Abstract
To assess the differences among seven different methods for the calculation of mean arterial pressure (MAP) and to identify the formula that provides MAP values that are more closely associated with target organ deterioration as expressed by the carotid cross-sectional area (CSA), carotid-to-femoral pulse-wave velocity (cf-PWV) and left ventricular mass (LVM). The study population consisted of 1878 subjects who underwent noninvasive cardiovascular risk assessment. Blood pressure (BP) was assessed in all subjects, and MAP was calculated by direct oscillometry and six different formulas. Carotid artery ultrasound imaging was performed in 1628 subjects. The CSA of the right and left common carotid artery (CCA) were calculated and used as surrogates of arterial wall mass and hypertrophy. Aortic stiffness was evaluated in 1763 subjects by measuring the cf-PWV. Finally, 218 subjects underwent echocardiographic examination for the assessment of LVM. Among the examined methods of MAP calculation, the formula MAP1=[diastolic BP]+0.412 × [pulse pressure] yielded the strongest correlations with the LVM, cf-PWV and CSA of the right and left CCA, even after adjusting for age and gender. The MAP calculation using the 0.412 was superior compared with the traditional formula that uses the 0.33 for the discrimination of subjects with left ventricular and carotid wall hypertrophy, as well as subjects with increased aortic stiffness. MAP estimated with the 0.412 is better correlated with target organ deterioration compared with other formulas. Future studies are needed to explore the accuracy of these formulas for MAP estimation compared with direct intra-arterial BP measurement.
Similar content being viewed by others
Introduction
Mean arterial blood pressure (MAP) is the major hemodynamic determinant of tissue perfusion regardless of pulse pressure, and it is also a key parameter that influences cardiac function and the wall properties of central arteries. Higher MAP levels are related to cardiovascular (CV) disease and target organ damage, whereas low levels may be detrimental in hemodynamically unstable, critically ill patients. Beyond the pathophysiological and clinical relevance of MAP, there are many circumstances in which a MAP calculation is required, such as the determination of peripheral vascular resistance, fractional pulse pressure, calibration of devices that estimate central blood pressure (BP) and others.1, 2, 3, 4
Undoubtedly, it is essential to estimate MAP values accurately. The gold-standard method for the measurement of the ‘actual’ value of MAP is the calculation of the area under the BP waveform, as determined by the time-averaged BP values over the cardiac cycle, which is recorded invasively by catheter-manometer systems. However, in routine clinical practice, MAP is estimated non-invasively either by using the internal proprietary algorithms of automated oscillometric sphygmomanometers or by mathematical formulas. The accuracy of MAP estimation using oscillometric devices is rarely reported in the literature, and most importantly, several commercial devices do not report MAP, but use it to calculate the systolic and diastolic BP via proprietary algorithms.
Pressure waveforms differ along the arterial tree due to wave propagation and reflection phenomena. The change in the shape of pressure waves can be quantified via the so-called ‘form factor,’ which characterizes the ratio of the difference between its mean and minimum values over the amplitude of a wave.5 Therefore, the form factor not only quantifies the shape of the wave, but it also expresses the percentage of pulse pressure to add to diastolic blood pressure (DBP) to estimate MAP.
On the basis of the concept of ‘form factor,’ several equations have been proposed for the calculation of MAP, as reported in Table 1. In 1939, Wezler and Bögerr6 proposed the formula MAP=0.42 × SBP+0.58 × DBP, where SBP is the systolic and DBP is the diastolic BP. Meaney et al.7 proposed an alternative expression of the above formula as follows: MAP1=DBP+0.412 × PP, where PP is the pulse pressure. The most common and widely used formula for MAP calculation is that proposed by Gauer in 1960:8 MAP2=DBP+0.33 × PP. In 1999, Chemla et al.9 proposed an improvement for the traditional formula, with MAP3=DBP+0.33 × PP+5 mm Hg. Razminia et al.10 in 2004 included the heart rate in the equation for MAP calculation as follows: MAP4=DBP+[0.33+(0.0012 × HR)] × PP. In essence, these formulas differ in the coefficient used to integrate PP in the algorithm, which actually represents the form factor of the pressure waveform.2 Chemla et al.,11 in 2005, proposed a different mathematical equation based on the product of SBP by DBP: MAP5=(SBP × DBP)½. MAP can also be calculated by the integration of pressure waveforms recorded non-invasively (that is, applanation tonometry) and calibrated by brachial SBP and DBP values (MAP6).12 Finally, in the present analysis, the ‘original’ MAP (MAP7), as provided by the proprietary algorithm of a commercially available automated oscillometric device, was also examined.
