Abstract
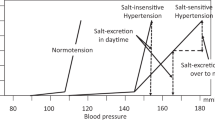
In patients with chronic kidney disease (CKD), the prevalence of increased blood pressure during sleep and blunted sleep-time-relative blood pressure decline (a nondipper pattern) is very high and increases substantially with disease severity. Elevated blood pressure during sleep is the major criterion for the diagnoses of hypertension and inadequate therapeutic ambulatory blood pressure control in these patients. Substantial, clinically meaningful ingestion-time-dependent differences in the safety, efficacy, duration of action and/or effects on the 24 h blood pressure pattern of six different classes of hypertension medications and their combinations have been substantiated. For example, bedtime ingestion of angiotensin-converting-enzyme inhibitors and angiotensin-receptor blockers is more effective than morning ingestion in reducing blood pressure during sleep and converting the 24 h blood pressure profile into a dipper pattern. We have identified a progressive reduction in blood pressure during sleep—a novel therapeutic target best achieved by ingestion of one or more hypertension medications at bedtime—as the most significant predictor of decreased cardiovascular risk in patients with and without CKD. Recent findings suggest that in patients with CKD, ambulatory blood pressure monitoring should be used for the diagnosis of hypertension and assessment of cardiovascular disease risk, and that therapeutic strategies given at bedtime rather than on awakening are preferable for the management of hypertension.
Key Points
-
24 h variations in blood pressure are the result of rest–activity alterations in behaviour, environmental phenomena and endogenous 24 h rhythms in neural, endocrine, endothelial and haemodynamic variables
-
A blunted sleep-time-relative blood pressure decline is significantly associated with an increased risk of end-organ injury and cardiovascular events
-
In patients with chronic kidney disease (CKD), the prevalence of increased blood pressure during sleep and the nondipper profile is very high and increases substantially with disease severity
-
Ingestion of one or more hypertension medications at bedtime is significantly associated with lower asleep systolic and diastolic blood pressure means and attenuated prevalence of the nondipper profile in patients with CKD
-
In patients with hypertension, including those with CKD, a progressive reduction of blood pressure during sleep is the most significant predictor of decreased cardiovascular disease risk
-
We recommend ambulatory blood pressure monitoring in patients with CKD to ensure accurate diagnosis of hypertension, assess cardiovascular disease risk and establish the optimal therapeutic strategy to reduce this risk
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Duguay, D. & Cermakian, N. The crosstalk between physiology and circadian clock proteins. Chronobiol. Int. 26, 1479–1513 (2009).
Touitou, Y. & Haus, E. (Eds) Biological rhythms in clinical and laboratory medicine. (Springer-Verlag, 1992).
Hermida, R. C., Ayala, D. E. & Portaluppi, F. Circadian variation of blood pressure: the basis for the chronotherapy of hypertension. Adv. Drug Deliv. Rev. 59, 904–922 (2007).
Smolensky, M. H., Hermida, R. C., Castriotta, R. J. & Portaluppi, F. Role of sleep–wake cycle on blood pressure circadian rhythms and hypertension. Sleep Med. 8, 668–680 (2007).
Portaluppi, F. et al. Circadian rhythms and cardiovascular health. Sleep Med. Rev. 16, 151–166 (2012).
Fabbian, F. et al. Dipper and non-dipper blood pressure 24-hour patterns: circadian rhythm-dependent physiologic and pathophysiologic mechanisms. Chronobiol. Int. 30, 17–30 (2013).
Manfredini, R., Gallerani, M., Portaluppi, F., Salmi, R. & Fersini, C. Chronobiological patterns of onset of acute cerebrovascular diseases. Thromb. Res. 88, 451–463 (1997).
Casetta, I., Granieri, E., Portaluppi, F. & Manfredini, R. Circadian variability in hemorrhagic stroke. JAMA 287, 1266–1267 (2002).
Gallerani, M., Portaluppi, F., Grandi, E. & Manfredini, R. Circadian rhythmicity in the occurrence of spontaneous acute dissection and rupture of thoracic aorta. J. Thorac. Cardiovasc. Surg. 113, 603–604 (1997).
