Abstract
Study design: A biomechanical unitary classification of spinal injuries is proposed.
Objective: To present an evaluation of spinal injuries based on the essential traumatic spinal mechanisms: axial deformation, torsion, translation and combined mechanisms in connection with the concept of the stabilizing axial spinal pillar.
Setting: Hospital ‘Sf. Treime’, Iasi, Romania.
Methods: The essential mechanisms of spinal injuries are considered: (1) axial deformation with (a) compression (centric or eccentric), most often eccentric, including compression in flexion or extension; (b) spinal elongation with distraction as centric elongation, but frequently axial eccentric elongation and a flexion or extension injury; (2) torsion or axial spinal rotation, (3) segmental translation, with a shearing version for the double translation and (4) combined mechanisms – the most frequent situation. Over 300 patients with spinal injuries were analysed and the spinal instability was determined using the criteria of clinical instability. The cases of spinal instability were studied in connection with the types of lesion of the central axial spinal pillar.
Results: All cases with lesions of the central axial spinal pillar had traumatic spinal instability. The spinal instability was absent in cases of isolated lesions of the anterior or posterior secondary pillar. The X-ray and spinal CT analysis of the traumatic spinal lesions showed the types of lesions and specified the mechanisms of spinal injuries. The combined mechanisms were responsible for the majority of the spinal injuries.
Conclusions: Spinal instability occurs because of the lesion of the central axial spinal pillar The types of lesions of the central spinal pillar and of the secondary spinal pillars are determined by the essential traumatic spinal mechanisms: axial deformation (with compression or elongation), axial rotation, translation and most frequently the above combined mechanisms.
Similar content being viewed by others
Introduction
The classifications of spinal injuries are related to those of spinal instability. After the introduction of the concept of spinal instability in the Watson-Jones1 classification of spinal fractures, 1931, Nicoll2 presented, in 1949 the acute and the secondary spinal instability and later numerous studies of spinal instability were completed.3,4
An interpretation of spinal instability based on the central axial spinal pillar pattern was recently proposed.5 The axial overlapping of the posterior third of the vertebral body continued by the pedicles and the articular processes, forms the central axial spinal pillar for stability and resistance.5 This model appears as a complete concept of Denis6,7 and Louis8 models: the posterior third of vertebral body and intervertebral disc as in Denis's concept joins with the two columns of articular facets as in Louis's concept (Figure 1). The vertebral segments situated in front of the central axial pillar form the anterior secondary pillar and the overlapping of the laminae, spinous processes, connecting ligaments, etc forms the posterior secondary pillar (Figures 2 and 3). The spinal instability appears because of the disruption of the biomechanical continuity of the central axial spinal pillar.5
The classical classifications of spinal injuries do not always incorporate the segmental biomechanical behaviour in the spinal function as a whole or in relation with the traumatic mechanisms.9,10,11,12,13 A classification of spinal injuries must be based on the essential traumatic spinal mechanisms in connection with the spinal instability determined by the lesions of the central axial spinal pillar.
This paper presents a unitary biomechanical classification of spinal fractures and a definition of spinal instability based on the concept of central vertebral pillar of stability and on the analysis of instability in over 300 spinal injuries.
Methods
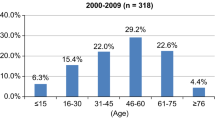
In all, 314 personal cases of spinal injuries were analysed for the present study. All cases of spinal injuries with isolated spinous process or transverse processes fractures were discarded.
Patient distribution was as follows:
-
125 cervical injuries,
-
163 thoracal injuries, and
-
26 lumbar injuries (Table 1)
Table 1 Cases of spinal injuries
The postinjury clinical condition was evaluated and a combination of X-ray and spinal CT established the diagnosis; as a result these investigations have showed the types of lesion of the central axial spinal pillar. The ASIA (modified by Frankel) scale9 was used for clinical evaluation, but the aim of this study was not primarily a clinical analysis.
