Abstract
Vasoactive intestinal polypeptide (VIP) is a putative neurotransmitter of the inhibitory non-adrenergic non-cholinergic nervous system and influences many aspects of mammalian airway function. VIP binds to two G-protein-coupled VPAC receptors that are highly homologous structurally but distinguished by their different affinities for peptide analogues of VIP. As VIP binding sites in the respiratory tract have only been examined by ligand binding and cytochemical techniques, we studied the distribution of the mRNA that encodes the inducible receptor subtype VPAC2 in the human respiratory tract. Northern blots demonstrated the expression of VPAC2 mRNA in human airways and other tissues. A human-specific VPAC2 cRNA probe was used to detect VPAC2 mRNA expression in human lung by nonradioactive in situ hybridization. In larger airways, positive VPAC2 mRNA signals were localized to tracheal and bronchial ciliated epithelial cells. There was also marked staining of mucous and serous cells of submucosal glands. No signals were obtained in airway and vascular smooth muscle myocytes and endothelial cells. In peripheral lung tissues, VPAC2 mRNA expression was localized to epithelial cells of the bronchioles. Specific staining was detected in immune cells and alveolar macrophages. In summary, VPAC2 is localized in airway epithelial, glandular, and immune cells of the lung but not in airway and vascular smooth muscle. The absence of VPAC2 mRNA in vascular and airway smooth muscle myocytes may indicate that the effects of VIP on vasodilation and bronchodilation are mediated by VPAC1 or undefined receptors. However, a paracrine modulation of the two most prominent effects of VIP in the respiratory tract by VPAC2 cannot be excluded.
Similar content being viewed by others

Introduction
The 28-amino acid vasoactive intestinal polypeptide (VIP) is a putative neurotransmitter or neuromodulator of the inhibitory non-adrenergic non-cholinergic nervous system in mammalian airways (Maggi et al, 1995). VIP-immunoreactivity (VIP-IR) is present in cells of the tracheobronchial smooth muscle layer, in the walls of pulmonary and bronchial vessels, around submucosal glands, in the lamina propria, and in pulmonary ganglia (Dey et al, 1981; Lundberg et al, 1984). VIP-IR nerve fibers are found as branching networks in the respiratory tract (Ghatei et al, 1982) They decrease in frequency as the airways become smaller but extend to peripheral bronchioles (Lundberg et al, 1984). The pattern of VIPergic nerves largely follows that of cholinergic nerves (Laitinen et al, 1985). VIP-IR is also present in sensory nerves (Lundberg et al, 1984; Luts and Sundler, 1989).
Several studies using receptor binding techniques have been performed to demonstrate the presence of VIP receptors and have shown abundant binding in different parts of the lungs (Carstairs and Barnes, 1986; Robberecht et al, 1981; 1988). Two types of VIP receptors have been cloned and characterized in the past years. They were termed the VPAC1 receptor, formerly described as the VIP1 receptor (Ishihara et al, 1992; Lutz et al, 1993), the VIP/PACAP type II receptor (Ciccarelli et al, 1994) or the PVR2 (Rawlings et al, 1995), and the VPAC2 receptor, formerly called the VIP2 receptor (Lutz et al, 1993), PACAPR-3 (Inagaki et al, 1994), or PVR3 (Rawlings et al, 1995). Several cyclic peptides and other analogues of VIP that act as agonists of high potency and selectivity distinguish VPAC2 receptors from VPAC1 receptors (Gourlet et al, 1997; O'Donnell et al, 1994a, 1994b; Xia et al, 1997) that have been cloned from rat, mouse, and human tissues so far (Adamou et al, 1995; Inagaki et al, 1994; Lutz et al, 1993; Svoboda et al, 1994; Usdin et al, 1994; Wei and Mojsov, 1996). In the current International Union of Pharmacology nomenclature, the receptors are classified as VPAC1 and VPAC2 (Harmar et al, 1998).
Human VPAC2 receptor mRNA was prominent in the central nervous system (CNS) and several other peripheral tissues, including lung (Adamou et al, 1995; Svoboda et al, 1994; Wei and Mojsov, 1996). As VIP binding sites in the airways have only been characterized by autoradiographic ligand binding studies and receptor immunoreactivity studies leading to controversial results, the present study was performed to define the localization of mRNA encoding the VPAC2 receptor in the human respiratory tract.
