Abstract
As the use of elderly kidney donors for transplantation is increasing with time, there is a need to understand which factors impact on their prognosis. No data exist on the impact of an impaired renal function (IRF) in such population. 116 kidney recipients from deceased kidney donors over 70 years were included from 2005 to 2015 in a single-center retrospective study. IRF before organ procurement was defined as a serum creatinine above 1.0 mg/dl or a transient episode of oligo-anuria. Mean ages for donors and recipients were respectively 74.8 ± 3.5 and 66.7 ± 8.0. Graft survival censored for death at 5 years was of 77%. Using a multivariate analysis by Cox model, the only predictor of graft loss present in the donor was IRF before organ procurement (HR 4.2 CI95[1.8–9.7]). IRF was also associated with significant lower estimated glomerular filtration rates up to 1 year post-transplantation. By contrast, KDPI score (median of 98 [96–100]), was not associated with the risk of graft failure. Then, IRF before kidney procurement may define a risk subgroup among very-old deceased kidney donors, in whom pre-implantatory biopsies, dual kidney transplantation or calcineurin inhibitor-free immunosuppressive regimen could help to improve outcomes.
Similar content being viewed by others
Introduction
In order to face the organ shortage crisis, the proportion of kidneys from deceased donors older than 70 years has significantly increased in the past few years. However, the use of elderly kidney donors varies between countries. For instance, in 2015 only 4.9% of deceased kidney donors were older than 65 years in the U.S1, compared to 35% in France2. The rate of discarded kidneys, which is almost twice as high in the US than in France, partly explains this difference3. Thus, it is crucial to identify specific prognostic factors related to these marginal kidneys in order to determine subgroups at risk which may benefit from protective strategies. Moreover, a recent analysis of disparities between France and the US revealed that a more aggressive policy of acceptance, especially in elderly donors, may reduce drastically the rate of discarded kidneys4.
Until 2014 in the U.S, grafts were classified as extended criteria donors (ECD) kidneys or standard criteria donors (SCD) kidneys5. However, this binary classification did not take into consideration other comorbidities apart from age, hypertension, serum creatinine and stroke, which are frequently observed in older donors. In 2014, the Organ Procurement and Transplantation Network and United Network for Organ Sharing (OPTN/UNOS) introduced a continuous score in the U.S allocation system, namely the Kidney Donor Profile Index (KDPI), based on 10 donor-factors to better estimate the quality of the graft6. The KDPI was built to be used in tandem with the estimated post-transplantation survival (EPTS) score for recipients in order to attribute the best kidneys to the best recipients, moving from an equity to a usefulness paradigm7. However, the KDPI did not reduce the discard rate of marginal kidneys. Indeed, analysis of the OPTN/UNOS register revealed that up to 62% of kidneys with a KDPI above 90% are not transplanted8. It is noteworthy that the KDPI of a donor older than 70 years, without any comorbidities, is higher than 80%.
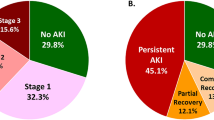
The present study focused on identifying risk factors for graft loss, in a population of recipients transplanted from deceased donors older than 70 years, in order to refine the prognosis of transplantation. Considering that kidney aging is associated with altered regenerative abilities9, we tested if an impaired renal function (IRF) prior to organ removal could impact long-term allograft outcomes. Indeed, donor renal function has never been evaluated in these old donors. The impact of donor renal function on kidney transplantation outcomes is difficult to assess, as controversy exists in the literature regarding the way to evaluate it. For instance, recent large-scaled studies did not demonstrate deleterious effects of donor acute kidney injury (AKI) on long-term outcomes, using the standard definition of KDIGO10,11,12. In the particular case of very-old donor kidneys, where the functional reserve may be decreased because of aging, we hypothesized that the combination of the peak serum creatinine value and the urine output, defining IRF, could be associated with graft outcomes.
Therefore, we retrospectively analyzed graft outcomes from deceased kidney donors older than 70 years according to the presence of IRF before organ procurement.