In the cervical and thoracal spine, the spinal instability was analysed using the checklist for the diagnosis of clinical instability:14 anterior elements destroyed=2 point value, posterior elements destroyed=2 point value, kyphotic angulation >11°=2 point value, anteroposterior translation >3.5 mm=2 points value, spinal cord injury=2 points value, disc narrowing=1 point value, etc; the five radiographic signs that indicate an unstable situation for the thoracic and lumbar vertebral injuries according to Daffner15 were also used: displacements, widening of the interspinous space, of the facet joints or of the interpedicle distance or disruption of the posterior vertebral body line.
Spinal instability, which occurs in the moment of trauma is an instantaneous instability; spinal instability detected within 3 months (usually 3–8 weeks) is precocious instability and late spinal instability appears usually after 6 months.16
Essential mechanisms of spinal injuries
The mechanisms of spinal injury production are related to the possibility of the exaggerated motions to produce fractures of the vertebrae.17,18 The analysis of the spinal segmental movements and of the spinal combined movements, according to the Cartesian coordinate system for the human spine, shows that different possible spinal lesions occur because of an exaggerated movement in one of the directions: axial (along the spine), axial spinal rotation, transversal as a segmental translation or combined mechanisms.
Therefore, the classification used is:
-
1
Axial deformation with two possible variants:
-
a)
Compression, centric but most often eccentric owing to the physiological curvatures and especially because of the specific posture in the moment of impact. The eccentric compression injury causes a flexion on one side of the spine and extension on the other side, thus including the compression in flexion or extension.
-
b)
Spinal elongation, which occurs most often at the cervical spine level; the elongation can also be axial centric (distraction) or more frequently axial eccentric, thus resulting in a flexion–distraction injury or an extension-distraction injury of the spine
-
a)
-
2
Torsion or axial rotation.
-
3
Segmental translation (transversal or cross-translation), with a shearing version for the double or repeated translation (with a ‘to and fro’ motion).
-
4
Combined mechanisms: at the same time or in a very rapid sequence; this is the most frequent situation.
Schematic drawings of some types of spine injuries are given in Figures 4, 5 and 6. These 314 cases of spinal injuries were systemized based on the above classification (Table 219 ) and a correlation between the type of mechanism injury, the spinal instability and the lesion of the central axial spinal pillar was investigated.
Schematic drawings of some types of spine injuries: (a) axial deformation through eccentric compression resulting in a superior wedge fracture; (b) axial deformation with eccentric compression and vertebral body collapse; (a and b) situation with an unaffected central axial spinal pillar and without spinal instability; (c) axial deformation through centric compression and burst fracture with partial lesion of the central axial spinal pillar and latent spinal instability
Schematic drawings of some types of spine injuries: (a) axial deformation through eccentric compression resulting in a partial anterior inferior body fracture but integrity of the central axial spinal pillar; (b) a combined mechanism through eccentric compression, posterior translation and with lesion of the axial spinal pillar and spinal instability; (c) axial deformation with eccentric distraction and posterior translation, lesion of axial spinal pillar is evident and spinal instability exists
Schematic drawings of some types of spine injuries: (a) combined mechanisms through axial deformation with eccentric compression (eccentric distraction) and anterior translation resulting a dislocation and spinal instability; (b) axial deformation through eccentric distraction resulting an inferior wedge fracture and fracture of the pars interarticularis; (c) combined mechanisms through axial eccentric compression (lateral bending), lateral translation and possible axial rotation
Results
The analysis of these 314 cases of spinal injuries on the basis of the diagnosis criteria for spinal instability showed 186 cases of spinal instability:
-
87 cases of spinal instability in cervical injuries and
-
99 cases of spinal instability in thoracic and lumbar injuries.
The 186 cases of spinal instability represent 59.23% of the studied patients. The 186 cases of spinal instability and the correlation with the type of vertebral lesion are presented in Table 3. In these 186 cases, there were five or more points of instability. The remainder of 128 cases with injured spines were stable in that they had less than 5 points. Spinal instability has appeared most frequently immediately after injuries, depending on the violence of impact and on individual factors, in 77 cases with 5–7 points value of elements of instability, that is equivalent to 41% of all spinal instability cases and to 24.52% of all cases of spinal injuries (Table 3).
