Abstract
Dysfunction of the host immune system in cancer patients can be due to a number of factors, including suppression of tumor-associated antigen reactive lymphocytes by CD4+CD25+ regulatory T (Treg) cells. Several studies suggest that Tregs are elevated in cancer patients and that depletion of Tregs may enhance the antitumor immunity of host, but the pathogenic and mechanistic relationship between cancer and Tregs is still unclear. In this report, we show that Tregs are increased in peripheral blood mononuclear cells (PBMCs) from hepatocellular carcinoma (HCC) patients and positively correlate with tumor burden. When PBMCs are co-cultured with human hepatoma cell lines Huh7, HepG2, and Hclone5, CD4+CD25+-T cell populations increase in frequency and undergo phenotypic and functional changes. CD45RA, CD45RO, CD69, CD62L, GITR, CTLA-4, Ki67, granzyme A, granzyme B, and FOXP3 expression were upregulated in CD4+CD25+ cells after in vitro exposure to HCC cell lines. CD4+CD25+ T cells from PBMCs that were co-cultured with Huh7 cells also have higher suppressor ability compared to that of the CD4+CD25+ T cells from control PBMC. Huh7 culture supernatants appear to promote CD4+CD25+ T-cell proliferation and inhibit CD4+CD25− T-cell proliferation. In conclusion, these results strongly suggest that tumor-related factors not only induce and expand CD4+CD25+ cells, but also enhance their suppressor ability.
Similar content being viewed by others
Main
Naturally occurring CD4+CD25+ regulatory T cells (Tregs) play a critical role in modulating immune responses by suppressing CD4+CD25− and CD8+ effector T-cell function.1 Their depletion leads to more effective immune responses to tumors and infections.2, 3, 4 In viral hepatitis, recent studies have shown that Tregs are elevated in chronic infection and contribute to viral persistence by suppressing viral-specific T-cell responses.5, 6, 7 Tregs have also been suggested to impede immune surveillance against cancer.8, 9, 10, 11, 12 Their inactivation improves tumor-specific immunity and leads to more efficient tumor rejection.13, 14, 15 Thus, manipulation of Tregs may represent a feasible immunotherapy strategy for cancer.
Hepatocellular carcinoma (HCC) is the fifth most common cancer worldwide and its incidence is increasing owing to the rising prevalence of advanced hepatitis C (HCV) disease.16 Surgical resection and liver transplantation can be curative when detected early. Unfortunately, the majority of patients are not candidates for these treatments and they have limited options, stressing the importance of a better understanding of HCC pathogenesis. Effector T lymphocytes are important in the control of tumor progression.17 Lymphocytes that infiltrate tumor have been described in HCC, and their presence after resection indicate a better survival.18, 19 However, the progression of tumors despite the presence of infiltrating lymphocytes suggests immunologic tolerance generated by tumors. An increase in the Treg population has been observed in both the periphery and tumor microenvironment in patients with cancer.20, 21, 22, 23, 24, 25, 26 Tumor-infiltrating lymphocytes in HCC appear to contain suppressive Tregs cells that accumulate locally and inhibit tumor-specific immune responses.27 The recent finding that the telomere length of Tregs is preserved, despite their loss of T-cell receptor circles, provides the first evidence that the increase of Tregs in cancer patients is due to active proliferation rather than redistribution.28 Nevertheless, the mechanisms involved in the observed expansion of Tregs from tumors remains poorly characterized.
In this study, a higher level of Tregs was found in the periphery of HCC patients, which correlated with the extent of tumor burden. We thus hypothesized that the HCC microenvironment must support Treg expansion and/or deplete CD4+CD25− effector cells to promote immune tolerance. To evaluate this hypothesis, a series of in vitro cultures using supernatants from human HCC cell lines and normal human hepatocytes were performed with peripheral mononuclear, CD4+CD25+, or CD4+CD25− cells. Our results indicate that HCC culture supernatants promoted expansion of Tregs and enhanced their suppressive function. This supports the hypothesis that the proliferation of Tregs is tumor driven via secretion of soluble factors.
Materials and methods
Study Population
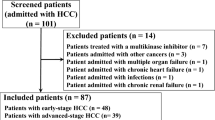
One hundred and eight individuals were recruited using a protocol approved by the University of Florida IRB. The study subjects included patients with chronic hepatitis C (CHC) (n=40), HCV with cirrhosis (n=15), viral-related HCC (n=33; 26 with HCV and seven with HBV), non-viral-related HCC (n=7), non-HCC liver lesions (hemangiomas, cysts, focal nodular hyperplasia; n=10) and healthy controls (n=20). HCC was diagnosed according to the diagnostic guidelines of the AASLD.29 Clinical data were collected to determine the tumor burden defined as: (1) single lesion <5 cm; (2) two to three lesions <3 cm; (3) multiple lesions not meeting number 2 criteria; (4) vessel involvement; and (5) metastatic disease.