Results
Donors’ and recipients’ baseline characteristics
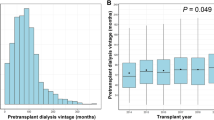
From 01/01/2005 to 31/12/2015, 116/1461 (8%) recipients received a kidney from a deceased donor older than 70 years. Median follow-up was 34 months (17–52).
All donors’ demographic characteristics are summarized in Table 1. Briefly, mean age was 74.8 ± 3.5 and most of them died from cerebrovascular events (75.9%). Mean KDPI was 97.1 ± 3.5.
31 donors (26.7%) presented with impaired renal function (IRF group) defined as oligo-anuria (25.8 of them versus 0% in the control group, p < 0.001) and/or SCr > 1 mg/dl at the time of procurement (1.22 IQR[1.07–1.40] versus 0.72 IQR[0.60–0.81], p < 0.001). The 1.0 mg/dl peak serum creatinine value cut-off corresponded to the fourth quartile of the distribution and was data-driven as it was associated with a significant lower graft survival when compared to other quartiles (Supplementary Fig. 1). When compared to the 85 remaining donors without renal failure (NoIRF group) they presented a higher body mass index (29.5 ± 6 versus 26.9 ± 5, p = 0.04), a more frequent diabetic history (22.6 versus 8.2%, p = 0.05) and their KDPI was slightly higher (98.2 ± 2.4 versus 96.7 ± 3.8, p = 0.014). 32.3% of them had recovered from a cardiac arrest before procurement (versus 6% in the control group, p < 0.001).
Demographic characteristics of the recipients are summarized in Table 2. Mean age was 66.7 ± 8.0. 14.7% of them had already benefited from previous kidney transplantation and 31% presented with preformed HLA antibodies. Median waiting time on dialysis was 31.5 (18–47.5) months. The recipients in the IRF group presented with a more frequent history of stroke (19.4% versus 3.5%, p = 0.011) and peripheral arteritis (19.4% versus 3.5%, p = 0.011). However, the Charlson comorbidity index was similar in both groups (5.7 ± 1.5 versus 5.3 ± 1.6, NS).
Post-transplantation outcomes
As shown in Table 3, the prevalence of DGF, surgical complications, acute rejection and infections was not significantly different between the 2 groups.
However, IRF was associated with a significant lower eGFR from month 1 (26.7 ± 12.4 versus 32.7 ± 12.7 ml/min/1.73 m2, p = 0.03) up to month 12 post transplantation (30.3 ± 12.3 versus 38.9 ± 13.9 ml/min/1.73 m2, p = 0.02).
Overall death-censored graft survival rates were respectively 91%, 86% and 77% at year 1, 3 and 5 post-transplant. Death-uncensored graft survival rates were respectively 83%, 73% and 59% at year 1, 3, and 5 post-transplant.
IRF was associated with lower death-censored (Fig. 1A, p < 0.001) or death-uncensored (Fig. 1B, p = 0.003) non-adjusted graft survival rates.
Graft survival rates: non-adjusted survival rates death-censored (A) and death-uncensored (B) and adjusted graft survival rate, death-censored (C) and death-uncensored (D). (C) Adjustment for post-transplant hematoma, acute rejection, BK virus nephropathy and BMI. (D) Adjustment for post-transplant hematoma and urinoma, acute rejection and BK virus nephropathy. Bold line = donor impaired renal function group. Dashed line = no donor impaired renal function group. Donor renal failure was defined as a donor with a serum creatinine over 1.0 mg/dl or with a transient oligo-anuria before organ procurement. p-values for non-adjusted curves were defined according to the log-rank test. p-values for adjusted curves were defined according to the Cox model analyses.
Risk factors for graft loss
Cox regression models were built (Tables 4, 5) to identify independent risk factors for graft loss in the overall population. Among recipient’s factors, univariate analysis revealed that post-transplant hematoma and urinoma, acute rejection and BK virus nephropathy were significantly associated with a higher risk of graft failure. BMI above 30 kg/m2 was also a risk factor of death-censored graft loss. Among donor’s related parameters, IRF was the only significant risk factor, both in death-censored and death-uncensored univariate analyses. In multivariate analysis, it remained significantly associated with a higher risk of graft loss (HR 4.0 [1.4–11.3] and 2.3 [1.2–4.4] for death-censored and death-uncensored multivariate models, respectively) and lower adjusted death-censored (Fig. 1C, p = 0.008) and death-uncensored (Fig. 1D, p = 0.016) graft survival rates.