The analysis of the above cases according to the central pillar model has shown that all patients with biomechanical instability had lesions of the spinal central pillar. The lack of the spinal central pillar lesions was correlated with spinal stability. Samples of analysed cases of spinal injuries are given in Figures 7, 8, 9, 10, 11 and 12. In 39 cases, equivalent to 12.42% of all spinal injuries cases, there was an isolated lesion only of the secondary anterior pillar, the points value of instability was 3–4 (>5=clinical instability) and spinal instability did not occur (Figure 7). In 29 cases with lesions of the vertebral body, without posterior cortical layer, the spinal instability did not occur, but in five cases spinal instability occurred later, giving a ratio of 29/5 or 84.3% of stable cases in these types of injuries.
Thoraco-lumbar spine injury through vertical compression: (a) lateral radiograph, (b) drawing and (c) CT scan; lesions of the vertebral body as ‘burst fracture’ without posterior cortical layer injury; spinal instability did not occur because the continuity of the central axial pillar was been in 84.3% of these cases
Thoracic spine injury: (a) lateral radiograph, (b) schematic drawing and (c) spinal CT scan complete lesion of the vertebral body and of the pedicles and facets, that means a lesion of the central axial spinal pillar with injuries of the anterior pillar and determines instantaneous instability (in 46 cases=24.73% of cases of spinal instability)
Lateral radiograph of complexe spinal injury: anterior vertebral body compression (vertebral body destroyed), facet joint-capsules disruption, interspinous ligament failure and a great spinal luxation with spinal cord injury and discontinuity of the central axial spinal pillar and clear spinal instability
Spinal instability did not occur in 29 cases of lesions of the posterior secondary pillar only. Complete lesions of the vertebral body (including a lesion of the posterior ligament) or extended lesions of the central pillar have caused instantaneous instability with 5–6 points value of instability, in 31 cases, equivalent to 166% of all spinal instability cases and to 9.87% of all analysed cases of spinal injurires (Figures 9 and 10).
Spinal CT may or may not show retropulsed bone in the spinal canal in the case of patients with burst fractures. However, the treatment is dictated by the emergency of spinal cord compression (Figure 9) rather than on spinal instability.
A full lesion of the central axial spinal pillar with injuries of the anterior and posterior pillars through vertebral fracture or/with lesions of the connecting ligaments has determined instantaneous instability, with 5–7 points value of instability, in 46 cases, equivalent to 24.73% of the cases of spinal instability (Figures 10, 11 and 12).
When partial central spinal pillar lesion coexists with the lesions of the secondary posterior pillar the following have occurred:
-
the facets and pedicles bilateral lesions caused a precocious gradual instability in 14 cases and
-
the facets bilateral injuries produced a late gradual instability in 29 cases=15.59%.
Nevertheless, lesions of the bilateral facets with the lesions of the secondary posterior pillar did not induce spinal instability in 31 cases (2–3 points value of instability), equivalent to 16.66% of cases of spinal instability (similar to the 29 cases with late spinal instability, 5–6 points value of instability and with the same lesions!) (Tables 3 and 4).
Discussion
A classification of spinal injuries must identify common injury patterns, determine prognosis by the presence or the possibility of spinal instability and assist in the treatment.9
Analysis of normal spinal movements can indicate possible spinal injury patterns. The normal spinal motions have their directions on the axes of motions and the postures resulting through motion combinations can be analysed on an axis parallel to the spine and a transversal plane of a functional spinal unit (the vertical axis of the spine and the cross-planes of the spine).19,22
The translations along the vertical spinal axis are axial centric deformations, while flexions-extensions and lateral bendings are axial eccentric deformations of the spine. Other postures are also caused by axial spinal rotation (torsion), by the spinal translations and by all possible combinations of these mechanisms.
Spinal traumas cause direct osteoligamental injuries if the lesion focus is at the level of impact, or indirect ones when the traumatic impact, is away from the lesion focus.
The direct spinal injury can be regarded as an immense spinal strain for a segmental intervertebral movement or a colossal spinal stress of loading for a vertebral segment or a combination of the two.3,23 The indirect spinal injury is also a nonphysiological excessive spinal requirement (or spinal strain) of loading or of movement. The direct or indirect spinal injury induces an anomalous movement and in this way the vertebral resistance is exceeded and the spinal injury occurs.19,24,25,26
Therefore, the spinal injury occurs through a nonphysiological posture strain (or posture stress). These nonphysiological postures can result through exaggerated axial spinal deformations: centric compressions or centric distractions and eccentric compressions or eccentric elongations. Also, other pathological postures can result from exaggerated axial spinal rotations, abnormal spinal translations and all possible combinations of the above pathological mechanisms.19,27
These pathological postures are the result of direct or indirect spinal trauma interpreted as spinal strain by motion or spinal loading stress.
