Abstract
Mesangial cell apoptosis occurs in experimental diabetic nephropathy, and this correlates with worsening albuminuria. This study examines the mechanism by which glucose modulates mesangial cell apoptosis. Apoptosis was induced in mesangial cells by serum deprivation in the presence of 5 or 25 mM D-glucose, and examined by expression of Annexin-V and disruption of mitochondrial transmembrane potential. Involvement of Bax, Bcl-2 and NF-κB were examined by RT-PCR and EMSA. Involvement of TGF-β1 was sought by determining the effect of recombinant TGF-β1on apoptosis and the mediators of the apoptotic pathway (Bcl2/Bax and NF-κB). Culture of cells in the presence of 25 mM D-glucose (i) enhanced apoptosis stimulated by serum depletion, (ii) enhanced activation of caspase-3, (iii) inhibited NF-κB activation, and (iv) decreased Bcl-2:Bax ratio. Inhibition of NF-κB using SN50, also increased mesangial cell apoptosis, and decreased Bcl-2:Bax ratio. Addition of TGF-β1 to mesangial cells mimicked the effect of high glucose reducing NF-κB expression and Bcl-2:Bax ratio. Furthermore glucose-mediated enhanced apoptosis was inhibited by the addition of a blocking antibody to TGF-β1. Exposure of mesangial cells to 25 mM D-glucose stimulated the generation of both total and active TGF-β1 in the cell culture supernatant, this increase was only significant after 48–72 h, that is at a time point later than enhanced apoptosis. Addition of 25 mM D-glucose, however, increased sensitivity of mesangial cells to TGF-β1 as assessed by luciferase activity of a Smad sensitive reporter construct. The data suggest that elevated glucose concentration enhanced the pathway leading to apoptosis following serum deprivation. Furthermore, it is likely that this is dependent on glucose-mediated enhanced sensitivity to endogenous TGF-β1 rather than glucose stimulated de novo TGF-β1 synthesis.
Similar content being viewed by others
Main
Diabetic nephropathy is a leading cause of end-stage renal disease, which confers high morbidity and mortality rates in diabetic patients. Although nephropathy is a complication of both type I and type II diabetes,1 the increase in its incidence relates predominantly to an increase in the incidence of type 2 diabetes.
Mesangial cells play a crucial role in maintaining structure and function of glomerular tufts, providing structural support for capillary loops and modulating glomerular filtration by their contractility.2, 3 The early stages of diabetic nephropathy are characterised by thickening of the glomerular basement membrane and glomerular hypertrophy. Increasing mesangial cell number has been documented in the incipient phase of nephropathy, with a direct correlation between mesangial cell number and albumin excretion rates.4 This relationship between mesangial cell number is, however, lost in patients with overt nephropathy and proteinuria. In overt nephropathy, expansion of the mesangial matrix, mesangial cell loss and glomerular sclerosis are prominent, associated with proteinuria, hypertension and renal dysfunction.5, 6 More recently, it has been demonstrated that loss of resident glomerular cells through apoptosis occurs in experimental diabetic nephropathy,7 and mesangial cell apoptosis has been demonstrated to correlate with worsening of albuminuria.8 Significantly recent studies suggest that high glucose evokes an intrinsic proapototic pathway in mesangial cells.8 Understanding the mechanisms, which regulate mesangial cell number in diabetes, is therefore an important goal.
Increased susceptibility to long-term diabetic complications in patients with poor glycaemic control has been demonstrated in a number of epidemiological studies.9 In addition, strict metabolic control in the very early stages of nephropathy may delay the development of microvascular complications of diabetes.10, 11, 12, 13 Numerous in vitro studies have suggested that elevated concentrations of glucose modify mesangial cell function. Studies by Wolf et al14 demonstrated a biphasic growth response of mesangial cells when they were cultured in high glucose concentration; initially there was stimulation of replication followed by a sustained inhibition after longer incubation periods. Exposure of mesangial cells to high glucose levels also promotes transcriptional activation of type IV collagen and fibronectin genes, and increased the synthesis of their respective proteins.15, 16, 17 There is also evidence that in addition to increased synthesis of extracellular matrix (ECM) components, glucose may also decrease degradation of matrix components which may also contribute to ECM accumulation in the diabetic state.18
In the current study, we have examined the mechanism by which high glucose modulates mesangial cell apoptosis. The results demonstrate that an elevated concentration of glucose sensitises mesangial cells to the effects of TGF-β1, which subsequently decreases NF-κB activation and in turn, alters the expression ratio of Bcl-2:Bax favouring caspase-3 activation and increased apoptosis.
Materials and methods
Reagents
Inhibitors, antibodies and reagents and their sources were as follows: cell culture media, penicillin/streptomycin, L-glutamine, HEPES and hydrocortisone (Life Technologies, Paisley, UK); insulin, transferrin and sodium selenite (Sigma-Aldrich Co Ltd, Gillingham, UK); foetal bovine serum (Autogen Bioclear UK Ltd, Calne, UK); recombinant human TGF-β1 (R&D Systems Europe Ltd, Abingdon, UK); pan-specific TGF-β antibody (R&D Systems Europe Ltd); SN50 cell permeable NFκB inhibitor peptide (Merck Biosciences Ltd, Nottingham, UK); alamar blue (Biosource UK Ltd, Nivelles, Belgium); Bright-Glo™ luciferase assay reporter system (Promega, Southampton, UK).
Cell Culture
All experiments were performed using spontaneously transformed rat mesangial cell lines. Cells were cultured in a 1:1 ratio of RPMI-1640/Dulbecco's modified Eagle's medium without glucose supplemented with 10% foetal bovine serum, insulin, transferrin, sodium selenite, penicillin, streptomycin and L-glutamine.
Flow Cytometry
Cell surface binding of Annexin-V was examined by flow-cytometry. The cells were washed in phosphate-buffered saline (PBS) and resuspended in 100 μl of the reaction mix made up of 90 μl distilled water, 10 μl 10 × binding buffer, 100 mM HEPES, 1.5 M NaCl, 50 mM KCl, 10 mM MgCl2 and 18 mM CaCl2, pH 7.4) 5 μl Annexin-V conjugated to FITC (Pharmingen, UK) and 5 μl propidium iodide (PI, Pharmingen, UK). The cells were incubated in the dark for 20 min at room temperature, centrifuged, washed in PBS and resuspended in 1 × binding buffer. The sample was analysed immediately by flow cytometry (FACSCalibur, Becton Dickinson, Oxford, UK). The viable cells were Annexin-V/PI negative, cells in early apoptosis were Annexin-V positive and PI negative and cells in late apoptosis/necrosis were Annexin-V/PI positive.