Cell Preparation
Peripheral blood mononuclear cells (PBMCs) were isolated as described previously.30 CD4+ T cells were purified from PBMC using the human EasySep™ CD4+ Enrichment Cocktail (Stemcell Technologies, Canada). Negatively selected CD4+ cells were incubated with anti-CD25 microbeads (50 μg/108 cells) and selected with the MS column (Miltenyi Biotech, CA, USA) to obtain the CD4+CD25+ and the CD4+CD25− fractions as described previously.5 The CD4+CD25+ and CD4+CD25− purity was more than 95 and 99%, respectively.
Antibodies
The following monoclonal antibodies were used: CD3-CyC, CD4-APC, CD4-FITC, CD25-PE, CD25-CyC, CD45RA-FITC, CD45RO-FITC, CD69-FITC, CD62L-FITC, CD152-APC, Granzyme A-FITC, Granzyme B-FITC, perforin-FITC, mouse anti-human CD28, mouse anti-human CD3 (BD PharMingen), CD127-PE, Glucocorticoid-induced TNF receptor (GITR)-FITC (R&D System), FOXP3-PE (eBioscience), and Ki67-FITC (Fitzgerald, Flanders, NJ, USA). Isotype-matched antibodies were used.
Cell Culture and Supernatants
The human hepatoma lines, Huh7, HepG2, Hep3B, Hclone5, and normal human hepatocytes (Cellzdirect) were cultured in DEME medium with 20% FBS, 2 mM HEPES, 2 mM L-glutamine, 100 U/ml penicillin, and 100 μg/ml streptomycin in 5% CO2 at 37°C. The supernatants were collected at 60–80% confluence, after centrifugation at 1200 r.p.m. for 10 min, and then passed through a 0.45 μm filter. Supernatants were stored at −20°C.
Transwell Experiments
Six-well transwell chambers with a 0.4 μm porous membrane (Corning-Costar) were used. Briefly, Huh7, HepG2, Hclone5, and normal hepatocytes (5 × 105/well) were plated underneath the transwell chamber for 4 h, and then 1 ml of PBMC (2.5 × 107/ml) was added to the inner chamber. After 48 h, PBMCs were harvested and stained for flow cytometry or used to obtain CD4+CD25+ and CD4+CD25− cells.
Flow Cytometry and Labeling
PBMCs were stained with various monoclonal antibodies to determine the frequency and phenotype of Tregs. Briefly, PBMCs were re-suspended at 1 × 107/ml; blocked with 100 μl human AB serum and then 100 μl (1 × 106) cells/tube were incubated with CD3, CD4, CD25, CD69, CD62L, CD45RA, CD45RO, CD127, and GITR for 30 min at 4°C for extracellular surface staining. Intracellular staining was performed with CD152, Ki67, FOXP3, perforin, Granzyme A, and Granzyme B. Acquisition and data analysis were performed with FACSCalibur and CellQuest software (Becton Dickinson, CA, USA). The gate for the CD25+ isotype was set at 0% to ensure that the analysis is performed on CD25 high cells. Additional gating on the CD4+CD25+ cells deliberately focused on the CD25 high cells to ensure that further analysis included Tregs as oppose to activated CD4+ T cells.
Cell Proliferation Assay
The [3H]thymidine incorporation assay was performed per standard technique. Briefly, PBMCs, CD4+CD25+ or CD4+CD25− cells (1 × 105/well) were seeded into 96-well plate in triplicate in 200 μl cRPMI with 5 μg/ml PHA in the presence or absence of Huh7 cell supernatants, the three molecular weight fractions or normal hepatocyte culture supernatants at 37°C and 5% CO2. After 72 h, each well was pulsed with 1 μCi [3H]thymidine in 20 μl cRPMI for 18 h, harvested, and incorporation measured using a β-scintillation counter. Results were expressed as the mean counts per min (c.p.m.).
A series of co-culture studies with CD4+CD25− 1 × 105/well cultured with CD4+CD25+ cells at various ratios with PHA (Sigma, MO, USA; 5 μg/ml) or soluble anti-CD3 (10 μg/ml) plus anti-CD28 (10 μg/ml) were performed. Proliferation was measured after 72 h by [3H]thymidine incorporation.
Apoptosis Assay
Apoptosis in the PBMC co-cultured with Huh7 cells was determined using the Vybrant® Apoptosis Assay Kit#3 (Molecular Probes, OR, USA). Briefly, after 48 h of co-culture with Huh7 cells, PBMCs were isolated from the inner chamber and stained with Annexin V and propidium iodide (PI). Apoptosis was assessed by flow cytometry.