The spinal deformation is the repercussion of the spinal overtaxation (as a overphysiological spinal requirement) and this spinal deformation is higher than the normal resistance of spinal osteoarticular and ligamental elements. The consequence of the traumatic incident depends on the position of the spine at the time of injury.
The classification of spinal injuries used is primarly based on the biomechanical mechanisms of the spinal injuries and the categories are formed in concordance with the same mechanisms of lesions.9 This classification defines spinal injuries in groups based on the essential spinal injury mechanisms (Table 2); each spinal injury is shown by exhibiting the pathological morphology of spinal lesion and of the spinal level.
The mechanisms are: (1) axial deformation injuries with two categories: (a) compressive, centric or eccentric injuries (Figures 4a–c and 6a) and (b) spinal elongation, centric or distraction and eccentric elongation (Figure 6b); (2) axial rotation or torsion (about the vertical spinal axis), which can induce an injury through rotational translation on the cross-plane of the spine; and (3) segmental translation on the spinal cross-plane or on an oblique-plane, which causes transverse or oblique disruptions. The mechanism of shearing is a repeated segmental translation with ‘to and fro’ motion; this shearing can also occur in an oblique or a quasivertical plane, especially at the posterior vertebral arch. These mechanisms can be combined simultaneously or successively in a very quick sequence and the multiple combinations of the injury forces (compressive, distractive, rotational, shear forces, etc) can induce different stages of spinal injuries; these combined mechanisms are the fourth type in this classification (Figures 5b, c, and 6a, c).
As a rule, the indirect traumatic impact has produced vertebral injury by compression (in flexion or in extension) or by torsion and in the direct traumatic impact the injury occurred through translation (or shearing) or through combined mechanisms.
The axial central spinal pillar maintains the orthostatic posture and transmits elastically and plastically the spinal stress conditions and the secondary pillars take over the loading elastically (the anterior pillar) and limit the movements' amplitude (posterior pillar) in order to protect the axial pillar.5 The vertical division of the central spinal pillar decreases spinal rigidity and increases overall spinal flexibility while at the same time reducing the loading shock by gradually lessening the impact acceleration.
The spinal instability analysis based on the diagnosis criteria of clinical instability has shown that the lesions of the two anterior thirds of vertebral body, that is, equivalent to the anterior secondary pillar, did not determine spinal instability, in 39 cases; and also an absence of instability in 29 cases with the lesions of the vertebral body without the posterior cortical layer. But in five cases with the same lesions of the vertebral body without the posterior cortical layer, spinal instability which was absent at the beginning has occurred gradually as late instability; the points value of clinical instability were 5–6 four –six months later, and this late instability was determined by a secondary intervertebral disc norrowing with a late radiculopathy (Table 4).
The injuries of the laminae with or without the spinous processes, and/or of the posterior connecting ligaments did not determine spinal instability; therefore, the injury of the posterior secondary pillar did not induce spinal instability. The complete injuries of the vertebral body (including a lesion of the vertebral posterior ligament) or extended lesions of the vertebral body including pedicles and facets have caused instability in all cases: instantaneous instability in 31 cases and precocious instability in nine cases. Full lesion of the posterior third of the vertebral body with pedicles and facets with injuries of the anterior and posterior pillars determined instantaneous instability in 46 cases (Figures 9, 10, 11 and 12).
Lesions of facets and pedicles bilaterally caused a precocious gradual instability in 14 cases and the bilateral facet injuries produced a late gradual instability in 29 cases (Figures 8 and 10).
The lesions of the central axial spinal pillar have determined spinal instability in all cases.5,28
However, in 31 cases, bilateral lesions of the facets with the lesions of the secondary posterior pillar did not induce spinal instability as compared to 29 cases with the same lesions and with late spinal instability. This late instability was determined often by a late radiculopathy, by a late kyphotic angulation, by a widening of the interspinous space or of the interpedicle distance.