Currently, there is no consensus regarding which formula yields the most accurate MAP estimation, although MAP2 is the most popular and widely used equation. In addition, there is a lack of evidence regarding which of these different MAP estimates is better associated with target organ damage. The objective of this study was to assess the differences among the original MAP values provided by a commercially available automated oscillometric device and the various MAP levels calculated using different formulas (Table 1). We also determined which method provides MAP values that are more closely associated with target organ characteristics and deterioration as expressed by the left ventricular mass, carotid wall thickness and stiffness of the aorta. Because aging and gender significantly modulate the form factor of the pressure waveform, these two parameters were taken into particular consideration in the present analysis.
Methods
Study population
The study population consisted of 1878 subjects (Caucasians) who were referred to the Cardiovascular Research Laboratory of the First Deptartment of Propaedeutic and Internal Medicine, Laiko University Hospital for CV risk assessment due to the presence of either classical and/or novel chronic inflammatory diseases. The population characteristics are shown in Table 2. All subjects had a normal sinus rhythm. Subjects with arrhythmia and severe obesity (body mass index >40 kg m−2) were excluded from the study because applanation arterial tonometry and pulse-wave analysis were not feasible or had an unacceptable quality. All subjects were examined in a quiet, temperature-controlled environment (22–25 °C). According to laboratory routine practice, patients under pharmaceutical treatment were advised to abstain from their medication for at least 10 h prior to the examination, as well as to abstain from alcohol, caffeinated beverages or any other vasoactive substances for at least 3 h. The study protocol complied with the declarations of Helsinki and was approved by the institutional scientific committee. All subjects gave informed consent before entering the study.
Blood pressure measurement at the brachial artery
Brachial BP was assessed at the supine position after at least 10 min of rest. Triple brachial BP recording was performed (with 1-min interval between readings) in the right arm with a validated automated oscillometric device (Microlife WatchBP Office, Microlife AG, Widnau, Switzerland).13 The average value of the three BP readings (for SBP and DBP) was used for the calculation of MAP values using the examined methods (Table 1).
Non-invasive recording of continuous blood pressure waves
MAP was also determined by the integration of calibrated radial pressure waves recorded by applanation tonometry, which was performed immediately after the BP triple measurement. In particular, continuous pressure waves were recorded by a high-fidelity tonometer (Millar Instruments, Houston, TX, USA), and an averaged single pressure wave was determined using the Sphygmocor Software (Atcor Medical, West Ryde, Australia). In addition, the average value for the heart rate was determined by the system based on the cardiac periods of the recorded pressure waves, and this value was used for the calculation of MAP4. The acquired tonometric waves were calibrated using the respective SBP and DBP levels measured at the brachial artery. The calibration of radial pressure waves using brachial SBP and DBP measured by cuff oscillometry assumes that the brachial BP is equal to the radial BP. However, this assumption may not be accurate because it is possible to have an amplification of the SBP between the brachial and radial artery.5
Left ventricular mass assessment
Left ventricular mass (LVM) and hypertrophy (LVH) were assessed as previously described.14 In brief, transthoracic echocardiography was performed in all patients by the same operator using a high-end ultrasound system (Vivid 7 Pro, General Electric, Fairfield, CT, USA) in accordance with the American Society of Echocardiography (ASE) and European Association of Echocardiography guidelines and recommendations.15 Measurements for the M-mode-guided calculation of LVM were recorded in the parasternal short-axis view. LVM was further standardized to body size, providing the LVM index (LVMI). LVMI was calculated by the ratio of LVM to body surface area (BSA), where BSA=[(weight × height)/3600]0.5.
Carotid wall hypertrophy
Carotid wall CSA, instead of intima-medial thickness, was used as a more comprehensive index of the arterial wall volume or mass because it is closer to arterial hypertrophy16 using a previously applied formula.17 Briefly, the common carotid artery was scanned for the presence of plaques. The average intimal-medial thickness of a plaque-free segment of the common carotid artery (1 cm proximally to the bifurcation) was measured by a dedicated inbuilt software (Vivid 7 Pro). Two sequential CSA of the same common carotid segment were analyzed, and their mean value was used in the analysis.