Mehta, H. R. et al. Chronobiological patterns of acute aortic dissection. Circulation 106, 1110–1115 (2002).
Agarwal, R. & Andersen, M. J. Blood pressure recordings within and outside the clinic and cardiovascular events in chronic kidney disease. Am. J. Nephrol. 26, 503–510 (2006).
Liu, M. et al. Non-dipping is a potent predictor of cardiovascular mortality and is associated with autonomic dysfunction in haemodialysis patients. Nephrol. Dial. Transplant. 18, 563–569 (2003).
Tripepi, G. et al. Prognostic value of 24-hour ambulatory blood pressure monitoring and of night/day ratio in nondiabetic, cardiovascular events-free hemodialysis patients. Kidney Int. 68, 1294–1302 (2005).
Agarwal, R. & Andersen, M. J. Prognostic importance of ambulatory blood pressure recordings in patients with chronic kidney disease. Kidney Int. 69, 1175–1180 (2006).
Minutolo, R. et al. Prognostic role of ambulatory blood pressure measurement in patients with nondialysis chronic kidney disease. Arch. Intern. Med. 171, 1090–1098 (2011).
Hermida, R. C. Ambulatory blood pressure monitoring in the prediction of cardiovascular events and effects of chronotherapy: rationale and design of the MAPEC study. Chronobiol. Int. 24, 749–775 (2007).
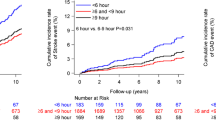
Hermida, R. C., Ayala, D. E., Mojón, A. & Fernández, J. R. Influence of circadian time of hypertension treatment on cardiovascular risk: results of the MAPEC study. Chronobiol. Int. 27, 1629–1651 (2010).
Hermida, R. C., Ayala, D. E., Mojón, A. & Fernández, J. R. Decreasing sleep-time blood pressure determined by ambulatory monitoring reduces cardiovascular risk. J. Am. Coll. Cardiol. 58, 1165–1173 (2011).
Hermida, R. C., Ayala, D. E., Mojón, A. & Fernández, J. R. Influence of time of day of blood pressure-lowering treatment on cardiovascular risk in hypertensive patients with type 2 diabetes. Diabetes Care 34, 1270–1276 (2011).
Hermida, R. C., Ayala, D. E., Mojón, A. & Fernández, J. R. Bedtime dosing of antihypertensive medications reduces cardiovascular risk in CKD. J. Am. Soc. Nephrol. 22, 2313–2321 (2011).
Hermida, R. C., Ayala, D. E., Mojón, A. & Fernández, J. R. Sleep-time blood pressure as a therapeutic target for cardiovascular risk reduction in type 2 diabetes. Am. J. Hypertens. 25, 325–334 (2012).
Ayala, D. E., Hermida, R. C., Mojón, A. & Fernández, J. R. Cardiovascular risk of resistant hypertension: dependence on treatment-time regimen of blood pressure-lowering medications. Chronobiol. Int. 30, 340–352 (2013).
Hermida, R. C. et al. Modeling the circadian variability of ambulatorily monitored blood pressure by multiple-component analysis. Chronobiol. Int. 19, 461–481 (2002).
O'Brien, E., Sheridan, J. & O'Malley, K. Dippers and non-dippers. Lancet 332, 397 (1988).
Sowers, J. R. & Vlachakis, N. Circadian variation in plasma dopamine levels in man. J. Endocrinol. Invest. 7, 341–345 (1984).
Somers, V. K., Dyken, M. E., Mark, A. L. & Abboud, F. M. Sympathetic-nerve activity during sleep in normal subjects. N. Engl. J. Med. 328, 303–307 (1993).
Linsell, C. R., Lightman, S. L., Mullen, P. E., Brown, M. J. & Causon, R. C. Circadian rhythms of epinephrine and norepinephrine in man. J. Clin. Endocrinol. Metab. 60, 1210–1215 (1985).
Lakatua, D. J. et al. Circadian characteristics of urinary epinephrine and norepinephrine from healthy young women in Japan and USA. Chronobiol. Int. 3, 189–195 (1986).