FOXP3 Quantitative Real-Time PCR
Total RNA was isolated from PBMCs using TRIzol (Invitrogen, CA, USA) and quantified using the Bio-RAC Smart Spec™ 3000. cDNA was prepared with high-capacity cDNA archive kit (AB Applied Biosystems, CA, USA). Forckhead/winged helix transcription factor (FOXP3) levels were quantified using Assay on Demand Gene Expression Products (TaqMan® MGB probes, FAM™ dye-labeled) kits and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) was used as the internal control. Primers for FOXP3 and GAPDH were obtained from Applied Biosystems. Amplification was conducted in a total volume of 25 μl in a GeneAmpR 7900 detection system with the following cycling conditions: 2 min at 50°C, 10 min at 95°C, followed by 40 cycles of 15 s at 95°C and 1 min at 60°C. Samples were run in duplicate, and their relative expression of FOXP3 was determined by normalizing the expression of each target to GAPDH and then comparing this normalized value to the normalized expression in a reference sample to calculate a fold change value using the delta-delta-Ct method. Results are shown as relative FOXP3 mRNA levels.
Statistical Analysis
Data are expressed as box plots and mean±s.e. Statistical analysis was performed using the Mann–Whitney U-test, and the Spearman correlation with the SPSS 10.1 program. All P values are two-tailed. Differences were considered to be significant if P<0.05.
Results
Frequency, Function, FOXP3 Expression and Correlation Analysis in Patients with HCC
We defined the number of CD4+CD25+ T cells in the peripheral blood of patients with HCC (n=33), chronic HCV infection (CHC; n=40), chronic HCV-related cirrhosis (n=15), and normal healthy controls (n=20) in an ex vivo fashion with flow cytometry. A significantly higher proportion of CD4+CD25+ cells were found in the periphery of HCC patients (mean, 6.34; s.e.±0.50%) when compared to healthy controls (2.06±0.19%), CHC (2.96±0.10%), and chronic HCVrelated cirrhosis (2.75±0.17%) (P<0.001) (Figure 1a). The presence or absence of cirrhosis did not change the level of CD4+CD25+ T cells in patients with chronic HCV infection. As shown in Figure 1b, the frequency of CD4+CD25+ T cells in viral-related HCC patients (6.32±0.50%) and non-viral HCC patients (5.14±1.12%) were equivalent, whereas subjects with non-tumor liver lesions had significantly lower levels of CD4+CD25+ T cells (2.31±0.18%; P=0.001).
CD4+CD25+ T-cell frequency and function in PBMCs. (a) Peripheral blood CD4+CD25+ T-cell frequency in normal healthy controls (n=20), CHC infection (n=40), chronic hepatitis C with cirrhosis (n=15), and viral-related HCC (n=33). Data are expressed as box plots, in which the horizontal lines illustrate the 25th, 50th, and 75th percentiles of the frequencies of the CD4+CD25+ T lymphocytes as assessed by flow cytometry. The vertical lines represent the 10th and 90th percentiles, and circles denote values outside these percentiles. (b) Peripheral blood CD4+CD25+T-cell frequency in viral hepatitis-related HCC (n=33), non-viral-related HCC (n=7), and non-HCC liver lesions including cysts, hemangiomas, fat, and focal nodular hyperplasia (n=10). (c) FOXP3 expression in patients with viral hepatitis (n=9), and viral hepatitis-related HCC (n=12) by quantitative real-time PCR analysis. The quantity of FOXP3 mRNA is expressed relative to normal healthy controls generated using the ΔΔCt method. (d) Mean proliferative response by [3H]thymidine incorporation of CD4+CD25− T cells in viral-related HCC (n=10) in response to PHA (5 μg/ml) when cultured alone (0:1) and on co-culture with CD4+CD25+ T cells (1:5). Isolated CD4+CD25+ cells suppressed CD4+CD25− proliferation on co-culture and failed to display any significant proliferation when cultured alone (1:0). (e) Correlation analysis between CD4+CD25+ T-cell frequency in viral-related HCC and tumor burden (n=30). Tumor burden is defined as the following: 1—single lesion <2 cm; 2—single lesion <5 cm; 3—multiple lesions; 4—vessel involvement; 5—evidence of metastatic disease. A significant correlation is found between CD4+CD25+ T-cell frequency and tumor burden by the nonparametric Spearman rank (R=0.537; P=0.002).
The transcription factor FOXP3 is a useful marker for the presence of Tregs as it is required for their development and function.31 Quantitation of FOXP3 by real-time PCR was performed on PBMCs from normal healthy controls, patients with viral hepatitis, and patients with HCC (Figure 1c). The relative quantity of the FOXP3 mRNA found in patients with chronic viral infection and HCC was normalized relative to healthy controls. FOXP3 expression was substantially higher in patients with HCC (sixfold) when compared to subjects with chronic viral infection (12.3±3.8 vs 1.9±0.9; P<0.05). The level of FOXP3 expression correlated well with the frequency of CD4+CD25+ T cells (R=0.776, P=0.02).