To determine disruption of mitochondrial transmembrane potential, cells were washed in PBS resuspended in 1 ml of diluted DePsipher solution (R&D Systems Europe Ltd) and incubated at 37°C, 5% CO2 for 30 min. The samples were washed twice, resuspended in PBS and analysed immediately with a flow cytometer.
Detection of Caspase-3
The caspase-3 assay kit (BD Biosciences) was used to quantify caspase-3 in cell lysates following the protocol of the manufacturer. Samples and standards were setup in duplicate in a 96-well plate and read at 405 nm in a microplate reader (FLUOstar and POLARstar OPTIMA, BMG Labtechnologies, Aylesbury, UK). Cell number was assessed by the ability of monolayers to reduce the dye alamarBlue. At the end of each experimental period/manipulation, alamarBlue reagent was added to make up a final volume of 10% of the culture medium. The cells were returned to the incubator for 1 h, after which 100 μl aliquots of medium were quantified for alamarBlue fluorescence using a Fluostar Optima Fluorescence Meter excitation wavelength 544 nm, detection wavelength 590 nm.
Immunobloting/Western Analysis
Total and activated/cleaved caspase-3 protein were examined by Western blot analysis using standard methodologies using a polyclonal caspase-3 antibody raised to a synthetic peptide corresponding to residues surrounding the cleavage site and the amino-terminus of the large fragment of human caspase-3 (Cell Signaling Technology Inc, Beverly, MA, USA). Bcl2 and Bax protein were examined by Western analysis using a monoclonal anti Bcl2 antibody (R&D Systems Europe Ltd) and a polyclonal rabitt anti Bax antibody (Autogen Bioclear UK Ltd) respectively. Briefly, cells were scraped off into 1.0 ml of PBS using a cell scraper, pelleted at 1600 r.p.m., 4°C for 7 min before resuspension of the pellet in 100 μl of NP-40 Buffer (0.5% NP-40 in TBS, 5 mM EDTA, 1 mM PMSF, 2% v/v protease inhibitors, pH 7.5). The samples were vortexed for 10 seconds, incubated on ice for 10 min followed by centrifugation at 13 000 r.p.m., 4°C for 3 min. The supernatant was transferred to a sterile eppendorf and stored at −20°C. The Bradford assay was used to quantify protein concentrations in the extracts. 100 μg of protein was prepared in SDS sample buffer (2%SDS, 10% v/v glycerol, 60 mM TRIS and 0.05% v/v mercaptoethanol) and boiled for 5 min prior to loading onto 12% SDS-PAGE gels. Electrophoresis was carried out under reducing conditions according to the procedure of Laemmli.19 After electrophoresis the separated proteins were transferred to a nitrocellulose membrane (Amersham Pharmacia, Biotech UK Ltd, Buckinghamshire, UK). The membrane was blocked with Tris-buffered saline containing 5% non-fat powdered milk for 1 h and then incubated with the primary antibody in Tris-buffered saline containing 1% bovine serum albumin and 0.1% Tween 20 (Tris-buffered saline-Tween) over-night at 4°C. The blots were subsequently washed in Tris-buffered saline-Tween and then incubated with an appropriate HRP-conjugated secondary antibody (Sigma) in Tris-buffered saline-Tween. Proteins were visualised using enhanced chemiluminescence (Amersham) according to the manufacturer's instructions.
RT-PCR
Alterations in of Bax and Bcl-2 mRNA expression were examined by RT-PCR performed using specific oligonucleotide primers as previously described20 (Table 1). PCR amplification was performed over a range of cycle numbers21, 22, 23, 24, 25, 26, 27, 28, 29, 30 to ensure that amplification was in the linear range of the curve. One-tenth of the PCR reaction from both test and control (β-actin) product were mixed and separated by flat bed electrophoresis in 3% w/v NuSieve GTG agarose gels (Flowgen Instruments Ltd, Sittingbourne, UK), stained with ethidium bromide (Sigma) and photographed. The negatives were scanned using a densitometer (Model 620 video densitometer, Bio-Rad Laboratories Ltd) and the density of the bands compared to those of the housekeeping gene.
EMSA-NF-κB
Cells were scraped, washed and suspended in 400 μl of ice-cold Buffer A (10 mM HEPES-KOH, 1.5 mM MgCl2, 10 mM KCl, 0.5 mM DTT and 0.2 mM PMSF, pH 7.9). The cells were incubated on ice for 10 min, vortexed, centrifuged for 10 s at 13 000 r.p.m. and resuspended in 50 μl ice-cold Buffer C (20 mM HEPES-KOH, 25% glycerol, 420 mM NaCl, 1.5 mM MgCl2, 0.2 mM EDTA, 0.3 mM DTT and 0.2 mM PMSF, pH 7.9). Subsequently cells were incubated on ice for 20 min, vortexed and centrifuged for 10 s at 13 000 r.p.m. The Bradford assay (BioRad) was used to quantify protein concentrations in the extracts.
An oligonucleotide containing the consensus motif for NFκB (5′-CGAAGTTGAGGGGACTTTCCCAGGC-3′, 5′-CGAGCCTGGGAAAGTCCCCTCAACT-3′) was prepared by annealing the two sequences. A 1 μg/μl stock of each strand was prepared in sterile water. A mixture of 10 μl (from 1 μg/μl stock) of each strand, 10 μl 1 M NaCl and 70 μl sterile water was prepared, heated to 95°C for 5 min and then allowed to cool at room temperature. The annealed oligonucleotide (10 ng/μl stock) was labelled with a dTTP-[32P] radioisotope (Amersham Biosciences). A labelling reaction mix was prepared, consisting of 2.5 μl oligonucleotide stock (25 ng/ml, Promega), 1.0 μl non-labelled dNTPs (2.5 mM × 3), 5 μl 10 × Klenow buffer (Promega), 5 μl 1 M NaCl and 32.5 μl distilled water. dTTP-[32P] (3 μl) was then added to the labelling reaction mix along with 1 μl of the Klenow fragment of DNA polymerase I (2 U/μl, Promega). The labelling reaction was incubated at room temperature for 20 min and the reaction stopped by the addition of 2 μl EDTA (0.5 M, pH 8.0) and 50 μl STE buffer (100 mM NaCl, 10 mM Tris-Cl and 1 mM EDTA, pH 8.0). The radiolabelled probe was cleaned of any excess radioactivity using ProbeQuant G-50 micro columns (Amersham Biosciences). A binding reaction mix was made up of 4 μl 5 × binding buffer (1 μl 0.1 M PMSF, 0.5 μl 1 M DTT, 10 μl acetylated BSA (Sigma) and 89 μl 5 × reactiob buffer—50 μl 1 M HEPES, 250 μl 1 M KCl, 500 μl 100% glycerol and 90 μl water), 5 μg nuclear protein extract, 1 μl poly dI/dC (Amersham Biosciences) and the total volume made up to 18 μl with distilled water. This mixture was incubated at room temperature for 10 min, 2 μl of the [32P]-labelled oligonucleotide probe was added and the mix incubated for a further 20 min and then loaded onto a 6% polyacrylamide gel with no tracker dye. The samples were electrophoresed at 100 V for 3–5 in 0.5% TBE (54 g Tris-base, 27.5 g boric acid, 20 ml 0.5 M EDTA and 1 L H2O, pH 8.0) at 4°C. Following electrophoresis, the gel was dried using a BioRad vacuum gel dryer for one hour at 70°C, and the dried gel exposed to an X-ray film (Hyperfilm, Amersham Biosciences) at −70°C for 6–48 h.