Results
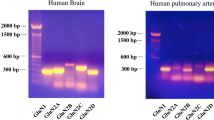
Detection of VPAC2 Receptor mRNA by Northern Blot
Northern blots were performed to demonstrate the expression of the VPAC2 receptor mRNA in human tissues. Using a radiolabeled human specific cRNA probe, VPAC2 receptor mRNA was detected at different levels in extracts of human lung and other tissues. The decreasing order of intensity of VPAC2 mRNA expression was as follows: CNS, heart, pancreas, skeletal muscle, kidney, lung, stomach, and liver (Fig. 1).
Detection of VPAC2 receptor mRNA in human lung by Northern Blot. Two micrograms of poly (A+) RNA prepared from human lung and other tissues was hybridized with a [32P]-labeled human-specific VPAC2 receptor probe. VPAC2 receptor mRNA levels are detected with decreasing intensity in central nervous system, heart, pancreas, skeletal muscle, kidney, lung, stomach, and liver.
Distribution of VPAC2 Receptor mRNA in Human Respiratory Tract
The expression of VPAC2 mRNA was detected by nonradioactive in situ hybridization and high-resolution interference contrast microscopy. Abundant staining of different cell types was present in all areas of larger airways and peripheral lung. Positive staining was reproducibly detected after hybridization with antisense probe. Control hybridizations on alternate sections with equivalent amounts of sense-probe using the same hybridization and washing stringency were unstained and demonstrated the specificity of antisense hybridization signals. Omission of labeled cRNA probes from the hybridization mixture also resulted in unstained sections being identical to results obtained when RNA was digested before hybridization.
In sections of trachea and extrapulmonary and intrapulmonary bronchi, positive VPAC2 mRNA signals were localized to the cytoplasm of basal and ciliated cells (Fig. 2A). Goblet cells did not show VPAC2 mRNA expression (Fig. 2A). There were also no hybridization signals present in airway and vascular smooth muscle myocytes (Fig. 3), connective and cartilaginous tissue, and endothelial cells (Fig. 2A). Control slides that were treated with the sense probe did not show specific staining (Fig. 2B).
Localization of VPAC2 receptor mRNA in larger airways by in situ hybridization. Eight-microgram cryostat sections of human main bronchus were subjected to nonradioactive in situ hybridization for VPAC2 mRNA. VPAC2 mRNA hybridization signals are localized to basal and ciliated cells of bronchial epithelium (ep, arrows in A). No signals are present in goblet cells and airway smooth muscle (asm) or connective and cartilaginous (ct) tissue. Control slides that were treated with the sense probe did not show specific staining (B). Bar = 40 μm.
Localization of VPAC2 receptor mRNA in airways by in situ hybridization. Positive VPAC2 mRNA signals are localized to epithelial cells of subsegmentary bronchi (arrows). No hybridization signals in endothelial cells (arrowheads), vascular smooth muscle cells (asterisks), and airway smooth muscle cells (asm). alu = airway lumen, vlu = vessel lumen. Bar = 20 μm.
VPAC2 mRNA signals were also present in submucosal gland cells that surrounded trachea and bronchi (Fig. 4A). In these submucosal glands, both serous and mucous cells were stained for VPAC2 mRNA (Fig. 4, A and C). Sense probes did not stain these cells (Fig. 4B).
Localization of VPAC2 receptor mRNA in bronchial glands by in situ hybridization. VPAC2 mRNA signals are present in acinar and ductal submucosal gland cells (gl) (A, C) of 8 μm human trachea crystate sections. Also, there is abundant staining of epithelial cells (ep) but not goblet cells (A). Negative airway smooth muscle (asm). Sense probes did show specific signals. Bar = 40 μm (A, B); Bar = 16 μm (C).
Differences in the distributional pattern of VPAC2 mRNA between trachea and extrapulmonary and intrapulmonary bronchi were not evident. In peripheral lung, the epithelium of small bronchioles displayed positive hybridization signals (Fig. 5A). In alveolar space, signals were found in cells that were identified as alveolar macrophages by their characteristic morphology in the alveolar lumen (Fig. 5c).
