Abstract
Several lines of evidence indicate that neutrophils act nonspecifically against tumor cells. The correlation between tumor-infiltrating neutrophils (TINs) and clinicopathological features remains unclear and deserves to be investigated. To analyze the prognostic influence of TINs in gastric carcinoma, the authors selected 273 patients with advanced gastric carcinoma who underwent gastrectomy at Cremona Hospital (Lombardia, Italy) between 1990 and 1995 and followed them for a period of 5 years. The number of TINs was assessed in a semiquantitative manner using the mean value of 20 nonoverlapping high-power fields (magnification, 400×; 0.08 mm2). The patients were divided into two groups: patients with a moderate or extensive amount of TINs (n = 76; >10 TINs per 20 high-power fields) and patients with a minor amount of TINs (n = 197; ≤10 TINs per 20 high-power fields). The Kaplan-Meier method and Greenwood formula were used to estimate the crude survival rates in the two groups. Multivariate analyses based on the Cox proportional hazard regression model were performed to assess the effect of the prognostic factors on survival. Among the potential prognostic factors analyzed by univariate analysis, sex, age, location of neoplasia, pTNM stage, TINs, and surgical curability were significantly associated with higher survival rate. The study of the possible interaction effects of the clinical-pathological factors with TINs reveals that female patients with a moderate or extensive amount of TINs have about a 39% reduction in their risk of mortality, whereas male patients do not seem to be affected by the level of TINs. These results suggest that women appear to have a better prognosis than men in advanced gastric carcinoma. Gender differences in some host defense mechanisms and particularly in neutrophil function may be responsible for this event. Confirmation of these findings would give valuable insights about host reaction to gastric cancer growth and, ultimately, possibly would have implications regarding the identification of low-risk patients who could be spared adjuvant therapy.
Similar content being viewed by others
INTRODUCTION
Gastric cancer is the second-leading cause of cancer death in the world (1). The 5-year survival rate of advanced gastric cancer, when a potentially curative operation has been carried out, is on the order of 20% (2). Gastric carcinomas are frequently characterized by a markedly heterogeneous polynuclear and mononuclear cell infiltrate containing macrophages, granulocytes, various subpopulations of T lymphocytes, and, in some cases, antibody-producing plasma cells and mast cells (3, 4, 5, 6, 7, 8, 9). This tumor may be associated with a high number of tumor-infiltrating neutrophils (TINs) that has been reported in 7.6% of the cases (3, 4).
Neutrophil effects on tumor cells represent opposite sides of a double-edged sword (10). In some experimental tumors, neutrophils are cytolytic and can eliminate tumor cell populations (11), whereas in others, neutrophils contribute to the invasive potential (10, 12). Therefore, the presence of TINs might be indicative for a better or worse host-antitumoral response. A parameter for an immunological host response would be survival. Whether such a relationship exists might be best investigated in those patients with advanced gastric carcinomas because this group has a comparable, relatively low survival rate.
In this article, we report the results of a study carried out in a high-risk area for gastric cancer in northern Italy to clarify the correlation between TINs in advanced gastric carcinoma and clinicopathologic factors, including survival time.
MATERIALS AND METHODS
This study was a hospital-based investigation of the survival of a cohort of patients diagnosed with primary advanced gastric carcinomas. Patients were identified in Cremona, a high-risk area located in northern Italy (13). This is a Phase I, early exploratory study (14), in which the main putative prognostic determinant to be investigated was the density of TINs in the gastric carcinomas. Only deaths due to gastric carcinoma were taken into account, whereas data from patients who died of other causes were treated as censored.
Patients
Between 1990 and 1995, 358 patients had undergone potentially curative surgery for gastric cancer at the Cremona Hospital, USSL 51, Cremona, Italy. The files of the Pathology Service included all of the histologically confirmed gastric cancer cases occurring in the resident population of USSL 51 of Cremona (161,935 inhabitants), which has a death rate from gastric cancer (calculated from data for the period 1977–1979) of 56.6/100,000 inhabitants (males, 73.4/100,000; females, 39.3/100,000; 13).
Patients with gastric carcinoma had received neither chemotherapy nor radiation therapy before surgery. As some information was incomplete, 12 cases were excluded. Patients with gastric carcinomas were followed up to 5 years or until the time of their death, whichever happened earlier. In this latter case, date and cause of death were recorded. To eliminate bias caused by deaths directly resulting from operations, five patients who died within 1 month after surgery were also excluded from the survival analysis.
