Abstract
Study design
Retrospective descriptive study.
Objectives
To summarize epidemiologic data on nontraumatic spinal cord injury (NTSCI) for the last 30 years and compare these findings to data from individuals with traumatic spinal cord injury (TSCI).
Setting
National Rehabilitation Center affiliated with the Ministry of Health and Welfare in Korea.
Methods
The medical records of 948 individuals with NTSCIs were retrospectively reviewed. Three groups were created based on onset period (1990–1999, 2000–2009, 2010–2019) and six groups based on age (≤15, 16–30, 31–45, 46–60, 61–75, and ≥76 years). Pearson’s chi-square and analysis of variance tests were used for statistical analysis.
Results
The male-to-female ratio was 1.30:1 for NTSCI individuals and 3.47:1 for TSCI individuals. The mean age (standard deviation [SD]) at the time of injury increased from 38.7 (SD = 18.1) years in the 1990s to 55.5 (SD = 16.6) years in the 2010s (F = 44.597, p ≤ 0.001). Vertebral column degenerative disorder was the primary cause of injury in 28.9% of the cases, and the most common neurologic level was T12-L2. Paraplegia occurred in 74.6% of cases, and tetraplegia in 25.4% of cases. The proportion of NTSCI individuals increased from 11.2% to 29.3% during the observation period.
Conclusions
The proportion of NTSCI among total spinal cord injuries has increased in Korea over the last 30 years (1990–2019). Compared to individuals with TSCI, those with NTSCI had a higher age at onset, with different male-to-female ratios. Our study is the most comprehensive investigation of NTSCI in Korea, and our findings can inform research directions and medical guidelines.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is one of the most devastating types of injury and can lead to various dysfunctions. Accurate epidemiologic data are needed to understand SCI risk factors and their etiology. In the United States, the National Spinal Injury Statistical Center (NSCISC) database and the Shriners Hospital Spinal Cord Injury database were created in the early 1970s and in 1987, respectively, for systematic collection of data on individuals with SCI. The annual incidence of SCI in the general population is approximately 54 cases per million people. Based on the United States population statistics from 2020, an estimated 17,810 new individuals experience traumatic SCI (TSCI) each year [1].
Nontraumatic SCI (NTSCI) is any spinal cord damage arising from causes other than major trauma. The reasons may include inflammatory and autoimmune disease, neoplastic disorder, infection, vertebral column degenerative disease, vascular disease, etc. The epidemiological data on individuals with NTSCI is scarce, and data collection is not generally systematic. Moreover, the quality of epidemiological data on NTSCI is extremely poor compared to data for TSCI. In Australia, representative international studies, including research by New et al. [2], have reported an average age-adjusted incidence rate of 26.3 cases per million per year of NTSCI among adults. Other studies conducted in the United States, Australia, France, Spain, the Netherlands, Denmark, and Fiji have reported NTSCI incidence rates ranging from 5.1 to 80 cases per million per year [3,4,5,6,7,8,9,10].
It is well documented that damage to the spinal cord can arise from sources other than trauma [11, 12], and it is anticipated that the incidence of NTSCI will increase substantially with aging [2]. This trend is likely to increase the importance of NTSCI in terms of medical and research prioritization. Therefore, studies involving systematic and in-depth analysis of the epidemiological data of NTSCI individuals are necessary to advance the knowledge in this area.
SCI epidemiological studies have been conducted in Korea in the past, including those by Yang et al. [13], Shin et al. [14]., and Han et al. [15]. Although there have been studies in South Korea focusing specifically on TSCI, no prior research has focused on NTSCI in the South Korean population. This study summarized the epidemiologic data from NTSCI individuals for the last 30 years in South Korea to analyze epidemiologic changes over time and compared the findings with those of individuals with TSCI.
Methods
The Ethics Committee of the Institutional Review Board of the National Rehabilitation Center in South Korea approved this study (approval number: NRC-2019-04-025) and waived the requirement for informed consent because of the retrospective design of this research.
