Abstract
Degenerative aortic stenosis (AS) has become the most common valvular heart disease and the definitive treatment of symptomatic, severe AS is surgical valve replacement. In the absence of symptoms, the presence of left ventricular (LV) systolic dysfunction is pivotal in making treatment decisions for patients with AS. However, the LV ejection fraction is not a sensitive marker of global LV systolic function in the presence of LV hypertrophy, implying that asymptomatic patients with AS can have myocardial dysfunction with preserved LV ejection fraction. Abnormal myocardial mechanics might explain the pathophysiological processes underlying chronic pressure overload in AS. In this article, we review how new echocardiographic deformation parameters—such as myocardial strain, strain rate, and twist measurements—offer the potential for clinicians to monitor the course of LV dysfunction in patients with AS. Quantifying disturbances in LV function might provide insight into the timing of aortic valve replacement and into the improvement of LV systolic and diastolic properties through regression of LV hypertrophy and fibrosis after valve implantation.
Key Points
-
Assessment of left ventricular (LV) function has a pivotal role in clinical decision making for patients with severe aortic stenosis, particularly if they are asymptomatic
-
Conventional echocardiography indices such as LV ejection fraction, LV volumes, and fractional shortening are load-dependent and are not sensitive markers of global LV systolic function, especially in the setting of LV hypertrophy
-
Assessment of myocardial deformation parameters can provide better quantitation of regional and global systolic function, and might have increased sensitivity in detecting subtle myocardial dysfunction
-
Combining myocardial deformation parameters with conventional echocardiographic measurements might be useful for determining the timing of aortic valve replacement or for monitoring the improvement of LV systolic and diastolic properties after valve replacement
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Nkomo, V. T. et al. Burden of valvular heart diseases: a population-based study. Lancet 368, 1005–1011 (2006).
Iung, B. et al. A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur. Heart J. 24, 1231–1243 (2003).
American College of Cardiology/American Heart Association Task Force on Practice Guidelines et al. ACC/AHA guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): developed in collaboration with the Society of Cardiovascular Anesthesiologists: endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. Circulation 114, e84–e231 (2006).
Baumgartner, H. et al. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. J. Am. Soc. Echocardiogr. 22, 1–23 (2009).
Lang, R. M. et al. Recommendations for chamber quantification. Eur. J. Echocardiogr. 7, 79–108 (2006).
Hachicha, Z., Dumesnil, J. G., Bogaty, P. & Pibarot, P. Paradoxical low-flow, low-gradient severe aortic stenosis despite preserved ejection fraction is associated with higher afterload and reduced survival. Circulation 115, 2856–2864 (2007).
Amundsen, B. H. et al. Noninvasive myocardial strain measurement by speckle tracking echocardiography: validation against sonomicrometry and tagged magnetic resonance imaging. J. Am. Coll. Cardiol. 47, 789–793 (2006).
Villari, B. et al. Influence of collagen network on left ventricular systolic and diastolic function in aortic valve disease. J. Am. Coll. Cardiol. 22, 1477–1484 (1993).
Weidemann, F. et al. Impact of myocardial fibrosis in patients with symptomatic severe aortic stenosis. Circulation 120, 577–584 (2009).
Azevedo, C. F. et al. Prognostic significance of myocardial fibrosis quantification by histopathology and magnetic resonance imaging in patients with severe aortic valve disease. J. Am. Coll. Cardiol. 56, 278–287 (2010).
Monrad, E. S. et al. Time course of regression of left ventricular hypertrophy after aortic valve replacement. Circulation 77, 1345–1355 (1988).
Sandstede, J. J. et al. Changes in left and right ventricular cardiac function after valve replacement for aortic stenosis determined by cine MR imaging. J. Magn. Reson. Imaging 12, 240–246 (2000).
Di Bello, V. et al. Severe aortic stenosis and myocardial function: diagnostic and prognostic usefulness of ultrasonic integrated backscatter analysis. Circulation 110, 849–855 (2004).
Fijalkowski, M. et al. Improvement of ultrasonic myocardial properties after aortic valve replacement for pure severe aortic stenosis: the predictive value of ultrasonic tissue characterization for left ventricle reverse remodeling. J. Am. Soc. Echocardiogr. 23, 1060–1066 (2010).
Villari, B. et al. Normalization of diastolic dysfunction in aortic stenosis late after valve replacement. Circulation 91, 2353–2358 (1995).
Gjertsson, P., Caidahl, K. & Bech-Hanssen, O. Left ventricular diastolic dysfunction late after aortic valve replacement in patients with aortic stenosis. Am. J. Cardiol. 96, 722–727 (2005).
