Abstract
Although the incidence of cervical spinal cord injury (CSCI) with ossification of the posterior longitudinal ligament (OPLL) has increased in older adults, its etiology and neurological outcomes remain unknown. We identified OPLL characteristics and determined whether they influence neurological severity and improvement of CSCI in older patients. This multicenter retrospective cohort study identified 1512 patients aged ≥ 65 years diagnosed with CSCI on admission during 2010–2020. We analyzed CSCI etiology in OPLL patients. We performed propensity score-adjusted analyses to compare neurological outcomes between patients with and without OPLL. Cases were matched based on variables influencing neurological prognosis. The primary neurological outcome was rated according to the American Spine Injury Association (ASIA) impairment scale (AIS) and ASIA motor score (AMS). In 332 OPLL patients, the male-to-female ratio was approximately 4:1. Half of all patients displayed low-energy trauma-induced injury and one-third had CSCI without a bony injury. Propensity score matching created 279 pairs. There was no significant difference in the AIS grade and AMS between patients with and without OPLL during hospitalization, 6 months, and 12 months following injury. OPLL patients tended to exhibit worse neurological findings during injury; nevertheless, OPLL was not associated with poor neurological improvement in older CSCI patients.
Similar content being viewed by others
Introduction
Cervical spinal cord injury (CSCI) in the older adults is expected to increase with an increase in the aging population1, and related falls among the older adults in recent decades, thus posing a serious public health concern2,3. CSCI in older adults is related to preexisting canal stenosis owing to the ossification of the posterior longitudinal ligament (OPLL)4. OPLL of the cervical spine is an inflammatory process that causes the replacement of the posterior longitudinal ligament by the lamellar bone, thereby resulting in spinal cord compression. Moreover, cervical OPLL develops in individuals in their 30 s and 40 s, and the progression halts in patients over 65 years5,6,7.
The presence of OPLL is a risk factor for CSCI. A recent nationwide cohort study investigating the impact of OPLL on the occurrence, severity, and prognosis of CSCI reported that OPLL is a risk factor for CSCI, and this risk is mitigated by surgical treatment8. Another study demonstrated that patients conservatively managed with OPLL displayed a 4.8-fold higher risk for CSCI than an age- and sex-matched population without OPLL9. Moreover, the influences of OPLL on CSCI are particularly strong for CSCI without bone injury4,10. CSCI without bone injury is increasing, a trend that may be related to OPLL and the aging population worldwide2,3. In individuals with cervical OPLL, the onset of CSCI is caused by trauma. In addition, it displays a poor prognosis11,12. Cervical myelopathy with OPLL leads to poorer postoperative outcomes and neurological improvement rates with cervical laminoplasty, compared with degenerative cervical myelopathy13. However, the epidemiology, severity, and prognosis of traumatic CSCI with OPLL in older adults are unknown.
We retrospectively evaluated a large number of older adults (aged ≥ 65 years) with CSCI and OPLL in the Japanese population. We aimed to identify the patient’s background characteristics and determine their impact on the severity of neurological deficits and their improvement in CSCI in older patients.
Methods
The Japan Association of Spine Surgeons with Ambition performed a multicenter retrospective cohort study on inpatients aged ≥ 65 with cervical spinal cord and spine injury at 33 medical centers between 2010 and 2020, with a minimum follow-up period of 3 months. The Institutional Review Board of the representative facility (No. 3352-1) and each center approved the study protocol. The current study is a report presentation collected from similar data as other studies14,15 and was conducted in compliance with the Declaration of Helsinki.
A total of 1512 patients with CSCI were included in this study. The variables included the age at injury, sex, height, weight, body mass index (BMI), pre-injury activities of daily living (ADL), the mechanism of injury, the number of diagnosed with OPLL before the injury, the number of vertebral levels of OPLL, the level of signal intensity change on magnetic resonance imaging (MRI), the presence of bone injury, the presence of diffuse idiopathic skeletal hyperostosis, American Spine Injury Association (ASIA) impairment scale (AIS) grade at the injury, complication injuries during injury, comorbidity before the injury, treatment, the period before surgery, surgical approach, and perioperative complications. OPLL was found in 332 of all patients. Moreover, the overall proportion of OPLL was 22.0% of the CSCI cases in older adults.