Other donor and recipients related variables such as cardiovascular comorbidities, post-transplant cardiovascular events, infections (see Supplementary Table 1), were also not significant.
Discussion
Several studies have reported the outcomes of renal transplant recipients who received a kidney from a deceased donor older than 70 years (Table 6)13,14,15,16,17,18,19,20. However, none of these studies have analyzed the impact of donor IRF before kidney procurement. In our study, we provide for the first-time evidence that IRF has a deleterious impact on long-term outcomes for donors older than 70 years old. Indeed we found that a peak serum creatinine above 1.0 mg/dl and/or an oligo-anuria episode before organ procurement is associated with a lower eGFR up to 1 year post transplantation and impairs graft survival, both in death-censored and death-uncensored analyses, after adjustment for confounding factors. These results may reflect a lower tissue repair capacity after ischemia–reperfusion9, due to kidney aging, which would account for the persistent altered renal function at 1 year. We used the serum creatinine peak instead of the standard classification of AKI11 or the final serum creatinine for several reasons21. It remains difficult to define renal function in deceased-donors, as their baseline serum creatinine is rarely available and the changes in the serum creatinine values during organ procurement may depends of hemodynamic parameters as well as haemodilution. Furthermore the impact of donor AKI on kidney transplantation outcomes is still controversial although recent large-scaled studies did not demonstrate deleterious effects10. The serum creatinine peak can reflect the renal function reserve which can be reduced in old donors and could be a relevant parameter in this population. Indeed an increased last serum creatinine in such donors leads frequently to kidney discard. The present study is limited by the sample size, and a larger cohort would be required to explore the impact of different serum creatinine cutoffs, although large observational studies would also be limited due to the reluctance to accept very-old donors’ kidney with a last serum creatinine above 1.5 mg/dl. Overall death-censored and death-uncensored 5-year graft survival rates were 77% and 59% respectively in line with previous reports13,14,15,16,17,18,19,20 (Table 6). These results may be considered as acceptable, since the median age of recipients was 66 (63–72) years, close to a so-called “old-for-old” allocation. Indeed Lloveras et al. showed that kidney recipients from donors older than 65 years, had a better prognosis than patients remaining on the waiting list, after matching for sex, age, primary renal disease, time on dialysis and cardiovascular comorbidities22. However, in the present study, when the donor presented with IRF before organ procurement, 5-year graft survival rates decreased to 55.3% and 49.8% for death-censored and death-uncensored analyses, respectively. This poor prognosis could jeopardize the benefits from transplantation, even in old recipients.
Unlike impaired renal function before procurement, KDPI failed to discriminate the “bad” and “good” grafts in these very old donors. Indeed KDPI was very high (97.1 ± 3.5), higher than 90% in most donors (97.4%). This could explain why KDPI was not associated with transplantation outcomes in this specific population, and may not be an accurate marker to assess the graft quality in older donors. Data from other European countries23,24,25 validated the use of KDPI to evaluate the graft prognosis. However KDPI is strongly correlated to age26. In line with our results, Dahmen et al. found that KDPI was higher that 90% when the donor age was over 70. Considering the kidney discard rates due to a high-KDPI in the US, we assume that most kidneys in the present study would have been discarded although Massie et al. showed a survival benefit in transplantations with high-KDPI kidney donors compared to patients remaining on the waiting list27. In the present study, recipients who received a kidney from an old donor without IRF had death-censored and death-uncensored 5-year survival graft rates of 79.1% and 70.2%, respectively, despite a KDPI at 96.7 ± 3.8. This confirms that such kidneys are worthy to be transplanted, if carefully selected, especially in older recipients.