Bartter, F. C., Chan, J. C. M. & Simpson, H. W. in Endocrine Rhythms (ed. Krieger, D. T.) 49–132 (Raven, 1979).
Angeli, A., Gatti, G. & Masera, R. in Biologic Rhythms in Clinical and Laboratory Medicine (eds Touitou, Y. & Haus, E.) 292–314 (Springer-Verlag, 1992).
Kool, M. J., Wijnen, J. A., Derkx, F. H., Struijker Boudier, H. A. & Van Bortel, L. M. Diurnal variation in prorenin in relation to other humoral factors and hemodynamics. Am. J. Hypertens. 7, 723–730 (1994).
Nicholls, M. G. et al. Hormone and blood pressure relationships in primary aldosteronism. Clin. Exp. Hypertens. A. 6, 1441–1458 (1984).
Portaluppi, F. et al. Circadian rhythm of calcitonin gene-related peptide in uncomplicated essential hypertension. J. Hypertens. 10, 1227–1234 (1992).
Sothern, R. B. et al. Temporal (circadian) and functional relationship between atrial natriuretic peptides and blood pressure. Chronobiol. Int. 12, 106–120 (1995).
Kanabrocki, E. L. et al. Day–night variations in blood levels of nitric oxide, T-TFPI and E-selectin. Clin. Appl. Thrombosis/Hemostasis. 7, 339–345 (2001).
Hermida, R. C. & Smolensky, M. H. Chronotherapy of hypertension. Curr. Opin. Nephrol. Hypertens. 13, 501–505 (2004).
Hermida, R. C., Ayala, D. E. & Calvo, C. Administration time-dependent effects of antihypertensive treatment on the circadian pattern of blood pressure. Curr. Opin. Nephrol. Hypertens. 14, 453–459 (2005).
Ohmori, M. & Fujimura, A. ACE inhibitors and chronotherapy. Clin. Exp. Hypertens. 2, 179–185 (2005).
Hermida, R. C., Ayala, D. E., Calvo, C., Portaluppi, F. & Smolensky, M. H. Chronotherapy of hypertension: Administration-time dependent effects of treatment on the circadian pattern of blood pressure. Adv. Drug Deliv. Rev. 59, 923–939 (2007).
Smolensky, M. H., Hermida, R. C., Ayala, D. E., Tiseo, R. & Portaluppi, F. Administration-time-dependent effect of blood pressure-lowering medications: Basis for the chronotherapy of hypertension. Blood Press. Monit. 15, 173–180 (2010).
Hermida, R. C. et al. Circadian rhythms in blood pressure regulation and optimization of hypertension treatment with ACE inhibitor and ARB medications. Am. J. Hypertens. 24, 383–391 (2011).
Smolensky, M. H., Siegel, R. A., Haus, E., Hermida, R. C. & Portaluppi, F. in Fundamentals and applications of controlled release drug delivery (eds Siepmann, J., Siegel, R. A. & Rathbone, M. J.) 359–443 (Springer-Verlag, 2012).
Hermida, R. C. et al. Administration-time-differences in effects of hypertension medications on ambulatory blood pressure regulation. Chronobiol. Int. 30, 280–314 (2013).
Reinberg, A. & Smolensky, M. H. Circadian changes of drug disposition in man. Clin. Pharmacokinet. 7, 401–420 (1982).
Bruguerolle, B. & Lemmer, B. Recent advances in chronopharmacokinetics: methodological problems. Life Sci. 52, 1809–1824 (1993).
Bélanger, P. M., Bruguerolle, B. & Labrecque, G. in Physiology and Pharmacology of Biological Rhythms (eds Redfern, P. H. & Lemmer, B.) 177–204 (Springer-Verlag, 1997).
Labrecque, G. & Beauchamp, D. in Chronotherapeutics Ch. 4 (ed. Redfern, P. H.) 75–110 (Pharmaceutical Press, 2003).
Witte, K. & Lemmer, B. in Chronotherapeutics Ch. 5 (ed. Redfern, P. H.) 111–126 (Pharmaceutical Press, 2003).