Localization of VPAC2 receptor mRNA in peripheral lung by in situ hybridization. Positive staining for VPAC2 mRNA in epithelial cells of small bronchioli and alveolar macrophages (arrows in A and C). Marked staining of clusters of immune cells (D). No specific staining in control sense probes (B, E). Bar = 40 μm (A, B, D, E); Bar = 25 μm (C). alu = airway lumen, vlu = vessel lumen.
Also, positive VPAC2 mRNA hybridization signals were localized to peribronchiolar and peribronchial clusters of immune cells (Fig. 5D). Controls using the sense-probe were unstained (Fig. 5, B and E).
Discussion
The present study was performed to localize the mRNA of the VIP receptor VPAC2 in human lung tissues. Although there is a large body of evidence on the functional role of the neuropeptide VIP in normal and pathological airway tissues, a detailed analysis of the expression of distinct VIP receptors does not exist so far.
VIP binding sites have been shown in airway tissues of several species by autoradiographic ligand binding studies using (125I)-VIP (Carstairs and Barnes, 1986; Robberecht et al, 1981; 1988) and by an immunocytochemical reporter for increases in intracellular cyclic AMP (Lazarus et al, 1986) that is formed when VIP stimulates adenylyl cyclase (Frandsen et al, 1978). Ligand binding sites were initially reported in airway smooth muscle of large but not small airways and in pulmonary vascular smooth muscle. Binding sites were also found in submucosal glands and in the alveolar wall (Carstairs and Barnes, 1986). Immunohistochemical studies using an antibody against cyclic AMP after stimulation by VIP confirmed the autoradiographic findings in different species (Lazarus et al, 1986).
Autoradiography with high-affinity radioligands allows a characterization of binding sites but is limited by a poor morphological resolution. Therefore, it does not reveal the exact cellular sites of the ligand binding. As two distinct receptors for VIP were identified and cloned (Adamou et al, 1995; Ciccarelli et al, 1994; Inagaki et al, 1994; Ishihara et al, 1992; Lutz et al, 1993; Rawlings et al, 1995; Svoboda et al, 1994; Wei and Mojsov, 1996), a localization of a specific receptor mRNA could distinguish the cellular distribution and molecular basis of VIP binding sites.
High resolution interference contrast microscopy revealed positive VPAC2 mRNA signals in tracheal and bronchial epithelial cells and glandular cells that corresponded to earlier binding studies for VIP (Carstairs and Barnes, 1986). These results demonstrate that the reported ligand binding of VIP in these cells is at least partly represented by the VPAC2 receptor.
In peripheral lung, there was staining for VPAC2 mRNA of clusters of immune cells and alveolar macrophages. Thus, some of the VIP binding sites reported for the alveolar wall (Carstairs and Barnes, 1986) may consist of VPAC2 receptor expression in macrophages and of expression of the more widespread VPAC1 as reported previously (Kaltreider et al, 1997).
VPAC1 expression has been previously detected in the lung by RT-PCR, Northern blotting, in situ hybridization (Usdin et al, 1994), and immunohistochemistry (Busto et al, 2000; Ichikawa et al, 1995). Localization studies lead to controversial results. Autoradiographic in situ hybridization revealed staining of the epithelium in large and moderate size bronchi as well as vascular endothelium (Usdin et al, 1994). One study in rat airways using immunohistochemistry for VPAC1 led to staining of macrophages and airway epithelium from trachea to terminal bronchioles, but not of bronchial smooth muscle or vascular smooth muscle other than infrequent staining of some intermediate-sized pulmonary veins (Ichikawa et al, 1995). A second study reported VPAC1-like immunoreactivity in leukocytes and vascular smooth muscle myocytes of some vessels but not in epithelial cells (Busto et al, 2000).
VIP potently relaxes the vessels that supply the upper airways (Lundberg et al, 1981; Lung and Widdicombe, 1987; Malm et al, 1980), trachea, bronchi (Laitinen et al, 1987), and pulmonary vessels (Hamasaki et al, 1983a, 1983b; Nandiwada et al, 1985; Obara et al, 1989), and VIP-induced vasodilation is more potent in tracheal circulation than in bronchial circulation (Matran et al, 1989a; 1989b). The vasodilation is reported to be independent of endothelial cells (Barnes et al, 1986; Greenberg et al, 1987). By demonstrating the absence of VPAC2 receptor mRNA in the vascular smooth muscle layer, our findings indicate that VIP-induced vasodilation has to be mediated by a different VIP receptor or by a paracrine VPAC2-dependent pathway.