TGF-β1 ELISA
Total TGF-β1 in the cell culture supernatant was measured by specific enzyme-linked immunosorbent assay (ELISA) (R&D Systems Europe Ltd) of cell culture supernatant samples. This assay has <1% cross-reactivity for TGF-β2 and TGF-β3.
TGF-β1 Bioactivity and Sensitivity
Activity of TGF-β1 was measured by determining the effect of mesangial cell conditioned medium on HK-2 cells transiently transfected with a Smad-responsive luciferase promoter construct as we have previously described.31 HK-2 cells were cultured in a 1:1 ratio of Ham's F12/Dulbecco's modified Eagle's medium supplemented with 10% fetal bovine serum, HEPES, L-glutamine, insulin, transferrin, sodium selenite and hydrocortisone. The Smad-responsive promoter (SBE)4-Lux, was a gift from Aristidis Moustakas.32 Cells (HK2 cell/TGF-β bioassay or mesangial cells/ TGF-β1 sensitivity) were transfected over night with 1 μg of the Smad responsive promoter-luciferase construct, using the lipofection reagent FuGene 6 (Roche) at a ratio of 3 μl Fugene to 1 μg DNA in serum-free and insulin-free medium.
For assessment of TGF-β1 bioactivity, conditioned media were added to transfected HK-2 cells prior to determination of luciferase activity. Conditioned medium was generated by culturing mesangial cells, under serum-free conditions, in either 5 or 25 mM D-glucose for 72 h. Subsequently either untreated conditioned medium or conditioned medium subjected to 10 cycles of freeze-thawing were added to cells transfected with the Smad reporter construct 24 h prior to determining luciferase activity. Repeated cycles of freeze-thawing of samples are well established in vitro mechanisms of activation of latent TGF-β1.33
Assessment of TGF-β1 sensitivity was determined by addition of 1 ng/ml of recombinant TGF-β1 to transfected mesangial cells and luciferase activity quantified.
Statistical Analysis
Statistical analysis was performed using the unpaired Student's t-test, with a value of P<0.05 considered to represent a significant difference. The data are presented as means±s.d. of n experiments as indicated in figure legends. For each individual experiment the mean of duplicate determinations was calculated.
Results
25 mM D-Glucose Induced Enhanced Mesangial Cell Apoptosis
To determine the time dependent effect of high glucose concentration on mesangial cell apoptosis induced by serum deprivation, confluent mesangial cells were cultured in serum-free medium containing 5 or 25 mM D glucose for up to 72 h. Annexin-V is a Ca2+ dependent phospholipid-binding protein that has high affinity for phosphatidylserine (PS) which itself is translocated from the inner to the outer leaflet of the plasma membrane during the early phase of the apoptotic process. Apoptotic cells were identified by flow cytometry using Annexin-V conjugated to fluorescein isothiocyanate (FITC), in conjunction with propidium iodide (PI) to distinguish apoptotic cells (Annexin-V-FITC positive, PI negative) from necrotic cells (Annexin-V-FITC positive, PI positive). Using this method as a marker of apoptosis, exposure of mesangial cells to 25 mM D-glucose under serum-free conditions for 72 h led to a significant increase (29.1% compared to 21.9% P=0.002) in the number of cells in early apoptosis as compared to cells exposed to 5 mM D-glucose for the same time (Figure 1a). Addition of 25 mM L-glucose did not affect apoptosis induced by serum withdrawal (data not shown).
Time dependent effects D-glucose on mesangial cell apoptosis and caspase-3 activation. Mesangial cells were grown to confluence. Subsequently apoptosis was induced by serum-deprivation either in the presence of 5 mM D-glucose (stippled bars) or 25 mM D-glucose (Solid bars). At the time points indicated, apoptotic cells were identified by flow cytometry using Annexin-V conjugated to fluorescein isothiocyanate (FITC), in conjunction with propidium iodide (PI) to distinguish apoptotic cells (Annexin-V-FITC positive, PI negative) from necrotic cells (Annexin-V-FITC positive, PI positive) (a), or by DePsipher flow cytometry assay (b). Results are presented graphically as the % of cells in early apoptosis and represent the mean±s.d. of six individual experiments. For both (a) and (b) the figure insert provides a representative scatter plot of flow cytometry results for both methods illustrating the population of early apoptotic cells. (c) Following serum-deprivation for the time points indicated, either in the presence of 5 mM D-glucose (stippled bars), or 25 mM D-glucose (solid bars) the cell layer was lysed as described in Materials and methods. Cell lysate caspase-3 was quantified by colorimetric assay. Data represents mean±s.d. of three individual experiments. (d) In parallel experiments caspase-3 expression and activation was assessed by Western blot analysis. Equal loading of gels was confirmed by re-probing the membranes for β-actin.