Okyar, A. et al. Circadian variations in exsorptive transport: in-situ intestinal perfusion data and in-vivo relevance. Chronobiol. Int. 29, 443–453 (2012).
Verdecchia, P. et al. Ambulatory blood pressure: an independent predictor of prognosis in essential hypertension. Hypertension 24, 793–801 (1994).
Sturrock, N. D. et al. Non-dipping circadian blood pressure and renal impairment are associated with increased mortality in diabetes mellitus. Diabet. Med. 17, 360–364 (2000).
Ohkubo, T. et al. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J. Hypertens. 20, 2183–2189 (2002).
Dolan, E. et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin outcome study. Hypertension 46, 156–161 (2005).
Astrup, A. S. et al. Predictors of mortality in patients with type 2 diabetes with or without diabetic nephropathy: a follow-up study. J. Hypertens. 25, 2479–2485 (2007).
Boggia, J. et al. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 370, 1219–1229 (2007).
Eguchi, K. et al. Ambulatory blood pressure is a better marker than clinic blood pressure in predicting cardiovascular events in patients with/without type 2 diabetes. Am. J. Hypertens. 21, 443–450 (2008).
Salles, G. F., Cardoso, C. R. & Muxfeldt, E. S. Prognostic influence of office and ambulatory blood pressures in resistant hypertension. Arch. Intern. Med. 168, 2340–2346 (2008).
Hermida, R. C., Ayala, D. E., Fernández, J. R. & Mojón, A. Sleep-time blood pressure: prognostic value and relevance as a therapeutic target for cardiovascular risk reduction. Chronobiol. Int. 30, 68–86 (2013).
Hermida, R. C., Ayala, D. E., Mojón, A. & Fernández, J. R. Blunted sleep-time relative blood pressure decline increases cardiovascular risk independent of blood pressure level—the “normotensive non-dipper” paradox. Chronobiol. Int. 30, 87–98 (2013).
Kikuya, M. et al. Ambulatory blood pressure and 10-year risk of cardiovascular and noncardiovascular mortality. The Ohasama Study. Hypertension. 45, 240–245 (2005).
Ben-Dov, I. Z. et al. Predictors of all-cause mortality in clinical ambulatory monitoring. Unique aspects of blood pressure during sleep. Hypertension 49, 1235–1241 (2007).
Fagard, R. H. et al. Daytime and night-time blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension 51, 55–61 (2008).
Fan, H. Q. et al. Prognostic value of isolated nocturnal hypertension on ambulatory measurement in 8711 individuals from 10 populations. J. Hypertens. 28, 2036–2045 (2010).
Hermida, R. C., Ayala, D. E., Mojón, A. & Fernández, J. R. Sleep-time blood pressure and the prognostic value of isolated-office and masked hypertension. Am. J. Hypertens. 25, 297–305 (2012).
Amar, J. et al. Nocturnal blood pressure and 24-hour pulse pressure are potent indicators of mortality in hemodialysis patients. Kidney Int. 57, 2485–2491 (2000).
Portaluppi, F., Montanari, L., Ferlini, M. & Gilli, P. Altered circadian rhythms of blood pressure and heart rate in non-hemodialysis chronic renal failure. Chronobiol. Int. 7, 321–327 (1990).
Agarwal, R. & Andersen, M. J. Correlates of systolic hypertension in patients with chronic kidney disease. Hypertension 46, 514–520 (2005).
Davidson, M. B., Hix, J. K., Vidt, D. G. & Brotman, D. J. Association of impaired diurnal blood pressure variation with a subsequent decline in glomerular filtration rate. Arch. Intern. Med. 166, 846–852 (2006).
Agarwal, R., Peixoto, A. J., Santos, S. F. F. & Zoccali, C. Out-of-office blood pressure monitoring in chronic kidney disease. Blood Press. Monit. 14, 2–11 (2009).
Pogue, V. et al. Disparate estimates of hypertension control from ambulatory and clinic blood pressure measurements in hypertensive kidney disease. Hypertension 53, 20–27 (2009).
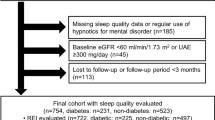
Mojón, A. et al. Comparison of ambulatory blood pressure parameters of hypertensive patients with and without chronic kidney disease. Chronobiol. Int. 30, 145–158 (2013).
