated platelets, 20 μl of diluted PRP aliquots were preincubated for 30 min at RT with 5 μl buffer A containing 50 μM CsA and 0.5% DMSO, followed by incubation for 15 min at RT with 5 μl buffer B. For A23187-treated platelets, 20 μl of diluted PRP aliquots were preincubated for 30 min at RT with 5 μl buffer B, followed by incubation for 15 min at RT with 5 μl buffer A containing 60 μM A23187 and 0.5% DMSO. For CsA- plus A23187-treated platelets, 20 μl of diluted PRP aliquots were preincubated for 30 min at RT with 5 μl buffer A containing 50 μM CsA and 0.5% DMSO, followed by incubation for 15 min at RT with 5 μl buffer A containing 60 μM A23187 and 0.5% DMSO.
In some experiments, platelets were titrated with CsA concentrations (0, 1, 10 and 100 μM) or the effect of the duration of CsA (15, 30 and 60 min) and A23187 (15, 30 and 60 min) treatment was studied.
Treatment of Platelets with Calpeptin and A23187
Platelet-rich plasma was diluted 1:7.5 with buffer A (for ΔΨm and caspase-3 assays) and 1:45 with buffer A (for PS assay), and apoptotic events were determined in three groups of platelet samples: (i) buffer B-treated platelets, (ii) A23187-treated platelets and (iii) calpeptin- plus A23187-treated platelets. All platelet treatments were performed in a total volume of 30 μl. For buffer B-treated platelets (used as the DMSO-diluent control for calpeptin and A23187 treatments), 15 μl of diluted PRP aliquots were incubated with 15 μl buffer B for 45 min at RT. For A23187-treated platelets, 15 μl of diluted PRP aliquots were preincubated for 30 min at RT with 10 μl buffer B, followed by incubation for 15 min at RT with 5 μl buffer A containing 60 μM A23187 and 0.5% DMSO. For calpeptin- plus A23187-treated platelets, 15 μl of diluted PRP aliquots were preincubated for 30 min at RT with 10 μl buffer A containing 500 μM calpeptin and 0.5% DMSO, followed by incubation for 15 min at RT with 5 μl buffer A containing 60 μM A23187 and 0.5% DMSO. As was shown earlier in titration experiments,42 this concentration of calpeptin (200 μM final) strongly inhibited the shedding of microparticles from agonist-treated platelets.
Determination of Platelet Apoptotic Responses
Platelet apoptosis was analyzed in four groups of appropriately treated platelet samples (see above) by flow cytometry (FACSCalibur, BD Biosciences). Depolarization of ΔΨm, caspase-3 activation, PS exposure, and platelet shrinkage and fragmentation to microparticles were used for characterizing mitochondrial, cytoplasmic, plasma membrane and cellular manifestations of platelet apoptosis, respectively.
Depolarization of ΔΨm was measured by the cell-penetrating lipophilic cationic fluorochrome JC-1, which accumulates in mitochondrial matrix, driven by ΔΨm.2, 24, 27 The JC-1 stock solution (2 mg/ml in DMSO) was diluted with buffer A to a final concentration of 1–2 μg/ml, mixed by vortex, incubated in the dark for 15 min at RT and centrifuged for 15 min at 16 000 g in 1.5 ml Eppendorf tubes in an Eppendorf 5415C microfuge (Eppendorf, Westbury, NY, USA). The supernatants were harvested, combined and used immediately as the JC-1 working solution in the ΔΨm depolarization assay. Aliquots (30 μl) of treated platelets were incubated in the dark for 30 min at 37°C with 470 μl of JC-1 working solution, and samples were acquired for flow cytometry. Platelets were gated by characteristic light forward scatter (FSC)—side scatter (SSC) dot plots and platelet-bound JC-1 monomers (fluorescence 1, FL1) and JC-1 aggregates (fluorescence 2, FL2) were analyzed as FL1-FL2 dot plots. Depolarization of ΔΨm was quantified as an increase of the percentage depolarized cells, which reflects the decrease in content of JC-1 aggregates when the inner mitochondrial membrane becomes depolarized.
Caspase-3 activation was determined using the cell-penetrating fluorescein-labeled peptide inhibitor of caspase-3, FAM-DEVD-FMK, which covalently binds to active caspase-3.22, 24, 26 Aliquots (3.3 μl) of 10 × working FAM-DEVD-FMK solution, prepared according to the manufacturer's recommendations, were added to 30 μl of treated platelet samples and incubated for 45 min at 37°C in the dark. Following dilution to 500 μl with buffer A, samples were acquired within 30–60 min at low acquisition rate. Fluorescent (FL1) histograms were analyzed and caspase-3 activation was quantified as the mean channel fluorescence of platelet-bound FAM-DEVD-FMK.