Assessment of aortic stiffness
Aortic stiffness was assessed by measuring the carotid-to-femoral pulse-wave velocity (cf-PWV) as previously described.18 In brief, cf-PWV is calculated by the ratio of the estimated pulse transit time and the distance travelled by the pressure wave between the two recording sites. Several methods exist for pulse transit time estimation, which may often yield divergent results.19 In this study, we used the tangential (or intersecting tangents) method, which was implemented at the SphygmoCor system (AtCor Medical, Sydney, Australia). At first, the travel distance of the pressure wave was determined as the distance from the suprasternic notch to the femoral artery minus the distance from the carotid artery to the suprasternic notch. Then, arterial pressure waves were recorded by applanation tonometry using a high-fidelity hand-held tonometer (SPT-301, Millar Instruments). Pressure waves were first recorded at the carotid artery and then, within a few seconds, at the femoral artery. The time delay between the two waves (transit time) was determined using registration with a simultaneously recorded ECG. All recordings were made at the supine position. At least two repeated measurements of PWV were performed, and their average value was used in the analysis as previously recommended.20
Assessment of target organ deterioration
The following indices were considered as indicators of target organ deterioration:
-
LVH defined as LVMI values >95 g m−2 in women or >115 g m−2 in men using the ASE formula.15
-
Increased aortic stiffness, defined as cf-PWV >10 m s−1.21
-
Carotid wall hypertrophy, defined arbitrarily by the 4th upper quartile of CSA-RCCA or CSA-LCCA values.
All vascular studies were performed by the same experienced operator using the same device for each examination.
Statistical analysis
The agreement between different MAP estimations was assessed using the Bland and Altman analysis.22 According to this method, the differences between the two measurements (bias)=(MAPi−MAPj) are plotted against their mean value, (MAPi+MAPj)/2. The s.d. of the differences between the two different MAP estimates was also determined. Furthermore, we used the Pearson correlation coefficient (r), intraclass correlation coefficient (ICC) and coefficient of variation (CVar) to assess the agreement, consistency and variation between different MAP estimates. These statistical methods and parameters were described thoroughly elsewhere.23, 24 The bivariate association of each MAP estimate with parameters assessing the target organs (LV and carotid wall mass as well as cf-PWV) was evaluated using the Pearson correlation coefficient. Further multivariate regression models were used to adjust the relationship of MAP with each parameter of target organ deterioration for age and gender. Williams’ statistic, which is often noted as Steiger’s Z-test, was used to compare the correlation coefficients of cardiovascular parameters with MAP values. Receiver operating characteristic (ROC) curve analysis was used to determine the comparative ability of different MAP estimates to discriminate subjects with target organ damage. Areas under the ROC curves were compared based on the methodology proposed by DeLong, DeLong and Clarke-Pearson.25 All tests were two-tailed, and statistical significance was indicated by P-values<0.05. Statistical analysis was performed using SPSS 20 (IBM Corp., Armonk, NY, USA).
Results
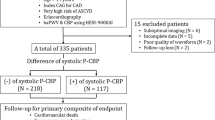
The demographic, clinical and hemodynamic characteristics of the study population are reported in Table 2. The MAP values estimated using the seven different formulas/methods were compared with each other. The statistical parameters indicating variation and agreement between different MAP estimates are shown in Table 3. The mean±s.d. value of the MAP values determined by each formula is depicted in Figure 1. The mean differences and s.d. of differences between each pair of different estimates for MAP are presented in Figure 2.
Mean differences and s.d. of differences from paired comparisons between MAP estimates derived by different methods/formulas as defined in Table 1. A full color version of this figure is available at Hypertension Research journal online.
Association of each MAP estimate with cardiovascular parameters
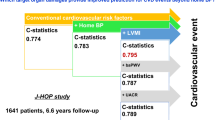
The bivariate correlations of each MAP estimate with LVMI, carotid wall mass and aortic stiffness are reported in Table 4. All MAP estimates are correlated with all of the examined cardiac and vascular parameters (P<0.01). Among the seven different MAP estimates, MAP1 yielded the strongest correlation with all three cardiovascular parameters. MAP7 provided the lowest correlation coefficient. We compared the correlation coefficient of LVMI with MAP1 (r=0.212) with the respective correlation coefficient of LVMI with the traditional MAP2 estimate (r=0.202). The two correlation coefficients were marginally not significantly different (P=0.052). The correlation coefficients of MAP1 with CSA-LCCA (r=0.35) and CSA-RCCA (r=0.365) were higher (P<0.001) than the respective coefficients of MAP2 (r=0.332 and r=0.344). Finally, the correlation of MAP1 with cf-PWV (r=0.441) was significantly stronger than the respective correlation (r=0.415) with MAP2 (P<0.001). MAP1 yielded significantly higher correlation coefficients with LVMI, the CSA of the right and left common carotid artery, as well as with cf-PWV compared with the MAP7 value estimated by the internal algorithm of the automated oscillometric device used in this study. The correlation coefficients of MAP1 with cardiovascular parameters were compared only with those of MAP2 because the latter provided the closest results to the former compared with the remaining MAP3,4,5,6,7 values.