Hermida, R. C. et al. Evaluation of the extent and duration of the “ABPM effect” in hypertensive patients. J. Am. Coll. Cardiol. 40, 710–717 (2002).
Hermida, R. C., Ayala, D. E., Fontao, M. J., Mojón, A. & Fernández, J. R. Ambulatory blood pressure monitoring: Importance of sampling rate and duration—48 versus 24 hours—on the accurate assessment of cardiovascular risk. Chronobiol. Int. 30, 55–67 (2013).
Ayala, D. E. et al. Circadian pattern of ambulatory blood pressure in hypertensive patients with and without type 2 diabetes. Chronobiol. Int. 30, 99–115 (2013).
Crespo, J. J. et al. Administration-time-dependent effects of hypertension treatment on ambulatory blood pressure in patients with chronic kidney disease. Chronobiol. Int. 30, 159–175 (2013).
Hermida, R. C. et al. Treatment-time regimen of hypertension medications significantly affects ambulatory blood pressure and clinical characteristics of patients with resistant hypertension. Chronobiol. Int. 30, 192–206 (2013).
Moyá, A. et al. Effects of time-of-day of hypertension treatment on ambulatory blood pressure and clinical characteristics of patients with type 2 diabetes. Chronobiol. Int. 30, 116–131 (2013).
Ríos, M. T. et al. Prevalence and clinical characteristics of isolated-office and true resistant hypertension determined by ambulatory blood pressure monitoring. Chronobiol. Int. 30, 207–220 (2013).
Levey, A. S. et al. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 67, 2089–2100 (2005).
Mancia, G. et al. 2007 guidelines for the management of arterial hypertension. The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J. Hypertens. 25, 1105–1187 (2007).
Hermida, R. C., Calvo, C., Ayala, D. E., Mojón, A. & López, J. E. Relationship between physical activity and blood pressure in dipper and nondipper hypertensive patients. J. Hypertens. 20, 1097–1104 (2002).
Pechère-Bertschi, A. et al. Renal response to the angiotensin II receptor subtype 1 antagonist irbesartan versus enalapril in hypertensive patients. J. Hypertens. 16, 385–393 (1998).
Kohno, I. et al. Effect of imidapril in dipper and nondipper hypertensive patients: comparison between morning and evening administration. Chronobiol. Int. 17, 209–219 (2000).
Kuroda, T. et al. Effects of bedtime vs. morning administration of the long-acting lipophilic angiotensin-converting enzyme inhibitor trandolapril on morning blood pressure in hypertensive patients. Hypertens. Res. 27, 15–20 (2004).
Balan, H., Popescu, E. & Angelescu, G. Comparing different treatment schedules of Zomen (zofenopril). Rom. J. Intern. Med. 49, 75–84 (2011).
Hermida, R. C. & Ayala, D. E. Chronotherapy with the angiotensin-converting enzyme inhibitor ramipril in essential hypertension: improved blood pressure control with bedtime dosing. Hypertension 54, 40–46 (2009).
Hermida, R. C. et al. Administration-time-dependent effects of spirapril on ambulatory blood pressure in uncomplicated essential hypertension. Chronobiol. Int. 27, 560–574 (2010).
Hermida, R. C. et al. Administration-time-dependent effects of valsartan on ambulatory blood pressure in hypertensive subjects. Hypertension 42, 283–290 (2003).
Hermida, R. C., Calvo, C., Ayala, D. E. & López, J. E. Decrease in urinary albumin excretion associated to the normalization of nocturnal blood pressure in hypertensive subjects. Hypertension 46, 960–968 (2005).
Hermida, R. C. et al. Administration-time-dependent effects of valsartan on ambulatory blood pressure in elderly hypertensive subjects. Chronobiol. Int. 22, 755–776 (2005).
O'Sullivan, C., Duggan, J., Atkins, N. & O'Brien, E. Twenty-four-hour ambulatory blood pressure in community-dwelling elderly men and women aged 60–102 years. J. Hypertens. 21, 1641–1647 (2003).