Phosphatidylserine exposure in treated platelet samples was quantified by dual-color staining with annexin V-PE and anti-GPIIbIIIa-FITC antibody for 15 min at RT as described earlier27 and expressed as the percentage annexin V-positive cells.
Platelet shrinkage and microparticle formation were detected using platelet- and microparticle-specific anti-GPIIbIIIa antibody. Aliquots (5 μl) of anti-GPIIbIIIa-FITC antibody were added to 30 μl of treated platelets and incubated for 15 min at RT in the dark. Samples were fixed with 100 μl of 1% paraformaldehyde in buffer A for 30 min at RT and diluted to 500 μl with buffer A. After acquisition, the FSC-FL1 dot plots were analyzed and platelets and microparticles were identified in platelet- and microparticle-specific gates, respectively.24 Platelet shrinkage was determined by analyzing FSC histograms as the decrease of FSC characteristics of GPIIbIIIa-positive events in platelet gate and expressed as the mean FSC. Fragmentation of platelets to microparticles was quantified by counting GPIIbIIIa-positive events in microparticle gate; 20 000 GPIIbIIIa-positive events were acquired totally in both platelet plus microparticle gates.
Calculation of Inhibitory Effect of CsA on Apoptotic Responses
To quantify the relative impact of CsA on different manifestations of platelet apoptosis, the inhibitory effect of CsA on A23187-induced apoptotic events was calculated for each apoptotic parameter. For A23187-upregulated apoptotic parameters (ΔΨm depolarization, caspase-3 activation, PS exposure and microparticle formation), the percentage of inhibition (I, %) of apoptotic parameters by CsA was calculated by the formula:

where A, B and C are the values of apoptotic parameters after the treatment of platelets with A23187 (A), control diluent buffer (B) or CsA+A23187 (C).
For A23187-downregulated apoptotic parameter (platelet shrinkage), the percentage of inhibition was calculated by the formula:

Statistical Analysis
Data are presented as means±s.e.m. The statistical significance of the differences between different platelet groups was determined by paired Student's t-test and one-way ANOVA as appropriate. Differences were considered significant when P<0.05.
RESULTS
Calcium Ionophore A23187 Induces Apoptotic Events in Human Platelets
Table 1 shows that calcium ionophore A23187 (10 μM) triggers a number of apoptotic alterations in human platelets. As the result of A23187 treatment, an average of approximately 40% of platelets had depolarized ΔΨm, as measured by JC-1 staining, and 99% of the cells had exposed PS on their surface, as detected by annexin V binding (Table 1). Caspase-3 activation was also observed, as measured by a 2.3-fold increase in the mean fluorescence of A23187-treated platelets stained with FAM-DEVD-FMK probe, which irreversibly binds to active caspase-3 (Table 1). Breakdown of platelets to microparticles was revealed as GPIIbIIIa-positive events in the microparticle gate: a 7.6-fold increase in the number of microparticles was observed following A23187 treatment (Table 1). Finally, platelet shrinkage was detected as a 1.5-fold decrease of the mean FSC of GPIIbIIIa-positive events in the platelet gate (Table 1). Assuming that FSC is directly proportional to the platelet size, this result indicates that A23187 causes a decrease in mean platelet size of 33%.
CsA Significantly Inhibits Apoptosis in A23187-stimulated Platelets
To examine how inhibition of MPTP formation affects platelet apoptosis, A23187-stimulated platelets were preincubated with CsA and different apoptotic responses were analyzed in comparison with responses observed in platelets incubated with A23187 only. Pretreatment of platelets with 10 μM CsA significantly inhibited all manifestations of platelet apoptosis induced by calcium ionophore, including ΔΨm depolarization (Figure 1, P=0.01), caspase-3 activation (Figure 2, P=0.02), PS externalization (Figure 3, P=0.04), shedding of microparticles (Figure 4, P=0.002) and platelet shrinkage (Figure 5, P=0.002).
Cyclosporin A inhibits depolarization of mitochondrial inner membrane potential (ΔΨm) in A23187-stimulated human platelets. Depolarization of ΔΨm was determined by JC-1 fluorochrome. (a–d) Representative dot plots are shown for platelets treated with control buffer (a), 10 μM A23187 (c), and preincubated with 10 μM CsA before treatment with buffer (b) or A23187 (d). Depolarization is characterized as the decrease in the content of JC-1 aggregates, as reflected in the decrease of red (FL2) fluorescence. Numbers in the lower parts of dot plots represent the percentage ΔΨm-depolarized cells. (e) Means and s.e.m. for five experiments and P-value between A23187- and CsA+A23187-treated platelet groups are shown: **P=0.01. P-value between A23187- vs control buffer-treated groups is presented in Table 1. Horizontal line indicates the mean percentage cells undergoing ΔΨm depolarization in buffer-treated platelet group.