The relationship of each MAP estimate with the parameters of target organ damage was further assessed after adjusting for age and gender (Table 5). MAP1 was, still, better associated with LVMI, CSA-LCCA, CSA-RCCA and cf-PWV compared with the traditional formula (MAP2).
Association of MAP1 and MAP2 estimates with target organ deterioration
Assessment of the comparative ability of MAP1 and MAP2 to discriminate target organ deterioration was performed by ROC curve analysis. MAP1 had a greater ability than MAP2 to discriminate LV hypertrophy and carotid wall hypertrophy (cross-sectional area at the fourth quartile of the studied population) as well as aortic stiffness (defined by cf-PWV values greater than 10 m s−1), as shown by the larger areas under the ROC curves (Table 6).
Discussion
The present study evaluated, for the first time, the association of 7 different MAP estimates using various methods (formulas) with LVM, carotid wall mass and aortic stiffness. The formula proposed by Meaney et al., MAP1=DBP+0.412 × PP,7 provided MAP values better related to these cardiovascular parameters than the respective MAP values estimated using the classic formula, MAP2=DBP+0.33 × PP. Furthermore, MAP1 was a better discriminator than MAP2 for subjects with left ventricular and carotid wall hypertrophy, as well as with increased aortic stiffness. The other MAP estimates (MAP3,4,5,6,7) were less able to discriminate subjects with target organ deterioration.
Physiological and clinical relevance of mean arterial blood pressure
The mean arterial BP is the actual driving pressure for peripheral blood flow and is, physiologically, a better indicator of perfusion to vital organs than systolic blood pressure. MAP values together with measures of cardiac output permit the estimation of peripheral resistance. When MAP is perturbed from the regulated level, cardiac output and total peripheral resistance are adjusted to restore MAP back to the appropriate level. This regulation occurs due to the reflex of baroreceptors, which are located in the carotid sinus and also in the aortic arch and ventricles.
In some populations, MAP is a stronger determinant of LV structural features compared with other BP parameters.26 Moreover, in specific populations, MAP may be more accurate in predicting cardiovascular prognosis than other BP parameters, such as systolic and diastolic pressure.27, 28 In addition, mean rather than systolic BP is the preferred metric in the intensive care unit to guide therapy.29 The superiority of MAP over the SBP was also observed in the BOSHI study,30 which compared measurements of maternal home BP with clinic BP before 20 weeks of gestation to determine associations with the risk of delivering a lower-birth-weight infant. It was reported that high maternal home DBP and MAP, but not SBP, before 20 weeks of gestation was independently associated with a higher risk of lower infant birth weight than clinic DBP and MAP.30
In clinical practice, there are several situations in which it is essential to monitor MAP levels. For example, in patients with sepsis, vasopressors are often titrated based on the MAP. According to the guidelines of the Surviving Sepsis Campaign,31 it is recommended that MAP should be maintained ⩾65 mm Hg. In addition, treatment of patients with stroke or head injury may depend on the patient’s MAP, whereas the admission MAP, as assessed using the form factor 0.3, in patients with stroke is an important parameter.32 Another recent but critical application of MAP is the calibration of devices for the noninvasive estimation of central aortic BP.33, 34, 35 A common method for the calibration of recorded arterial pulse waves relies on the use of MAP and DBP values, which strongly affect the accuracy of measurements.36
However, until now, clinical practice has traditionally relied on the noninvasive auscultatory method to measure SBP and DBP. By contrast, MAP constitutes the sole parameter physically measured by the most current oscillometric techniques, but these values are often not reported. Thus, alternatively, MAP is calculated using a formula, most often one of those examined in this study. It should be noted, however, that current practice guidelines have been slow to integrate MAP evaluation in vital sign monitoring. For example, Cardiology and Hypertension Societies define hypertension based on SBP and DBP measurements only.37 By contrast, the Society for Critical Care Medicine38 has utilized both systolic and mean arterial blood pressure for defining sepsis-induced hypotension, whereas MAP is used as a therapeutic target.