Pathological Review
The size and location of the tumors were determined after a review of the surgical and gross pathologic findings. Tumors located predominantly in the gastroesophageal junction and cardia were determined to be in the upper third of the stomach; tumors located in the midbody and pylorus were determined to be in the middle third and lower third, respectively. The cancers involving all three gastric portions were considered to be entire-stomach cancers. The resected specimen was subjected to detailed pathological examination, which identified the depth of penetration of the stomach wall, whether the margins were free of tumor, and the presence of secondary deposits in 15 or more lymph nodes and tiers, according to the pTNM system (15). Curative surgery was defined as the removal of all gross tumor and the demonstration of tumor-negative surgical margins by microscopic examination of the total circumference of the gastric resection line (R0 resection according to the pTNM classification). All specimens were fixed in 10% formalin solution, embedded in paraffin, and stained with hematoxylin and eosin (H & E). In each case, there were at least two sample blocks of each tumor, with a range from 3 to 8 blocks per case.
For each case, all available hematoxylin and eosin-stained sections were reviewed to evaluate the tumor type, according to Laurèn classification (16). The Laurèn classification (16) has the following categories: intestinal type, diffuse type, and mixed (e.g., tumors having equal proportions of intestinal and diffuse characteristics, and others with a solid growth pattern). Gastric carcinomas were also grouped into two categories: (1) early gastric cancer, demonstrating invasion into the mucosa or into the mucosa and submucosa only, irrespective of whether or not metastasis to lymph nodes has occurred; and (2) advanced gastric cancer, exhibiting invasion beyond the submucosa, regardless of nodal or distant metastatic status. The results derive from independent histopathologic review by three different pathologists (RAC, GB, CI) on separate occasions. Diagnostic differences between the three pathologists' assessments were resolved by consensus.
Follow-Up
Vital status information was sought for all patients by periodic linkage to Municipal Population Offices and to the Regional Mortality Registry on December 30, 2000. Sixty-eight patients with early gastric cancer were excluded because of the high survival rate, leaving 273 for the final study.
Tracing of patients was practically complete, and the information on vital status at 5 years was available for all but 6 patients. These patients were censored at the date of the last follow-up. At the time of analysis, 74 patients had survived more than 5 years, 159 died of gastric carcinoma or metastasis from this tumor within 5 years, and 34 died of other diseases within 5 years.
Neutrophil Counting
Two representative paraffin blocks were selected for subsequent neutrophil counting after carefully screening for representative pattern of lesion. The H & E-stained sections were examined under low power (40×) to identify the areas of neutrophilic aggregates within the tumor tissue from all tissue blocks. Areas of infarct-like necrosis and areas immediately adjacent to ulcerations were not considered in neutrophil counts. In areas of infarctlike necrosis, there is involvement of both stroma and adenocarcinoma glands, and tumor cells appear only as pale-staining “ ghosts” of their previous viable cytomorphological state.
Ten nonoverlapping fields were examined on two slides in representative areas of a given tumor (i.e., a total of 20 fields per patient). The number of stromal neutrophils was assessed in a semiquantitative manner using the mean value of 20 nonoverlapping high power fields (HPF; magnification of 400×; 0.08 mm2) by using a 40× objective and a square grid mounted in a 10× microscopic eyepiece. After the examination of histograms that revealed the distribution of TINs, the neutrophil counts were divided into three categories based on numbers of neutrophils detected and expressed as minor, moderate, and extensive. When <10 neutrophils were present, it was regarded as a minor amount of TINs. When >50 neutrophils were present, it was considered an extensive amount of TINs. In the moderate group, neutrophils were either seen as a series of “hot spots” scattered throughout the tumor stroma or as a considerable amount, between 10 and 50 neutrophils per HPF. No adjustments to the counting procedures were made to accommodate tumors with large areas of stromal fibrosis. Lymph nodes were assessed as positive or negative for the presence of a substantial amount of neutrophils as well. The specimens were scored by two independent investigators (RAC, LR), who had no knowledge of the other prognostic factors and/or survival. For 90% of the slides, the two observers' evaluations concurred; the remaining slides were reevaluated and consensus decisions were made by means of a double-headed microscope.
Statistical Analysis
Chi-square test was used to compare characteristics between groups. Continuous variables, such as age and cancer size, were categorized in three classes according to Altman et al. (17). The choice of the cut points was guided by biological reason (e.g., age of <50; 50–65; or >65 y) or simplicity (i.e., cancer size categorized at the tertiles: <4 cm; 5–6 cm; >7 cm). Nominal variables were divided into two, three, or four subgroups: sex (male versus female), location (upper, middle, lower, and entire stomach), histological type according to Laurèn (intestinal versus nonintestinal), TINs (minor versus moderate to extensive), pTNM stage (Ib; II; IIIa, b; IV), surgical curability (R0 versus non-R0), and gastric resection (total versus partial).