Cyclosporin A inhibits activation of executioner caspase-3 in A23187-stimulated human platelets. (a) Representative histograms are shown for platelets treated with control buffer (thin line 1), 10 μM A23187 (thick line 2) or 10 μM CsA+10 μM A23187 (mid-thickness line 3). (b) Means and s.e.m. for four experiments and P-value between A23187- and CsA+A23187-treated platelet groups are shown: *P=0.02. P-value between A23187- and control buffer-treated groups is presented in Table 1. MCF: mean channel fluorescence of cell-penetrating FAM-DEVD-FMK dye that determines active caspase-3. Horizontal line indicates the mean fluorescence of platelet-bound FAM-DEVD-FMK in buffer-treated platelet group.
Cyclosporin A inhibits phosphatidylserine exposure in A23187-stimulated human platelets. (a–d) Representative dot plots and the percentage annexin V-positive cells (numbers in the upper parts of dot plots) are shown for platelets treated with control buffer (a), 10 μM A23187 (c), and preincubated with 10 μM CsA before treatment with buffer (b) or A23187 (d). (e) Means and s.e.m. for five experiments and P-value between A23187- and CsA+A23187-treated platelet groups are shown: *P=0.04. P-value between A23187- and buffer-treated groups is presented in Table 1. Horizontal line indicates the mean percentage annexin V-positive cells in buffer-treated platelet group.
Cyclosporin A inhibits fragmentation of human platelets to microparticles induced by A23187. Platelets (PLTs) and microparticles (MPs) were stained with anti-GPIIbIIIa antibody. (a–d) Representative dot plots and gating for PLTs and MPs are shown for platelets treated with control buffer (a), 10 μM A23187 (c), and preincubated with 10 μM CsA before treatment with buffer (b) or A23187 (d). The gate of MPs was used for counting microparticles as GPIIbIIIa-positive events with low forward scatter (FSC), whereas the gate of PLTs was used for analyzing platelet shrinkage from FSC histograms (Figure 5a) and mean FSC values (Figure 5b). (e) Means and s.e.m. for five experiments and P-value between A23187- and CsA+A23187-treated platelet groups are shown: **P=0.002. P-value between A23187- and buffer-treated groups is presented in Table 1. Horizontal line indicates the mean number of microparticles in buffer-treated platelet group.
Cyclosporin A inhibits shrinkage of human platelets induced by A23187. (a) Representative histograms are shown for platelets treated with control buffer (thin line 1), 10 μM A23187 (thick line 2) or 10 μM CsA+10 μM A23187 (mid-thickness line 3). FSC histograms were obtained from the platelet gate (PLTs) as shown in Figure 4a, c and d. Note that platelet shrinkage, induced by A23187, is characterized by FSC downregulation. (b) Means and s.e.m. for five experiments and P-value between A23187- and CsA+A23187-treated platelet groups are shown: **P=0.002. P-value between A23187- and buffer-treated groups is presented in Table 1. Horizontal line indicates the mean FSC of platelets in buffer-treated platelet group.
Quantification of Inhibitory Effect of CsA on Different Apoptotic Events in A23187-stimulated Platelets
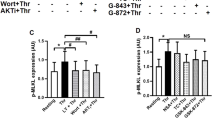
Figure 6 shows further quantitative analysis of the CsA inhibitory effect on different apoptotic parameters in A23187-induced platelets. This showed that CsA strongly inhibited ΔΨm dissipation (106.3±1.2%), platelet shrinkage (118.3±13.4%), fragmentation of platelets to microparticles (101.5±2.3%) and caspase-3 activation (85.9±8.3%), but only moderately (23.9±7.9%) inhibited PS exposure (Figure 6). The mean inhibitory effect of CsA on ΔΨm depolarization, platelet shrinkage and microparticle formation, calculated as described above (Materials and Methods), exceeded 100%, reflecting the fact that CsA extremely efficiently inhibits these apoptotic events; platelets treated with CsA plus A23187 become even slightly less apoptotic than platelets treated with the control buffer (Figures 1, 4 and 5). The differences between the inhibitory effect of CsA on ΔΨm depolarization, platelet shrinkage, microparticle formation and caspase-3 activation, characterized by the high mean level of inhibition (86–118%), were not significant (Figure 6, all P-values >0.05), showing that CsA completely prevents triggering these apoptotic responses in A23187-stimulated platelets.
Comparison between inhibitory effects of cyclosporin A on different apoptotic events in A23187-stimulated human platelets. Percentage of inhibition by CsA of ΔΨm depolarization (ΔΨm), platelet shrinkage (Shr), microparticle formation (MPs), caspase-3 activation (Cas-3) and PS exposure (PS) was calculated from the data presented in Figures 1, 2, 3, 4, 5 as described in Materials and Methods. Means and s.e.m. are shown and P-values calculated by one-way ANOVA between PS exposure vs other apoptotic events are presented: ***P<0.001. Note that preincubation of A23187-stimulated platelets with CsA completely prevents ΔΨm depolarization, platelet shrinkage, fragmentation of platelets to microparticles, and caspase-3 activation (differences between these apoptotic events are not significant, P>0.05) but only moderately inhibits PS externalization.