To verify that the elevated population of CD4+CD25+ cells in the HCC subjects represented the Treg phenotype with suppressive properties, a series of co-culture proliferation assays were performed to assess their inhibitory capacity. Purified CD4+CD25+ cells were cultured with autologous target CD4+CD25− cells at various ratios in the presence of polyclonal stimulation with PHA. Proliferation of the target cells was determined by incorporation of [3H]thymidine (Figure 1d). When cultured at a 1:5 ratio, purified CD4+CD25+ T cells inhibited the proliferation of CD4+CD25− cells (10 835±2495 c.p.m.) when compared to their proliferative capacity in the absence of CD4+CD25+ cells (0:1 ratio; 22 945±3530 c.p.m.). There was minimal proliferation by the pure isolated CD4+CD25+ T cells when cultured alone with PHA (524±191 c.p.m.).
To evaluate for any relationship between the frequency of CD4+CD25+ T cells and extent of tumor burden in patients with HCC, correlation analysis was performed. Correlation analysis showed a significant correlation between CD4+CD25+ T-cell frequency and tumor burden in HCC patients (R=0.489, P=0.01) (Figure 1e).
In Vitro Cultures of Hepatoma Cell Lines with Transwelled PBMC
To evaluate further the mechanism of how HCC may upregulate Tregs, we established an in vitro culture system with Huh7 cells, normal hepatocytes, and PBMCs from healthy controls. PBMCs were separated from cells using a transwell chamber to limit their interaction to soluble factors from Huh7 or normal hepatocyte supernatant. Changes in the frequency of the CD4+CD25+ T cells were assessed as a percentage of total CD4+ T cells by flow cytometry after labeling for CD3, CD4, and CD25 surface expression. These studies showed that supernatants from Huh7 and two additional liver cancer lines (HepG2 and Hclone5) significantly increase the CD4+CD25+ T-cell frequency from baseline levels before culture (mean±s.e.; 6.6±0.8%) after a 48 h culture period (n=8: Huh7 14.4±2.4%; HepG2 14.4±1.3%; Hclone5 15.1±2.7%) (all P<0.05, Figure 2a).
Increase of CD4+CD25+ and decrease of CD4+ lymphocytes in cultured PBMCs with liver cancer cells by transwell. (a) Mean CD4+CD25+ frequency in CD4+ population from PBMCs before and after co-culture with Huh7, HepG2, and Hclone5 cells (n=8). (b) A representative flow cytometric data showing the frequency of CD4+ lymphocytes (CD4+CD3+) and CD4+CD25+ T cells in the PBMCs from a normal healthy control prior to co-culture with Huh7 (no culture), after culture with medium alone (medium), after culture with normal human hepatocytes (normal) or after culture with Huh7 cells (Huh7).
To assess if the observed increase in Treg expansion is specific for cancer cell lines, we performed a series of PBMC co-cultures in the presence of medium alone, normal human hepatocytes or Huh7 cells. The result for a representative culture is shown in Figure 2b. There was a significant increase in the Treg frequency in the PBMC co-cultures with Huh7 cells (Huh7) when compared to the controls of PBMCs before culture (no culture), PBMCs with medium alone (medium) or PBMCs with normal hepatocytes (normal) (n=5, Huh7 14.02±1.93%, vs normal hepatocytes 8.53±0.32% P=0.0026). In contrast to the normal hepatocyte co-cultures, there was a noticeable decrease in the CD4+ population in Huh7 cell co-cultures during the culture period (49.59±1.14 vs 43.34±2.75%, P=0.0162).
Phenotype Analysis of CD4+CD25+ T Cells in PBMCs Co-Cultured with Huh7
The CD4+CD25+ T cells from the transwell culture studies were analyzed for expression of typical cell surface markers, which have been well documented in Treg cells32 as well as for Ki67, granzyme A, and granzyme B. Representative histograms and dot plots showing the impact of co-culture with Huh7 cells on the phenotype of Tregs are shown in Figure 3. The phenotype of the Tregs was also determined in the PBMCs from control cultures that included medium alone and normal human hepatocytes. The frequency of the extracellular and intracellular markers that were stained was statistically equivalent to those observed within the normal PBMCs before co-culture with Huh7 cells (data not shown). In general, all the markers assessed were upregulated on CD4+CD25+ T cells during co-culture of PBMCs with Huh7. However, those markers whose levels were markedly increased included CD62L (20–126%), GITR (16–31%), CD45RO (71–150%), FOXP3 (13.72–18.86%), and CTLA-4 (CD152, 17–61%). CD69, CD45RA, Ki67, granzyme A, and granzyme B expression were also upregulated but to a lesser degree.