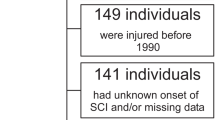
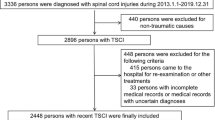
Of the 4951 SCI individuals initially collected, those who were re-admitted (318 individuals), injured before 1990 (149 individuals), or had an unknown onset or missing data (141 individuals) were excluded. After exclusion, this study was conducted on 948 individuals with NTSCIs from a total of 4343 individuals with SCIs who were admitted to a single rehabilitation center between 1990 and 2019. This study includes data on participant sex as well as hospital admission, age of injury onset, cause of injury (i.e., injury etiology), American Spinal Injury Association (AIS) impairment scale data, individuals’ neurological level of injury, and neurological data on individuals’ degree of impairment. Individuals’ neurological level of injury, as well as the degree of impairment after the injury, were assessed by a physician. In most cases, the examination was performed during the first week after admission.
Data were divided into three groups based on 10-year intervals according to the year of onset (1990–1999, 2000–2009, and 2010–2019), with a total enrollment of 87 individuals in 1990–1999, 318 individuals in 2000–2009, and 543 individuals in 2010–2019.
The classification of NTSCI has not been standardized until recently when the International Spinal Cord Society and American Spinal Injury Association approved the International NonTraumatic Spinal Cord Injury Datasets [16]. In this study, the etiology of NTSCI was classified into six categories according to the information presented within international SCI datasets for NTSCI: neoplastic disorder, inflammatory and autoimmune disease, infection, vertebral column degenerative disorder, vascular disorder, and others. The “others” category in this study includes syringomyelia, meningomyelocele, Neuro-Behçet’s disease, and radiation-related myelopathy. According to NTSCI datasets, vertebral column degenerative disorders include disc prolapse, ligamentum flavum hypertrophy, ossification of the posterior longitudinal ligament, spinal osteophytosis, spondylolisthesis, spondylosis, spinal stenosis, and spinal cord compression due to a combination of multiple developmental and/or acquired factors. For individuals with these types of vertebral column degenerative disorders, if the individual suffered a traumatic event, the individual was classified as having TSCI and was excluded from this study.
Iatrogenic injury was classified as TSCI because the International Classification of External Causes of Injury indicates that iatrogenic injury is considered traumatic. This category includes complications of healthcare, including medical or surgical care, unintentionally leading to injury or harm as well as acts of omission and commission [16].
Only one etiology was coded for each case. If individuals presented with an NTSCI lesion that occurred as a result of different causes, they were placed in a class based on the condition that caused the most severe neurological impairment. In contrast, if an individual presented with a single cause of NTSCI that could possibly be placed in two or more different etiological groups within the classification, a specific appropriate etiology was selected for the classification [16].
All statistical analyses were performed using IBM SPSS Statistics for Windows, ver. 26 (IBM Corp., Armonk, NY, USA). Categorical data were compared using Pearson’s chi-square test, and the mean age was compared using the analysis of variance. For all tests, statistical significance was defined as p < 0.05, and all effect estimates were presented with 95% confidence intervals.
Results
Sex and age
We present an overview of the demographic and clinical characteristics of the 948 enrolled NTSCI individuals in Table 1. In total, 536 (56.5%) participants were male, and 412 (43.5%) were female, with a male-to-female ratio of approximately 1.30:1. The male-to-female ratio was 1.29:1 for 1990–1999, 1.47:1 for 2000–2009, and 1.22:1 for 2010–2019. There was no statistically significant correlation between injury onset and sex (χ2 = 1.694, p > 0.05). The mean age at the time of SCI onset was 38.7 years (SD = 18.1) in 1990–1999, 47.6 years (SD = 18.8) in 2000–2009, and 55.5 years (SD = 16.6) in 2010–2019, indicating an increasing trend for SCI with increasing mean age (F = 44.597, p < 0.001). In addition, we observed statistically significant differences between all groups in the post-hoc test. From the 1990s to the 2010s, the number of individuals aged ≤15, 16–30, and 31–45 decreased gradually, while the number of individuals aged 46–60, 61–75, and ≥76 increased gradually. The changes of age distribution among NTSCI individuals over the three decades are shown in Fig. 1.