In contrast, differences between the CsA inhibitory effect on PS exposure vs the effect on other apoptotic events were highly significant (Figure 6, P<0.001). This indicates that, in comparison with other apoptotic events, A23187-induced PS exposure is much less sensitive to inhibition of MPTP formation by CsA. Moderate inhibitory effect of CsA on PS exposure was persistent in a wide range of CsA concentrations from 1 to 100 μM (Figure 7a), and the magnitude of the effect did not depend on the duration of platelet treatment with CsA (Figure 7b) and A23187 (Figure 7c).
Effect of cyclosporin A (CsA) on phosphatidylserine exposure in A23187-stimulated human platelets does not depend on CsA concentration (a) and the duration of platelet treatment with CsA (b) and A23187 (c). Exposure of phosphatidylserine (PS) on the platelet surface was determined by annexin V-binding assay and expressed as the percentage annexin V-positive cells in A23187 only-treated platelets assigned 100%; all incubations were performed at room temperature. (a) Dependence of PS exposure on CsA concentration. Platelets were preincubated with control diluent buffer (0 μM CsA) or 1, 10 and 100 μM CsA for 30 min followed by incubation with 10 μM A23187 for 15 min. Means and s.e.m. for six experiments and P-value between CsA+A23187-treated platelet groups vs A23187 only-treated group are shown: **P<0.01; P-values between three CsA+A23187-treated platelet groups (1, 10 and 100 μM CsA) are not significant: P>0.05. (b) Dependence of PS exposure on preincubation time with CsA. Platelets were preincubated with 10 μM CsA for 15, 30 or 60 min followed by incubation with 10 μM A23187 for 15 min. Means and s.e.m. for three experiments are presented; P-values between different CsA+A23187-treated platelet groups are not significant: P>0.05. (c) Dependence of PS exposure on incubation time with A23187. Platelets were preincubated with 10 μM CsA for 30 min followed by incubation with 10 μM A23187 for 15, 30 or 60 min. Means and s.e.m. for three experiments are presented; P-values between different CsA+A23187-treated platelet groups are not significant: P>0.05.
Calpeptin, an Inhibitor of Calcium-Dependent Proteinase Calpain, Has No Effect on Mitochondrial Inner Membrane Depolarization
Wolf et al19 showed that calpeptin, an inhibitor of calcium-dependent proteinase calpain,43 strongly inhibited some apoptotic events in A23187-treated platelets, including generation of microparticles, and suggested a role for calpain in platelet apoptosis.
In this study, we analyzed the effect of calpeptin on depolarization of mitochondrial inner membrane and extra-mitochondrial apoptotic events in A23187-stimulated platelets. Figure 8a shows that, in accordance with the earlier published data,19 calpeptin significantly inhibited fragmentation of platelets to microparticles (P=0.008). However, calpeptin did not affect mitochondrial ΔΨm depolarization, caspase-3 activation and PS exposure (Figure 8b), indicating that not all manifestations of platelet apoptosis can be modulated by calpain.
Calpeptin inhibits generation of microparticles (a) but does not affect ΔΨm depolarization, caspase-3 activation and phosphatidylserine exposure (b) in A23187-stimulated human platelets. Platelets were pretreated with control diluent buffer followed by incubation with 10 μM A23187 (open bars) or pretreated with 200 μM calpeptin followed by incubation with 10 μM A23187 (closed bars). Platelet apoptosis was determined as MP formation (four experiments), ΔΨm depolarization (four experiments), caspase-3 activation (six experiments) and PS exposure (four experiments), and expressed as the percentage of the averaged values of apoptotic events in platelets treated with A23187 in the absence of calpeptin assigned 100%. Means and s.e.m. are shown and P-values calculated between calpeptin+A23187- vs A23187-treated platelet groups: **P=0.008 for MPs, P=0.64 for ΔΨm, P=0.88 for caspase-3 and P=0.40 for PS.