Cellular energy produced during mitochondrial respiration is stored as an electrochemical gradient across the mitochondrial membrane, creating a mitochondrial transmembrane potential. Disruption of this potential is one of the first intracellular changes following the onset of apoptosis. DePsipher™ is a lipophilic cation (5,5′,6,6′-tretrachloro-1,1′3,3′-tetraethylbenzimidazolyl carbocyanine iodide) which can be used as a mitochondrial activity marker. It has the property of aggregating upon membrane polarization forming an orange–red fluorescent compound. If the potential is disturbed, the dye cannot access the trans-membrane space and remains in its green monomeric form. Fluorescence can be analysed by flow cytometry, and thus this method was also used to detect early apoptosis. By DePsipher flow cytometry assay, exposure of mesangial cells to 25 mM D-glucose under serum-free conditions led to a significant increase in the number of cells in early apoptosis compared to that seen following addition of 5 mM D-glucose (Figure 1b), both at 48 h (27 vs 18%, P=0.007) and 72 h (30 vs 15% P=0.026).
Caspase-3 is an active cell-death protease involved in the execution phase of apoptosis. Further confirmation of activation of the apoptotic pathway was therefore sought by colorimetric assay of caspase-3. Consistent with the data demonstrating alteration in Annexin-V and altered membrane potential, exposure of mesangial cells to 25 mM D-glucose for 72 h under serum-free conditions, led to a 2.7-fold increase (n=3, P=0.02) in caspase-3 activity compared to exposure to 5 mM D-glucose (Figure 1c). Similarly using Western blot analysis, there was an increase in both total caspase-3 expression, and caspase-3 activation as demonstrated by the appearance of cleaved caspase-3 products upon exposure of mesangial cells to 25 mM D-glucose (Figure 1d).
Glucose Augments Increased Bax:Bcl2 Ratio Following Serum Withdrawal
To examine the potential mediators of glucose induced apoptosis, we analysed the relative mRNA expression of the Bcl-2 related proteins, Bcl-2 and Bax. A correlation between mRNA and protein expression has been demonstrated for Bax and Bcl-2 in mesangial cells in vivo.34 Confluent cells were exposed to either 25 mM D-glucose or 5 mM D-glucose under serum-free conditions for up to 72 h. Total mRNA was isolated at the indicated time points and Bcl-2 or Bax mRNA expression examined by RT-PCR (Figure 2a). Under serum-free conditions no change in Bax mRNA expression was seen. In contrast, serum deprivation led to a reduction in Bcl-2 expression. The decrease in Bcl-2 mRNA expression was significantly more pronounced at all time points studied, when cells were exposed to 25 mM D-glucose as compared to 5 mM D-glucose. Consequently there was a significantly greater increase in the Bax:Bcl-2 mRNA ratio in the cells exposed to 25 mM D-glucose as compared to those exposed to 5 mM D-glucose (Figure 2b). In all experiments, the housekeeping gene β-actin was used to ensure equal loading of the gels. In parallel experiments, Western blot analysis confirmed that the changes in Bcl2/Bax mRNA reflected the level of endogenous protein (Figure 2c). Exposure of mesangial cells to serum-free conditions Bax protein levels did not change the level of Bax protein. In contrast and consistent with RT-PCR results, addition of serum-free medium resulted in reduced expression of Bcl2 protein levels which was more pronounced when cells were exposed to 25 mM D-glucose as compared to those exposed to 5 mM D-glucose.
Effect of glucose on Bax:Bcl2 expression. Mesangial cells were grown to confluence. Subsequently apoptosis was induced by serum-deprivation either in the presence of 5 mM D-glucose or 25 mM D-glucose. At the time points indicated total RNA was isolated and RT-PCR performed as described in Materials and methods. Ethidium bromide stained PCR products were separated on a 3% agarose gel (a). For Bcl2 (upper panel), Bax (middle panel) amplification was performed for 33 cycles. PCR amplification for β-actin (lower panel) was performed for 26 cycles. Scanning densitometry of three individual experiments was performed (b), and the results expressed as the mean±s.d. ratio of Bax:Bcl2 mRNA corrected at each time point for the house keeping gene β-actin. To confirm that alterations in Bcl2/Bax reflect the level of endogenous protein, in parallel experiments, cell lysates prepared from confluent mesangial cell exposed to serum deprivation in the presence of 5 mM D-glucose or 25 mM D-glucose at the time points indicated were subject to Western blot analysis for either Bcl2 or Bax protein (c).
Increased Apoptosis is Associated with Reduced Activation of NF-κB and Inhibition of NF-κB Mimics the Effects of Elevated Glucose on Apoptosis
There is strong evidence implicating a role for the transcription factor NF-κB as a cell survival factor.35 Furthermore diminished nuclear translocation of NF-κB has been associated with impaired mesangial cell survival.21 To determine whether NF-κB is involved in glucose-induced apoptosis, gel shift assays were performed with nuclear proteins and an NF-κB site-specific probe. Nuclear proteins from mesangial cells maintained under serum-free conditions exhibited decreased binding which was further suppressed by exposure to 25 mM D-glucose as compared to 5 mM D-glucose at all time points studied (Figure 3a). The cell permeable NF-κB inhibitor peptide SN50, which inhibits translocation of NF-κB to the nucleus was used to further investigate the role of NF-κB in glucose induced mesangial cell apoptosis. Inhibition of NF-κB nuclear translocation was confirmed by gel shift assay (Figure 3b). Furthermore, addition of SN50 (in serum free, 5 mM D-glucose medium) led to a time dependent increase in the Bax:Bcl-2 mRNA ratio which was greater than that seen following addition of serum-free medium alone. This was accompanied by a significant increase in mesangial cell apoptosis as assessed by flow cytometry using Annexin-V/PI as described above, compared to the addition of serum-free medium (% apoptotic cells control: 27.6±2.8 vs SN50: 40.66±7.0, mean±s.d., n=3, P=0.02).
Inhibition of NF-κB is associated with enhanced mesangial cell apoptosis. Confluent monolayers of mesangial cells were exposed to either serum-free medium in the presence of 5 mM D-glucose (SF 5 mM) or serum-free medium in the presence of 25 mM D-glucose (SF 25 mM) for up to 72 h. Subsequently nuclear proteins were prepared and gel shift assays were performed using an NF-κB site-specific probe (a). Specificity of binding EMSA was examined by preparation of nuclear proteins from mesangial cells exposed to either 5 or 25 mM D-glucose for 48 h. Subsequently gel shift assays were performed using either the NF-κB site-specific probe alone (lanes 1 and 2) or in the presence of excess unlabelled probe (lanes 3 and 4) (b). The role of NF-κB was further examined by the use of the cell permeable NF-κB inhibitor peptide SN50. Mesangial cells were incubated with increasing doses of SN50 in the absence of serum for 24 h. Inhibition of NF-κB nuclear translocation was confirmed by gel shift assay (c). In a parallel experiments mesangial cells were incubated with serum-free medium with a glucose concentration of 5 mM, in the presence of 10 μM SN50 for up to 72 h. Subsequently total RNA was isolated and RT-PCR performed as described in Materials and methods. Ethidium bromide stained PCR products were separated on a 3% agarose gel (d). For Bcl2 (upper panel), Bax (middle panel) amplification was performed for 33 cycles. PCR amplification for β-actin (lower panel) was performed for 26 cycles. Scanning densitometry of three individual experiments was performed (e), and the results expressed as the mean±s.d. ratio of Bax:Bcl2 mRNA corrected at each time point for the house keeping gene β-actin, *P<0.05 compared to corrected Bax:Bcl2 mRNA ratio at time zero.
