Abstract
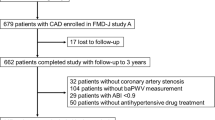
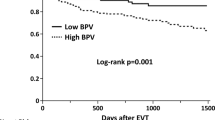
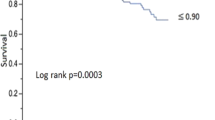
Peripheral blood pressure (PBP) is usually higher than central blood pressure (CBP) due to pulse amplification; however, it is not well understood why cuff-measured PBP can be lower than CBP estimated by the late systolic pressure of radial pulse waves. We explored the implications of systolic PBP–CBP (P-CBP) differences for cardiovascular (CV) prognosis. In total, 335 patients at very high risk of atherosclerotic cardiovascular disease (ASCVD) underwent automated applanation tonometry and brachial-ankle pulse wave velocity (baPWV), and they were classified into groups according to positive or negative systolic P-CBP differences. Between-group characteristics and clinical outcomes (the composite of coronary revascularization, stroke, heart failure hospitalization, and CV death) were evaluated. Patients with negative differences had significantly higher frequency of hypertension, coronary artery disease, higher ASCVD risk burden, and elevated N-terminal pro b-type natriuretic peptide. They had higher left atrial volume index (LAVI) and lower systolic mitral septal tissue velocity (TVI-s’) than those with a positive difference. These patients showed higher systolic PBP and CBP, and a higher baPWV. Multivariable analysis indicated that TVI-s’, LAVI, and ASCVD risk burden were independent determinants of such systolic P-CBP differences. During a median follow-up of 12.6 months, clinical outcomes were significantly related to a negative difference (11.5% vs. 3.4%, p = 0.014), and a systolic P-CBP difference ≤ −8 mmHg was associated with a threefold higher likelihood of poor prognosis. In patients at very high risk of ASCVD, systolic P-CBP difference was associated with cardiac dysfunction and ASCVD risk burden, allowing further risk stratification.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73:3168–209.
Yandrapalli S, Gupta S, Andries G, Cooper HA, Aronow WS. Drug therapy of dyslipidemia in the elderly. Drugs Aging. 2019;36:321–40.
Williams B, Lacy PS, Thom SM, Cruickshank K, Stanton A, Collier D, et al. Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation. 2006;113:1213–25.
Ryuzaki M, Morimoto S, Niiyama M, Seki Y, Yoshida N, Oshima Y, et al. The relationships between the differences in the central blood pressure and brachial blood pressure and other factors in patients with essential hypertension. Intern Med. 2017;56:587–96.
Sharman J, Stowasser M, Fassett R, Marwick T, Franklin S. Central blood pressure measurement may improve risk stratification. J Hum Hypertens. 2008;22:838–44.
Wang KL, Cheng HM, Chuang SY, Spurgeon HA, Ting CT, Lakatta EG, et al. Central or peripheral systolic or pulse pressure: which best relates to target organs and future mortality? J Hypertens. 2009;27:461–7.
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082–143.
Takazawa K, Kobayashi H, Shindo N, Tanaka N, Yamashina A. Relationship between radial and central arterial pulse wave and evaluation of central aortic pressure using the radial arterial pulse wave. Hypertens Res. 2007;30:219–28.
Clark TG, Altman DG, De, Stavola BL. Quantification of the completeness of follow-up. Lancet. 2002;359:1309–10.
Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJ, Michelson EL, et al. Effects of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM-Overall program. Lancet. 2003;362:759–66.
Narayan O, Parker KH, Davies JE, Hughes AD, Meredith IT, Cameron JD. Reservoir pressure analysis of aortic blood pressure: an in-vivo study at five locations in humans. J Hypertens. 2017;35:2025–33.
Hametner B, Wassertheurer S, Hughes AD, Parker KH, Weber T, Eber B. Reservoir and excess pressures predict cardiovascular events in high-risk patients. Int J Cardiol. 2014;171:31–6.
Miyashita H. Clinical assessment of central blood pressure. Curr Hypertens Rev. 2012;8:80–90.
Wang JJ, O’Brien AB, Shrive NG, Parker KH, Tyberg JV. Time-domain representation of ventricular-arterial coupling as a windkessel and wave system. Am J Physiol Heart Circ Physiol. 2003;284:H1358–68.
Cui R, Li Y, Krisztina G, Yamagishi K, Umesawa M, Imano H, et al. An association between central aortic pressure and subclinical organ damage of the heart among a general Japanese cohort: Circulatory Risk in Communities Study (CIRCS). Atherosclerosis. 2014;232:94–8.