Association of MAP with target organ deterioration
In this study, we found that MAP is positively associated with LVM, which is consistent with previous findings.39, 40, 41 However, the present study showed that the MAP calculation using a form factor of 0.412 is better related to LVM than MAP values derived from the form factor 0.33 (1/3). Furthermore, MAP1 (vs. the traditional MAP2) was a better discriminator of subjects with LV hypertrophy. Similarly, all MAP values were positively related with the right and left carotid wall mass, which is consistent with previous studies,42, 43, 44 but again, MAP1 was the strongest determinant of the carotid wall mass. Finally, aortic stiffness, as assessed by carotid-to-femoral PWV, was positively related with MAP levels.45, 46 MAP1 yielded the highest correlation coefficient and was also a better discriminator of subjects with increased aortic stiffness (PWV>10 m s−1). Of the seven examined methods for MAP estimation, the internal proprietary algorithm of the utilized automated oscillometric device provided MAP values, which had the lowest association with the parameters of target organ damage.
Notably, all formulas using a single form factor for the estimation of MAP based on brachial BP measurements have inherent flaws when applied to different populations. However, in the Asklipeios Study,5 Segers et al. found that the values of the form factor at the brachial artery for different age groups and gender are close to the value of 0.4. Furthermore, there is a non-negligible amplification of SBP between the brachial and the radial artery,5 which suggests that the use of the MAP6 method may include an additional source of error in MAP estimation. More importantly, in a previous invasive study providing intra-arterial pressures at the brachial artery, it was observed that the mean pressure at the upper arm is underestimated when calculated using the traditional formula of adding one-third of the pulse pressure to the diastolic pressure.47 Conversely, this underestimation can be avoided by adding 40% of the pulse pressure to the diastolic pressure,47 suggesting that the use of the form factor 0.4 yields more accurate MAP estimations compared to invasive measurements. The above studies5, 47 further support our findings. Undoubtedly, invasive studies are needed to examine the accuracy of the various methods and techniques for the noninvasive estimation of MAP and larger scale studies are needed in different populations to further determine whether the most accurate MAP estimation is translated to superior clinical relevance.
Limitations
This study did not evaluate the accuracy of each different MAP estimation, which could ideally be achieved by comparison of the estimated MAP values with directly measured MAP through the intra-arterial, continuous recording of blood pressure waves. Therefore, substantial and thorough reasoning for which method of MAP estimation should be considered the most accurate cannot be derived by the present analysis. Consequently, these findings regarding the highest correlation to target organ deterioration should not be confused with better accuracy.
Unfortunately, LVM was assessed only in a small number of patients (N=218) compared to the total population (N=1878). In addition, there were no available data with which to test the association of MAP7 with LVM.
Conclusions
In the existing literature, it is evident that MAP is most frequently calculated by the MAP2 formula. This formula is basically derived using the widely applied rule of thumb that assumes a form factor of one-third (33%). However, it has been previously found that ‘this value is too low and that the one-third rule to estimate mean arterial pressure should be reconsidered.’5
In many published studies, which formula was used for the MAP calculation is often unknown. In the present study, we demonstrated that the estimation of MAP using the form factor value 0.412 provides values that are more strongly related with cardiovascular parameters compared with MAP determined by the traditional formula, which uses the form factor value 0.33. More importantly, we found that the parameters of target organ deterioration, such as left ventricular and carotid wall hypertrophy as well as increased aortic stiffness, are better related with MAP1 than MAP2 values. This evidence supports that MAP1 may have a superior diagnostic or even prognostic ability compared with the traditional formula (MAP2), but this should be investigated further. In addition, future invasive validation studies are required to determine the accuracy of the different MAP estimates using the various available formulas compared with intra-arterially measured mean arterial pressures.
References
Nakayama Y, Ueda H, Tsumura K, Yoshimaru K, Hayashi T . Ascending fractional pulse pressure closely relating to large artery function. J Hum Hypertens 2002; 16: 243–247.
Salvi P . Pulse Waves: How Vascular Hemodynamics Affects Blood Pressure. Springer-Verlag. 2012.
