Key Points
-
Transplantation of kidneys from living donors is an important treatment for kidney failure, but the long-term risks to kidney donors are unclear; understanding the risks could improve the informed consent process
-
Studies suggest that living kidney donors are at increased risk of developing end-stage renal disease relative to healthy nondonors, but the 15-year cumulative incidence remains <1%
-
All-cause mortality in the first decade after nephrectomy seems to be lower or no different among donors than among healthy nondonors; one study suggests that over 25 years, the incidence might increase by 5%
-
The absolute incidence of gout might increase by <2% in the first decade after donation among donors compared with healthy matched nondonors
-
Women should be informed that complications of pregnancy are more likely after donation than before donation and that their risk of gestational hypertension and pre-eclampsia is 6% higher than that in nondonors
-
Risks of acute kidney injury, cardiovascular events, kidney stones requiring surgical intervention, major gastrointestinal bleeding and skeletal fractures do not seem to be increased in the decade after kidney donation
Abstract
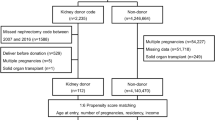
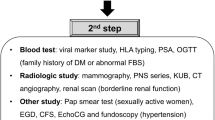
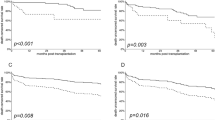
Living kidney donation benefits recipients and society but carries short-term and long-term risks for the donor. This Review summarizes the studies that underlie our current understanding of these risks in the first decade after donation, with a view to improving the informed consent process. Two studies report a higher risk of end-stage renal disease (ESRD) among donors than among healthy nondonors; however, the absolute 15-year incidence of ESRD is <1%. All-cause mortality and the risk of cardiovascular events are similar among donors and healthy nondonors, although one study provides evidence for a 5% increase in all-cause mortality after 25 years that is attributable to donation. Some evidence suggests that the 20-year incidence of gout is slightly higher among donors than among healthy nondonors. The risks of gestational hypertension or pre-eclampsia seem to be 6% higher in pregnancies among donors than in pregnancies among healthy nondonors. The incidences of acute kidney injury, kidney stones that require surgical intervention, gastrointestinal bleeding and fractures seem no higher among donors than among healthy nondonors, although some of these conclusions are based on a small number of events. Future studies must clarify the lifetime incidence of long-term outcomes, particularly in relation to a donor's age, race, and history of comorbidities.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Horvat, L. D., Shariff, S. Z., Garg, A. X. & Donor Nephrectomy Outcomes Research DONOR Network. Global trends in the rates of living kidney donation. Kidney Int. 75, 1088–1098 (2009).
Garg, A. X. et al. Proteinuria and reduced kidney function in living kidney donors: a systematic review, meta-analysis, and meta-regression. Kidney Int. 70, 1801–1810 (2006).
Coresh, J. et al. Decline in estimated glomerular filtration rate and subsequent risk of end-stage renal disease and mortality. JAMA 311, 2518–2531 (2014).
Sarnak, M. J. et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation 108, 2154–2169 (2003).
Matsushita, K. et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet 375, 2073–2081 (2010).
Matas, A. J. & Ibrahim, H. N. The unjustified classification of kidney donors as patients with CKD: critique and recommendations. Clin. J. Am. Soc. Nephrol. 8, 1406–1413 (2013).
Srinivas, T. R. & Poggio, E. D. Do living kidney donors have CKD? Adv. Chronic Kidney Dis. 19, 229–236 (2012).
Lin, J., Kramer, H. & Chandraker, A. K. Mortality among living kidney donors and comparison populations. N. Engl. J. Med. 363, 797–798 (2010).
Boudville, N. et al. Meta-analysis: risk for hypertension in living kidney donors. Ann. Intern. Med. 145, 185–196 (2006).
Ibrahim, H. N. et al. Long-term consequences of kidney donation. N. Engl. J. Med. 360, 459–469 (2009).
Fehrman-Ekholm, I., Elinder, C. G., Stenbeck, M., Tydén, G. & Groth, C. G. Kidney donors live longer. Transplantation 64, 976–978 (1997).