Analysis 1: OPLL vs. non-OPLL
We divided 1512 patients into two groups: those diagnosed with OPLL (OPLL group) and those without OPLL (non-OPLL group). The variables included the age at injury, sex, height, weight, BMI, smoking history, pre-injury ADL (independent walker or not), the presence of diabetes mellitus, dementia, cervical bone injury, signal intensity change on MRI, and surgical treatment. Injury mechanisms were classified as falling from the level ground (low energy) and more, such as high falls, traffic accidents, and others, including unspecified (high energy).
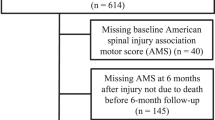
The moderator variables influencing the neurological prognosis (age, sex, BMI, pre-injury ADL, diabetes mellitus, dementia, bone injury, signal intensity change on MRI, and surgical treatment) were matched between the groups using propensity score matching (PSM). At baseline, 6 months, and 12 months of follow-up, the primary outcome measure comprised the ordinal change in the AIS grade and ASIA motor score (AMS). The time of admission was designated as baseline. We each assigned 5 points using 10 pairs of key muscles to evaluate the AMS. The scores ranged from 0 to 100. Higher scores in this range indicated stronger motor recovery. The secondary outcomes were morbidity and mortality from the baseline to 6 months and 12 months following injury.
Analysis 2: OPLL vs. non-OPLL in CSCI without bone injury
In patients with CSCI without bone injury, we compared the OPLL and non-OPLL groups. The moderator variables included age, sex, BMI, pre-injury ADL, diabetes mellitus, dementia, signal intensity change on MRI, and surgical treatment. Similar to Analysis 1, we compared the primary and secondary outcomes by adjusting the PSM.
Statistical analyses
Descriptive statistics for qualitative data are expressed as numbers and percentages, while quantitative data are expressed as the mean and standard deviation. We performed the Chi-square or Fisher’s exact tests and the t-test for the categorical and continuous variables, respectively. Following PSM, we conducted the McNemar test and paired t-test for the categorical and continuous variables, respectively.
Statistical test results were considered significant for p-values < 0.05, and all p-values were two-sided. All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria, http://www.R-project.org/, version 4.1.1)16. More precisely, it is a modified version of the R commander designed to add frequently used statistical functions in biostatistics.
Ethical approval
The institutional review board of representative facility reviewed and approved this study (Kanazawa University, No. 3352 1).
Informed consent
Informed consent was obtained from all participants in this study.
Results
In the patients with OPLL in CSCI, the mean age was 75.3 ± 6.7 years, and the male-to-female ratio was 268:64, with men accounting for 80.7% of the population. The mean height and weight were 161.8 ± 8.7 cm and 59.6 ± 10.9 kg, respectively. Before the injury, 88.0% of patients could walk independently, and approximately half of the injuries were caused by ground-level falls. Sixty-four percent of patients had CSCI without bone injury, and 31.6% developed diffuse idiopathic skeletal hyperostosis. The AIS grade at the time of injury ranged from A to C in 46.4% of patients. Comorbidities before injury included hypertension in 50.9% of patients and diabetes mellitus in 26.2% of patients. Surgical treatment was performed in 67.7% of patients, and the mean waiting period for surgery was 21.6 ± 46.1 days. The posterior surgical approach was adopted in 97.8% of cases (Table 1). Figure 1 depicts the sum of the levels with OPLL and signal intensity changes detected on MRI. Of the 175 patients for whom conservative treatment was selected as the initial treatment, 68 (38.9%) were eventually converted to surgery. As for reasons for conversion to surgery, 46 cases were because of worsening or persistent symptoms, 6 were because of complications that initially made surgery not an option, and 16 cases were unknown.