Zhu XL, Wang J, Jiang RZ, Teng YC . Pulsatility index in combination with biomarkers or mean arterial pressure for the prediction of pre-eclampsia: Systematic literature review and meta-analysis. Ann Med 2015; 47: 414–422.
Hsu CH, Chang JB, Liu IC, Lau SC, Yu SM, Hsieh CH, Lin JD, Liang YJ, Pei D, Chen YL . Mean arterial pressure is better at predicting future metabolic syndrome in the normotensive elderly: a prospective cohort study in Taiwan. Prev Med 2015; 72: 76–82.
Segers P, Mahieu D, Kips J, Rietzschel E, De Buyzere M, De Bacquer D, Bekaert S, De Backer G, Gillebert T, Verdonck P, Van Bortel L, Asklepios I . Amplification of the pressure pulse in the upper limb in healthy, middle-aged men and women. Hypertension 2009; 54: 414–420.
Wezler K, Böger A . Die Dynamik des arteriellen Systems: Der arterielle Blutdruck und seine Komponenten. Ergebn Physiol 1939; 41: 292–606.
Meaney E, Alva F, Moguel R, Meaney A, Alva J, Webel R . Formula and nomogram for the sphygmomanometric calculation of the mean arterial pressure. Heart 2000; 84: 64.
Gauer O . Kreislauf des Blutes. Lehrbuch der Physiologie des Menschen. Landois L RH-U, editor: Von Urban and Schwarzenberg, 1960.
Chemla D, Hebert JL, Zamani K, Coirault C, Lecarpentier Y . Estimation of mean aortic pressure. Lancet 1999; 354: 596.
Razminia M, Trivedi A, Molnar J, Elbzour M, Guerrero M, Salem Y, Ahmed A, Khosla S, Lubell DL . Validation of a new formula for mean arterial pressure calculation: the new formula is superior to the standard formula. Catheter Cardiovasc Interv 2004; 63: 419–425.
Chemla D, Nitenberg A . A call for improving mean aortic pressure estimation. Am J Hypertens 2005; 18: 891.
O’Rourke MF, Pauca A, Jiang XJ . Pulse wave analysis. Br J Clin Pharmacol 2001; 51: 507–522.
Stergiou GS, Tzamouranis D, Protogerou A, Nasothimiou E, Kapralos C . Validation of the Microlife Watch BP Office professional device for office blood pressure measurement according to the International protocol. Blood Press Monit 2008; 13: 299–303.
Protogerou AD, Argyris AA, Papaioannou TG, Kollias GE, Konstantonis GD, Nasothimiou E, Achimastos A, Blacher J, Safar ME, Sfikakis PP . Left-ventricular hypertrophy is associated better with 24-h aortic pressure than 24-h brachial pressure in hypertensive patients: the SAFAR study. J Hypertens 2014; 32: 1805–1814.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise J, Solomon S, Spencer KT, John Sutton M St, Stewart W American Society of Echocardiography’s N, Standards C, Task Force on Chamber Q, American College of Cardiology Echocardiography C, American Heart A, European Association of Echocardiography ESoC. Recommendations for chamber quantification. Eur J Echocardiogr 2006; 7: 79–108.
Roman MJ, Devereux RB, Schwartz JE, Lockshin MD, Paget SA, Davis A, Crow MK, Sammaritano L, Levine DM, Shankar BA, Moeller E, Salmon JE . Arterial stiffness in chronic inflammatory diseases. Hypertension 2005; 46: 194–199.
Roman MJ, Pickering TG, Schwartz JE, Pini R, Devereux RB . Relation of arterial structure and function to left ventricular geometric patterns in hypertensive adults. J Am Coll Cardiol 1996; 28: 751–756.
Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, Pannier B, Vlachopoulos C, Wilkinson I, Struijker-Boudier H European Network for Non-invasive Investigation of Large A. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 2006; 27: 2588–2605.
Papaioannou TG, Vardoulis O, Protogerou A, Konstantonis G, Sfikakis PP, Stefanadis C, Stergiopulos N . In vivo evaluation of a novel ‘diastole-patching’ algorithm for the estimation of pulse transit time: advancing the precision in pulse wave velocity measurement. Physiol Meas 2015; 36: 149–161.