Phenotype analysis. Representative plots of PBMCs before and after co-culture with Huh7 cells. (a) Extracellular markers. (b) Intracellular markers. The degree of staining for the extracellular and intracellular markers for the control cultures (medium alone and normal hepatocytes) were statistically equivalent to the level of staining on the PBMCs before co-culture with Huh7 cells (data not shown) when labeled with antibodies for CD3, CD4, CD25, CD69, CD62L, CD45RA, CD45RO, GITR, CTLA-4, Ki67, FOXP3, granzyme A, granzyme B, and isotypes. Profiles were generated by gating on the CD25 high cells.
FOXP3 Expression in PBMCs Exposed to Huh7 Supernatant during Cultures
As shown in Figure 4a, there was a twofold increase in FOXP3 expression at the mRNA level from baseline when PBMCs were co-cultured with Huh7 for 48 h. The induction of FOXP3 mRNA expression accompanied the upregulation of CD4+CD25+ T cells and its expression remained stable 72 h into the culture period. A similar induction of FOXP3 mRNA was observed when PBMCs were cultured with increasing concentrations of Huh7 supernatant (Figure 4b).
Functional Analysis of CD4+CD25+ T Cells from Huh7 and PBMC Cultures
CD4+CD25− cells were isolated from fresh PBMCs and stimulated with soluble anti-CD3 and anti-CD28, and cultured with different ratios of CD4+CD25+ T cells derived from fresh PBMCs (before culture) or PBMC from the transwell cultures (after culture) (Figure 5). Isolated CD4+CD25+ cells had no significant proliferative response to anti-CD3 and anti-CD28 stimulation but suppressed the proliferation of target CD4+CD25− T cells. In contrast to the suppression observed by the CD4+CD25+ cells from control PBMCs (1:1; 13852±4406 c.p.m.), the suppressor ability of the CD4+CD25+ cells from the PBMC co-cultures with Huh7 was more pronounced (1:1; 4369±614 c.p.m.) (P=0.006).
Functional analysis of CD4+CD25+ T cells derived from cultured PBMCs with Huh7 cells. CD4+CD25+ cells from PBMCs before and after co-culture with Huh7 cells were evaluated for their ability to suppress CD4+CD25− target cell proliferation by [3H]thymidine incorporation when stimulated with anti-CD3 and anti-CD28 at various ratios. Co-culture of PBMCs with Huh7 by transwell enhanced the suppressor ability of CD4+CD25+ T cells when compared to the suppressor ability of CD4+CD25+ T cells derived from PBMCs before culture with Huh7.
HCC Supernatants Specifically Suppress PBMC Proliferation in Dose-Dependent Way
We compared the effect of supernatants derived from HCC cell lines (Huh7, HepG2, Hep3B) and normal hepatocytes on PBMC proliferation (Figure 6a). Suppression of PBMC proliferation [3H]thymidine incorporation in response to polyclonal stimulation was consistently observed with the use of HCC supernatants and not with supernatant from normal hepatocytes. Serial dilutions of the Huh7 supernatant (1:2, 1:4, 1:8, 1:16, and 1:32) revealed a dose-dependent suppression of PBMC proliferation (Figure 6b).
Supernatants from Huh7 cells inhibit T-cell proliferation and induce CD4+ T-cell apoptosis. PBMCs were cultured with supernatants from various liver cancer cell lines (Huh7, Hep G2, Hep3B) and controls (medium alone, normal hepatocytes) for 3 days to assess their ability to proliferate in response to stimulation with anti-CD3 (10 μg/ml) by [3H]thymidine incorporation (a). PBMCs were cultured with different dilutions of Huh7 supernatants for 3 days in response to stimulation with anti-CD3 (10 ìg/ml) by [3H]thymidine incorporation (b). Proliferation data are expressed as mean±s.d. (*P<0.05 vs control). PBMC were co-cultured with Huh7 cells for 48 h by transwell, collected, and stained with Annexin V and PI to evaluate for apoptosis. Representative dot plots for CD4+ lymphocytes apoptosis are shown (c).
Huh7 Cells Induce CD4+ T-Cell Apoptosis, Promote CD4+CD25+ Expansion and Inhibit CD4+CD25− Proliferation
To evaluate the mechanism by which Huh7 cells alter total CD4+ cell numbers, the level of CD4+ cells were followed during the co-cultures of Huh7 with transwelled PBMCs. Although these studies showed an increase in CD4+CD25+ T cells, the total CD4+ population decreased from 52 to 43% (Figure 2). Annexin V and PI staining showed this decrease to be related to induction of apoptosis in the CD4+ T-cell population (Figure 6c). Proliferation studies showed that the relative increase of CD4+CD25+ T cells was due to proliferation as Huh7 supernatants selectively promoted CD4+CD25+ T-cell expansion (1490±57 c.p.m. vs 125±55 c.p.m., P=0.0010) whereas inhibiting CD4+CD25− T-cell proliferation (1031±114 vs 18972±3176 c.p.m., P=0.0096). In contrast, normal hepatocyte culture supernatants promoted CD4+CD25− T-cell expansion (28391±3147 vs 18972±3176 c.p.m., P=0.0187) with no effect on CD4+CD25+ T-cell proliferation (147±19 vs 125±55 c.p.m., P=0.5336).