Survival distribution curves were computed by the Kaplan-Meier method (18) and compared statistically by the log-rank test. The Cox proportional hazards regression model was used to estimate hazard ratios (HRs) of death, both in a univariate and multivariate setting, where the effect of one factor or the combined effects of two or more factors were assessed (19). Confidence intervals (CI) at 95% for HRs were calculated. Model fitting was performed by graphical and test-based techniques with martingale residuals (20)
Univariate and multivariate survival data analyses were performed using STATA 7 (21).
RESULTS
The main clinicopathologic features of our patients are summarized in Table 1. The study population was composed of 161 males (59%) and 112 (41%) females. The median age was 65 (range, 28–85) years. Even though the results are reported stratified by gender, we observe only marginal differences between the two groups.
Infiltration of neutrophils was identified in the intratumoral stroma. In those cases with a minor amount of TINs, neutrophils infiltrated occasionally as single cells into the tumor stroma, and there were not marked differences in neutrophil density between different areas. An extensive amount of TINs consisted of a single massive infiltrate of neutrophils (Fig. 1a). Neutrophil density was similar in deep and superficial portions of the same tumor. Neutrophils could form varied-sized aggregates composed from 3 up to 200 cells (Fig. 1a). In the cases with a moderate amount of TINs, neutrophils were either diffusely scattered as single cells or were seen as a series of “hot spots” in the tumor stroma. Patients with moderate or extensive amount of TINs were regarded as having a significant higher amount of TINs, and these groups were combined in the multivariate analysis (76 cases).
In these 76 cases, lymph node metastasis was observed in 56 cases. In 32 of 56 cases, neutrophil infiltration, similar to that observed in primary tumors, was found in tumor-positive lymph node, whereas in 5 of 20 cases it was also present in tumor-negative lymph node (P = .02). Figures 1a and 1b and show an example of a light-microscopic picture from a patient with an extensive TINs at the primary tumor site and in the tumor-positive lymph node.
Also, patients with tumors localized in the lower and middle third of the stomach were combined in the multivariate analysis, because of a similar survival pattern.
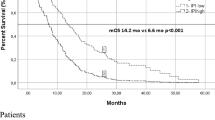
In Table 2 univariate estimates are reported. According to these, gender, age, pTNM stage, TINs, surgical curability, and tumor location were associated with survival and therefore were selected for potential inclusion in a multivariate Cox regression model. In Figure 2, we show the Kaplan-Meier distribution of these factors.
In the first step of multivariate analysis, risk of mortality was lower among female patients younger than 65 years, with curative stages of tumor, and with tumor location in the upper third of the stomach. In the second step, we considered possible interaction effects of the factors under study with TINs. We found that gender significantly changed the effect of TINs on survival time. We do not see any substantial confounding effect between Laurèn histological type and TINs. In the multivariate analysis, female gender and TINs appear to be independent. Histologic type was analyzed by sex, but without significant results. In Table 3, we show gender-stratified results. Female patients with moderate or extensive amount of TINs have about 39% reduction (with a confidence upper bound of 67% and a lower bound of .13%) in their risk of mortality, whereas male patients do not seem to be affected by the level of TINs.
DISCUSSION
The results and inferences of many statistical analyses are extremely sensitive to misclassification, omission, manipulation of data, and error (22). However, bias appears unlikely to explain our findings. A few cases were lost to follow-up during the 5-year period. This study was based on a consecutive series of patients from a single geographic area who were surgically treated for advanced gastric carcinoma. Because of these characteristics, our results cannot be generalized to the overall patient population, and they must be confirmed in multicenter studies. Pathologists who quantified TINs were blinded of follow-up of patients. Therefore, procedures used to recruit and follow these patients seem unlikely to have resulted in a selected or unusual group of patients. In our study, clinical (female sex, age ≤65 y) and morphologic parameters (pTNM stage, residual tumor [R], site of neoplasm) showed a significant correlation with prognosis, whereas no such correlation was observed with tumor histotype, according to Laurèn classification (16). These results are consistent with most other reports concerning prognostic factors in gastric carcinoma and support the reliability of our data.
Although it is well known that the incidence of gastric carcinoma is higher for men than for women, the existence of a sex-specific prognosis has only recently been assessed. In a multicenter study in northern Italy (23), a reduced gastric cancer risk was observed in women with later menopause and longer duration of fertile life. The favorable prognostic value of females, mainly younger patients, has been shown not only in gastric carcinoma (24), but also in tumors of other organs such as lung, liver, and colorectum (25, 26, 27).