Glucose-Enhanced Apoptosis is Mediated by TGF-β1
Next, we assessed whether recombinant TGF-β1 mimicked the effect of elevated D-glucose. Addition of recombinant TGF-β1, for 72 h, led to a significant increase in mesangial cell apoptosis compared to serum deprivation alone, as assessed by flow cytometry using Annexin-V/PI (Figure 4a). The role of TGF-β1 in glucose-enhanced mesangial cell apoptosis was further examined by blockade of TGF-β1 function. Addition of a blocking antibody to TGF-β1 significantly attenuated glucose induced apoptosis (Figure 4b). In contrast, addition of control antibody, did not affect glucose-induced mesangial cell apoptosis. The efficacy of the antibody was confirmed demonstration of a dose dependent inhibition of TGF-β1-induced mesangial cells apoptosis in the presence of the blocking antibody (Figure 4c).
TGF-β1 induces mesangial cell apoptosis and mediates glucose-enhanced apoptosis. (a) Confluent mesangial cell monolayers were incubated with either serum-free medium, or serum-free medium in the presence of increasing doses of recombinant TGF-β1 for 72 h. (b) In a parallel set of experiments the role of TGF-β1 in glucose-enhanced apoptosis was examined. Confluent monolayers of mesangial cells were incubated with either 5 mM D-glucose, 25 mM D-glucose, 25 mM D-glucose in the presence of 10 μg/ml of blocking antibody to TGF-β1, or 25 mM D-glucose in the presence of 10 μg/ml of goat anti mouse IgG for 72 h. (c) Efficacy of the blocking antibody was confirmed by incubation of mesangial cells with 5 mM D-glucose, 5 mM D-glucose together with 1 ng/ml of recombinant TGF-β1, or 25 mM D-glucose together with 1 ng/ml of recombinant TGF-β1 in the presence of an increasing concentration of blocking antibody to TGF-β1 as indicated. In each of the experiments, apoptotic cells were identified by flow cytometry using Annexin-V and propidium iodide cell surface staining results represent mean±s.d. of three individual experiments, *P<0.05 compared to the % apoptotic cells in the control.
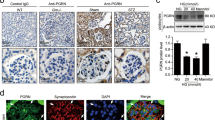
In parallel experiments, stimulation of mesangial cells under serum-free conditions with recombinant TGF-β1, led to a significant reduction in nuclear translocation of NF-κB (Figure 5a). This decrease in NF-κB nuclear translocation was associated with a reduction in the expression of Bcl-2 mRNA, with no alteration in Bax mRNA expression (Figure 5b), thus resulting in an increase in the ratio of Bax:Bcl-2 mRNA (Figure 5c). In addition, recombinant TGF-β1 stimulated an increase in caspase-3 expression and activation as assessed by Western blot analysis (Figure 5d). Inhibition of the translocation of NF-κB by the inhibitor peptide SN50, also led to induction and activation of caspase-3.
Inhibition of NF-κB activation and suppression of Bcl2 by TGF-β1. Confluent monolayers of mesangial cells were exposed to serum-free medium in the presence of 1 ng/ml recombinant TGF-β1 for up to 24 h. Subsequently nuclear proteins were prepared and gel shift assays were performed using an NF-κB site-specific probe (a). In a parallel experiment mesangial cells were incubated with serum-free medium with a glucose concentration of 5 mM either in the presence of 1 ng/ml of recombinant for up to 72 h prior to isolation of total RNA. RT-PCR performed as described in Materials and methods. Ethidium bromide-stained PCR products were separated on a 3% agarose gel (b). For Bcl2 (upper panel), Bax (middle panel) amplification was performed for 33 cycles. PCR amplification for β-actin (lower panel) was performed for 26 cycles. Scanning densitometry of three individual experiments was performed (c), and the results expressed as the mean±s.d. ratio of Bax:Bcl2 mRNA corrected at each time point for the house keeping gene β-actin, *P<0.05 compared to corrected Bax:Bcl2 mRNA ratio at time zero. In a further set of experiments confluent mesangial cells were exposed to serum-free medium containing 5 mM D-glucose (NG), 25 mM D-glucose (HG), recombinant TGF-β1 or the NF-κB inhibitor SN50 (10 μM) for 24 h prior to lysis of cells and Western blot analysis of caspase-3.
Previous studies have demonstrated that glucose-induced alterations in mesangial cell function may be mediated by the pro-fibrotic cytokine TGF-β1. We, therefore, sought to determine the role of glucose-induced TGF-β1 in induction of apoptosis and its relationship with suppressed NF-κB nuclear translocation. Under serum-free conditions, maintenance of mesangial cells under serum-free conditions in the presence of 25 mM D-glucose led to an increase in TGF-β1 as assessed by ELISA (Figure 6a). Confirmation of the active nature of TGF-β1 was sought by addition of conditioned medium from mesangial cells exposed to either 5 mM D-glucose or 25 mM D-glucose to HK2 cells transiently transfected with the Smad responsive promoter-luciferase construct. There was a significant increase in luciferase activity of the promoter construct following addition of 25 mM compared to 5 mM D-glucose-conditioned medium (Figure 6b). Following in vitro activation of latent TGF-β1 performed by repeated cycles of freeze thawing of the samples, a significant increase in Smad responsive promoter activity was seen following addition of 5 mM D-glucose-conditioned medium. In contrast, repeated cycles of freeze thawing of 25 mM D-glucose-conditioned medium did not increase luciferase activity compared to that seen following addition of untreated 25 mM D-glucose-conditioned medium. These data, therefore, confirm that following addition of 25 mM D-glucose the increase in TGF-β1 was of its active form.