A recent study reported the presence of VPAC2-like immunoreactivity in myocytes of peripheral arteries but not airway smooth muscle cells. However, these signals were extremely weak and restricted to a minority of smooth muscle cells. The specificity of the reaction was not confirmed by preabsorption techniques and, therefore, not proven as specific for the VPAC2 protein (Busto et al, 2000).
A dense network of VIP-IR nerve fibers (Lundberg et al, 1984; Luts and Sundler, 1989), VIP binding sites (Carstairs and Barnes, 1986; Elgavish et al, 1989), and VIP-receptor immunoreactivity (Fischer et al, 1992) has been reported around and in submucosal glands, and a complex action of VIP on mucus secretion has been suggested (Maggi et al, 1995). Our findings support these suggestions by directly localizing VPAC2 mRNA to serous and mucous cells of submucosal glands.
It has been shown that VIP relaxes airways size-dependently and dilates only bronchi but not smaller bronchioles (Altiere and Diamond, 1984). There was no expression of VPAC2 receptor mRNA in airway smooth muscle myocytes. Therefore, the bronchodilation may be mediated by a paracrine transcellular VPAC2 signal pathway or a different receptor.
The absence of VPAC2 mRNA in vascular and airway smooth muscle cells may imply that this receptor subtype does not directly mediate vasodilatory and bronchodilatory effects in the respiratory tract. However, a paracrine modulation of the two most prominent effects of VIP in the respiratory tract by VPAC2 cannot be excluded.
The demonstration of VPAC2 mRNA in airway immune cells is a finding that affects the significance of VIP in immunomodulation. So far, various functional studies have reported the ability of VIP to influence complex cellular and subcellular immunologic events such as migration, antigen-induced proliferation, and cytokine production (Bellinger et al, 1996). Together with the recent demonstration of VPAC2-like immunoreactivity in macrophages and leukocytes (Kaltreider et al, 1997), our finding provides evidence for the participation of VIP in immunomodulation via the VPAC2 receptor subtype.
We have demonstrated that VPAC2 receptor mRNA is widely distributed in the human respiratory tract and have identified the cellular sites of expression. The VPAC2 receptor mRNA distribution does not correspond with all cellular sites reported by previous ligand binding studies. The failure to detect VPAC2 transcripts in both airway and vascular smooth muscle myocytes is a novel aspect of VIP signaling in the lung, indicating that the previously reported functional VIP binding sites are represented by different receptor types.
Our findings are the first report on the distribution of VPAC2 receptor mRNA in the human respiratory tract, and they support the view that VIP is an important neuromodulator that acts by molecular distinct receptor pathways.
Materials and Methods
Tissues and Materials
Surgically resected human lung tissues (n = 6) from patients with central carcinoma were provided by the Departments of Surgery and Pathology, University of Giessen. The tissues were examined for malignant cells, and only areas with normal histology and cytology were subjected to the study protocol. If not stated otherwise, all solutions were supplied by Sigma, Deisenhofen, Germany.
Northern Blot
Two micrograms of poly (A+) RNA from human CNS, lung, heart, kidney, stomach, pancreas, skeletal muscle, and liver were electrophoresed and blotted onto a nylon membrane. VPAC2 receptor mRNA was identified by overnight hybridization at 42° C with a [32P]-labeled PCR-derived 0.6-kbp probe representing the transmembrane domains 3 to 6 of VPAC2. After hybridization, membranes were washed twice for 15 minutes at 65° C in 2 × SSC containing 0.1% SDS and twice for 15 minutes at 65° C in 0.5 × SSC containing 0.1% SDS and examined after development.