Etiology
Of all the SCI cases, 28.9% were due to vertebral column degenerative disorder, 19.9% due to inflammatory and autoimmune diseases, 18.5% were caused by neoplastic disorders, 15.5% were caused by vascular disorders, and 13.6% were caused by infection. The change of etiology distribution among NTSCI individuals over the three decades are shown in Fig. 2. In 1990–1999, inflammatory and autoimmune diseases were the most common causes of injury. In contrast, vertebral column degenerative disorder was the most common cause of injury in 2000–2009 and 2010–2019 (Fig. 2). The proportion of neoplastic disorders, inflammatory and autoimmune diseases, and infections gradually decreased over the course of the study, whereas the proportion of vertebral column degenerative disorders and vascular disorders showed a gradual increase (Fig. 2). Table 2 outlines etiologic differences in NTSCI individuals according to age. Inflammatory and autoimmune diseases were identified as the primary cause of injury in individuals aged ≤15 years (35.1%) and 31–45 years (27.2%). The neoplastic disorder was identified as the primary cause of injury in individuals aged 16–30 years (27.1%). In contrast, the degenerative disorder was identified as the cause of injury in individuals aged 46–60 years (25.8%), 61–75 years (39.5%), and ≥76 years (61.8%). Nontraumatic etiology showed statistically significant differences between the onset groups (χ2 = 40.850, p < 0.001). Several causes fell under the category of “Others”: four individuals had myelomeningocele in 1990–1999, ten individuals had syringomyelia (four in 1990–1999, five in 2000–2009, and one in 2010–2019), one individual had radiation myelitis in 2000–2009, and one individual suffered SCI from rheumatic arthritis (a rheumatic disease) in 2010–2019.
The top figure shows the etiology distribution of NTSCI individuals from 1990–1999. The middle figure corresponds to 2000–2009 data and the bottom figure corresponds to 2010–2019 data, respectively. Because five of the etiology presented in the text except for ‘others’, the total percentages of the five etiology groups are not 100%.
Neurologic level of injury and degree of impairment
During the entire study period, 74.6% of individuals presented with paraplegia—a higher proportion than those with tetraplegia. In the 2010s, individuals with paraplegia decreased from 81.6% to 73.3% compared with the 1990s, and tetraplegia cases increased from 18.4% to 26.7%. We did not observe differences between the onset groups for the level of injury (χ2 = 2.751, p > 0.05).
We observed the following neurologic levels that occur most commonly in NTSCI: L2 (11.0%), T12 (9.9%), L1 (8.9%), C4 (7.9%), and T9 (7.6%). The distribution of NTSCI individuals with tetraplegia and paraplegia was 25.4% and 74.6%, respectively (Table 1). For individuals with tetraplegia and paraplegia, the proportion of AIS-A lesions decreased, and the proportion of AIS-D lesions increased. According to the onset group, the difference in severity of the injury was statistically significant (χ2 = 39.956, p < 0.001).
Comparison of traumatic and NTSCI
The overall comparison between data for NTSCI and TSCI individuals is presented in Table 3. During the last 30 years, the proportion of NTSCI individuals increased from 11.2% to 29.3%, and the proportion of individuals with TSCI decreased from 88.8% to 70.7%. There was a statistically significant correlation between the onset group and the cause of injury (χ2 = 121.694, p < 0.001). The male-to-female ratio was 1.30:1 in NTSCI individuals, which was lower than the male-to-female ratio of 3.47:1 in TSCI individuals observed during the same period. As for the age of onset, the age of NTSCI onset increased from 38.7 years in 1990–1999 to 55.5 years in 2010–2019. During the same period, the age of TSCI onset at this center showed a gradually increasing trend from 32.6 years (SD = 12.4) to 47.6 years (SD = 16.2) (F = 222.317, p < 0.001). In all groups, the mean age of individuals with NTSCI was higher than that of individuals with TSCI (t = −14.776, p < 0.001). For NTSCI individuals at this center, we observed neurologic levels of L2 (11.0%), T12 (9.9%), L1 (8.9%), C4 (7.9%), and T9 (7.6%), whereas the neurologic levels for TSCI individuals involved C4 (24.0%), C5 (15.3%), C3 (8.2%), C6 (6.5%), and L1 (5.3%). NTSCI individuals had lower ratios of complete tetraplegia, incomplete tetraplegia, and complete paraplegia compared to TSCI individuals, whereas the incomplete paraplegia ratio was 60.9% in NTSCI individuals and 16.7% in TSCI individuals.