DISCUSSION
The mitochondrion plays a key role in the control of apoptosis in nucleated cells, and permeabilization of mitochondrial membranes is crucial in apoptotic cell demise. Two general mechanisms are responsible for mitochondrial membrane permeabilization during apoptosis of nucleated cells. In the first mechanism, the pore (MPTP) opens in the inner mitochondrial membrane, allowing water and molecules up to 1.5 kDa to pass through. Opening of the MPTP can be triggered by multiple apoptotic stimuli and leads to depolarization of ΔΨm, and swelling of the mitochondrial matrix with following permeabilization of the outer mitochondrial membrane and release of proteins normally confined to the intermembrane space, including cytochrome c and apoptosis-inducing factor. The second mechanism is mediated by members of the Bcl-2 family of apoptosis-regulating proteins acting directly on the outer membrane.1, 2, 3, 4, 5, 8
Numerous reports indicate that MPTP formation plays a critical role in the control of nucleated cell apoptosis.1, 2, 4, 5, 8 CsA, a pharmacological agent that inhibits MPTP formation in nucleated cells,2, 4, 5, 8, 44 reduced infarct size in the heart and brain45 and enhanced the functional recovery after hypothermic heart preservation.46
In contrast to nucleated cells, much less is known about mitochondrial control and the role of MPTP in apoptosis of anucleated platelets. In this study, five key markers were used for characterizing platelet apoptotic events in mitochondria, cytosol, plasma membrane and at the whole-cell level. Apoptotic alterations in mitochondria were detected by the ΔΨm depolarization, a hallmark of mitochondrial inner membrane permeabilization. Cytosolic apoptotic events were determined by measuring activation of caspase-3, an executioner caspase cleaving vital cell proteins. Apoptotic changes in plasma membrane were analyzed by evaluating PS externalization on the platelet surface and, finally, cellular manifestations of platelet apoptosis were detected by quantifying shedding of membrane-enclosed vesicles (microparticles) resembling apoptotic bodies and by platelet shrinkage. These apoptotic markers were used to characterize apoptosis in platelets treated with a powerful platelet agonist, A23187. We found that all five apoptotic responses were triggered in human platelets, covering different aspects of apoptosis, ranging from an early mitochondrial ΔΨm depolarization and activation of apoptosis executioner caspase-3 in the cytosol, ultimately culminating in the terminal biochemical and morphological alterations, such as exposure of PS on the cell surface and platelet shrinkage and fragmentation to microparticles (Tables 1 and 2). Earlier, we reported that the same wide spectrum of apoptotic events was induced in platelets exposed to another strong stimulus, a very high pathological shear stresses.24 Thus, as an inducer of platelet apoptosis, by the breadth and strength of platelet apoptotic responses, A23187 corresponds to pathological high shear stresses.
In this study, we also tested the hypothesis that MPTP formation plays a crucial role in the control of apoptosis in A23187-stimulated human platelets. Recently, it has been shown that a targeted deletion of the Ppif gene in null mice (characterized by the complete absence of the Ppif gene product, CypD9) results in attenuation of two apoptosis-related events, ΔΨm depolarization and PS exposure, in murine-coated platelets costimulated with collagen-mimetic convulxin plus thrombin.40 Using another approach, we elucidated whether CsA, an inhibitor of MPTP formation in nucleated cells, is able to protect human platelets from apoptosis when platelets, isolated from healthy volunteers with normal functional CypD-producing gene, were stimulated with Ca2+-mobilizing/overloading agent A23187 (Table 3). The CsA-dependency test allowed us to quantify the contribution of MPTP formation in triggering different apoptotic events in A23187-stimulated platelets and to examine upstream–downstream relationships between MPTP opening and other apoptotic alterations. We showed that CsA completely prevents mitochondrial apoptotic event, ΔΨm depolarization, and extra-mitochondrial cytosolic event, caspase-3 activation. Surprisingly, CsA is also able to completely prevent two complex terminal manifestations of apoptosis at the whole-cell level, platelet shrinkage and degradation of platelets to microparticles, but only partially (≈25%) inhibits the third terminal apoptotic event, PS exposure on the platelet surface (Figure 6, Table 2). The moderate effect of CsA on PS exposure is persistent and does not depend on CsA concentration and the duration of platelet treatment with CsA and A23187 (Figure 7).
These results indicate that biochemical apoptotic markers (mitochondrial ΔΨm depolarization and cytosolic caspase-3 activation) and cellular morphological alterations that accompany terminal phase of apoptosis (platelet shrinkage and fragmentation to microparticles) are strongly dependent on the MPTP formation (Table 2) and are kept under the stringent control of MPTP. However, another terminal apoptotic event (PS externalization) is only moderately dependent on the MPTP formation (Table 2), suggesting that this manifestation of platelet apoptosis is mostly controlled by MPTP-independent mechanisms. Consistent with this, it was recently reported that calcium-ionophore ionomycin increased PS exposure to the same level both in control (CypD+/+) and CypD-deficient (CypD−/−) mouse platelets.40 MPTP-independent PS externalization has been also shown in nucleated cells: CypD+/+ and CypD−/− murine thymocytes, and embryonic fibroblasts underwent the same level of PS externalization when exposed to various apoptotic stimuli, including A23187, etoposide, staurosporin and tumour-necrosis factor-α plus cycloheximide.47 However, in contrast to calcium-ionophore stimulated platelets, CypD-deficient mouse platelets40 and CsA-treated human platelets39 stimulated with convulxin plus thrombin are characterized by impaired PS exposure, ie, are strongly dependent on MPTP formation.