Hirata K, Kojima I, Momomura S. Noninvasive estimation of central blood pressure and the augmentation index in the seated position: a validation study of two commercially available methods. J Hypertens. 2013;31:508–15.
Davies JE, Lacy P, Tillin T, Collier D, Cruickshank JK, Francis DP, et al. Excess pressure integral predicts cardiovascular events independent of other risk factors in the conduit artery functional evaluation substudy of Anglo-Scandinavian Cardiac Outcomes Trial. Hypertension. 2014;64:60–8.
Piskorski J, Krauze T, Katulska K, Wykrętowicz M, Milewska A, Przymuszała D, et al. Contribution of arterial excess pressure and arterial stiffness to central augmentation pressure in healthy subjects. Int J Cardiol. 2013;168:2899–900.
Bulas J, Potocarova M, Kupcova V, Gaspar L, Wimmer G, Murin J. Central systolic blood pressure increases with aortic stiffness. Bratisl Lek Listy. 2019;120:894–8.
Schultz MG, Hughes AD, Davies JE, Sharman JE. Associations and clinical relevance of aortic-brachial artery stiffness mismatch, aortic reservoir function, and central pressure augmentation. Am J Physiol Heart Circ Physiol. 2015;309:H1225–33.
Zhang Y, Li Y, Ding FH, Sheng CS, Huang QF, Wang JG. Cardiac structure and function in relation to central blood pressure components in Chinese. J Hypertens. 2011;29:2462–8.
Rossi A, Vassanelli C. Left atrium: no longer neglected. Ital Heart J. 2005;6:881–5.
Chirinos JA, Phan TS, Syed AA, Hashmath Z, Oldland HG, Koppula MR, et al. Late systolic myocardial loading is associated with left atrial dysfunction in hypertension. Circ Cardiovasc Imaging. 2017;10:e006023.
Chirinos JA, Segers P, Hughes T, Townsend R. Large-artery stiffness in health and disease: JACC state-of-the-art review. J Am Coll Cardiol. 2019;74:1237–63.
Cauwenberghs N, Hedman K, Kobayashi Y, Vanassche T, Haddad F, Kuznetsova T. The 2013 ACC/AHA risk score and subclinical cardiac remodeling and dysfunction: complementary in cardiovascular disease prediction. Int J Cardiol. 2019;297:67–74.
Kim G, Kim JH, Moon KW, Yoo KD, Kim CM, Moon D, et al. The relationships between the arterial stiffness index measured at the radial artery and left ventricular diastolic dysfunction in asymptomatic high risk patients without atherosclerotic cardiovascular disease. Int Heart J. 2016;57:73–9.
Picone DS, Schultz MG, Otahal P, Black JA, Bos WJ, Chen CH, et al. Influence of age on upper arm cuff blood pressure measurement. Hypertension. 2020;75:844–50.
Carlsen RK, Peters CD, Khatir DS, Laugesen E, Bøtker HE, Winther S, et al. Estimated aortic blood pressure based on radial artery tonometry underestimates directly measured aortic blood pressure in patients with advancing chronic kidney disease staging and increasing arterial stiffness. Kidney Int. 2016;90:869–77.
Boutouyrie P, London GM, Sharman JE. Estimating central blood pressure in the extreme vascular phenotype of advanced kidney disease. Kidney Int. 2016;90:736–9.
Picone DS, Schultz MG, Peng X, Black JA, Dwyer N, Roberts-Thomson P, et al. Discovery of new blood pressure phenotypes and relation to accuracy of cuff devices used in daily clinical practice. Hypertension. 2018;71:1239–47.
Chirinos JA, Sweitzer N. Ventricular-arterial coupling in chronic heart failure. Card Fail Rev. 2017;3:12–8.
Baba BA, Johan PT, Mohan JC. Comparison of central aortic pressure to brachial artery pressure in hypertensive patients on drug treatment: an observational study. Indian Heart J. 2018;70:S208–12.
Armstrong MK, Schultz MG, Picone DS, Black JA, Dwyer N, Roberts-Thomson P, et al. Brachial and radial systolic blood pressure are not the same. Hypertension. 2019;73:1036–41.
Acknowledgements
This research was supported by the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (HI18C0575) in addition to the National Research Foundation of Korea (NRF) by the Korea government (MSIT) (No. 2017R1C1B5017661). The authors would like to also acknowledge J-H Jeon, RN and S-Y Kim, RN for their significant contribution to this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, H., Kim, IC., Hwang, J. et al. Features and implications of higher systolic central than peripheral blood pressure in patients at very high risk of atherosclerotic cardiovascular disease. J Hum Hypertens 35, 994–1002 (2021). https://doi.org/10.1038/s41371-020-00472-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-020-00472-6