VPAC2 receptor cRNA Probes
Digoxigenin-labeled VPAC2 receptor-specific cRNA probes were produced with restriction and in vitro transcription kits (Boehringer Mannheim, Mannheim, Germany) as follows: a human-specific VPAC2 receptor PCR fragment (sequence of the region spanning from TM 3 to 7 of the VPAC2 receptor from TSUP1 human T lymphoblast cDNA) was subcloned into the pGEM-T vector (Promega, Mannheim, Germany). The plasmid was transfected into Escherichia coli and amplified. After linearization of the plasmid with NcoI (for sense probe) or SpeI (for anti-sense probe) the nonradioactive cRNA probes were synthesized and labeled by in vitro transcription using digoxigenin-11-UTP. For generation of anti-sense probes, the SpeI-linearized plasmid was transcribed with T7 polymerase. For the sense probe, the NcoI-linearized plasmid was transcribed with SP6 polymerase. For transcription, 1 μg of linearized plasmid was incubated in transcription buffer with 150 μmole of UTP, 600 μmole of digoxigenin-labeled UTP, 750 μmole of ATP, CTP, and GTP, 1 U/μl RNase inhibitor, and 2 U/μl polymerase for 2 hours at 37° C. A DNase I step at 37° C for 15 minutes was followed by the addition of 0.2 m EDTA (pH 8). The transcripts were isolated by LiCl and ethanol precipitation and checked for probe length by TAE-agarose gel electrophoresis (Seakem-ME Agarose, Biozym, Oldendorf, Germany) and ethidium bromide staining.
Nonradioactive mRNA In Situ Hybridization
Localization of VPAC2 receptor mRNA was performed by nonradioactive in situ hybridization. Cryostat (Jung Frigocut 2800E, Leica, Bensheim, Germany) sections of human lung between 8 μm and 12 μm were thawed onto precoated glass slides (Hybri Slips, Sigma, Deisenhofen, Germany) and air-dried for 15 minutes. The sections were then fixed by immersion for 30 minutes in 4% paraformaldehyde containing PBS (pH 7.4). After rinsing in PBS 3 × 10 minutes and in distilled water for 1 minute the slides were permeablized with 0.1 m HCl for 10 minutes and acetylated with 0.1 m triethanolamine (pH 8.0) containing 0.25% acetic anhydride for 10 minutes. After washes in PBS (10 minutes) and distilled water (1 minute), the slides were dehydrated in 70%, 80%, and 96% ethanol. Each section was air-dried for 15 minutes and covered with 100 μl of prehybridization buffer [50% formamide, 1 × Denhardt's, 10 mm triethanolamine, 5 mm EDTA, 6.25% dextransulfate, 0.3 m NaCl, 1 mg/ml tRNA (Roche, Mannheim, Germany)] for 1 to 2 hours at 40° C in a moist chamber. After removal of the prehybridization buffer, the slides were covered with 50 μl of hybridization buffer (containing 10 ng/μl VPAC2-specific digoxigenin-labeled sense or antisense probe in 50% formamide, 1 × Denhardt's, 10 mm triethanolamine, 5 mm EDTA, 6.25% dextransulfate, 0.3 m NaCl, 1 mg/ml tRNA) and protected with coverslips (Hybrislips, Sigma). Hybridization was performed at 40° C for 14 to 16 hours in a moist chamber.
After hybridization, several washing steps were performed, including the following: 20 minutes in 2 × SSC and 20 minutes in 1 × SSC at room temperature (rt); RNase treatment for 30 minutes at 37° C; 1 × SSC for 20 minutes, 0.5 × SSC for 20 minutes, and 0.2 × SSC for 20 minutes at rt; 0.2 × SSC at 50° C for 1 hour; and 0.2 × SSC for 15 minutes and distilled water for 15 minutes at rt.
To detect hybridization signals with the digoxigenin detection kit (Boehringer), sections were rinsed in buffer I (100 mm Tris-HCl; 150 mm NaCl; pH 7, 5) for 10 minutes at rt, and unspecific binding sites were blocked with 1% bovine serum albumin and 10% normal swine serum in 1 × PBS in buffer I for 30 minutes at rt. After removal of the blocking medium, the sections were incubated with 40 μl of sheep-anti-digoxigenin-alkaline-phosphatase conjugate (1:500) diluted in blocking medium for 12 hours at 4° C in a moist chamber. Sections were then rinsed twice in Buffer I for 15 minutes and equilibrated in Buffer III (100 mm Tris-HCl; 100 mm NaCl; 50 mm MgCl2; pH 9, 5) for 2 minutes at rt. Detection of the signal was performed by incubation with 150 μl of chromogen solution per slide [45 μl of nitroblue tetrazolium (75 mg/ml) in 70% dimethylformamide], 35 μl of 5-bromo-4-chloro-3-indolyl-phosphate (50 μg/ml in 100% dimethylformamide), and levamisole in 10 ml of Buffer II in a moist chamber at 4° C. Slides were checked for color development after 1 to 15 hours. The reaction was stopped by rinsing the slides in 10 mm Tris HCl with 1 mm EDTA (pH 8.0) for 15 minutes. After washing in PBS twice for 15 minutes the slides were coverslipped with Kaisers glycerine gelatin (Merck, Darmstadt, Germany) and examined with an Olympus BX 60 microscope (Olympus, Hamburg, Germany).