Segev, D. L. et al. Perioperative mortality and long-term survival following live kidney donation. JAMA 303, 959–966 (2010).
Mjøen, G., Øyen, O., Holdaas, H., Midtvedt, K. & Line, P. D. Morbidity and mortality in 1022 consecutive living donor nephrectomies: benefits of a living donor registry. Transplantation 88, 1273–1279 (2009).
Okamoto, M. et al. Short- and long-term donor outcomes after kidney donation: analysis of 601 cases over a 35-year period at Japanese single center. Transplantation 87, 419–423 (2009).
Clemens, K. et al. The long-term quality of life of living kidney donors: a multicenter cohort study. Am. J. Transplant. 11, 463–469 (2011).
Clemens, K. K. et al. Psychosocial health of living kidney donors: a systematic review. Am. J. Transplant. 6, 2965–2977 (2006).
Smith, G. C., Trauer, T., Kerr, P. G. & Chadban, S. J. Prospective psychosocial monitoring of living kidney donors using the Short Form-36 health survey: results at 12 months. Transplantation 78, 1384–1389 (2004).
Klarenbach, S. et al. Economic consequences incurred by living kidney donors: a Canadian multi-center prospective study. Am. J. Transplant. 14, 916–922 (2014).
Clarke, K. S. et al. The direct and indirect economic costs incurred by living kidney donors—a systematic review. Nephrol. Dial. Transplant. 21, 1952–1960 (2006).
Yang, R. C. et al. Life insurance for living kidney donors: a Canadian undercover investigation. Am. J. Transplant. 9, 1585–1590 (2009).
Yang, R. C. et al. Insurability of living organ donors: a systematic review. Am. J. Transplant. 7, 1542–1551 (2007).
Iordanous, Y. et al. Recipient outcomes for expanded criteria living kidney donors: the disconnect between current evidence and practice. Am. J. Transplant. 9, 1558–1573 (2009).
Young, A. et al. Living kidney donor estimated glomerular filtration rate and recipient graft survival. Nephrol. Dial. Transplant. 29, 188–195 (2014).
Kim, S. H. et al. Long-term risk of hypertension and chronic kidney disease in living kidney donors. Transplant. Proc. 44, 632–634 (2012).
Helal, I. et al. Short- and long-term outcomes of kidney donors: a report from Tunisia. Saudi J. Kidney Dis. Transpl. 23, 853–859 (2012).
Gracida, C., Espinoza, R. & Cancino, J. Can a living kidney donor become a kidney recipient? Transplant. Proc. 36, 1630–1631 (2004).
Wafa, E. W. et al. End-stage renal disease among living-kidney donors: single-center experience. Exp. Clin. Transplant. 9, 14–19 (2011).
Kido, R. et al. How do living kidney donors develop end-stage renal disease? Am. J. Transplant. 9, 2514–2519 (2009).
Gibney, E. M., King, A. L., Maluf, D. G., Garg, A. X. & Parikh, C. R. Living kidney donors requiring transplantation: focus on African Americans. Transplantation 84, 647–649 (2007).
Fehrman-Ekholm, I. et al. Incidence of end-stage renal disease among live kidney donors. Transplantation 82, 1646–1648 (2006).
Gossmann, J. et al. Long-term consequences of live kidney donation follow-up in 93% of living kidney donors in a single transplant center. Am. J. Transplant. 5, 2417–2424 (2005).
Fournier, C. et al. Very long-term follow-up of living kidney donors. Transpl. Int. 25, 385–390 (2012).
Rosenblatt, G. S., Nakamura, N. & Barry, J. M. End-stage renal disease after kidney donation: a single-center experience. Transplant. Proc. 40, 1315–1318 (2008).
Cherikh, W. S. et al. Ethnic and gender related differences in the risk of end-stage renal disease after living kidney donation. Am. J. Transplant. 11, 1650–1655 (2011).