Hermida, R. C. et al. Influence of age and hypertension treatment-time on ambulatory blood pressure in hypertensive patients. Chronobiol. Int. 30, 176–191 (2013).
Hermida, R. C. et al. Treatment of non-dipper hypertension with bedtime administration of valsartan. J. Hypertens. 23, 1913–1922 (2005).
Hermida, R. C., Ayala, D. E., Chayán, L., Mojón, A. & Fernández, J. R. Administration-time-dependent effects of olmesartan on the ambulatory blood pressure of essential hypertension patients. Chronobiol. Int. 26, 61–79 (2009).
Tofé, S. & García, B. 24-hour and nighttime blood pressures in type 2 diabetic hypertensive patients following morning or evening administration of olmesartan. J. Clin. Hypertens. (Greenwich) 11, 426–431 (2009).
Equiluz-Bruck, S., Schnack, C., Kopp, H. P. & Schernthaner, G. Nondipping of nocturnal blood pressure is related to urinary albumin excretion rate in patients with type 2 diabetes mellitus. Am. J. Hypertens. 9, 1139–1143 (1996).
Palmas, W. et al. Nocturnal blood pressure elevation predicts progression of albuminuria in elderly people with type 2 diabetes. J. Clin. Hypertens. (Greenwich) 10, 12–20 (2008).
Hermida, R. C., Ayala, D. E., Fernández, J. R. & Calvo, C. Comparison of the efficacy of morning versus evening administration of telmisartan in essential hypertension. Hypertension 50, 715–722 (2007).
Umeda, T. et al. Timing for administration of an antihypertensive drug in the treatment of essential hypertension. Hypertension. 23 (Suppl. 1), I211–I214 (1994).
Qiu, Y. G., Chenm J. Z., Zhum J. H. & Yao, X. Y. Differential effects of morning or evening dosing of amlodipine on circadian blood pressure and heart rate. Cardiovasc. Drugs Ther. 17, 335–341 (2003).
Kitahara, Y. et al. Effect of morning and bedtime dosing with cilnidipine on blood pressure, heart rate, and sympathetic nervous activity in essential hypertensive patients. J. Cardiovasc. Pharmacol. 43, 68–73 (2004).
Hermida, R. C., Ayala, D. E., Mojón, A. & Fernández, J. R. Chronotherapy with nifedipine GITS in hypertensive patients: Improved efficacy and safety with bedtime dosing. Am. J. Hypertens. 21, 948–954 (2008).
Hermida, R. C., Ayala, D. E., Fontao, M. J., Mojón, A. & Fernández, J. R. Chronotherapy with valsartan/amlodipine combination in essential hypertension: Improved blood pressure control with bedtime dosing. Chronobiol. Int. 27, 1287–1303 (2010).
Meng, Y., Zhang, Z., Liang, X., Wu, C. & Qi, G. Effects of combination therapy with amlodipine and fosinopril administered at different times on blood pressure and circadian blood pressure pattern in patients with essential hypertension. Acta Cardiol. 65, 309–314 (2010).
Zeng, J. et al. Fixed-combination of amlodipine and diuretic chronotherapy in the treatment of essential hypertension: improved blood pressure control with bedtime dosing—a multicenter, open-label randomized study. Hypertens. Res. 34, 767–772 (2011).
Hoshino, A., Nakamura, T. & Matsubara, H. The bedtime administration ameliorates blood pressure variability and reduces urinary albumin excretion in amlodipine-olmesartan combination therapy. Clin. Exp. Hypertens. 32, 416–422 (2010).
Hermida, R. C., Ayala, D. E., Mojón, A., Fontao, M. J. & Fernández, J. R. Chronotherapy with valsartan/hydrochlorothiazide combination in essential hypertension: improved sleep-time blood pressure control with bedtime dosing. Chronobiol. Int. 28, 601–610 (2011).
Minutolo R. et al. Changing the timing of antihypertensive therapy to reduce nocturnal blood pressure in CKD: an 8-week uncontrolled trial. Am. J. Kidney Dis. 50, 908–917 (2007).