Glucose increases total (a) and active (b) TGF-β1. Confluent mesangial cells were incubated under serum-free conditions with either 5 mM D-glucose (stippled bars) or 25 mM D-glucose (solid bars) for up to 72 h. At the time points indicated cell culture supernatant was collected and TGF-β1 quantified by ELISA. Results represent mean±s.d. of six individual experiments. To determine TGF-β1 bioactivity (b) conditioned medium (CM) collected from mesangial cells exposed to either 5 mM D-glucose (5 CM) or 25 mM D-glucose (25 CM) for 72 h was added to HK-2 cells transfected with a Smad responsive promoter-luciferase construct. In addition, to activate latent TGF-β1, conditioned medium from either 5 mM D-glucose (5 CM FT) or 25 mM D-glucose (25 CM FT) were subjected to 10 cycles of freeze thawing prior to addition to transfected cells. In control experiments, culture medium alone was added to the transfected cells (5 mM). Luciferase activity was quantified 24 h after the addition of conditioned medium. Results represent means±s.d. of three individual experiments.
The time course of TGF-β1 stimulation would suggest that this is unlikely to mediate glucose-dependent apoptosis, as significant increase was seen at a later time point than the observed effect on apoptosis. Recent studies, however, suggest that high-ambient glucose enhances sensitivity to TGF-β1.22 The effect of 25 mM D-glucose on TGF-β1 sensitivity was therefore examined by transfection of mesangial cells with a Smad responsive luciferase reporter construct, addition of either 5 or 25 mM D-glucose for 24 h and stimulation with recombinant TGF-β1 for a further 24 h. Under these conditions, luciferase activity was significantly greater in the cells exposed to 25 mM D-glucose than 5 mM D-glucose prior to addition of TGF-β1 (Figure 7).
Glucose increases mesangial cell sensitivity to recombinant TGF-β1. Mesangial cells were transfected with the Smad responsive luciferase reporter construct. Subsequently serum-free medium with a D-glucose concentration of either 5 or 25 mM was added for 24 h prior to stimulation with recombinant TGF-β1 for a further 24 h again under serum-free conditions prior to quantitation of luciferase activity. In control experiments, luciferase activity of transfected mesangial cells maintained under serum-free conditions in the absence of recombinant TGF-β1 was quantified. Results represent means±s.d. of three individual experiments.
Discussion
The late phase of diabetic nephropathy is characterised by loss of resident glomerular cells, a process which correlates with the decline in glomerular filtration rate.23 Mesangial cell death by apoptosis is known to be involved in the resolution of glomerular hyper-cellularity following injury suggesting that apoptosis may be a homeostatic mechanisms regulating the glomerular cell population.24 It is also clear that apoptosis may also play a pathologic role leading to deletion of mesangial cells associated with progressive glomerulosclerosis.25 Numerous studies have implicated hyperglycaemia as a regulator of apoptosis in numerous cell types. Hyperglycaemia mediates apoptotic myocyte death suggesting a role in diabetic myopathy.26 Similarly high glucose triggered apoptosis in cultured endothelial cells27 and also in neuro-epithelial cells,28 implicating glucose regulation of apoptotic cell fate in vascular disease and congenital malformations associated with diabetic pregnancy respectively. In contrast hyperglycaemia inhibits vascular smooth muscle cell apoptosis, thus demonstrating the cell-specific nature of glycaemic injury.29 In the current study, we have used numerous different methodological approaches to demonstrate that elevated glucose concentration increases the pro-apoptotic pathway activated by serum deprivation in renal mesangial cells. In addition, we have demonstrated enhanced activation of one of the key executioners of apoptosis, capsase-3 following exposure to glucose.
The data also demonstrate that maintenance of mesangial cells under conditions of elevated glucose leads to augmentation of NF-κB inhibition and that this is associated with an alteration in the ratio of Bax:Bcl-2 which favours increased apoptotic cell death. More specifically our data demonstrate a decrease in the expression of the cell survival factor Bcl-2 with no change in the expression of Bax, which facilitates apoptosis. The transcription factor NF-κB is a critical immediate early response gene involved in modulating cellular responses. NF-κB plays a complex role in apoptosis since it has been found to depend on the cell type. Some studies have implicated NF-κB in promoting apoptosis in certain cells.30, 36 Conversely several reports provide convincing evidence that NF-κB is involved in inhibition of apoptosis.37, 38, 39, 40 Recent studies have demonstrated that activating NF-κB prior to injury was anti-apoptotic only following stimuli dependent on tyrosine kinase activation of I-κB alpha, but not IKK-dependent serine phosphorylation of I-κB alpha. This suggests that cell fate may be both dependent on the cell type and the pathway mediating regulation of NF-κB.41 In this study, we have demonstrated that not only is glucose-enhanced apoptosis associated with reduced NF-κB activation, but that inhibition of NF-κB activation with a peptide which prevents NF-κB translocation mimics the effects of glucose in enhancing apoptosis and also downregulating Bcl-2 expression, thus providing convincing evidence that glucose-mediated inhibition of NF-κB activity is involved in determination of apoptotic cell fate. Our data is consistent with numerous studies which have demonstrated that NF-κB is a cell survival factor in mesangial cells.21, 42
Numerous studies have demonstrated that TGF-β1 mediates many of the effects of glucose on mesangial cell function. Elevated glucose leads to transcriptional activation of TGF-β1.43, 44 Furthermore, glucose-mediated alterations in mesangial cell function are mediated by autocrine activation of TGF-β1.45 Recent reports suggest that glucose also enhances sensitivity of mesangial cells to the effects of TGF-β,22 consistent with enhanced luciferase activity of the TGF-β1 responsive promoter when stimulated by TGF-β1 in the presence of elevated glucose concentration in our study. The demonstration that inhibition of TGF-β1 action using a blocking antibody abrogated 25 mM D-glucose-enhanced apoptosis, confirms the central role of TGF-β1 in this response. Although we have confirmed increased generation of bio-active TGF-β1 in mesangial cells exposed to an elevated concentration of D-glucose, the delayed time course for TGF-β1 generation relative to altered Bcl2/Bax ratio and NF-κB activation, suggests that stimulation of de novo synthesis is unlikely to be the sole mediator of apoptosis in these in vitro experiments. Enhanced sensitivity to TGF-β1 signaling is therefore likely to be an important mechanism contributing to the pro-apoptotic effect of glucose.