Fehrman-Ekholm, I., Dunér, F., Brink, B., Tydén, G. & Elinder, C. G. No evidence of accelerated loss of kidney function in living kidney donors: results from a cross-sectional follow-up. Transplantation 72, 444–449 (2001).
Mjøen, G. et al. Long-term risks for kidney donors. Kidney Int. 86, 162–167 (2014).
Muzaale, A. D. et al. Risk of end-stage renal disease following live kidney donation. JAMA 311, 579–586 (2014).
Boudville, N. & Garg, A. X. End-stage renal disease in living kidney donors. Kidney Int. 86, 20–22 (2014).
Lam, N. N., Lentine, K. L. & Garg, A. X. End-stage renal disease risk in live kidney donors: what have we learned from two recent studies? Curr. Opin. Nephrol. Hypertens. 23, 592–596 (2014).
Mjøen, G., Hallan, S. & Holdaas, H. The authors reply. Kidney Int. 85, 1241–1242 (2014).
Gaston, R. S., Kumar, V. & Matas, A. J. Reassessing medical risk in living kidney donors. J. Am. Soc. Nephrol. http://dx.doi.org/10.1681/ASN.2014030227.
Gill, J. S. & Tonelli, M. Understanding rare adverse outcomes following living kidney donation. JAMA 311, 577–579 (2014).
Lam, N. et al. Acute dialysis risk in living kidney donors. Nephrol. Dial. Transplant. 27, 3291–3295 (2012).
Garg, A. X. et al. Cardiovascular disease in kidney donors: matched cohort study. BMJ 344, e1203 (2012).
Mjøen, G. et al. Overall and cardiovascular mortality in Norwegian kidney donors compared to the background population. Nephrol. Dial. Transplant. 27, 443–447 (2012).
Reese, P. P. et al. Mortality and cardiovascular disease among older live kidney donors. Am. J. Transplant. 14, 1853–1861 (2014).
Delmonico, F. A report of the Amsterdam Forum on the Care of the Live Kidney Donor: data and medical guidelines. Transplantation 79 (6 Suppl.), S53–S66 (2005).
Thomas, S. M. et al. Risk of kidney stones with surgical intervention in living kidney donors. Am. J. Transplant. 13, 2935–2944 (2013).
Boyle, J. M. & Johnston, B. Acute upper gastrointestinal hemorrhage in patients with chronic renal disease. Am. J. Med. 75, 409–412 (1983).
Holden, R. M., Harman, G. J., Wang, M., Holland, D. & Day, A. G. Major bleeding in hemodialysis patients. Clin. J. Am. Soc. Nephrol. 3, 105–110 (2008).
Thomas, S. M. et al. Risk of serious gastrointestinal bleeding in living kidney donors. Clin. Transplant. 28, 530–539 (2014).
Kovesdy, C. P. & Kalantar-Zadeh, K. Bone and mineral disorders in pre-dialysis CKD. Int. Urol. Nephrol. 40, 427–440 (2008).
Nickolas, T. L., McMahon, D. J. & Shane, E. Relationship between moderate to severe kidney disease and hip fracture in the United States. J. Am. Soc. Nephrol. 17, 3223–3232 (2006).
Kasiske, B. L. et al. A prospective controlled study of kidney donors: baseline and 6-month follow-up. Am. J. Kidney Dis. 62, 577–586 (2013).
Young, A. et al. Bone and mineral metabolism and fibroblast growth factor 23 levels after kidney donation. Am. J. Kidney Dis. 59, 761–769 (2012).
Garg, A. X. et al. Fracture risk in living kidney donors: a matched cohort study. Am. J. Kidney Dis. 59, 770–776 (2012).
Campion, E. W., Glynn, R. J. & DeLabry, L. O. Asymptomatic hyperuricemia. Risks and consequences in the Normative Aging Study. Am. J. Med. 82, 421–426 (1987).
Krishnan, E. Reduced glomerular function and prevalence of gout: NHANES 2009–10. PLoS ONE 7, e50046 (2012).
Lipkowitz, M. S. Regulation of uric acid excretion by the kidney. Curr. Rheumatol. Rep. 14, 179–188 (2012).