References
Adamou JE, Aiyar N, Van Horn S, and Elshourbagy NA (1995). Cloning and functional characterization of the human vasoactive intestinal peptide (VIP)-2 receptor. Biochem Biophys Res Commun 209: 385–392.
Altiere RJ and Diamond L (1984). Comparison of vasoactive intestinal peptide and isoproterenol relaxant effects in isolated cat airways. J Appl Physiol 56: 986–992.
Barnes PJ, Cadieux A, Carstairs JR, Greenberg B, Polak JM, and Rhoden K (1986). Vasoactive intestinal peptide in bovine pulmonary artery: Localisation, function and receptor autoradiography. Br J Pharmacol 89: 157–162.
Bellinger DL, Lorton D, Brouxhon S, Felten S, and Felten DL (1996). The significance of vasoactive intestinal polypeptide (VIP) in immunomodulation. Adv Neuroimmunol 6: 5–27.
Busto R, Prieto JC, Bodega G, Zapatero J, and Carrero I (2000). Immunohistochemical localization and distribution of VIP/PACAP receptors in human lung. Peptides 21: 265–269.
Carstairs JR and Barnes PJ (1986). Visualization of vasoactive intestinal peptide receptors in human and guinea pig lung. J Pharmacol Exp Ther 239: 249–255.
Ciccarelli E, Vilardaga JP, De Neef P, Di Paolo E, Waelbroeck M, Bollen A, and Robberecht P (1994). Properties of the VIP-PACAP type II receptor stably expressed in CHO cells. Regul Pept 54: 397–407.
Dey RD, Shannon WA Jr, and Said SI (1981). Localization of VIP-immunoreactive nerves in airways and pulmonary vessels of dogs, cat, and human subjects. Cell Tissue Res 220: 231–238.
Elgavish A, Pillion DJ, and Meezan E (1989). Evidence for vasoactive intestinal peptide receptors in apical membranes from tracheal epithelium. Life Sci 44: 1037–1042.
Fischer A, Kummer W, Couraud JY, Adler D, Branscheid D, and Heym C (1992). Immunohistochemical localization of receptors for vasoactive intestinal peptide and substance P in human trachea. Lab Invest 67: 387–393.
Frandsen EK, Krishna GA, and Said SI (1978). Vasoactive intestinal polypeptide promotes cyclic adenosine 3′,5′-monophosphate accumulation in guinea-pig trachea. Br J Pharmacol 62: 367–369.
Ghatei MA, Sheppard MN, O'Shaughnessy DJ, Adrian TE, McGregor GP, Polak JM, and Bloom SR (1982). Regulatory peptides in the mammalian respiratory tract. Endocrinology 111: 1248–1254.
Gourlet P, Vertongen P, Vandermeers A, Vandermeers-Piret MC, Rathe J, De Neef P, Waelbroeck M, and Robberecht P (1997). The long-acting vasoactive intestinal polypeptide agonist RO 25–1553 is highly selective of the VIP2 receptor subclass. Peptides 18: 403–408.
Greenberg B, Rhoden K, and Barnes PJ (1987). Relaxant effects of vasoactive intestinal peptide and peptide histidine isoleucine in human and bovine pulmonary arteries. Blood Vessels 24: 45–50.
Hamasaki Y, Mojarad M, and Said SI (1983a). Relaxant action of VIP on cat pulmonary artery: Comparison with acetylcholine, isoproterenol, and PGE1. J Appl Physiol 54: 1607–1611.
Hamasaki Y, Saga T, Mojarad M, and Said SI (1983b). Vasoactive intestinal peptide counteracts leukotriene D4-induced contractions of guinea pig trachea, lung, and pulmonary artery. Trans Assoc Am Physicians 96: 406–411.