Discussion
The immune system plays a critical role in the surveillance of malignancy and control of tumor progression. In this study, we initially describe an increase in the frequency of Tregs in the peripheral blood of HCC patients, which suggests that they play a central role in tumor immunity. The relative level of FOXP3 mRNA expression along with the functional suppression assay results provide support that the elevated population of CD4+CD25+ T cells identified by flow cytometry in the HCC patients represents a suppressive Treg population. In addition, a significant correlation was found between CD4+CD25+ T-cell frequency and tumor stage in our HCC cohort with higher levels seen in those with vascular involvement and metastatic disease. Recently, a similar difference was found in the prevalence of CD4+CD25+high T cells between early and advanced disease stages in both gastric cancer and esophageal cancer.33 Patients with a higher proportion of CD4+CD25+high T cells had worse survival rates when compared to those patients with a lower proportion of CD4+CD25+high T cells for both gastric and esophageal cancers. These data provide clinical evidence for the concept that HCC affect the Treg subset promoting tolerance to tumor antigens. Further studies of sufficient sample size are needed to draw valid conclusions regarding the use of Treg frequency as a diagnostic or prognostic tool.
We then used an in vitro HCC transwell model to understand the underlying mechanisms responsible for the upregulation of Tregs observed in our clinical cohort. The in vitro co-cultures of hepatoma cells with PBMCs from healthy donors led to an increase in the number of CD4+CD25+ T cells, suggesting that cancer-derived soluble factors result in the expansion of Tregs. This increase was observed using three different liver cancer cell lines, suggesting that the expansion is not an artifact of a single liver cancer cell line but feature common to hepatoma cell lines. Human CD4+CD25+ T cells consist of a heterogeneous population containing regulatory and nonsuppressive effector/memory T cells. It is the CD4+CD25high T cells that garner the suppressive function characteristic of Tregs.34 In addition to the discriminating Tregs from activated CD4+ T cells by the comparatively high expression of CD25, additional markers such as CTLA-4, GITR, and CD45RO show strong expression in the CD4+CD25high T cells, which corresponds to Tregs. The subset of T cells in our cultures with the phenotype CD4+CD25+ express high levels of markers characteristic of Tregs including CD62L, GITR, CD45RO, and CD152. This analysis also found increased CD45RA expression, which is not a typical marker of Tregs. However, a recent study describes the existence of CD45RA+ Tregs in the periphery of humans that express high levels of FOXP3 and manifests equivalent suppressive activity in vitro when compared to their CD45RO+ Tregs counterparts.35 Of note, upregulation of FOXP3 mRNA expression occurred during the co-cultures of PBMCs with Huh7 supernatant supporting that the increased CD4+CD25+ T cells in the cultures represent Tregs.
Although the presence of these markers is helpful in enumerating and detecting the presence of Tregs, the ultimate test for their presence is demonstrating suppression of target CD4+CD25− T-cell activity. Analysis of the CD4+CD25+ T cells induced by the supernatant of Huh7 co-cultures by proliferation assays reveals that these cells inhibited the proliferative response of CD4+CD25− T cells and induce relative anergy towards TCR stimulation. This functional analysis further confirms that the population of CD4+CD25+ T cells in the co-cultures corresponds to Tregs. An important finding is also the enhancement of suppressor ability by the CD4+CD25+ T cells derived from the co-cultures, which indicates that tumor factors may not only increase Treg numbers but also increases their suppressive activity. Some insight into the mechanisms for increased Treg numbers and function can be inferred from our data.
Although prior studies show that CD4+CD25− T cells can be induced into suppressing CD4+CD25+ T cells by peripheral expansion,36 we were able to demonstrate that the increase in Treg frequency was derived from natural Treg self-expansion promoted by factors secreted by Huh7 cells and not from conversion of naïve CD4+CD25− T cells. Our data also show that Huh7 supernatants and not normal hepatocyte culture supernatants inhibited PBMC proliferation in dose-dependent manner. The flow cytometry analysis also showed that Huh7 supernatants induced CD4+ T cells apoptosis while increasing CD4+CD25+ T-cell frequency. Both naturally occurring and adaptive Tregs have been shown to kill autologous target cells, including activated CD4+ and CD8+ T cells, CD14+ monocytes, and both immature and mature dendritic cells, in a CD18 and perforin-dependent manner.37 Here, we demonstrate that CD4+CD25+ cells express higher levels of granzyme A and granzyme B when cultured with the supernatant from a liver cancer cell line. These findings suggest that the granzyme pathway may be one of the mechanisms that Tregs use in the tumor environment to induce cell-contact dependent suppression and kill effector T cells to control immune responses.