As follows from the quantitative evaluation of the effect of CsA on different apoptotic parameters, ΔΨm depolarization, caspase-3 activation, platelet shrinkage and release of microparticles are located downstream of MPTP formation. In contrast, it appears that although some processes involved in PS externalization may be located downstream of MPTP formation, they are mainly not associated with and/or are located upstream of MPTP formation.
In this report, we also showed that calcium-dependent proteinase calpain is not involved in depolarization of mitochondrial inner membrane in A23187-stimulated human platelets (Figure 8). We (Table 1) and others have shown activation of caspase-3 in A23187-stimulated platelets18, 23, 26 as well as in platelets stimulated with thrombin,18, 26, 29 collagen,18 collagen plus thrombin,18 anti-platelet antibodies22, 27 and long-term platelet storage under blood banking conditions.26 Wolf et al19 reported caspase-3 activation in vitro in platelet cytosolic extracts treated with cytochrome c and dATP, but did not find caspase-3 activation in whole unfractionated platelets stimulated with A23187, thrombin or collagen plus thrombin. In contrast, these authors presented the evidence that calpain, rather than caspases, promotes several apoptotic events during platelet activation.19 The basis for this discrepancy is not known and may reflect the effect of subtle differences in the incubation conditions used in these studies on the assays of caspase activity. It appears that both calcium-dependent proteinases, caspases and calpain, can execute platelet apoptosis.
To investigate whether calpain is involved in depolarization mitochondrial inner membrane and execution of other apoptotic events, we analyzed the effect of calpain inhibitor, calpeptin, on ΔΨm depolarization, caspase-3 activation, PS exposure and microparticle formation (Figure 8). Experiments with calpeptin were performed in the incubation conditions used for the analysis of the CsA effect on apoptotic parameters, such as preincubation with calpeptin for 30 min at RT, followed by incubation with 10 μM A23187 for 15 min at RT. Using this experimental setting, we found that, in comparison with platelets stimulated with A23187 only, pretreatment of platelets with 200 μM calpeptin followed by incubation with 10 μM A23187, significantly inhibited generation of platelet microparticles (Figure 8a) but did not affect mitochondrial ΔΨm depolarization, caspase-3 activation and PS exposure (Figure 8b).
Under different experimental conditions (pretreatment of platelets with 25 μM calpeptin for 30 min at RT and subsequent incubation with 2 μM A23187 for 15 min at 37°C), Wolf et al19 also showed that calpeptin strongly inhibited some apoptosis-related events in A23187-activated platelets, including shedding of microparticles, processing of procaspase-3 to proteolytically inactive 30 kDa fragment and cleavage of ‘apoptotic’ substrates, gelsolin and protein kinase C-δ. However, as in our study (Figure 8b), in these conditions, PS exposure was not affected by calpeptin.19 Furthermore, in accordance with our data on the absence of calpeptin effect on caspase-3 activation in unfractionated A23187-treated platelets (Figure 8b), these authors reported that calpeptin was a poor inhibitor of caspase-3 proteinase activity when calpeptin in various concentrations was incubated with purified caspase-3 in cell-free enzymatic reaction.19
Taken together, these results indicate that, under experimental conditions used in this and earlier19 studies, calpeptin significantly inhibited microparticle formation19 (Figure 8a) and cleavage of apoptotic substrates19 but did not affect mitochondrial ΔΨm depolarization (Figure 8b), caspase-3 activation and PS exposure19 (Figure 8b) in A23187-stimulated human platelets. These data suggest that during platelet activation some apoptotic events can be modulated by calpain, whereas the others, including depolarization of mitochondrial membrane, are calpain-independent.
In summary, the data presented indicate that, as in nucleated cells, mitochondria play a crucial role in the control of apoptosis in anucleated platelets and that the formation of MPTP is a key mechanism in mitochondrial control of platelet apoptosis. We showed that MPTP formation in A23187-stimulated human platelets is strongly involved not only in the ‘neighboring’ MPTP-associated manifestation of mitochondrial apoptosis, ΔΨ depolarization, but also in the executioner and terminal apoptotic events, activation of caspase-3, platelet shrinkage and breakdown of platelets to microparticles. However, MPTP formation only moderately contributes to the PS exposure on the platelet surface, suggesting that the externalization of PS only partially depends on the release of proapoptotic factors from permeabilized mitochondria in A23187-stimulated platelets, in contrast to platelets stimulated with physiologically relevant inducers colvulxin plus thrombin.