Discussion
To the best of our knowledge, we conducted the largest epidemiologic study of NTSCI individuals in South Korea. Although the available data were TSCI data instead of NTSCI data, the number of cases was compared between the Korea health insurance data and the hospitalization record of our hospital for the period from 2007 to 2017. The result showed that on average, 17.5% of SCI individuals in Korea were admitted to this hospital [17]. Therefore, it is likely that our results are generalizable to NTSCI populations in all of South Korea, hence also enabling comparisons with epidemiological data from other countries. This study compares differences between TSCI and NTSCI individuals who were admitted to this rehabilitation center during the same period.
In a study conducted in Australia by New et al. [18], the male-to-female ratio (1179 men, 1067 women) of NTSCI individuals was 1.10:1. The male-to-female ratio of NTSCI individuals in this study was 1.30:1 (536 men, 412 women), suggesting a possible higher ratio of male individuals than that of New et al. [18]. In contrast, the male-to-female ratio of global TSCI has been reported from 2.5:1 to 5:1 [19], and the male-to-female ratio of TSCI individuals in this study conducted during the same period was 3.47:1. Thus, the male-to-female ratio of individuals with NTSCI was lower than that of individuals with TSCI. This is thought to be because risk factors mainly observed in male individuals with TSCI have little impact on NTSCI individuals. For example, historically, men were more likely to engage in high-risk activities, both occupational and recreational. Certain occupations, such as truck driving and construction, occur in dangerous environments. This was the primary reason for the high incidence of TSCI observed in men versus women [20, 21]. Since these risk factors have little effect on NTSCI individuals, the difference in male and female ratios was smaller in NTSCI individuals than in TSCI individuals.
In the United States, the mean age at SCI onset showed an increasing trend from 29 years in the 1970s to 43 years in 2015 [1]. Another Korean study conducted by Shin et al. [14] showed a similar trend, with the mean age of individuals with SCI increasing from 32.3 years (1987–1996) to 43.6 years (2004–2008) [14]. This study also showed a similar trend: the mean age of all individuals with SCI increased from 33.3 years (1990–1999) to 49.9 years (2010–2019). Furthermore, as described earlier, the mean age of NTSCI individuals was higher than that of TSCI individuals, with mean ages of 38.7 years in 1990–1999 and 55.5 years in 2010–2019. Similarly, New et al. [18] reported that the median age of NTSCI individuals was higher than that of TSCI individuals. In a Korean study conducted by Shin et al. [14], a similar trend was observed, with a higher mean age for NTSCI individuals than for TSCI individuals.
The leading cause of NTSCI was vertebral column degenerative disease, followed by inflammatory and autoimmune diseases and neoplastic disorders. Generally, developed countries tend to have a higher proportion of NTSCI cases caused by degenerative conditions and tumors. In comparison, developing countries tend to have a higher proportion of NTSCI cases caused by infections, particularly tuberculosis and HIV. The data of NTSCI individuals in this center show a pattern similar to that reported in developed countries [22].
Among the NTSCI individuals in this study, 74.4% of individuals had paraplegia while 25.6% had tetraplegia, indicating a trend similar to that of New et al. [18] who reported more cases of paraplegia (69.2%) than tetraplegia (30.8%) among NTSCI individuals. Global data from the New et al. [22] study also showed a similar trend. Among the NTSCI individuals in this center, motor incomplete (AIS-C, D) lesions were more common than motor complete (AIS-A, B) lesions. AIS-D lesions showed an increasing trend, whereas AIS-A lesions showed a decreasing trend.