The injuries of the central spinal pillar have always been accompanied by a lesion of the secondary pillar, but the lesions of the secondary pillars could be isolated, partially or completely, according to the mechanisms of injuries.
Theoretically an isolated lesion of the central axial spinal pillar can be thought to be able to appear through possible mechanisms such as torsion with bilateral facets injury, bilateral traumatic isthmic injuries, bilateral fractures of the pedicles, etc; in this study the lesions of central axial spinal pillar were accompanied always by lesions of the secondary pillars. Injuries of the secondary pillars can be thought to not cause biomechanical instability; injuries of the posterior arch could produce spinal cord compression, although the spine could be stable.
The lesions of the secondary posterior pillar and partially of the central spinal pillar have caused: late gradual instability in the facets bilateral lesions, precocious gradual instability in the facets and pedicles bilateral lesions, and instantaneous instability in full lesions of the central axial spinal pillar.
The essential mechanisms of spinal injuries presented above are in concordance with the types of spinal lesions, and this spinal injuries classification included all the spinal injury cases which were studied.
The lack of spinal central pillar lesions was correlated with spinal stability and the lesions of the central axial spinal pillar have determined spinal instability in all cases, therefore the spinal instability can be considered to be determined by the central spinal pillar injury.5
The surgical approach in traumatic spinal instability must be reconsidered according to this biomechanical concept of the central axial spinal pillar of stability. Thus the fixations on anterior or posterior approach must stabilize the spine by stabilization of this central spinal pillar.
Conclusion
The first objective of a neurologic examination of the patient with spinal injury is to establish if spinal cord/roots injury exists and secondly if spinal injury is stable or unstable. Traumatic spinal instability is caused by the discontinuity of the central axial spinal pillar. It occurs when the lesion of the central spinal pillar exceeds a limit value in cross-section and height: full lesions of the central axial spinal pillar determine instantaneous instability, facets and pedicles bilateral lesions cause precocious gradual instability and the facets bilateral lesions induce late gradual instability.
The mechanisms of the central axial spinal pillar lesions are the essential traumatic spinal mechanisms.
The proposed classification of the spinal injuries is based on these abnormal forces acting on the central axial spinal pillar and determining exagerated movements:
-
1
Axial deformation with two variants:
-
a)
Compression: Centric or most often eccentric; the eccentric compression injury includes the compression in flexion or in extension.
-
b)
Spinal elongation: The centric (diastraction) or more frequently eccentric elongation causes flexion- or extension-distraction injuries.
-
a)
-
2
Torsion or axial rotation.
-
3
Segmental translation, with a shearing version for the repeated translation.
-
4
The three above mechanisms combined, simultaneous or successive.
Each spinal injury is shown by exhibiting the pathological morphology of spinal lesion and of the spinal level.
This classification of spinal injury is unitary and can be applied to the whole spine.
The injuries of the central spinal pillar have always been accompanied by a lesion of the secondary pillar. Injuries of the secondary pillars do not cause biomechanical instability; injuries of the posterior arch can produce spinal cord compression, although the spine can be stable.
The treatment in spinal injuries is made in connection with the spinal cord compression and the stabilization of the unstable spine must restore the continuity of the central axial spinal pillar.
References
Watson-Jones R . Fracture and Joint Injuries. 3rd edn. Williams & Wilkins: Baltimore 1943.
Nicoll EA . Fractures of the dorso-lumbar spine. J Bone Joint Surg Br 1949; 31376–31394.
Argeson C, Boileau P . Classification of thoracolumbar spine fractures. In: Floman Y, Farcy J-PC, Argeson C (eds). Thoracolumbar Spine fractures. Raven Press: New York, 1993.
Haher TR, Felmy WT, O'Brien M . Thoracic and lumbar fractures: diagnosis and management (chapter 36). In: Bridwell K, De Wald R (eds). Textbook of Spinal Surgery. JB Lippincott: Philadelphia, PA, 1991, pp 857–906.
Iencean SM . The stabilizing axial spinal pillar in the lumbar spine. Spinal Cord 2002; 40: 178–185.
Denis F . The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine 1983; 8: 817–831.