The aim of our study was to provide easy tools to better assess the risk when using very-old kidney donors. The present results suggest that a peak serum creatinine level above 1.0 mg/dl could lead to better investigate the quality of the graft. In this context a pre-implantatory biopsy would help to assess the presence of acute tubular injuries or chronic lesions related to an underlying CKD, as suggested by the pre-implantatory Remuzzi score28, in order to refine acceptance and utilization of these kidneys (i.e. single or dual transplantation). Moreover this strategy can significantly reduce the discard rate without worsening the outcomes3,29. This is however dependent on high-quality standards to perform the biopsies and on dedicated analyses made by trained pathologists30,31. Considering only the donors presenting with peak serum creatinine above 1.0 mg/dl may rationalize resources and facilitate this strategy in routine practice. Other strategies to improve the prognosis of these very-old kidneys are the use of the perfusion machine and calcineurin inhibitor-free regimen. The use of hypothermic perfusion machine is indeed associated with better outcomes for ECD-recipients, both for the risk of DGF and graft loss32. However our data collection was not designed to study the effect of hypothermic perfusion machine. In the present study we did not find any association with graft survival in univariate analysis, although it seemed to be protective considering the risk of DGF (data not shown). Calcineurin inhibitor-free regimen may also be an alternative to improve long term results. Nevertheless, to date no study found a benefit of these strategies on graft survival33,34,35. Indeed the 7-year results of the BENEFIT-EXT clinical trial revealed better glomerular filtration rates in ECD-recipients36 but did not significantly reduce the graft loss rate.
This study carries several limitations. First, data were retrospectively collected, which conveys a risk of information loss. Data regarding the exposure and the definition of IRF may be partly biased. Indeed, oligo-anuria is determined and defined according to the French Registry, and the number of serum creatinine measurements per donor may influence the characterization of the donor status. Second, this is a small-sized single center cohort. Other variables, such as donor age, diabetes, hypertension, and others, may be not significant because of a lack of power. Recipients with IRF also presented more vascular comorbidities (background of stroke or peripheral arteritis) which worsen the long-term outcomes. Due to the sample size of the present study, we were not able to stratify on other variables, such as donor vascular comorbidities or cause of death, which would result in a very small number of events in each strata. Third, the European population included in the present study may significantly differs from the U.S population. Indeed, donor ethnicity could not be included in this analysis, due to French ethical issues37 and it seems likely that the proportion of African-Americans may affect post-transplantation outcomes in the U.S38. Ethnicity accounts for a significant part of the calculation of KDPI in the US system6, which might bias our conclusions. Thus, comparison regarding donors, discard rates and transplant outcomes in the US system and European countries should be interpreted with caution, and requires further investigation in wider cohorts. Ultimately, our results suggest that the peak serum creatinine could help to better assess the risk of graft failure in very-old donors where KDPI is systematically above 90%. Markers of kidney injuries (i.e. a peak SCr over 1 mg/dl and/or an oligo-anuria episode before organ procurement) should warn of the risk of poor transplantation outcomes. However, our findings cannot provide evidence to discard these grafts. First we did not assess the benefit to be transplanted with these marginal kidneys compared to stay longer on the waiting list, expecting another graft proposal. Second, we did not analyze the discarded kidneys characteristics. Thus our study does not intend to affect the decision-making process to accept or refuse these grafts. It only suggests that, in very old donors, KDPI does not provide a sufficient discrimination level to guide the physician’s choice.
To conclude, in the current context of organ shortage where very-old donors remain an important pool of kidneys, impaired renal function before kidney procurement could lead to histological evaluation in order to refine acceptance and allocation.
Patients and methods
Data source and ethical statement
This study was performed according to the Declaration of Helsinki and the Declaration of Istanbul. All data were collected from the CRISTAL database (French Biomedical Agency, which rules the allocation system in France) and from the recipients’ medical files. No organs were procured from prisoners. As the French Biomedical Agency regulates the allocation system in France, every organ was allocated by the Agency and transplanted in Lille, France (Centre Hospitalier Régional, Lille). Ethical committee was bypassed, according to French laws and the local institutional review board (Centre Hospitalier Régional Universitaire de Lille), as the study was monocentric and observational. Informed consent was obtained from all subjects. No subjects under 18 were involved in the study. Patients and laboratory data were analyzed anonymously and registered in respect with the French data protection registry (Commission Nationale de l’Informatique et des Libertés, i.e. CNIL), referenced #DEC16-235.