Table 2 summarizes surgery-related and in-hospital complications.
Analysis 1: OPLL vs. non-OPLL
There were 332 patients in the OPLL group and 1,180 in the non-OPLL group. Patients in the OPLL group displayed a higher men-to-women ratio (80.7% vs. 62.6%, p < 0.001), higher BMI (22.7 ± 3.9 vs. 21.7 ± 4.2, p < 0.001), higher rate of smoking history (39.8% vs. 27.1%, p = 0.001), higher prevalence of low energy trauma (50.2% vs. 35.2%, p < 0.001), higher prevalence of diabetes mellitus (26.7% vs. 21.0%, p = 0.035), a higher proportion of signal intensity change on MRI (78.1% vs. 57.9%, p < 0.001), and a higher proportion of surgical treatment (67.8% vs. 57.5%, p = 0.001) than the non-OPLL group (Table 3). The baseline AIS grade was not significantly different between the groups before matching (p = 0.630). In contrast, the baseline AMS in the OPLL group was significantly lower than in the non-OPLL group (55.6 ± 34.2 vs. 60.7 ± 32.7, p = 0.029). Patients in the OPLL group displayed a higher in-hospital complication rate than those in the non-OPLL group (38.0% vs. 30.6%, p = 0.013). There were no significant differences in the in-hospital mortality between the groups (5.8% vs. 3.9%, p = 0.170) (Table 4). Following PSM of the baseline characteristics, both groups had 279 patients. The AIS grade and AMS from baseline were not significantly different between each group. There were no significant differences in the in-hospital complication rate. However, the OPLL group displayed significantly higher in-hospital mortality than the non-OPLL group (5.4% vs. 1.4%, p = 0.010). Changes in the AIS grade and AMS from the baseline to 6 months and 12 months following injury were not significantly different between the groups. There was no significant difference in the comorbidity and mortality at 6 months and 12 months following injury (Table 4).
Analysis 2: OPLL vs. non-OPLL in CSCI without bone injury
There were 221 patients with CSCI without bone injury in the OPLL group and 403 in the non-OPLL group. Patients in the OPLL group demonstrated younger age (74.4 ± 6.6 vs. 75.9 ± 6.7, p = 0.008), higher men-to-women ratio (78.7% vs. 68.2%, p = 0.006), higher BMI (22.8 ± 4.2 vs. 22.0 ± 4.0, p = 0.020), higher rate of smoking history (39.8% vs. 27.1%, p = 0.001), and a higher proportion of surgical treatment (61.6% vs. 44.2%, p < 0.001) than those in the non-OPLL group14 (Table5). Patients in the OPLL group displayed a lower baseline AIS grade (p = 0.032) and baseline AMS (58.2 ± 32.8 vs. 65.2 ± 29.2, p = 0.009) than those in the non-OPLL group before matching15. There were no significant differences in the in-hospital complications and mortality between the groups (28.0% vs. 22.9%, p = 0.166; 2.4% vs. 2.0%, p = 0.770) (Table 6). Following PSM of the baseline characteristics, both groups had 176 patients. The AIS grade from baseline was significantly lower in the OPLL group than in the non-OPLL group (p = 0.045). Changes in the AIS grade and AMS from the baseline to 6 months and 12 months post-injury were not significantly different between the groups. There were only significant differences in the comorbidity at 12 months following injury (8.2% vs. 1.0%, p = 0.016) (Table 6).
Discussion
This large multicenter study investigated the epidemiology of CSCI with OPLL in older adults. Our results showed that CSCI occurred in concomitance with OPLL in 22.0% of the older population. The male-to-female ratio in the OPLL group was approximately 4:1. Half of all patients experienced low-energy trauma-induced injury, and one-third had CSCI without bony injury. A total of 279 pairs were created using PSM. There was no significant difference in the AIS grade and AMS between patients with and without OPLL during hospitalization, and 6 and 12 months after injury. Our findings suggested that patients with CSCI with OPLL can be expected to improve in a manner similar to that in patients without OPLL.