In summary, we found an elevation of Tregs with enhanced suppressive function in the peripheral blood of patients with HCC, which correlated with stage of HCC. Collectively, our clinical and experimental data strongly suggest that HCC-derived soluble factor(s) selectively enhances their immunosuppression capabilities and leads to apoptosis of effector T cells. We have begun to isolate the cellular fractions that are responsible for this ‘suppressive’ effect. A better understanding of the mechanisms of the Treg increase in HCC may allow for future immunotherapeutic and diagnostic opportunities in this population.
References
Piccirillo CA, Shevach EM . Cutting edge: control of CD8+ T cell activation by CD4+CD25+ immunoregulaotry cells. J Immunol 2001;167:1137–1140.
Takahashi T, Kuniyasu Y, Toda M, et al. Immunologic self-tolerance maintained by CD25+CD4+ naturally anergic and suppressive T cells: induction of autoimmune diseases by breaking their anergic/suppressive state. Int Immunol 1998;10:1969–1980.
Shimizu J, Yamazaki S, Sakaguchi S . Induction of tumor immunity by removing CD25+CD4+ T cells: a common basis between tumor immunity and autoimmunity. J Immunol 1999;163:5211–5218.
Belkaid Y, Piccirillo CA, Mendez S, et al. CD4+CD25+ regulatory T cells control Leishmania major persistence and immunity. Nature 2002;420:502–507.
Cabrera R, Tu Z, Xu Y, et al. An immunomodulatory role for CD4+CD25+ regulatory T lymphocytes in hepatitis C virus infection. Hepatology 2004;40:1062–1071.
Stoop JN, van der Molen RG, Baan CC, et al. Regulatory T cells contribute to the impaired immune response in patients with chronic hepatitis B virus infection. Hepatology 2005;41:771–778.
Sugimoto K, Ikeda F, Stadanlick J, et al. Suppression of HCV-specific T cells without differential hierarchy demonstrated ex vivo in persistent HCV infection. Hepatology 2003;38:1437–1448.
Linehan DC, Goedegebuure PS . CD25+CD4+ regulatory T-cells in cancer. Immunol Res 2005;32:155–168.
Awwad M, North RJ . Cyclophosphamide-induced immunologically mediated regression of a cyclophosphamide-resistant murine tumor: a consequence of eliminating precursor L3T4+ suppressor T-cells. Cancer Res 1989;49:1649–1654.
Awwad M, North RJ . Radiosensitive barrier to T-cell-mediated adoptive immunotherapy of established tumors. Cancer Res 1990;50:2228–2233.
Rakhmilevich AL, North RJ, Dye ES . Presence of CD4+ T suppressor cells in mice rendered unresponsive to tumor antigens by intravenous injection of irradiated tumor cells. Int J Cancer 1993;55:338–343.
Shevach EM . Certified professionals: CD4+CD25+ suppressor T cells. J Exp Med 2001;193:F41–F46.
Sutmuller RP, van Duivenvoorde LM, van Elsas A, et al. Synergism of cytotoxic T lymphocyte-associated antigen 4 blockade and depletion of CD25+ regulatory T cells in antitumor therapy reveals alternative pathways for suppression of autoreactive cytotoxic T lymphocyte responses. J Exp Med 2001;194:823–832.
Onizuka S, Tawara I, Shimizu J, et al. Tumor rejection by in vivo administration of anti-CD25 (interleukin-2 receptor α) monoclonal antibody. Cancer Res 1999;59:3128–3133.
Yu P, Lee Y, Liu W, et al. Intratumor depletion of CD4+ cells unmasks tumor immunogenicity leading to the rejection of late-stage tumors. J Exp Med 2005;201:779–791.
Llovet JM, Burroughs A, Bruix J . Hepatocellular carcinoma. Lancet 2003;362:1907–1917.
Kalos M . Tumor antigen-specific T cells and cancer immunotherapy: Current issues and future prospects. Vaccine 2003;21:781–786.
Chavan SS, Chiplunkar SV . Immunophenotypes and cytotoxic functions of lymphocytes in patients with hepatocellular carcinoma. Tumori 1997;83:762–767.
Wada Y, Nakashima O, Kutami R, et al. Clinicopathological study on hepatocellular carcinoma with lymphocytic infiltration. Hepatology 1998;27:407–414.
Curiel TJ, Coukos G, Zou L, et al. Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat Med 2004;10:942–949.