Lam, N. N. et al. Gout after living kidney donation: a matched cohort study. Am. J. Kidney Dis. http://dx.doi.org/10.1053/j.ajkd.2015.01.017
Reisaeter, A. V, Røislien, J., Henriksen, T., Irgens, L. M. & Hartmann, A. Pregnancy and birth after kidney donation: the Norwegian experience. Am. J. Transplant. 9, 820–824 (2009).
Ibrahim, H. N. et al. Pregnancy outcomes after kidney donation. Am. J. Transplant. 9, 825–834 (2009).
Garg, A. X. et al. Gestational hypertension and preeclampsia in living kidney donors. N. Engl. J. Med. 372, 124–133 (2015).
Ahmadi, A. R. et al. Shifting paradigms in eligibility criteria for live kidney donation: a systematic review. Kidney Int. 87, 31–45 (2015).
Steiner, R. W., Ix, J. H., Rifkin, D. E. & Gert, B. Estimating risks of de novo kidney diseases after living kidney donation. Am. J. Transplant. 14, 538–544 (2014).
Steiner, R. W. 'Normal for now' or 'at future risk': a double standard for selecting young and older living kidney donors. Am. J. Transplant 10, 737–741 (2010).
MacDonald, D. et al. Medical outcomes of adolescent live kidney donors. Pediatr. Transplant. 18, 336–341 (2014).
Lentine, K. L. et al. Consistency of racial variation in medical outcomes among publicly and privately insured living kidney donors. Transplantation 97, 316–324 (2014).
Lentine, K. L. et al. Racial variation in medical outcomes among living kidney donors. N. Engl. J. Med. 363, 724–732 (2010).
Storsley, L. J. et al. Long-term medical outcomes among Aboriginal living kidney donors. Transplantation 90, 401–406 (2010).
Rogers, N. M., Lawton, P. D. & Jose, M. D. Indigenous Australians and living kidney donation. N. Engl. J. Med. 361, 1513–1516 (2009).
Reese, P. P. et al. Substantial variation in the acceptance of medically complex live kidney donors across US renal transplant centers. Am. J. Transplant. 8, 2062–2070 (2008).
Taler, S. J. et al. Demographic, metabolic, and blood pressure characteristics of living kidney donors spanning five decades. Am. J. Transplant. 13, 390–398 (2013).
Young, A. et al. Health outcomes for living kidney donors with isolated medical abnormalities: a systematic review. Am. J. Transplant. 8, 1878–1890 (2008).
Kumar, A., Das, S. K. & Srivastava, A. Expanding the living related donor pool in renal transplantation: use of marginal donors. Transplant. Proc. 35, 28–29 (2003).
Tsinalis, D., Binet, I., Steiger, J., Gasser, T. & Thiel, G. Can “borderline” living kidney donors (BLKD) be used safely for transplantation? Kidney Blood Press. Res. 22, 388–389 (1999).
Srivastava, A. et al. Experience with marginal living related kidney donors: are they becoming routine or are there still any doubts? Urology 66, 971–975 (2005).
Sahin, S. et al. Transplantation from living related marginal donors. Nephrol. Dial. Transplant. 15, A275 (2000).
Gracida, C., Espinoza, R., Cedillo, U. & Cancino, J. Kidney transplantation with living donors: nine years of follow-up of 628 living donors. Transplant. Proc. 35, 946–947 (2003).
Textor, S. C. et al. Blood pressure and renal function after kidney donation from hypertensive living donors. Transplantation 78, 276–282 (2004).
Jacobs, S. C. et al. Laparoscopic nephrectomy in the markedly obese living kidney donor. Urology 56, 926–929 (2000).
Chavin, K. D. et al. Laparoscopic donor nephrectomy is safe for the obese living kidney donor [abstract]. J. Am. Soc. Nephrol. 13, 597A (2002).
Chow, G. K., Prieto, M., Bohorquez, H. E. & Stegall, M. D. Hand-assisted laparoscopic donor nephrectomy for morbidly obese patients. Transplant. Proc. 34, 728 (2002).