According to a report by New et al. [23], complete tetraplegia was present in 20% of TSCI individuals, incomplete tetraplegia in 27%, complete paraplegia in 31%, and incomplete paraplegia in 20%. Complete tetraplegia, incomplete tetraplegia, complete paraplegia, and incomplete paraplegia were present in 0%, 27%, 9%, and 64% of NTSCI individuals, respectively. In this study, we observed incomplete paraplegia in 60.9% of NTSCI individuals, showing a similar trend. Overall, the ratios of incomplete lesions and paraplegia were high in NTSCI individuals. This is because injury in the thoracolumbar region was more common in NTSCI individuals than in TSCI individuals, leading to a higher ratio of paraplegia. Moreover, the onset was usually insidious, resulting in a higher proportion of incomplete lesions [23].
The proportion of NTSCI individuals increased during the last 30 years, and this finding is similar to that of Shin et al. [14] in another SCI epidemiologic study conducted in South Korea. Overall, NTSCI individuals had a higher age at onset than individuals with TSCIs, with different male-to-female ratios. Also, more than half (62.3%) of NTSCI etiologies identified in this study were age-related conditions such as vertebral column degenerative disease, neoplastic disorder, and vascular disorder. According to the 2019 population projections for Korea from Statistics Korea, the mean age of the general population increased from 29.5 years in 1990 to 42.2 years in 2019, an increase of 12.7 years over the period. Life expectancy also increased by 11.6 years from 71.7 years in 1990 to 83.3 years in 2019 [24]. Therefore, the prevalence and hence the importance of NTSCI is expected to increase over time. Consequently, examining etiologies associated with age-related conditions will draw increasing attention.
Despite the above significant contributions of the present study, there are some limitations to this study that must be taken into account while interpreting our results. First, although the number of participants in this study is sufficiently large, this study is a single-center study; thus, we cannot generalize these data to estimate the country-wide incidence of NTSCI. If extensive and systematic data on NTSCI individuals are collected in the future, determining the prevalence and incidence for the South Korean population will be easier. We recommend that future studies examine and present country-wide incidence and prevalence statistics. Second, since this was a retrospective study, there were inevitable inaccuracies that may arise from incorrect or incomplete documentation in the medical records of all SCI individuals. However, inaccurate data were excluded from the data analysis in this study, and the reliability of the data is expected to be high because of the large number of total individuals. Furthermore, this study has strength in that it compares NTSCI demographic characteristics with TSCI demographic characteristics.
In conclusion, we have examined the epidemiologic data for NTSCI individuals at a single rehabilitation center during the last 30 years in South Korea. Compared to individuals with TSCI, those with NTSCI had a different mean age at onset, male-to-female ratios, and severity of injury. The proportion of NTSCI has increased due to aging and increased life expectancy. The findings of this study may contribute to the treatment and prevention of NTSCI.
Data availability
Although the data for this study are not publicly available, data will be made available to other researchers upon reasonable request.
References
National Spinal Cord Injury Statistical Center. Spinal cord injury facts and figures at a glance, 2021 SCI Data Sheet. 2021. https://www.nscisc.uab.edu/Public/Facts%20and%20Figures%20-%202021.pdf
New PW, Sundararajan V. Incidence of non-traumatic spinal cord injury in Victoria, Australia: a population-based study and literature review. Spinal Cord. 2008;46:406–11.
Kurtzke JF. Epidemiology of spinal cord injury. Exp Neurol. 1975;48:163–236.
Murray P, Kusior M, editors. Epidemiology of nontraumatic and traumatic spinal-cord injury. In: Archives of physical medicine and rehabilitation. Philadelphia: WB Saunders Company; 1984.
New PW. Non-traumatic spinal cord injury: what is the ideal setting for rehabilitation? Aust Health Rev. 2006;30:353–61.
Minaire P, Castanier M, Girard R, Berard E, Deidier C, Bourret J. Epidemiology of spinal cord injury in the Rhône-Alpes Region, France, 1970-75. Paraplegia. 1978;16:76–87.
Garcia-Reneses J, Herruzo-Cabrera R, Martinez-Moreno M. Epidemiological study of spinal cord injury in Spain 1984-1985. Spinal Cord. 1991;29:180–90.
Schönherr MC, Groothoff JW, Mulder GA, Eisma WH. Rehabilitation of individuals with spinal cord lesions in The Netherlands: an epidemiological study. Spinal Cord. 1996;34:679–83.