Neutrophil count was a significant prognosticator in our study of 273 patients with gastric carcinoma. TINs represent a part of the stromal response to malignant tumors. The mechanism whereby patients with cancer may be associated with moderate or extensive level of TINs is not clear. It can be argued that increasing bulk of carcinoma provides potential for greater tumor necrosis and secondary neutrophil infiltration. In the present study, however, when a multivariate analysis was performed, the high levels of TINs were a significant prognosticator independent of pTNM stage (or size). Furthermore, 56 out of 76 cases of gastric cancer with moderate or extensive TINs showed lymph node metastasis. Presence of neutrophils in lymph node was found in 37 cases, of which 5 were tumor negative (P = .02), suggesting that neutrophil infiltrate is tumor related. Therefore, TINs may reflect a natural cytoxicity of the host against the tumor or may be the result of direct cytokine production by the tumor cells. There are a few studies that analyze the prognostic influences of neutrophils in human carcinomas and the possible associations between this parameter and others with well-known prognostic significance. TINs were not found significantly to be associated with prognosis in colorectal (28) and non-small cell lung (29) cancer. Neutrophil alveolitis was significantly associated with a poorer outcome in patients with bronchioloalveolar carcinoma (30). In our multivariate analysis, the study of possible interaction effects of the clinicopathological factors with TINs revealed that female patients with a moderate or extensive amount of TINs had about a 39% reduction in their risk of mortality. Male patients do not seem to be affected by the level of TINs. A possible explanation for the interaction between TINs and female patients is that sexual dimorphism exists in the immune response (31). Both humoral and cell-mediated immunity are more active in females than in males, and steroid gonadal hormones may play an important role in regulating this response (32). These observations suggest the possibility of an inflammatory (neutrophil) and gender-dependent host natural cytoxicity in the microenvironment of gastric carcinomas. Confirmation of these findings would give valuable insight into gastric cancer growth and, ultimately, has possible implications regarding the selection of low-risk patients who could be spared adjuvant therapy.
References
Correa P . The epidemiology of gastric cancer. World J Surg 1991; 15: 228–234.
Morson BC, Dawson IMP, Day DW, Jass JR, Price AB, Williams GT . Morson & Dawson's gastrointestinal pathology. 3rd ed. Oxford, England: Blackwell; 1990.p. 159.
Griffiths AP, Rice A, Dixon MF . Anaplastic gastric adenocarcinoma with extensive neutrophil infiltration. Histopathology 1998; 33: 392–393.
Rice AJ, Griffiths AP, Martin IG, Dixon MF . Gastric carcinoma with prominent neutrophil infiltration. Histopathology 2000; 37: 289–290.
Caruso RA, Speciale G, Inferrera C . Neutrophil interaction with tumor cells in small early gastric cancer: ultrastructural observations. Histol Histopathol 1994; 9: 295–303.
Caruso RA, Fedele F, Rigoli L, Inferrera C . Mast cell interaction with tumor cells in small early gastric cancer: ultrastructural observations. Ultrastruct Pathol 1997; 21: 173–181.
Caruso RA, Vitullo P, Modesti A, Inferrera C . Small early gastric cancer with special reference to macrophage infiltration. Mod Pathol 1999; 12: 386–390.
Ishigami S, Natsugoe S, Tokuda K, Nakajo A, Che X, Iwashige H, et al. Prognostic value of intratumoral natural killer cells in gastric carcinoma. Cancer 2000; 88: 577–583.
Iwasaki K, Torisu M, Fujimara T . Malignant tumor and eosinophils. I. Prognostic significance in gastric cancer. Cancer 1986; 58: 1321–1327.
Aeed PA, Nakajima M, Welch DR . The role of polymorphonuclear leukocytes (PMN) on the growth and metastatic potential of 13762NF mammary adenocarcinoma cells. Int J Cancer 1988; 42: 748–759.
Di Carlo E, Forni G, Lollini P, Colombo MP, Modesti A, Musiani P . The intriguing role of polymorphonuclear neutrophils in antitumor reactions. Blood 2001; 97: 339–345.
Welch DR, Schissel DJ, Howrey RP, Aeed PA . Tumor-elicited polymorphonuclear cells, in contrast to “normal” circulating polymorphonuclear cells, stimulate invasive and metastatic potentials of rat mammary adenocarcinoma cells. Proc Natl Acad Sci U S A 1989; 86: 5859–5863.
Decarli A, La Vecchia C, Cislaghi C, Mezzanotte G, Marubini E . Descriptive epidemiology of gastric cancer in Italy. Cancer 1986; 58: 2560–2569.
Simon R, Altman DG . Statistical aspects of prognostic factor studies in oncology. Br J Cancer 1994; 69: 979–985.