The prevalence of OPLL within a Japanese older patient population with CSCI was 22.0% and that of CSCI without bone injury in older adults was 34.4%. Kawano et al.17 reported that 22.2% of patients with traumatic CSCI had OPLL, and Boody et al.18 reported that approximately 30% of the patients with CSCI had OPLL. Endo et al.19 identified OPLL in 6.5% of the patients with CSCI. In contrast, Okada et al.20 reported OPLL in 10.1% of the patients with CSCI. Chikuda et al.4 reported that 34% of those with CSCI without bone injury had OPLL, compared with 38% of patients identified by Koyanagi et al.21. Approximately 26–38% of CSCI cases without bone injury are associated with OPLL22,23. Our results are similar to previous reports.
Regarding sex differences in OPLL, the men-to-women ratio was 80.7% in the older adults with CSCI and OPLL. Ohtsuka et al.24 reported that the prevalence of OPLL was 4.3% and 2.4% in men and women, respectively, in an X-ray survey of healthy Japanese. Previous observational studies demonstrated that the prevalence of OPLL in the general population is approximately two-fold higher in men than in women25,26. A nationwide survey in Japan showed that the men-to-women ratio was 3:1 in those with traumatic CSCI2. Our study displayed a high proportion of men, nearly four times that of women, considering the prevalence of OPLL in the general population. In older adults with OPLL, we observed a higher proportion of men with CSCI.
The OPLL group tended to display severe paralysis during the injury. After adjusting for the background variables affecting the neurological findings during injury, there were no significant differences in the AIS grade and AMS between the OPLL and non-OPLL groups, except for the AIS grade in patients with CSCI without bone injury. There was no significant difference in the rate of improvement in the neurological findings between patients with and without OPLL in either the AIS grade or AMS. Few reports have compared the rate of improvement of the neurological findings in patients with and without OPLL. These results indicated that the presence of OPLL exacerbates the neurological symptoms at the time of injury, but it had less impact on the recovery process of the neurological symptoms.
In this study, the in-hospital complication rate was 9.6% and 7.2% in the OPLL and non-OPLL groups, respectively, which was not significantly different and lower than in previous reports. However, patients with CSCI are frail and have a significant risk of complications. In previous reports, the in-hospital complication rate for spine surgery in older adults was approximately 20%, with hemorrhage, delirium, and UTI as the most common complications27,28. Bernstein et al.29 reported that the number of surgical cases of OPLL has increased significantly and provided national estimates for 21% of inpatient postoperative complications. For patients requiring surgical treatment for degenerative cervical myelopathy, OPLL can present a significant surgical challenge, with complication rates ranging from 5.2 to 57.6%30. Moreover, in a prospective, multicenter study, OPLL was an independent risk factor for perioperative complications in patients surgically treated for cervical myelopathy31. One factor contributing to the low complication rate in this study was that morbidity in retrospective studies is not calculated as accurately as in prospective studies and may be underestimated32. The comorbidity rate at 6 months and 12 months following injury was higher in the OPLL group with CSCI without bone injury, even after adjusting for the PSM using background variables. There was no significant difference in mortality between the groups. Similar to previous reports, we observed a trend towards a higher complication rate in patients with OPLL, and the OPLL group demonstrated a tendency to have greater complications.