Biering-Sørensen E, Pedersen V, Clausen S. Epidemiology of spinal cord lesions in Denmark. Paraplegia. 1990;28:105–18.
Maharaj JC. Epidemiology of spinal cord paralysis in Fiji: 1985-1994. Spinal Cord. 1996;34:549–59.
Adams RD, Salam-Adams M. Chronic nontraumatic diseases of the spinal cord. Neurol Clin. 1991;9:605–23.
Dawson DM, Potts F. Acute nontraumatic myelopathies. Neurol Clin. 1991;9:585–603.
Yang J-Y, Shim D-M, Kim T-K, Moon E-S, Sohn H-M, Hong C-H, et al. Epidemiology of the spinal cord and cauda equina injury in Korea-Multicenter Study. J Korean Soc Spine Surg. 2011;18:83–90.
Shin JC, Kim DH, Yu SJ, Yang HE, Yoon SY. Epidemiologic change of individuals with spinal cord injury. Ann Rehabil Med. 2013;37:50–6.
Han ZA, Lee BS, Kim W, Lee SJ, Im HJ, Kim C, et al. People with spinal cord injury in Korea. Am J Phys Med Rehabil. 2017;96:S83–S85.
New PW, Marshall R. International spinal cord injury data sets for non-traumatic spinal cord injury. Spinal Cord. 2014;52:123–32.
Choi SH, Sung CH, Heo DR, Jeong SY, Kang CN. Incidence of acute spinal cord injury and associated complications of methylprednisolone therapy: a national population-based study in South Korea. Spinal Cord. 2020;58:232–7.
New PW, Simmonds F, Stevermuer T. A population-based study comparing traumatic spinal cord injury and non-traumatic spinal cord injury using a national rehabilitation database. Spinal Cord. 2011;49:397–403.
Singh A, Tetreault L, Kalsi-Ryan S, Nouri A, Fehlings MG. Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol. 2014;6:309–31.
Chen CF, Lien IN. Spinal cord injuries in Taipei, Taiwan, 1978-1981. Paraplegia. 1985;23:364–70.
Pajareya K. Traumatic spinal cord injuries in Thailand: an epidemiologic study in Siriraj Hospital, 1989-1994. Spinal Cord. 1996;34:608–10.
New PW, Cripps RA, Bonne Lee B. Global maps of non-traumatic spinal cord injury epidemiology: towards a living data repository. Spinal Cord. 2014;52:97–109.
New PW, Rawicki HB, Bailey MJ. Nontraumatic spinal cord injury: demographic characteristics and complications. Arch Phys Med Rehabil. 2002;83:996–1001.
Statistics Korea. Population projections for Korea 2019. 2019. https://kosis.kr/eng/statisticsList/statisticsListIndex.do?menuId=M_01_01&vwcd=MT_ETITLE&parmTabId=M_01_01&statId=1962001&themaId=#SelectStatsBoxDiv
Author contributions
BSL was responsible for designing the review protocol, conducting the search, and screening potentially eligible studies. OYK and DHH were responsible for updating reference lists and creating tables and figures. All authors (BSL, OYK, and DHH) were responsible for writing the protocol and report, extracting and analyzing data, interpreting results, and approving the final version of the manuscript.
Funding
International spinal cord injury survey (InSCI) – comparative analysis between the countries of the Western Pacific Region (WPR) spinal cord injury database.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. The Ethics Committee of the Institutional Review Board of the National Rehabilitation Center in South Korea approved this study (approval number: NRC-2019-04-025) and waived the requirement for informed consent because of the retrospective design of this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, BS., Kim, O. & Ham, D. Epidemiologic changes in nontraumatic spinal cord injury for the last 30 years (1990–2019) in South Korea. Spinal Cord 60, 268–273 (2022). https://doi.org/10.1038/s41393-021-00695-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-021-00695-5
This article is cited by
-
Traumatic spinal cord injury in South Korea for 13 years (2008–2020)
Scientific Reports (2024)
-
Caregiver burden according to ageing and type of care activity in caregivers of individuals with spinal cord injury
Spinal Cord Series and Cases (2023)