Sobin LH, Wittekind C, editors. Digestive system tumours: stomach.In: TNM classification of malignant tumours. 5th ed. New York: Wiley-Liss; 1997.p. 59–62.
Laurèn P . The two histological main types of intestinal metaplasia in the gastric mucosa: diffuse and so-called intestinal type carcinoma. An attempt at a histo-clinical classification. Acta Pathol Microbiol Scand 1965; 64: 31–49.
Altman DG, Lansen B, Sawerbrei W, Schumacher M . Dangers of using ‘optimal’ cutpoints in the evaluation of prognostic factors. J Natl Cancer Inst 1994; 86: 829–835.
Kaplan EL, Meier P . Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958; 53: 457–481.
Cox DR . Regression models and life tables (with discussion). J R Stat Soc 1972(B); 34: 187–202.
Therneau TM, Grambsch PM, Fleming TR . Martingale based residuals for survival models. Biometrika 1990; 77: 147–160.
Stata Corp. Stata statistical software. Release 7.0. College Station, TX: Stata; 2001.
Levitt SH, Aeppli DM, Potish RA, Lee CK, Nierengarten ME . Influences on inferences. Effect of errors in data on statistical evaluation. Cancer 1993; 72: 2075–2082.
Palli D, Cipriani F, Decarli A, Galli M, Saieva C, Fraumeni JF Jr, et al. Reproductive history and gastric cancer among post-menopausal women. Int J Cancer 1994; 56: 812–825.
Maguire A, Porta M, Sanz-Anquela JM, Ruano I, Malats N, Pinol JL . Sex as a prognostic factor in gastric cancer. Eur J Cancer 1996; 32: 1303–1309.
Bokey EL, Chapuis PH, Dent OF, Newland RC, Koorey SG, Zelas PJ, Stewart PJ . Factors affecting survival after excision of the rectum for cancer: a multivariate analysis. Dis Colon Rectum 1997; 40: 3–10.
Nzeako UC, Goodman ZD, Ishak KG . Comparison of tumor pathology with duration of survival of North American patients with hepatocellular carcinoma. Cancer 1995; 76: 579–588.
Ferguson MK, Wang J, Hoffman PC, Haraf DJ, Olak J, Masters GA, Vokes EE . Sex-associated differences in survival of patients undergoing resection for lung cancer. Ann Thorac Surg 2000; 69: 245–249.
Nielsen HJ, Hansen U, Christensen IJ, Reimert CM, Brunner N, Moesgaard F . Independent prognostic value of eosinophil and mast cell infiltration in colorectal cancer tissue. J Pathol 1999; 189: 487–495.
Lee T-K, Horner RD, Silverman JF, Chen Y-H, Jenny C, Scarantino CW . Morphometric and morphologic evaluations in Stage III non-small cell lung cancers. Cancer 1989; 63: 309–316.
Bellocq A, Antoine M, Flahault A, Philippe C, Crestani B, Bernaudin JF, et al. Neutrophil alveolitis in bronchioloalveolar carcinoma: induction by tumor-derived interleukin-8 and relation to clinical outcome. Am J Pathol 1998; 152: 83–92.
Spitzer JA, Zhang P . Gender differences in neutrophil function and cytokine-induced neutrophil chemoattractant generation in endotoxic rats. Inflammation 1996; 20: 485–498.
Da Silva JA . Sex hormones and glucocorticoids: interactions with the immune system. Ann N Y Acad Sci 1999; 876: 102–117.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Caruso, R., Bellocco, R., Pagano, M. et al. Prognostic Value of Intratumoral Neutrophils in Advanced Gastric Carcinoma in a High-Risk Area in Northern Italy. Mod Pathol 15, 831–837 (2002). https://doi.org/10.1097/01.MP.0000020391.98998.6B
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/01.MP.0000020391.98998.6B
Keywords
This article is cited by
-
Clinical Significance of CD66b Expression in Non-Small Cell Lung Cancer
Bulletin of Experimental Biology and Medicine (2023)
-
A critical role of STING-triggered tumor-migrating neutrophils for anti-tumor effect of intratumoral cGAMP treatment
Cancer Immunology, Immunotherapy (2021)
-
High density of CD66b in primary high-grade ovarian cancer independently predicts response to chemotherapy
Journal of Cancer Research and Clinical Oncology (2020)
-
Tumour-associated neutrophils in patients with cancer
Nature Reviews Clinical Oncology (2019)
-
Integrating histopathology, immune biomarkers, and molecular subgroups in solid cancer: the next step in precision oncology
Virchows Archiv (2019)