Papaioannou TG, Protogerou AD, Nasothimiou EG, Tzamouranis D, Skliros N, Achimastos A, Papadogiannis D, Stefanadis CI . Assessment of differences between repeated pulse wave velocity measurements in terms of ‘bias’ in the extrapolated cardiovascular risk and the classification of aortic stiffness: is a single PWV measurement enough? J Hum Hypertens 2012; 26: 594–602.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F Task Force M 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013; 31: 1281–1357.
Bland JM, Altman DG . Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1: 307–310.
Papaioannou TG, Argyris A, Protogerou AD, Vrachatis D, Nasothimiou EG, Sfikakis PP, Stergiou GS, Stefanadis CI . Non-invasive 24 hour ambulatory monitoring of aortic wave reflection and arterial stiffness by a novel oscillometric device: the first feasibility and reproducibility study. Int J Cardiol 2013; 169: 57–61.
Bartko JJ . The intraclass correlation coefficient as a measure of reliability. Psychol Rep 1966; 19: 3–11.
DeLong ER, DeLong DM, Clarke-Pearson DL . Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988; 44: 837–845.
Rosendorff C, Go O, Schmeidler J, Silverman JM, Beeri MS . Correlation of arterial blood pressure and compliance with left ventricular structure and function in the very elderly. J Am Soc Hypertens 2012; 6: 48–55.
Avanzini F, Alli C, Boccanelli A, Chieffo C, Franzosi MG, Geraci E, Maggioni AP, Marfisi RM, Nicolosi GL, Schweiger C, Tavazzi L, Tognoni G, Valagussa F, Marchioli R . Investigators GI-P. High pulse pressure and low mean arterial pressure: two predictors of death after a myocardial infarction. J Hypertens 2006; 24: 2377–2385.
Zheng L, Sun Z, Li J, Yu J, Wei Y, Zhang X, Liu S, Li J, Xu C, Hu D, Sun Y . Mean arterial pressure: a better marker of stroke in patients with uncontrolled hypertension in rural areas of China. Intern Med 2007; 46: 1495–1500.
Lehman LW, Saeed M, Talmor D, Mark R, Malhotra A . Methods of blood pressure measurement in the ICU. Crit Care Med 2013; 41: 34–40.
Iwama N, Metoki H, Ohkubo T, Ishikuro M, Obara T, Kikuya M, Yagihashi K, Nishigori H, Sugiyama T, Sugawara J, Yaegashi N, Hoshi K, Suzuki M, Kuriyama S, Imai Y Group BS. Maternal clinic and home blood pressure measurements during pregnancy and infant birth weight: the BOSHI study. Hypertens Res 2015; 39: 151–157.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb S, Beale RJ, Vincent JL, Moreno R . Surviving Sepsis Campaign Guidelines Committee including The Pediatric S. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 2013; 39: 165–228.
Eizenberg Y, Koton S, Tanne D, Grossman E . Association of age and admission mean arterial blood pressure in patients with stroke-data from a national stroke registry. Hypertens Res 2016; 39: 356–361.
Papaioannou TG, Protogerou AD, Stamatelopoulos KS, Vavuranakis M, Stefanadis C . Non-invasive methods and techniques for central blood pressure estimation: procedures, validation, reproducibility and limitations. Curr Pharm Des 2009; 15: 245–253.
Salvi P, Grillo A, Parati G . Noninvasive estimation of central blood pressure and analysis of pulse waves by applanation tonometry. Hypertens Res 2015; 38: 646–648.
Martin JS, Borges AR, Christy JBt, Beck DT . Considerations for SphygmoCor radial artery pulse wave analysis: side selection and peripheral arterial blood pressure calibration. Hypertens Res 2015; 38: 675–683.
Laugesen E, Rossen NB, Peters CD, Maeng M, Ebbehoj E, Knudsen ST, Hansen KW, Botker HE, Poulsen PL . Assessment of central blood pressure in patients with type 2 diabetes: a comparison between SphygmoCor and invasively measured values. Am J Hypertens 2014; 27: 169–176.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Redon J, Dominiczak A, Narkiewicz K, Nilsson PM, Burnier M, Viigimaa M, Ambrosioni E, Caufield M, Coca A, Olsen MH, Schmieder RE, Tsioufis C, van de Borne P, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Clement DL, Coca A, Gillebert TC, Tendera M, Rosei EA, Ambrosioni E, Anker SD, Bauersachs J, Hitij JB, Caulfield M, De Buyzere M, De Geest S, Derumeaux GA, Erdine S, Farsang C, Funck-Brentano C, Gerc V, Germano G, Gielen S, Haller H, Hoes AW, Jordan J, Kahan T, Komajda M, Lovic D, Mahrholdt H, Olsen MH, Ostergren J, Parati G, Perk J, Polonia J, Popescu BA, Reiner Z, Ryden L, Sirenko Y, Stanton A, Struijker-Boudier H, Tsioufis C, van de Borne P, Vlachopoulos C, Volpe M, Wood DA . 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013; 34: 2159–2219.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb SA, Beale RJ, Vincent JL, Moreno R . Surviving Sepsis Campaign Guidelines Committee including the Pediatric S. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med 2013; 41: 580–637.