Although the data presented provides evidence for a mechanism by which glucose through enhanced sensitisation of TGF-β1 signalling increases mesangial cell apoptosis, it is likely that this is not the sole mechanism by which apoptosis may be stimulated in diabetic nephropathy. For example, glucose is known to modulate mesangial cell function by enhanced activity of aldose reductase, protein kinase C isoforms and the synthesis of advanced glycation end products.46, 47 Activation of these pathways, in turn, is known to be associated with glucose-mediated apoptosis related to the development of microvascular complication of diabetes.48, 49, 50, 51 Recent studies have demonstrated that the pro-apoptotic effects of these pathways may each be mediated by increased generation of superoxide, as normalising mitochondrial superoxide production prevents glucose induced activation of protein kinase C, sorbitol accumulation of formation of advanced glycation end products in cultured endothelial cells.52 This is also consistent with recent data suggesting that high glucose may promote mesangial cell apoptosis by oxidant-dependent mechanisms.53 Furthermore treatment with antioxidants reduce glomerular cell apoptosis in a model of diabetic nephropathy in vivo.51
In conclusion, we have demonstrated that glucose-enhanced mesangial cell apoptosis is mediated by autocrine TGF-β1 activity, which leads to inhibition of nuclear translocation of NF-κκB and suppression of Bcl2 expression. The data provide insight as to how alterations in glucose related to diabetes mellitus may influence mesangial cell number and contribute to glomerulosclerosis associated with diabetic nephropathy.
References
White KE, Bilous RW . Type 2 diabetic patients with nephropathy show structural-functional relationships that are similar to type 1 disease. J Am Soc Nephrol 2000;11:1667–1673.
Kreisberg JI, Venkatachalam M, Troyer D . Contractile properties of cultured glomerular mesangial cells. Am J Physiol 1985;249 (4 Part 2):F457–F463.
Dworkin LD, Ichikawa I, Brenner BM . Hormonal modulation of glomerular function. Am J Physiol 1983;244:F95–F104.
White KE, Bilous RW, Marshall SM, et al. Podocyte number in normotensive type 1 diabetic patients with albuminuria. Diabetes 2002;51:3083–3089.
Sharma K, Ziyadeh FN . Hyperglycaemia and diabetic kidney disease. Diabetes 1995;44:1139–1146.
Steffes MW, Osterby R, Chavers B, et al. Mesangial expansion as a central mechanism for loss of kidney function in diabetic patients. Diabetes 1989;38:1077–1081.
Pesce C, Menini S, Pricci F, et al. Glomerular cell replication and cell loss through apoptosis in experimental diabetes mellitus. Nephron 2002;90:484–488.
Mishra R, Emancipator SN, Kern T, et al. High glucose evokes an intrinsic proapoptotic signaling pathway in mesangial cells. Kidney Int 2005;67:82–93.
Chase HP, Jackson WE, Hoops SL, et al. Glucose control and the renal and retinal complications of insulin dependant diabetes. J Am Med Assoc 1989;261:1155–1160.
The Diabetes Control and Complications Research Group. Effect of intensive therapy on the development and progression of diabetic nephropathy in the Diabetes Control and Complications Trial. Kidney Int 1995;47:1703–1720.
The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long term complications in insulin dependant Diabetes Mellitus. N Engl J Med 1993;329:977–986.
The diabetes control and complications trial/epidemiology of diabetes intervention and complications research group. Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. N Engl J Med 2000;342:381–389.
UK Prospective Diabetes Study Group. Intensive blood glucose control with sulphonylurease or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes. Lancet 1998;352:837–853.
Wolf G, Sharma K, Chen Y, et al. High glucose-induced proliferation in mesangial cells is reversed by autocrine TGF-β. Kidney Int 1992;42:647–656.
Ayo SH, Radnik RA, Glass WF, et al. Increased extracellular matrix synthesis and mRNA in mesangial cells grown in high glucose medium. Am J Physiol 1991;260:F185–F191.
Fumo P, Kuncio G, Ziyadeh FN . PKC and high glucose stimulated collagen α1 (IV) transcriptional activity in a reporter mesangial cell line. Am J Physiol 1994;267:F632–F638.
Nahman NS, Leonharat KL, Cosio FG, et al. Effects of high glucose on cellular proliferation and fibronectin production by cultured human mesangial cells. Kidney Int 1992;41:396–402.
McLennan SV, Fisher EJ, Yue DK, et al. High glucose concentration causes a decrease in mesangium degradation. Diabetes 1994;43:1041–1046.
Laemmli UK . Cleavage of structural proteins during the assembly the head of bacteriophage T4. Nature 1970;227:680–685.
Phillips AO, Steadman R, Topley N, et al. Elevated D-glucose concentrations modulate TGF-β1 synthesis by human cultured renal proximal tubular cells: the permissive role of platelet derived growth factor. Am J Pathol 1995;147:362–374.
Kochlatyi S, Gibbons N, Mattana J . Extracellular matrix modulates survival, NF-kappaB translocation, and MAPK activity in mesangial cells. Exp Mol Pathol 2002;73:191–197.
Hayashida T, Schnaper HW . High ambient glucose enhances sensitivity to TGF-beta1 via extracellular signal—regulated kinase and protein kinase Cdelta activities in human mesangial cells. J Am Soc Nephrol 2004;15:2032–2041.
Osterby R, Schmitz A, Nyberg G, et al. Renal structural changes in insulin-dependent diabetic patients with albuminuria. Comparison of cases with onset of albuminuria after short or long duration. APMIS 1998;106:361–370.
Baker AJ, Mooney A, Hughes J, et al. Mesangial cell apoptosis: The major mechanism for resolution of glomerular hypercellularity in experimental mesangial proliferative nephritis. J Clin Invest 1994;94:2105–2116.
Sugiyama H, Kashihara N, Makino H, et al. Apoptosis in glomerular sclerosis. Kidney Int 1996;49:103–111.
Fiordaliso F, Leri A, Cesselli D, et al. Hyperglycemia activates p53 and p53-regulated genes leading to myocyte cell death. Diabetes 2001;50:2363–2375.
Du X, Stockklauser-Farber K, Rosen P . Generation of reactive oxygen intermediates, activation of NF-kB and induction of apoptosis in human endothelial cells by glucose. Free Rad Biol Med 1999;27:752–763.
Fine EL, Horal M, Chang TI, et al. Evidence that elevated glucose causes altered gene expression, apoptosis, and neural tube defects in a mouse model of diabetic pregnancy. Diabetes 1999;48:2454–2462.
Hall JL, Matter CM, Wang X, et al. Hyperglycemia inhibits vascular smooth muscle cell apoptosis through a protein kinase C-dependent pathway. Circ Res 2000;87:574–580.