Harmar AJ, Arimura A, Gozes I, Journot L, Laburthe M, Pisegna JR, Rawlings SR, Robberecht P, Said SI, Sreedharan SP, Wank SA, and Waschek JA (1998). International Union of Pharmacology. XVIII. Nomenclature of receptors for vasoactive intestinal peptide and pituitary adenylate cyclase-activating polypeptide. Pharmacol Rev 50: 265–270.
Ichikawa S, Sreedharan SP, Owen RL, and Goetzl EJ (1995). Immunochemical localization of type I VIP receptor and NK-1-type substance P receptor in rat lung. Am J Physiol 268: L584–588.
Inagaki N, Yoshida H, Mizuta M, Mizuno N, Fujii Y, Gonoi T, Miyazaki J, and Seino S (1994). Cloning and functional characterization of a third pituitary adenylate cyclase-activating polypeptide receptor subtype expressed in insulin-secreting cells. Proc Natl Acad Sci USA 91: 2679–2683.
Ishihara T, Shigemoto R, Mori K, Takahashi K, and Nagata S (1992). Functional expression and tissue distribution of a novel receptor for vasoactive intestinal polypeptide. Neuron 8: 811–819.
Kaltreider HB, Ichikawa S, Byrd PK, Ingram DA, Kishiyama JL, Sreedharan SP, Warnock ML, Beck JM, and Goetzl EJ (1997). Upregulation of neuropeptides and neuropeptide receptors in a murine model of immune inflammation in lung parenchyma. Am J Respir Cell Mol Biol 16: 133–144.
Laitinen A, Partanen M, Hervonen A, Pelto-Huikko M, and Laitinen LA (1985). VIP like immunoreactive nerves in human respiratory tract. Light and electron microscopic study. Histochemistry 82: 313–319.
Laitinen LA, Laitinen A, Salonen RO, and Widdicombe JG (1987). Vascular actions of airway neuropeptides. Am Rev Respir Dis 136: S59–64.
Lazarus SC, Basbaum CB, Barnes PJ, and Gold WM (1986). cAMP immunocytochemistry provides evidence for functional VIP receptors in trachea. Am J Physiol 251: C115–119.
Lundberg JM, Anggard A, Emson P, Fahrenkrug J, and Hokfelt T (1981). Vasoactive intestinal polypeptide and cholinergic mechanisms in cat nasal mucosa: Studies on choline acetyltransferase and release of vasoactive intestinal polypeptide. Proc Natl Acad Sci USA 78: 5255–5259.
Lundberg JM, Fahrenkrug J, Hokfelt T, Martling CR, Larsson O, Tatemoto K, and Anggard A (1984). Co-existence of peptide HI (PHI) and VIP in nerves regulating blood flow and bronchial smooth muscle tone in various mammals including man. Peptides 5: 593–606.
Lung MA and Widdicombe JG (1987). Lung reflexes and nasal vascular resistance in the anaesthetized dog. J Physiol 386: 465–474.
Luts A and Sundler F (1989). Peptide-containing nerve fibers in the respiratory tract of the ferret. Cell Tissue Res 258: 259–267.
Lutz EM, Sheward WJ, West KM, Morrow JA, Fink G, and Harmar AJ (1993). The VIP2 receptor: Molecular characterisation of a cDNA encoding a novel receptor for vasoactive intestinal peptide. FEBS Lett 334: 3–8.
Maggi CA, Giachetti A, Dey RD, and Said SI (1995). Neuropeptides as regulators of airway function: Vasoactive intestinal peptide and the tachykinins. Physiol Rev 75: 277–322.
Malm L, Sundler F, and Uddman R (1980). Effects of vasoactive intestinal polypeptide on resistance and capacitance vessels in the nasal mucosa. Acta Otolaryngol 90: 304–308.
Matran R, Alving K, Martling CR, Lacroix JS, and Lundberg JM (1989a). Effects of neuropeptides and capsaicin on tracheobronchial blood flow of the pig. Acta Physiol Scand 135: 335–342.
Matran R, Alving K, Martling CR, Lacroix JS, and Lundberg JM (1989b). Vagally mediated vasodilation by motor and sensory nerves in the tracheal and bronchial circulation of the pig. Acta Physiol Scand 135: 29–37.
Nandiwada PA, Kadowitz PJ, Said SI, Mojarad M, and Hyman AL (1985). Pulmonary vasodilator responses to vasoactive intestinal peptide in the cat. J Appl Physiol 58: 1723–1728.