Monrad, E. S. et al. Abnormal exercise hemodynamics in patients with normal systolic function late after aortic valve replacement. Circulation 77, 613–624 (1988).
Krayenbuehl, H. P. et al. Left ventricular myocardial structure in aortic valve disease before, intermediate, and late after aortic valve replacement. Circulation 79, 744–755 (1989).
Brown, J., Shah, P., Stanton, T. & Marwick, T. H. Interaction and prognostic effects of left ventricular diastolic dysfunction and patient-prosthesis mismatch as determinants of outcome after isolated aortic valve replacement. Am. J. Cardiol. 104, 707–712 (2009).
Lund, O., Emmertsen, K., Dørup, I., Jensen, F. T. & Flø, C. Regression of left ventricular hypertrophy during 10 years after valve replacement for aortic stenosis is related to the preoperative risk profile. Eur. Heart J. 24, 1437–1446 (2003).
Bruch, C. et al. Tissue Doppler imaging in patients with moderate to severe aortic valve stenosis: clinical usefulness and diagnostic accuracy. Am. Heart J. 148, 696–702 (2004).
Kowalski, M. et al. One-dimensional ultrasonic strain and strain rate imaging: a new approach to the quantitation of regional myocardial function in patients with aortic stenosis. Ultrasound Med. Biol. 29, 1085–1092 (2003).
de Simone, G. et al. Assessment of left ventricular function by the midwall fractional shortening/end-systolic stress relation in human hypertension. J. Am. Coll. Cardiol. 23, 1444–1451 (1994).
Shimizu, G., Zile, M. R., Blaustein, A. S. & Gaasch, W. H. Left ventricular chamber filling and midwall fiber lengthening in patients with left ventricular hypertrophy: overestimation of fiber velocities by conventional midwall measurements. Circulation 71, 266–272 (1985).
Shimizu, G. et al. Left ventricular midwall mechanics in systemic arterial hypertension. Myocardial function is depressed in pressure-overload hypertrophy. Circulation 83, 1676–1684 (1991).
Cuspidi, C., Negri, F., Giudici, V., Sala, C. & Mancia, G. Impaired midwall mechanics and biventricular hypertrophy in essential hypertension. Blood Press. 19, 234–239 (2010).
Ballo, P., Mondillo, S., Motto, A. & Faraguti, S. A. Left ventricular midwall mechanics in subjects with aortic stenosis and normal systolic chamber function. J. Heart Valve Dis. 15, 639–650 (2006).
Mayet, J. et al. Improvement in midwall myocardial shortening with regression of left ventricular hypertrophy. Hypertension 36, 755–759 (2000).
Carroll, J. D. et al. Sex-associated differences in left ventricular function in aortic stenosis of the elderly. Circulation 86, 1099–1107 (1992).
Orsinelli, D. A., Aurigemma, G. P., Battista, S., Krendel, S. & Gaasch, W. H. Left ventricular hypertrophy and mortality after aortic valve replacement for aortic stenosis. A high risk subgroup identified by preoperative relative wall thickness. J. Am. Coll. Cardiol. 22, 1679–1683 (1993).
Gunther, S. & Grossman, W. Determinants of ventricular function in pressure-overload hypertrophy in man. Circulation 59, 679–688 (1979).
Ross, J. Jr Afterload mismatch and preload reserve: a conceptual framework for the analysis of ventricular function. Prog. Cardiovasc. Dis. 18, 255–264 (1976).
Huber, D., Grimm, J., Koch, R. & Krayenbuehl, H. P. Determinants of ejection performance in aortic stenosis. Circulation 64, 126–134 (1981).
Hachicha, Z., Dumesnil, J. G., Bogaty, P. & Pibarot, P. Paradoxical low-flow, low-gradient severe aortic stenosis despite preserved ejection fraction is associated with higher afterload and reduced survival. Circulation 115, 2856–2864 (2007).
Cramariuc, D. et al. Low-flow aortic stenosis in asymptomatic patients: valvular-arterial impedance and systolic function from the SEAS Substudy. JACC Cardiovasc. Imaging 2, 390–399 (2009).
Dumesnil, J. G., Pibarot, P. & Carabello, B. Paradoxical low flow and/or low gradient severe aortic stenosis despite preserved left ventricular ejection fraction: implications for diagnosis and treatment. Eur. Heart J. 31, 281–289 (2010).