Denis F . Spinal instability as defined by the three-column spine concept in acute spinal trauma. Clin Orthop 1984; 189: 65–76.
Louis R . Spinal stability as defined by the three-column spine concept. Anat Clin 1985; 7: 33–42.
Anderson PA . Spinal cord injury and lower cervical spine injuries. In: An HS (ed). Principles and Techniques of Spine Surgery. Williams &Wilkins: Baltimore 1998, pp 295–330.
Levine AM, Edwards CC . Lumbar spine trauma In: Camins M, O'Leary P (eds). The Lumbar Spine. Raven Press; New York, 1987, pp 183–212.
Mager1 F, Aebi M . A comprehensive classification of thoracic and lumbar injuries. In: Aebi M, Thalgott JS, Webb JK (eds). AO ASIF Principles in Spine Surgery. Springer: Berlin 1998, pp 20–41.
Simpson JM, Sutton D, Rizzolo SJ, Cotler JM . Traumatic injuries to the adult lower cervical spine. In: Ann HS, Simpson JM (eds). Surgery of the Cervical Spine. Williams & Wilkins: Baltimore 1994, pp 267–293.
Ziegler R, Scheidt-Nave C, Leidig-Bruckner G . What is a vertebral fracture? Bone 1996; 18: 169–177.
White AA, Panjabi MM (eds). The problem of clinical instability in the human spine: a systematic approach. In" Clinical Biomechanics of the Spine. 2nd edn. JB Lippincott: Philadelphia 1990, pp 277–378.
Daffner RH . Thoracic and lumbar vertebral injuries. Semin Musculoskeletal Radiol 1998; 2: 45–63.
Iencean SM . Physiopathology (spinal instability). In: Iencean SM (ed). Lumbar Spondylolisthesis. Editura BIT: Iasi 1996, pp 33–37.
McCullen GM, Yuan HA, Fredrickson BE . Thoraco-lumbar spine injuries. In: An HS (ed). Principles and Techniques of Spine Surgery. Williams &Wilkins: Baltimore 1998, pp 359–384.
Lindsay KW, Bone I . Spinal trauma. In: Lindsay KW, Bone I (eds). Neurology and Neurosurgery Illustrated. 3rd edn. Churchill Livingstone: Edinburgh 1998, pp 401–404.
Iencean SM . New biomechanical classification of the spinal injuries. In: McCulloch G, Reilly P (eds). Proceedings 12th World Congress of Neurosurgery. Openbook Publishers: Adelaide, 2001, pp 269–272.
Effendi B et al. Fracture of the ring and axis. A classification based on the analysis of 131 cases. J Bone Joint Surg Br 1981; 63: 319–327.
Levine AM, Edwards CC . The management of the traumatic spondylolisthesis of the axis. J Bone Joint Surg Am 1985; 67: 217–226.
Hayes WC, Nachemson AL, White AA . Forces in the lumbar spine. In: Camins MA, O'Leary PF (eds). The Lumbar Spine. Raven Press: New York, 1987, pp 1–21.
Pope MH, DeVocht JW . The clinical relevance of biomechanics. Neurol Clin 1999; 17: 17–41.
Winkelstein BA, Myers BS . The biomechanics of cervical spine injury and implications for injury prevention. Med Sci Sports Exerc 1997; 29 (7 Suppl): 246–255.
Panjabi MM . Thoracolumbar burst fracture. A biomechanical investigation of its multidirectional flexibility. Spine 1994; 19: 578–585.
Yoganandan N, Pintar FA . Inertial loading of the human cervical spine. J Biomech Eng 1997; 119: 237–240.
Kaneoka K, Ono K, Inami S, Hayashi K . Motion analysis of cervical vertebrae during whiplash loading. Spine 1999; 24: 763–769.
Judet J et al. Tetraplegia caused by fracture-dislocations of the cervical spine treated by emergency reduction and osteosynthesis. J Chir (Paris) 1971; 101: 249–258.
Acknowledgements
I appreciate very much the critical comments of the peer-reviewers. I grateful acknowledge the help in English language of Dr LS Illis.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Iencean, S. Classification of spinal injuries based on the essential traumatic spinal mechanisms. Spinal Cord 41, 385–396 (2003). https://doi.org/10.1038/sj.sc.3101468
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101468