This study has several limitations. First, it was not excluded from sampling bias because it cannot be extracted from medical records. Second, we did not evaluate the ossification type. There was no information available about the length and thickness of OPLL, which might be correlated with CSCI. We did not comprehensively investigate the relationship between the diameter of the spinal canal, the degree of cord compression, and the risk of myelopathy. Therefore, this necessitated further research on the morphology of OPLL. Third, the treatment contents and policies are not standardized among facilities, a limitation in a retrospective multicenter study; thus, prospective studies are desirable in the future. Fourth, the 12-month follow-up after PSM may have insufficient power to compare the mortality and morbidity in a reduced sample size. However, this novel study analyzed a large amount of sample data comparison among patients with or without OPLL. Prospective studies are preferred for an accurate assessment of morbidity and mortality.
Conclusions
The prevalence of OPLL in CSCI was 22.0% in older adults. Patients with OPLL had a higher proportion of men, higher BMI, higher smoking history rate, greater injuries owing to low energy as falling from the level ground, higher prevalence of diabetes mellitus, a higher proportion of signal intensity changes on MRI, and a higher proportion of surgical treatment.
In this study, patients with OPLL tended to display worse neurological findings during the injury; nonetheless, OPLL was not associated with poorer neurological improvement after CSCI.
Data availability
The study data and materials’ details may be made available upon reasonable request by e-mail the corresponding author.
References
Christensen, K., Doblhammer, G., Rau, R. & Vaupel, J. W. Ageing populations: The challenges ahead. Lancet 374, 1196–1208 (2009).
Miyakoshi, N. et al. A nationwide survey on the incidence and characteristics of traumatic spinal cord injury in Japan in 2018. Spinal Cord. 59, 626–634 (2021).
Jain, N. B. et al. Traumatic spinal cord injury in the United States, 1993–2012. JAMA 313, 2236–2243 (2015).
Chikuda, H. et al. Acute cervical spinal cord injury complicated by preexisting ossification of the posterior longitudinal ligament: A multicenter study. Spine 36, 1453–1458 (2011).
Sohn, S., Chung, C. K., Yun, T. J. & Sohn, C. H. Epidemiological survey of ossification of the posterior longitudinal ligament in an adult Korean population: Three-dimensional computed tomographic observation of 3,240 cases. Calcif. Tissue Int. 94, 613–620 (2014).
Tsuyama, N. Ossification of the posterior longitudinal ligament of the spine. Clin. Orthop. Relat. Res. 184, 71–84 (1984).
Hori, T., Kawaguchi, Y. & Kimura, T. How does the ossification area of the posterior longitudinal ligament thicken following cervical laminoplasty?. Spine 32, E551–E556 (2007).
Chen, L. F. et al. Risk of spinal cord injury in patients with cervical spondylotic myelopathy and ossification of posterior longitudinal ligament: A national cohort study. Neurosurg. Focus. 40, E4 (2016).
Wu, J. C. et al. Conservatively treated ossification of the posterior longitudinal ligament increases the risk of spinal cord injury: A nationwide cohort study. J. Neurotrauma. 29, 462–468 (2012).
Kato, H. et al. Cervical spinal cord injury without bony injury: A multicenter retrospective study of emergency and critical care centers in Japan. J. Trauma. 65, 373–379 (2008).
Jung, J. M., Chung, C. K., Kim, C. H. & Choi, Y. Risk factors and prognosis for acute progression of myelopathic symptoms in patients ossification of the posterior longitudinal ligament after minor trauma. Spine 43, E171–E176 (2018).
Matsunaga, S. et al. Trauma-induced myelopathy in patients with ossification of the posterior longitudinal ligament. J. Neurosurg. 97(Supplement), 172–175 (2002).
Takeuchi, K., Yokoyama, T., Wada, K. I. & Kudo, H. Relationship between enlargement of the cross-sectional area of the dural sac and neurological improvements after cervical laminoplasty: Differences between cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament. Spine Surg. Relat. Res. 3, 27–36 (2019).
Nori, S. et al. Does surgery improve neurological outcomes in older individuals with cervical spinal cord injury without bone injury? A multicenter study. Spinal Cord. 60, 895–905 (2022).