Barasch, E. et al. Severe isolated aortic stenosis with normal left ventricular systolic function and low transvalvular gradients: pathophysiologic and prognostic insights. J. Heart Valve Dis. 17, 81–88 (2008).
Vinten-Johansen, J. & Weiss, H. R. Oxygen consumption in subepicardial and subendocardial regions of the canine left ventricle. The effect of experimental acute valvular aortic stenosis. Circ. Res. 46, 139–145 (1980).
Marcus, M. L., Doty, D. B., Hiratzka, L. F., Wright, C. B. & Eastham, C. L. Decreased coronary reserve: a mechanism for angina pectoris in patients with aortic stenosis and normal coronary arteries. N. Engl. J. Med. 307, 1362–1366 (1982).
Hein, S. et al. Progression from compensated hypertrophy to failure in the pressure-overloaded human heart: structural deterioration and compensatory mechanisms. Circulation 107, 984–991 (2003).
Zile, M. R. et al. Cardiocyte cytoskeleton in patients with left ventricular pressure overload hypertrophy. J. Am. Coll. Cardiol. 37, 1080–1084 (2001).
Takeda, S., Rimington, H., Smeeton, N. & Chambers, J. Long axis excursion in aortic stenosis. Heart 86, 52–56 (2001).
Van Pelt, N. C. et al. Longitudinal left ventricular contractile dysfunction after exercise in aortic stenosis. Heart 93, 732–738 (2007).
Donal, E. et al. Impact of aortic stenosis on longitudinal myocardial deformation during exercise. Eur. J. Echocardiogr. 12, 235–241 (2011).
Bauer, F. et al. Acute improvement in global and regional left ventricular systolic function after percutaneous heart valve implantation in patients with symptomatic aortic stenosis. Circulation 110, 1473–1476 (2004).
Becker, M. et al. Impact of left ventricular loading conditions on myocardial deformation parameters: analysis of early and late changes of myocardial deformation parameters after aortic valve replacement. J. Am. Soc. Echocardiogr. 20, 681–689 (2007).
Delgado, V. et al. Strain analysis in patients with severe aortic stenosis and preserved left ventricular ejection fraction undergoing surgical valve replacement. Eur. Heart J. 30, 3037–3047 (2009).
Carasso, S. et al. Differential effects of afterload on left ventricular long- and short-axis function: insights from a clinical model of patients with aortic valve stenosis undergoing aortic valve replacement. Am. Heart J. 158, 540–545 (2009).
Carasso, S. et al. Relation of myocardial mechanics in severe aortic stenosis to left ventricular ejection fraction and response to aortic valve replacement. Am. J. Cardiol. 102, 1052–1057 (2011).
Sengupta, P. P., Khandheria, B. K. & Narula, J. Twist and untwist mechanics of the left ventricle. Heart Fail. Clin. 4, 315–324 (2008).
Notomi, Y. et al. Enhanced ventricular untwisting during exercise: a mechanistic manifestation of elastic recoil described by Doppler tissue imaging. Circulation 113, 2524–2533 (2006).
Burns, A. T., La Gerche, A., Prior, D. L. & Macisaac, A. I. Left ventricular untwisting is an important determinant of early diastolic function. JACC Cardiovasc. Imaging 2, 709–716 (2009).
Geyer, H. et al. Assessment of myocardial mechanics using speckle tracking echocardiography: fundamentals and clinical applications. J. Am. Soc. Echocardiogr. 23, 351–369 (2010).
Stuber, M. et al. Alterations in the local myocardial motion pattern in patients suffering from pressure overload due to aortic stenosis. Circulation 100, 361–368 (1999).
Nagel, E. et al. Cardiac rotation and relaxation in patients with aortic valve stenosis. Eur. Heart J. 21, 582–589 (2000).
Biederman, R. W. et al. Physiologic compensation is supranormal in compensated aortic stenosis: does it return to normal after aortic valve replacement or is it blunted by coexistent coronary artery disease? An intramyocardial magnetic resonance imaging study. Circulation 112, 1429–1436 (2005).
Sandstede, J. J. et al. Cardiac systolic rotation and contraction before and after valve replacement for aortic stenosis: a myocardial tagging study using MR imaging. AJR Am. J. Roentgenol. 178, 953–958 (2002).
Van der Toorn, A. et al. Transmural gradients of cardiac myofiber shortening in aortic valve stenosis patients using MRI tagging. Am. J. Physiol. Heart Circ. Physiol. 283, H1609–H1615 (2002).