Carter BD, Kaltschmidt C, Kaltschmidt B, et al. Selective activation of NF-kappa B by nerve growth factor through the neurotrophin receptor p75. Science 1996;272:542–545.
Fraser DJ, Brunskill NJ, Phillips AO . Long-term exposure of proximal tubular epithelial cells to glucose induces TGF-β1 synthesis via an autocrine PDGF loop. Am J Pathol 2003;163:2565–2574.
Piek E, Moustakas A, Kurisaki A, et al. TGF-(beta) type I receptor/ALK-5 and Smad proteins mediate epithelial to mesenchymal transdifferentiation in NMuMG breast epithelial cells. J Cell Sci 1999;112 (Part 24):4557–4568.
Brown PD, Wakefield L, Levinson AD, et al. Physiochemical activation of recombinant latent transforming growth factor β's 1, 2 and 3. Growth Factors 1990;3:35–43.
Yang B, Johnson TS, Thomas GL, et al. A shift in the Bax/Bcl-2 balance may activate caspase-3 and modulate apoptosis in experimental glomerulonephritis. Kidney Int 2002;62:1301–1313.
Barkett M, Gilmore TD . Control of apoptosis by Rel/NF-kappaB transcription factors. Oncogene 1999;18:6910–6924.
Grilli M, Pizzi M, Memo M, et al. Neuroprotection by aspirin and sodium salicylate through blockade of NF-kappaB activation. Science 1996;274:1383–1385.
Wu M, Lee H, Bellas RE, et al. Inhibition of NF-kappaB/Rel induces apoptosis of murine B cells. EMBO J 1996;15:4682–4690.
Van Antwerp DJ, Martin SJ, Kafri T, et al. Suppression of TNF-alpha-induced apoptosis by NF-kappaB. Science 1996;274:787–789.
Wang CY, Guttridge DC, Mayo MW, et al. NF-kappaB induces expression of the Bcl-2 homologue A1/Bfl-1 to preferentially suppress chemotherapy-induced apoptosis. Mol Cell Biol 1999;19:5923–5929.
Wang CY, Mayo MW, Korneluk RG, et al. NF-kappaB antiapoptosis: induction of TRAF1 and TRAF2 and c-IAP1 and c-IAP2 to suppress caspase-8 activation. Science 1998;281:1680–1683.
Fan C, Yang J, Engelhardt JF . Temporal pattern of NFkappaB activation influences apoptotic cell fate in a stimuli-dependent fashion. J Cell Sci 2002;115(Part 24):4843–4853.
Furusu A, Nakayama K, Xu Q, et al. Expression, regulation, and function of inhibitor of apoptosis family genes in rat mesangial cells. Kidney Int 2001;60:579–586.
Hoffman BB, Sharma K, Zhu Y, et al. Transcriptional activation of transforming growth factor-beta1 in mesangial cell culture by high glucose concentration. Kidney Int 1998;54:1107–1116.
Daniels MC, McClain DA, Crook ED . Transcriptional regulation of transforming growth factor beta1 by glucose: investigation into the role of the hexosamine biosynthesis pathway. Am J Med Sci 2000;319:138–142.
Ziyadeh FN, Sharma K, Ericksen M, et al. Stimulation of collagen gene expression and protein synthesis in murine mesangial cells by high glucose is mediated by autocrine activation of transforming growth factor beta. J Clin Invest 1994;93:536–542.
Henry DN, Busik JV, Brosius FC, et al. Glucose transporters control gene expression of aldose reductase, PKC and GLUT1 in mesangial cell in vitro. Am J Physiol 1999;277:F97–F104.
Silbiger S, Crowley S, Shan Z, et al. Nonenzymatic glycation of mesangial matrix and prolonged exposure of mesangial matrix to elvated glucose reduces collagen synthesis and proteoglycan charge. Kidney Int 1993;43:853–864.
Galvez AS, Ulloa JA, Chiong M, et al. Aldose reductase induced by hyperosmotic stress mediates cardiomyocyte apoptosis: differential effects of sorbitol and mannitol. J Biol Chem 2003;278:38484–38494.
Naruse K, Nakamura J, Hamada Y, et al. Aldose reductase inhibition prevents glucose-induced apoptosis in cultured bovine retinal microvascular pericytes. Exp Eye Res 2000;71:309–315.
Quagliaro L, Piconi L, Assaloni R, et al. Intermittent high glucose enhances apoptosis related to oxidative stress in human umbilical vein endothelial cells: the role of protein kinase C and NAD(P)H-oxidase activation. Diabetes 2003;52:2795–2804.
Odetti P, Pesce C, Traverso N, et al. Comparative trial of N-acetyl-cysteine, taurine, and oxerutin on skin and kidney damage in long-term experimental diabetes. Diabetes 2003;52:499–505.
Nishikawa T, Edelstein D, Du XL, et al. Normalizing mitochondrial superoxide production blocks three pathways of hyperglycaemic damage. Nature 2000;404:787–790.
Kang BPS, Frencher S, Reddy V, et al. High glucose promotes mesangial cell apoptosis by oxidant-dependent mechanism. Am J Physiol 2003;284:F455–F466.
Acknowledgements
AOP is supported by a senior Fellowship from GlaxoSmithKline. The work was presented in abstract form at the Annual meeting of the American Society of Nephrology 2004 St Louis. The Institute of Nephrology is supported by The Kidney Wales Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khera, T., Martin, J., Riley, S. et al. Glucose enhances mesangial cell apoptosis. Lab Invest 86, 566–577 (2006). https://doi.org/10.1038/labinvest.3700418
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.3700418
Keywords
This article is cited by
-
Trigonelline reverses high glucose-induced proliferation, fibrosis of mesangial cells via modulation of Wnt signaling pathway
Diabetology & Metabolic Syndrome (2022)
-
Involvement of Endoplasmic Reticulum Stress, Autophagy and Apoptosis in Advanced Glycation End Products-Induced Glomerular Mesangial Cell Injury
Scientific Reports (2016)
-
Type 2 diabetic patients and their offspring show altered parameters of iron status, oxidative stress and genes related to mitochondrial activity
BioMetals (2012)
-
Enhanced expression of naofen in kidney of streptozotocin-induced diabetic rats: possible correlation to apoptosis of tubular epithelial cells
Clinical and Experimental Nephrology (2010)
-
Effects of thiamine and benfotiamine on intracellular glucose metabolism and relevance in the prevention of diabetic complications
Acta Diabetologica (2008)