Schaefer C, Kim GG, Albers A, et al. Characteristics of CD4+CD25+ regulatory T cells in the peripheral circulation of patients with head and neck cancer. Br J Cancer 2005;92:913–920.
Wolf AM, Wolf D, Steurer M, et al. Increase of regulatory T cells in the peripheral blood of cancer patients. Clin Cancer Res 2003;9:606–612.
Gray CP, Arosio P, Hersey P . Association of increased levels of heavy-chain ferritin with increased CD4+ CD25+ regulatory T-cell levels in patients with melanoma. Clin Cancer Res 2003;9:2551–2559.
Ichihara F, Kono K, Takahashi A, et al. Increased populations of regulatory T cells in peripheral blood and tumor-infiltrating lymphocytes in patients with gastric and esophageal cancers. Clin Cancer Res 2003;9:4404–4408.
Woo EY, Chu CS, Goletz TJ, et al. Regulatory CD4+CD25+ T cells in tumors from patients with early-stage non-small cell lung cancer and late-stage ovarian cancer. Cancer Res 2001;61:4766–4772.
Ormandy LA, Hillemann T, Wedemeyer H, et al. Increased populations of regulatory T cells in peripheral blood of patients with hepatocellular carcinoma. Cancer Res 2005;65:2457–2464.
Unitt E, Rushbrook SM, Marshall A, et al. Compromised lymphocytes infiltrate hepatocellular carcinoma: the role of T-regulatory cells. Hepatology 2005;41:722–730.
Wolf D, Rumpold H, Koppelstatter C, et al. Telomere length of in vivo expanded CD4+CD25+ regulatory T-cells is preserved in cancer patients. Cancer Immunol Immunother 2005;16:1–11.
Bruix J, Sherman M . Practice Guidelines Committee, American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma. Hepatology 2005;42:1208–1236.
Nelson DR, Tu Z, Soldevila-Pico C, et al. Long-term interleukin 10 therapy in chronic hepatitis C patients has a proviral and anti-inflammatory effect. Hepatology 2003;38:859–868.
Ramsdell F . FOXP3 and natural regulatory T cells: key to a cell lineage? Immunity 2003;19:165–168.
Baecher-Allan C, Brown JA, Freeman GJ, et al. CD4+CD25high regulatory cells in human peripheral blood. J Immunol 2001;167:1245–1253.
Kono K, Kawaida H, Takahashi A, et al. CD4+CD25high regulatory T cells increase with tumor stage in patients with gastric and esophageal cancers. Cancer Immunol Immunother 2005;23:1–8.
Baecher-Allan C, Viglietta V, Hafler DA . Human CD4+CD25+ regulatory T cells. Semin Immunol 2004;26:89–97.
Seddiki N, Santner-Nanan B, Tangye SG, et al. Persistence of naive CD45RA+ regulatory T cells in adult life. Blood 2006;107:2830–2838.
Chen ZM, O'Shaughnessy MJ, Gramaglia I, et al. IL-10 and TGF-beta induce alloreactive CD4+CD25- T cells to acquire regulatory cell function. Blood 2003;101:5076–5083.
Grossman WJ, Verbsky JW, Barchet W, et al. Human T regulatory cells can use the perforin pathway to cause autologous target cell death. Immunity 2004;21:589–601.
Acknowledgements
This work was supported by NIH Grant DK2595, HL64817, GCRC Grant RR00082 and R01 (DRN); American Liver Foundation and NIDDK Grant DK02958 (CL); and NIH T32 training grant and NIH-LRP (RC).
Author information
Authors and Affiliations
Corresponding author
Additional information
Duality of interest
None declared.
Rights and permissions
About this article
Cite this article
Cao, M., Cabrera, R., Xu, Y. et al. Hepatocellular carcinoma cell supernatants increase expansion and function of CD4+CD25+ regulatory T cells. Lab Invest 87, 582–590 (2007). https://doi.org/10.1038/labinvest.3700540
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.3700540
Keywords
This article is cited by
-
Presence of regulatory T-cells in endometrial cancer predicts poorer overall survival and promotes progression of tumor cells
Cellular Oncology (2022)
-
Effects of transarterial chemoembolization on regulatory T cell and its subpopulations in patients with hepatocellular carcinoma
Hepatology International (2020)
-
Current perspectives on the immunosuppressive tumor microenvironment in hepatocellular carcinoma: challenges and opportunities
Molecular Cancer (2019)
-
CD4+ regulatory T cells in gastric cancer mucosa are proliferating and express high levels of IL-10 but little TGF-β
Gastric Cancer (2017)
-
High seroprevalence of human herpesvirus type 8 in patients with hepatocellular carcinoma
European Journal of Clinical Microbiology & Infectious Diseases (2015)