Corea L, Bentivoglio M, Verdecchia P . Echocardiographic left ventricular hypertrophy as related to arterial pressure and plasma norepinephrine concentration in arterial hypertension. Reversal by atenolol treatment. Hypertension 1983; 5: 837–843.
Mittal SR . Mean arterial pressure may affect LV mass even when clinic BP is 120/80 mm Hg or less. J Assoc Physicians India 2013; 61: 713–715.
Atas N, Erten Y, Okyay GU, Inal S, Topal S, Onec K, Akyel A, Celik B, Tavil Y, Bali M, Arinsoy T . Left ventricular hypertrophy and blood pressure control in automated and continuous ambulatory peritoneal dialysis patients. Ther Apher Dial 2014; 18: 297–304.
Poyrazoglu HM, Dusunsel R, Yikilmaz A, Narin N, Anarat R, Gunduz Z, Coskun A, Baykan A, Ozturk A . Carotid artery thickness in children and young adults with end stage renal disease. Pediatr Nephrol 2007; 22: 109–116.
Maple-Brown L, Hodge A, Cunningham J, Celermajer DS, O’Dea K . Risk factors for cardiovascular disease do not fully explain differences in carotid intima-media thickness between Indigenous and European Australians without diabetes. Clin Endocrinol (Oxf) 2009; 71: 189–194.
Rogowicz-Frontczak A, Araszkiewicz A, Pilacinski S, Zozulinska-Ziolkiewicz D, Wykretowicz A, Wierusz-Wysocka B . Carotid intima-media thickness and arterial stiffness in type 1 diabetic patients are dependent on age and mean blood pressure. Exp Clin Endocrinol Diabetes 2011; 119: 281–285.
Demirci MS, Gungor O, Kircelli F, Carrero JJ, Tatar E, Demirci C, Kayikcioglu M, Asci G, Toz H, Ozkahya M, Ok E . Impact of mean arterial pressure on progression of arterial stiffness in peritoneal dialysis patients under strict volume control strategy. Clin Nephrol 2012; 77: 105–113.
Cypiene A, Dadoniene J, Rugiene R, Ryliskyte L, Kovaite M, Petrulioniene Z, Venalis A, Laucevicius A . The influence of mean blood pressure on arterial stiffening and endothelial dysfunction in women with rheumatoid arthritis and systemic lupus erythematosus. Medicina (Kaunas) 2010; 46: 522–530.
Bos WJ, Verrij E, Vincent HH, Westerhof BE, Parati G, van Montfrans GA . How to assess mean blood pressure properly at the brachial artery level. J Hypertens 2007; 25: 751–755.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Papaioannou, T., Protogerou, A., Vrachatis, D. et al. Mean arterial pressure values calculated using seven different methods and their associations with target organ deterioration in a single-center study of 1878 individuals. Hypertens Res 39, 640–647 (2016). https://doi.org/10.1038/hr.2016.41
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.41
Keywords
This article is cited by
-
Single-Field Fundus Photography for Screening of Diabetic Retinopathy: The Prevalence and Associated Factors in a Population-Based Study
Diabetes Therapy (2023)
-
Impact of arterial location, pressure wave indicators, and measurement devices on arterial form factor and mean and central arterial pressure
Journal of Human Hypertension (2022)
-
A Prospective Study to Determine the Predictive Ability of HDP-Gestosis Score for the Development of Pre-eclampsia
The Journal of Obstetrics and Gynecology of India (2022)
-
Altered cardiac structure and function in newly diagnosed people living with HIV: a prospective cardiovascular magnetic resonance study after the initiation of antiretroviral treatment
The International Journal of Cardiovascular Imaging (2022)
-
Association of cardio-ankle vascular index with blood pressure indices: mathematical and methodological perspectives
Journal of Human Hypertension (2020)