Study design
This is a retrospective monocentric study performed at the Lille University Hospital, France. All consecutive adult recipients who were transplanted between the 1st of January 2005 and the 31st of December 2015, with a kidney from deceased kidney donors older than 70 years were included. All of them received an induction therapy consisting in either basiliximab (20 mg at day 0 and day 4) for non-sensitized recipient older than 55 years or thymoglobulin (1.25 mg/kg from day 0 to day 3) for recipient younger than 55 years or presenting with HLA immunization. Maintenance immunosuppression associated tacrolimus, mycophenolate mofetil and steroids. Early steroid withdrawal (day 7) was performed in non-sensitized recipients. Valganciclovir was given during the first 6 months post transplantation in Cytomegalovirus (CMV) seronegative patients who received a CMV seropositive kidney. Prophylaxis for Pneumocystis jirovecii (trimethoprim-sulfamethoxazole) was given during the first 3–6 months post transplantation.
The following donors’ parameters were collected: age, sex, weight, height, HLA antigens, comorbidities (diabetes, hypertension, cardiovascular diseases, heart failure, and tobacco consumption), type of donor [brain deceased donor (DBD) or donor deceased after cardiac arrest (DCD)], cause of death, KDPI score, hemodynamic data (cardiac arrest, use of pressor amines) and renal function (urine output, serum creatinine, serum urea, and proteinuria) before organ procurement. Cold and warm ischemia times as well as the conservation modality (hypothermic perfusion machine (HPM) or static cold storage) were also registered.
The following recipients’ baseline parameters were collected: age, sex, weight, height, HLA antigens, comorbidities [diabetes, hypertension, coronary artery diseases, stroke, peripheral arteritis, arrhythmia, heart failure, tobacco consumption, chronic obstructive pulmonary disease (COPD), and cirrhosis], cause of end stage renal disease (ESRD), time on dialysis, time on waiting list, Charlson comorbidity index, dual kidney transplantation, previous transplantation, HLA sensitization. After transplantation, main complications (immediate post-transplantation hematoma, urinoma, or lymphocele, infections, and cardiovascular events), estimated glomerular filtration rate (eGFR using MDRD formula) at day 15, months 1, 3, 6, 12, and acute rejection episodes were registered. Delayed graft function (DGF) was defined as the need for dialysis during the first week post transplantation. Primary graft non-function (PGNF) was defined as failure of the graft to function the first 3 months after transplantation.
The KDPI score for each donor was retrospectively calculated using the OPTN calculator (https://optn.transplant.hrsa.gov/resources/allocation-calculators/kdpi-calculator/), except for ethnicity which is not available in the CRISTAL database.
Exposure
In order to avoid collinearity, donor variables “oligo-anuria” and “serum creatinine > 1.0 mg/dl” were tested separately in the univariate analysis and then pooled in one variable IRF in the multivariate analysis.
Donor IRF before procurement was defined as following:
-
a peak serum creatinine above 1.0 mg/dl. The threshold of 1.0 mg/dl represents the fourth quartile of serum creatinine peak in this very-old donor cohort.
-
and/or a transient episode of oligo-anuria in intensive care unit before the organ procurement defined by KDIGO stage I (< 0.5 ml/kg/h for 6 h), according to data available in the French CRISTAL Registry.
Statistical analysis
Qualitative variables were expressed in number and percentage. Quantitative variables were expressed in means and standard deviations or in median and interquartile according to their distribution estimated by the Shapiro–Wilk test.
Qualitative variables were compared by a chi-2 test. A student t-test or a Mann–Whitney test, when appropriate, was used to compare quantitative variables. Actuarial survivals were depicted with the Kaplan–Meier method and compared by the log-rank test. A Cox model was used to identify factors associated with graft survival, censored or not for death. All the variables with a p-value under 0.2 in univariate analysis were introduced in the multivariate models. Acute rejection and BK virus infection were analyzed as time dependent variables. A stepwise regression using a backward elimination was performed to obtain the final multivariate model.