Morgan, T. O. Does it matter when drugs are taken? Hypertension 54, 23–24 (2009).
Parati, G. & Bilo, G. Evening administration of antihypertensive drugs: filling a knowledge gap. J. Hypertens. 28, 1390–1392 (2010).
Iskedjian, M. et al. Relationship between daily dose frequency and adherence to antihypertensive pharmacotherapy: evidence from a meta-analysis. Clin. Ther. 24, 302–316 (2002).
Flack, J. M. & Nasser, S. A. Benefits of once-daily therapies in the treatment of hypertension. Vasc. Health Risk Manag. 7, 777–787 (2011).
Hermida, R. C. et al. 2013 ambulatory blood pressure monitoring recommendations for the diagnosis of adult hypertension, assessment of cardiovascular and other hypertension-associated risk, and attainment of therapeutic goals. Joint recommendations from the International Society for Chronobiology (ISC), American Association of Medical Chronobiology and Chronotherapeutics (AAMCC), Spanish Society of Applied Chronobiology, Chronotherapy, and Vascular Risk (SECAC), Spanish Society of Atherosclerosis (SEA), and Romanian Society of Internal Medicine (RSIM). Chronobiol. Int. 30, 355–410 (2013).
American Diabetes Association: Standards of medical care in diabetes—2012. Diabetes Care 35 (Suppl. 1), S11–S63 (2012).
Sternberg, H., Rosenthal, T., Shamiss, A. & Green, M. Altered circadian rhythm of blood pressure in shift workers. J. Hum. Hypertens. 9, 349–353 (1995).
Sundberg, S., Kohvakka, A. & Gordin, A. Rapid reversal of circadian blood pressure rhythm in shift workers. J. Hypertens. 6, 393–396 (1988).
Ohira, T. et al. Effects of shift work on 24-hour ambulatory blood pressure and its variability among Japanese workers. Scand. J. Environ. Health. 26, 421–426 (2000).
Kitamura, T. et al. Circadian rhythm of blood pressure is transformed from a dipper to a non-dipper pattern in shift workers with hypertension. J. Hum. Hypertens. 16, 193–197 (2002).
Portaluppi, F. & Smolensky, M. H. Perspectives on the chronotherapy of hypertension based on the results of the MAPEC study. Chronobiol. Int. 27, 1652–1667 (2010).
Acknowledgements
The authors' research is supported by unrestricted grants from the Ministerio de Ciencia e Innovación (SAF2009-7028-FEDER), the Consellería de Economía e Industria, Xunta de Galicia (INCITE07-PXI-322003ES, INCITE08-E1R-322063ES, INCITE09-E2R-322099ES, IN845B-2010/114 and 09CSA018322PR), the European Research Development Fund, the Consellería de Cultura, Educación e Ordenación Universitaria, Xunta de Galicia (CN2012/251 & CN2012/260) and Vicerrectorado de Investigación, University of Vigo (awarded to R. C. Hermida, D. E. Ayala, A. Mojón and J. R. Fernández).
Author information
Authors and Affiliations
Contributions
R. Hermida, D. E. Ayala and M. H. Smolensky researched the data for the article and wrote the manuscript. All authors made a substantial contribution to discussions of the content and reviewed and/or edited the article before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Hermida, R., Ayala, D., Smolensky, M. et al. Chronotherapy improves blood pressure control and reduces vascular risk in CKD. Nat Rev Nephrol 9, 358–368 (2013). https://doi.org/10.1038/nrneph.2013.79
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneph.2013.79
This article is cited by
-
Circadian rhythm as a therapeutic target
Nature Reviews Drug Discovery (2021)
-
The deadly line linking sympathetic overdrive, dipping status and vascular risk: critical appraisal and therapeutic implications
Hypertension Research (2016)
-
Chronotherapy with conventional blood pressure medications improves management of hypertension and reduces cardiovascular and stroke risks
Hypertension Research (2016)
-
Chronotherapeutics of Conventional Blood Pressure-Lowering Medications: Simple, Low-Cost Means of Improving Management and Treatment Outcomes of Hypertensive-Related Disorders
Current Hypertension Reports (2014)