Mateo, R. B. et al. Comparison of outcomes in noncomplicated an in higher-risk donors after standard versus hand-assisted laparoscopic nephrectomy. Am. Surg. 69, 771–778 (2003).
Bachmann, A. et al. Obese donors report more pain after donor nephrectomy. Eur. Urol. Suppl. 4, 168 (2005).
Kuo, P. C., Plotkin, J. S., Stevens, S., Cribbs, A. & Johson, J. B. Outcomes of laparoscopic donor nephrectomy in obese patients. Transplantation 69, 180–182 (2000).
Rea, D. J. et al. Glomerular volume and renal histology in obese and non-obese living kidney donors. Kidney Int. 70, 1636–1641 (2006).
Heimbach, J. K. et al. Obesity in living kidney donors: clinical characteristics and outcomes in the era of laparoscopic donor nephrectomy. Am. J. Transplant. 5, 1057–1064 (2005).
Espinoza, R., Gracida, C., Cancino, J. & Ibarra, A. Effect of obese living donors on the outcome and metabolic features in recipients of kidney transplantation. Transplant. Proc. 38, 888–889 (2006).
Okamoto, M. et al. The consequences for live kidney donors with preexisting glucose intolerance without diabetic complication: analysis at a single Japanese center. Transplantation 89, 1391–1395 (2010).
Chandran, S., Masharani, U., Webber, A. B. & Wojciechowski, D. M. Prediabetic living kidney donors have preserved kidney function at 10 years after donation. Transplantation 97, 748–754 (2014).
Housawi, A. A. et al. Transplant professionals vary in the long-term medical risks they communicate to potential living kidney donors: an international survey. Nephrol. Dial. Transplant. 22, 3040–3045 (2007).
Moody, E. M. et al. Improving on-line information for potential living kidney donors. Kidney Int. 71, 1062–1070 (2007).
Acknowledgements
N.N.L. is supported by the Clinical Investigator Program at Western University and by a Kidney Research Scientist Core Education and National Training Program postdoctoral fellowship award. K.L.L. is supported by a grant from the NIH National Institute of Diabetes and Digestive and Kidney Diseases, entitled “Long-term health outcomes after live kidney donation in African Americans” (R01-DK096008). B.L.K. is supported by a grant from the NIH National Institute of Diabetes and Digestive and Kidney Diseases, entitled “Assessing long-term outcomes of living donation” (U01-DK066013-09). A.X.G. is supported by the Dr Adam Linton Chair in Kidney Health Analytics.
Author information
Authors and Affiliations
Contributions
N.N.L. and A.X.G. researched data for the article. N.N.L., K.L.L. and A.X.G. wrote the article. All authors contributed to discussion of the content and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
A.X.G. has received an investigator-initiated grant from Astellas Pharma and Roche to support a Canadian Institutes of Health Research study in living kidney donors, and his institution received unrestricted research funding from Pfizer. The other authors declare no competing interests.
PowerPoint slides
Rights and permissions
About this article
Cite this article
Lam, N., Lentine, K., Levey, A. et al. Long-term medical risks to the living kidney donor. Nat Rev Nephrol 11, 411–419 (2015). https://doi.org/10.1038/nrneph.2015.58
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneph.2015.58
This article is cited by
-
The Minnesota attributable risk of kidney donation (MARKD) study: a retrospective cohort study of long-term (> 50 year) outcomes after kidney donation compared to well-matched healthy controls
BMC Nephrology (2023)
-
Pregnancy in Living Kidney Donors: An Evidence-Based Review
Current Transplantation Reports (2023)
-
Managing the Costs of Routine Follow-up Care After Living Kidney Donation: a Review and Survey of Contemporary Experience, Practices, and Challenges
Current Transplantation Reports (2022)
-
Long-term mortality of living kidney donors: a systematic review and meta-analysis
International Urology and Nephrology (2021)
-
Low Birth Weight, Blood Pressure and Renal Susceptibility
Current Hypertension Reports (2019)