For all tests a p-value < 0.05 was considered as significant. The statistical analysis was performed with R software (R Development Core Team (2008). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria).
References
Tullius, S. G. & Rabb, H. Improving the supply and quality of deceased-donor organs for transplantation. N. Engl. J. Med. 378, 1920–1929 (2018).
Agence de la Biomédecine 2015: Annual Data Report. https://www.agence-biomedecine.fr/annexes/bilan2015/accueil.htm. Accessed date: 30/07/2020.
Gandolfini, I. et al. The Kidney Donor Profile Index (KDPI) of marginal donors allocated by standardized pretransplant donor biopsy assessment: Distribution and association with graft outcomes: Biopsy-based allocation of high KDPI donors. Am. J. Transplant. 14, 2515–2525 (2014).
Aubert, O. et al. Disparities in acceptance of deceased donor kidneys between the United States and France and estimated effects of increased US acceptance. JAMA Intern. Med. 179, 1365 (2019).
Sung, R. S. et al. Impact of the expanded criteria donor allocation system on candidates for and recipients of expanded criteria donor kidneys. Transplantation 84, 1138–1144 (2007).
Rao, P. S. et al. A comprehensive risk quantification score for deceased donor kidneys: The Kidney Donor Risk Index. Transplantation 88, 231–236 (2009).
Lee, A. P. K. & Abramowicz, D. Is the Kidney Donor Risk Index a step forward in the assessment of deceased donor kidney quality?. Nephrol. Dial. Transplant. 30, 1285–1290 (2015).
Tanriover, B. et al. Kidneys at higher risk of discard: Expanding the role of dual kidney transplantation: Dual kidney transplantation in the United States. Am. J. Transplant. 14, 404–415 (2014).
Slegtenhorst, B. R. et al. Mechanisms and consequences of injury and repair in older organ transplants. Transplantation 97, 1091–1099 (2014).
Hall, I. E. et al. Deceased-donor acute kidney injury is not associated with kidney allograft failure. Kidney Int. 95, 199–209 (2019).
Acute Kidney Injury (AKI)—KDIGO. https://kdigo.org/guidelines/acute-kidney-injury/. Accessed date: 30/07/2020.
Zheng, Y.-T., Chen, C.-B., Yuan, X.-P. & Wang, C.-X. Impact of acute kidney injury in donors on renal graft survival: A systematic review and meta-analysis. Ren. Fail. 40, 649–656 (2018).
Chavalitdhamrong, D. et al. Patient and graft outcomes from deceased kidney donors age 70 years and older: An analysis of the organ procurement transplant network/united network of organ sharing database. Transplantation 85, 1573–1579 (2008).
Collini, A., Kalmar, P., Dhamo, A., Ruggieri, G. & Carmellini, M. Renal transplant from very old donors: How far can we go?. Transplantation 87, 1830–1836 (2009).
Foss, A. et al. Kidneys from deceased donors more than 75 years perform acceptably after transplantation. Transplantation 87, 1437–1441 (2009).
Gavela, E. et al. Renal allografts from donors older than 70 years are useful for single transplantation. Transplant. Proc. 41, 2047–2049 (2009).
Galeano, C. et al. Utilization of elderly kidney donors (>70 years) does not affect graft survival in the medium term. Transplant. Proc. 42, 3935–3937 (2010).
Gallinat, A. et al. Single-center experience with kidney transplantation using deceased donors older than 75 years. Transplantation 92, 76–81 (2011).
Machado, S. et al. Kidney transplantation using donors over 70 years old: Are the criteria for organ allocation too expanded?. Transplant. Proc. 44, 2289–2292 (2012).
Marconi, L. et al. Renal transplantation with donors older than 70 years: Does age matter?. Transplant. Proc. 45, 1251–1254 (2013).
Metzger, R. A. et al. Expanded criteria donors for kidney transplantation. Am. J. Transplant. 3, 114–125 (2003).
Lloveras, J., Arcos, E., Comas, J., Crespo, M. & Pascual, J. A paired survival analysis comparing hemodialysis and kidney transplantation from deceased elderly donors older than 65 years. Transplantation 99, 991–996 (2015).