Obara H, Kusunoki M, Mori M, Mikawa K, and Iwai S (1989). The effects of various peptides on the isolated pulmonary artery. Peptides 10: 241–243.
O'Donnell M, Garippa RJ, Rinaldi N, Selig WM, Simko B, Renzetti L, Tannu SA, Wasserman MA, Welton A, and Bolin DR (1994a). Ro 25-1553: A novel, long-acting vasoactive intestinal peptide agonist. Part I: In vitro and in vivo bronchodilator studies. J Pharmacol Exp Ther 270: 1282–1288.
O'Donnell M, Garippa RJ, Rinaldi N, Selig WM, Tocker JE, Tannu SA, Wasserman MA, Welton A, and Bolin DR (1994b). Ro 25-1553: A novel, long-acting vasoactive intestinal peptide agonist. Part II: Effect on in vitro and in vivo models of pulmonary anaphylaxis. J Pharmacol Exp Ther 270: 1289–1294.
Rawlings SR, Piuz I, Schlegel W, Bockaert J, and Journot L (1995). Differential expression of pituitary adenylate cyclase-activating polypeptide/vasoactive intestinal polypeptide receptor subtypes in clonal pituitary somatotrophs and gonadotrophs. Endocrinology 136: 2088–2098.
Robberecht P, Chatelain P, de Neef P, Camus JC, Waelbroeck M, and Christophe J (1981). Presence of vasoactive intestinal peptide receptors coupled to adenylate cyclase in rat lung membranes. Biochim Biophys Acta 678: 76–82.
Robberecht P, Waelbroeck M, de Neef P, Camus JC, Coy DH, and Christophe J (1988). Pharmacological characterization of VIP receptors in human lung membranes. Peptides 9: 339–345.
Svoboda M, Tastenoy M, Van Rampelbergh J, Goossens JF, de Neef P, Waelbroeck M, and Robberecht P (1994). Molecular cloning and functional characterization of a human VIP receptor from SUP-T1 lymphoblasts. Biochem Biophys Res Commun 205: 1617–1624.
Usdin TB, Bonner TI, and Mezey E (1994). Two receptors for vasoactive intestinal polypeptide with similar specificity and complementary distributions. Endocrinology 135: 2662–2680.
Wei Y and Mojsov S (1996). Tissue specific expression of different human receptor types for pituitary adenylate cyclase activating polypeptide and vasoactive intestinal polypeptide: Implications for their role in human physiology. J Neuroendocrinol 8: 811–817.
Xia M, Sreedharan SP, Bolin DR, Gaufo GO, and Goetzl EJ (1997). Novel cyclic peptide agonist of high potency and selectivity for the type II vasoactive intestinal peptide receptor. J Pharmacol Exp Ther 281: 629–633.
Acknowledgements
We thank E. J. Goetzl and S. P. Sreedharan for the generation of VPAC2 probes and northern blots, C. Peiser and J. Springer for critical comments, and S. Wiegand and M. Scheibner for their expert assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Groneberg, D., Hartmann, P., Dinh, Q. et al. Expression and Distribution of Vasoactive Intestinal Polypeptide Receptor VPAC2 mRNA in Human Airways. Lab Invest 81, 749–755 (2001). https://doi.org/10.1038/labinvest.3780283
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.3780283
This article is cited by
-
Die humane Ehrlichiose und Anaplasmose
Zentralblatt für Arbeitsmedizin, Arbeitsschutz und Ergonomie (2019)
-
Neuropeptides in asthma, chronic obstructive pulmonary disease and cystic fibrosis
Respiratory Research (2018)
-
Prospect of vasoactive intestinal peptide therapy for COPD/PAH and asthma: a review
Respiratory Research (2011)
-
Neuromediatoren, Mastzellen und Umweltinteraktionen (NeuroMastER): Expression von VPAC2-mRNA durch In-situ-Hybridisierung bei Bullösem Pemphigoid
Zentralblatt für Arbeitsmedizin, Arbeitsschutz und Ergonomie (2011)
-
Lebertoxizität — molekulare Analyse von Leberfunktionsstörungen in der Arbeitsmedizin und Umweltmedizin
Zentralblatt für Arbeitsmedizin, Arbeitsschutz und Ergonomie (2007)