There is great interest in developing drugs that modulate cell apoptosis.4, 5, 44 Data presented in this and earlier studies indicate that preservation of mitochondrial integrity with CsA efficiently rescues platelets from a wide spectrum of apoptotic alterations by targeting MPTP, suggesting a novel potential application of this drug for inhibiting platelet demise through apoptosis in thrombocytopenias associated with enhanced platelet apoptosis.22, 27
References
Bernardi P, Scorrano L, Colonna R, et al. Mitochondria and cell death. Mechanistic aspects and methodological issues. Eur J Biochem 1999;264:687–701.
Kroemer G, Reed JC . Mitochondrial control of cell death. Nat Med 2000;6:513–519.
Danial NN, Korsmeyer SJ . Cell death: critical control points. Cell 2004;116:205–219.
Green DR, Kroemer G . Pharmacological manipulation of cell death: clinical applications in sight? J Clin Invest 2005;115:2610–2617.
Kroemer G, Galluzzi L, Brenner C . Mitochondrial membrane permeabilization in cell death. Physiol Rev 2007;87:99–163.
Steller H . Mechanisms and genes of cellular suicide. Science 1995;267:1445–1449.
Kerr JF, Wyllie AH, Currie AR . Apoptosis: a basic biological phenomenon with wide-ranging implications in tissue kinetics. Br J Cancer 1972;26:239–257.
Crompton M . The mitochondrial permeability transition pore and its role in cell death. Biochem J 1999;341:233–249.
Baines CP, Kaiser RA, Purcell NH, et al. Loss of cyclophilin D reveals a critical role for mitochondrial permeability transition in cell death. Nature 2005;434:658–662.
Basso E, Fante L, Fowlkes J, et al. Properties of the permeability transition pore in mitochondria devoid of Cyclophilin D. J Biol Chem 2005;280:18558–18561.
Kokoszka JE, Waymire KG, Levy SE, et al. The ADP/ATP translocator is not essential for the mitochondrial permeability transition pore. Nature 2004;427:461–465.
Halestrap A . A pore way to die. Nature 2005;434:578–579.
Leung AW, Helestrap AP . Recent progress in elucidating the molecular mechanism of the mitochondrial permeability transition pore. Biochim Biophys Acta 2008;1777:946–952.
Jacobson MD, Burne JF, Raff MC . Programmed cell death and Bcl-2 protection in the absence of a nucleus. EMBO J 1994;13:1899–1910.
Schulze-Osthoff K, Walczak H, Droge W, et al. Cell nucleus and DNA fragmentation are not required for apoptosis. J Cell Biol 1994;127:15–20.
Martin SJ, Finucane DM, Amarante-Mendes GP, et al. Phosphatidylserine externalization during CD95-induced apoptosis of cells and cytoplasts requires ICE/CED-3 protease activity. J Biol Chem 1996;271:28753–28756.
Vanags DM, Orrenius S, Aguilar-Santelises M . Alterations in Bcl-2/Bax protein levels in platelets form part of an ionomycin-induced process that resembles apoptosis. Br J Haematol 1997;99:824–831.
Shcherbina A, Remold-O’Donnell E . Role of caspase in a subset of human platelet activation responses. Blood 1999;93:4222–4231.
Wolf BB, Goldstein JC, Stennicke HR, et al. Calpain functions in a caspase-independent manner to promote apoptosis-like events during platelet activation. Blood 1999;94:1683–1692.
Brown SB, Clarke MC, Magowan L, et al. Constitutive death of platelets leading to scavenger receptor-mediated phagocytosis. A caspase-independent cell clearance program. J Biol Chem 2000;275:5987–5996.
Li J, Xia Y, Bertino AM, et al. The mechanism of apoptosis in human platelets during storage. Transfusion 2000;40:1320–1329.
Piguet PF, Vesin C . Modulation of platelet caspases and life-span by anti-platelet antibodies in mice. Eur J Haematol 2002;68:253–261.
Leytin V, Freedman J . Platelet apoptosis in stored platelet concentrates and other models. Transfus Apheresis Sci 2003;28:285–295.
Leytin V, Allen DJ, Mykhaylov S, et al. Pathologic high shear stress induces apoptosis events in human platelets. Biochem Biophys Res Commun 2004;320:303–310.
Rand ML, Wang H, Bang KW, et al. Procoagulant surface exposure and apoptosis in rabbit platelets: association with shortened survival and steady-state senescence. J Thromb Haemost 2004;2:651–659.
Leytin V, Allen DJ, Mykhaylov S, et al. Thrombin-triggered platelet apoptosis. J Thromb Haemost 2006;4:2656–2663.
Leytin V, Mykhaylov S, Starkey AF, et al. Intravenous immunoglobulin inhibits anti-glycoprotein IIb-induced platelet apoptosis in a murine model of immune thrombocytopenia. Br J Haematol 2006;133:78–82.
Leytin V, Allen DJ, Lyubimov E, et al. Higher thrombin concentrations are required to induce platelet apoptosis than to induce platelet activation. Br J Haematol 2007;136:762–764.