Nakajima, H. et al. JASA study group. Prognostic factors for cervical spinal cord injury without major bone injury in elderly patients. J. Neurotrauma. 39, 658–666 (2022).
Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 48, 452–458 (2013).
Kawano, O. et al. Influence of spinal cord compression and traumatic force on the severity of cervical spinal cord injury associated with ossification of the posterior longitudinal ligament. Spine 39, 1108–1112 (2014).
Boody, B. S., Lendner, M. & Vaccaro, A. R. Ossification of the posterior longitudinal ligament in the cervical spine: A review. Int. Orthop. 43, 797–805 (2019).
Endo, S. et al. Cervical spinal cord injury associated with ossification of the posterior longitudinal ligament. Arch. Orthop. Trauma. Surg. 113, 218–221 (1994).
Okada, S. et al. Does ossification of the posterior longitudinal ligament affect the neurological outcome after traumatic cervical cord injury?. Spine 34, 1148–1152 (2009).
Koyanagi, I. et al. Acute cervical cord injury without fracture or dislocation of the spinal column. J. Neurosurg. 93(Supplement), 15–20 (2000).
Epstein, N. Ossification of the cervical posterior longitudinal ligament: A review. Neurosurg. Focus. 13, ECP1 (2002).
Epstein, N. E. Laminectomy for cervical myelopathy. Spinal Cord. 41, 317–327 (2003).
Ohtsuka, K. et al. A radiological population study on the ossification of the posterior longitudinal ligament in the spine. Arch. Orthop. Trauma. Surg. 1978(106), 89–93 (1987).
Fujimori, T. et al. Prevalence, concomitance, and distribution of ossification of the spinal ligaments: Results of whole spine CT scans in 1500 Japanese patients. Spine 41, 1668–1676 (2016).
Maeda, S. et al. Gender-specific haplotype association of collagen alpha2 (XI) gene in ossification of the posterior longitudinal ligament of the spine. J. Hum. Genet. 46, 1–4 (2001).
Li, H. & Dai, L. Y. A systematic review of complications in cervical spine surgery for ossification of the posterior longitudinal ligament. Spine J. 11, 1049–1057 (2011).
Lee, N. J. et al. What is the impact of surgical approach in the treatment of degenerative cervical myelopathy in patients with OPLL? A propensity-score matched, multicenter analysis on inpatient and post-discharge 90-day outcomes. Glob. Spine J. https://doi.org/10.1177/2192568221994797 (2021).
Bernstein, D. N. et al. National trends and complications in the surgical management of ossification of the posterior longitudinal ligament (OPLL). Spine 44, 1550–1557 (2019).
Nakashima, H. et al. Comparison of outcomes of surgical treatment for ossification of the posterior longitudinal ligament Versus other forms of degenerative cervical myelopathy: Results from the prospective, multicenter AOSpine CSM-international study of 479 patients. J. Bone Joint Surg. Am. 98, 370–378 (2016).
Tetreault, L. et al. Clinical and surgical predictors of complications following surgery for the treatment of cervical spondylotic myelopathy: Results from the multicenter, prospective AOSpine international study of 479 patients. Neurosurgery 79, 33–44 (2016).
Nasser, R. et al. Complications in spine surgery. J. Neurosurg. Spine. 13, 144–157 (2010).
Acknowledgements
The authors acknowledge the contributions of the members of the 33 participating institutions in the assistance with data collection.
Author information
Authors and Affiliations
Contributions
S.O. and T.F. were responsible for the conception and design of the study. S.O., T.F., M.K., K.A., G.I., T.K., S.K., T.F., and K.W. performed data cleaning, statistical analysis and interpretation of results. All the authors have reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Okuwaki, S., Funayama, T., Koda, M. et al. Characteristics of the cervical spine and cervical cord injuries in older adults with cervical ossification of the posterior longitudinal ligament. Sci Rep 13, 2689 (2023). https://doi.org/10.1038/s41598-023-29877-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-29877-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.