Calvillo-Arbizu, J. et al. Predice el Kidney Donor Profile Index (KDPI) la supervivencia del injerto y del paciente en una población española?. Nefrologia 38, 587–595 (2018).
Arias-Cabrales, C. et al. Usefulness of the KDPI in Spain: A comparison with donor age and definition of standard/expanded criteria donor. Nefrologia 38, 503–513 (2018).
Lehner, L. J. et al. Assessment of the Kidney Donor Profile Index in a European cohort. Nephrol. Dial. Transplant. 33, 1465–1472 (2018).
Dahmen, M. et al. Validation of the Kidney Donor Profile Index (KDPI) to assess a deceased donor’s kidneys’ outcome in a European cohort. Sci. Rep. 9, 11234 (2019).
Massie, A. B. et al. Survival benefit of primary deceased donor transplantation with high-KDPI kidneys: Benefit of transplantation with high-KDPI kidneys. Am. J. Transplant. 14, 2310–2316 (2014).
Remuzzi, G. et al. Early experience with dual kidney transplantation in adults using expanded donor criteria. Double Kidney Transplant Group (DKG). J. Am. Soc. Nephrol. 10, 2591–2598 (1999).
Ruggenenti, P. et al. Long-term outcome of renal transplantation from octogenarian donors: A multicenter controlled study. Am. J. Transplant. 17, 3159–3171 (2017).
Sagasta, A. et al. Pre-implantation analysis of kidney biopsies from expanded criteria donors: Testing the accuracy of frozen section technique and the adequacy of their assessment by on-call pathologists. Transpl. Int. 29, 234–240 (2016).
Girolami, I. et al. Pre-implantation kidney biopsy: Value of the expertise in determining histological score and comparison with the whole organ on a series of discarded kidneys. J. Nephrol. 33, 167–176 (2020).
Gallinat, A. et al. Machine perfusion versus static cold storage in expanded criteria donor kidney transplantation: 3-year follow-up data. Transpl. Int. 26, E52–E53 (2013).
Andrés, A. et al. A randomized trial of basiliximab with three different patterns of cyclosporin A initiation in renal transplant from expanded criteria donors and at high risk of delayed graft function. Clin. Transplant. 23, 23–32 (2009).
Guba, M. et al. Calcineurin-inhibitor avoidance in elderly renal allograft recipients using ATG and basiliximab combined with mycophenolate mofetil. Transpl. Int. 21, 637–645 (2008).
Durrbach, A. et al. Prospective comparison of the use of sirolimus and cyclosporine in recipients of a kidney from an expanded criteria donor. Transplantation 85, 486–490 (2008).
Florman, S. et al. Efficacy and safety outcomes of extended criteria donor kidneys by subtype: Subgroup analysis of BENEFIT-EXT at 7 years after transplant. Am. J. Transplant. 17, 180–190 (2017).
INSEE. Ethnic-based statistics. (2016). https://www.insee.fr/en/information/2388586. Accessed date: 30/07/2020.
Newell, K. A. et al. Integrating APOL1 gene variants into renal transplantation: Considerations arising from the American society of transplantation expert conference. Am. J. Transplant. 17, 901–911 (2017).
Acknowledgements
We would like to thank Mr. Sébastien Gomis (CHU Lille, Data-Manager) for his help concerning the data-mining.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conception or design, or analysis and interpretation of data, or both: M.M., F.P., S.B., M.F., C.L., F.G., M.H. Drafting of the manuscript: M.M., F.P., R.L., V.F., M.H. Providing intellectual content of critical importance to the work described: M.M., F.P., A.L., M.H. Final approval of the version to be published: M.M., F.P., S.B., A.L., R.L., V.F., M.F., C.L., F.G., M.H. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maanaoui, M., Provôt, F., Bouyé, S. et al. Impaired renal function before kidney procurement has a deleterious impact on allograft survival in very old deceased kidney donors. Sci Rep 11, 12226 (2021). https://doi.org/10.1038/s41598-021-91843-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-91843-7
This article is cited by
-
Kidney transplantation from elderly donors (> 70 years): a systematic review
World Journal of Urology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.