Lopez JJ, Salido GM, Gomez-Arteta E, et al. Thrombin induces apoptotic events through the generation of reactive oxygen species in human platelets. J Thromb Haemost 2007;5:1283–1291.
Mason KD, Carpinelli MR, Fletcher JI, et al. Programmed anuclear cell death delimits platelet life span. Cell 2007;128:1173–1186.
Leytin V, Allen DJ, Mutlu A, et al. Platelet activation and apoptosis are different phenomena: evidence from the sequential dynamics and the magnitude of responses during platelet storage. Br J Haematol 2008;142:494–497.
Holmsen H . Biochemistry of the platelet: energy metabolism. In: Colman RW (ed). Hemostasis and Thrombosis. Lippincott: Philadelphia, 1987, pp 631–643.
Shuster RC, Rubenstein AJ, Wallace DC . Mitochondrial DNA in anucleate human blood cells. Biochem Biophys Res Commun 1988;155:1360–1365.
White JG . Platelet structure. In: Michelson AD (ed). Platelets, 2nd edn. Academic Press: San Diego, 2007, pp 45–73.
Weyrich AS, Dixon DA, Pabla R, et al. Signal-dependent translation of a regulatory protein, Bcl-3, in activated human platelets. Proc Natl Acad Sci USA 1998;95:5556–5561.
Lindemann S, Gawaz M . The active platelet: translation and protein synthesis in an anucleate cell. Semin Thromb Hemost 2007;33:144–150.
Zimmerman GA, Weyrich AS . Signal-dependent protein synthesis by activated platelets: new pathways to altered phenotype and function. Arterioscler Thromb Vasc Biol 2008;28:s17–s24.
Pereira J, Soto M, Palomo I, et al. Platelet aging in vivo is associated with activation of apoptotic pathways: studies in a model of suppressed thrombopoiesis in dogs. Thromb Haemost 2002;87:905–909.
Remenyi G, Szasz R, Friese P, et al. Role of mitochondrial permeability transition pore in coated-platelet formation. Arterioscler Thromb Vasc Biol 2005;25:467–471.
Jobe SM, Wilson KM, Leo L, et al. Critical role for the mitochondrial permeability transition pore and cyclophilin D in platelet activation and thrombosis. Blood 2008;111:1257–1265.
Horstman LL, Ahn YS . Platelet microparticles: a wide-angle perspective. Crit Rev Oncol Hematol 1999;30:111–142.
Fox JEB, Austin CD, Reynolds CC, et al. Evidence that agonist-induced activation of calpain causes the shedding of procoagulant-containing microvesicles from the membrane of aggregating platelets. J Biol Chem 1991;266:13289–13295.
Tsujinaka T, Kajiwara Y, Kambayashi J, et al. Synthesis of a new cell penetrating calpain inhibitor (calpeptin). Biochem Biophys Res Commun 1988;153:1201–1208.
Waldmeier PC, Zimmermann K, Lemasters JJ . Cyclophilin D as a drug target. Curr Med Chem 2003;10:1485–1506.
Mattson MP, Kroemer G . Mitochondria in cell death: novel targets for neuroprotection and cardioprotection. Trends Mol Med 2003;9:196–205.
Rajesh KG, Sasaguri S, Ryoko S, et al. Mitochondrial permeability transition-pore inhibition enhances functional recovery after long-time hypothermic heart preservation. Transplantation 2003;76:1314–1320.
Nakagawa T, Shimizu S, Watanabe T, et al. Cyclophilin D-dependent mitochondrial permeability transition regulates some necrotic but not apoptotic cell death. Nature 2005;434:652–658.
Acknowledgements
This work was supported by Grant T 6285 from the Heart and Stroke Foundation of Ontario, Canada.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure/duality of interest
The authors declare no competing financial interest.
Rights and permissions
About this article
Cite this article
Leytin, V., Allen, D., Mutlu, A. et al. Mitochondrial control of platelet apoptosis: effect of cyclosporin A, an inhibitor of the mitochondrial permeability transition pore. Lab Invest 89, 374–384 (2009). https://doi.org/10.1038/labinvest.2009.13
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.2009.13
Keywords
This article is cited by
-
Platelet mitochondrial membrane depolarization reflects disease severity in patients with preeclampsia
Molecular Medicine (2022)
-
Functional cyclophilin D moderates platelet adhesion, but enhances the lytic resistance of fibrin
Scientific Reports (2018)
-
Low-level light treatment ameliorates immune thrombocytopenia
Scientific Reports (2016)
-
Platelet mitochondrial membrane depolarization reflects disease severity in patients with sepsis and correlates with clinical outcome
Critical Care (2014)
-
Crocin prevents sesamol-induced oxidative stress and apoptosis in human platelets
Journal of Thrombosis and Thrombolysis (2014)