Laser, K. T. et al. Is torsion a suitable echocardiographic parameter to detect acute changes in left ventricular afterload in children? J. Am. Soc. Echocardiogr. 22, 1121–1128 (2009).
van Dalen, B. M. et al. Delayed left ventricular untwisting in hypertrophic cardiomyopathy. J. Am. Soc. Echocardiogr. 22, 1320–1326 (2009).
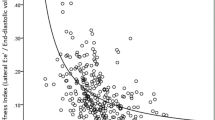
Popescu, B. A. et al. Left ventricular torsional dynamics in aortic stenosis: relationship between left ventricular untwisting and filling pressures. A two-dimensional speckle tracking study. Eur. J. Echocardiogr. 11, 406–413 (2010).
Tzemos, N., Silversides, C. K., Carasso, S., Rakowski, H. & Siu, S. C. Effect of pregnancy on left ventricular motion (twist) in women with aortic stenosis. Am. J. Cardiol. 101, 870–873 (2008).
Park, S. J. et al. Left ventricular torsion by two-dimensional speckle tracking echocardiography in patients with diastolic dysfunction and normal ejection fraction. J. Am. Soc. Echocardiogr. 21, 1129–1137 (2008).
Tan, Y. T. et al. The pathophysiology of heart failure with normal ejection fraction: exercise echocardiography reveals complex abnormalities of both systolic and diastolic ventricular function involving torsion, untwist, and longitudinal motion. J. Am. Coll. Cardiol. 54, 36–46 (2009).
Wang, J., Buergler, J. M., Veerasamy, K., Ashton, Y. P. & Nagueh, S. F. Delayed untwisting: the mechanistic link between dynamic obstruction and exercise tolerance in patients with hypertrophic obstructive cardiomyopathy. J. Am. Coll. Cardiol. 54, 1326–1334 (2009).
Cramariuc, D., Gerdts, E., Davidsen, E. S., Segadal, L. & Matre, K. Myocardial deformation in aortic valve stenosis: relation to left ventricular geometry. Heart 96, 106–112 (2009).
Rosenhek, R., Maurer, G. & Baumgartner, H. Should early elective surgery be performed in patients with severe but asymptomatic aortic stenosis? Eur. Heart J. 23, 1417–1421 (2002).
Brown, M. L. et al. The benefits of early valve replacement in asymptomatic patients with severe aortic stenosis. J. Thorac. Cardiovasc. Surg. 135, 308–315 (2008).
Rosenhek, R. et al. Natural history of very severe aortic stenosis. Circulation 121, 151–156 (2010).
Sun, J. P. et al. Noninvasive quantification of regional myocardial function using Doppler-derived velocity, displacement, strain rate, and strain in healthy volunteers: effects of aging. J. Am. Soc. Echocardiogr. 17, 132–138 (2004).
Giorgi, D. et al. Myocardial function in severe aortic stenosis before and after aortic valve replacement: a Doppler tissue imaging study. J. Am. Soc. Echocardiogr. 18, 8–14 (2005).
Iwahashi, N. et al. Acute improvement in myocardial function assessed by myocardial strain and strain rate after aortic valve replacement for aortic stenosis. J. Am. Soc. Echocardiogr. 19, 1238–1244 (2006).
Poulsen, S. H., Sogaard, P., Nielsen-Kudsk, J. E. & Egeblad, H. Recovery of left ventricular systolic longitudinal strain after valve replacement in aortic stenosis and relation to natriuretic peptides. J. Am. Soc. Echocardiogr. 20, 877–884 (2007).
Bauer, F. et al. Early improvement of left ventricular function after implantation of a transcutaneous aortic valve: a tissue Doppler ultrasound study. Arch. Cardiovasc. Dis. 102, 311–318 (2009).
Author information
Authors and Affiliations
Contributions
All authors contributed equally to the research of data and the writing of the article, provided substantial contributions to the discussion of content, and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Figures
Supplementary Figures 1–3 (PDF 738 kb)
Supplementary Video 1
Left-ventricular longitudinal strain analysis using transthoracic, two-dimensional speckle tracking echocardiography. The video shows an apical four chamber view of the heart during one cardiac cycle of a patient with aortic stenosis before aortic valve replacement. Segments of the myocardial wall are marked by dotted lines for segmental strain analysis. Red indicates myocardial shortening and blue indicates lengthening. In this patient, global left-ventricular longitudinal strain was quantified as 8.2%. See Supplementary Figure 1 for details on data analysis. (MOV 392 kb)
Supplementary Video 2
This video shows transthoracic, two-dimensional speckle tracking echocardiography performed 6 months after aortic valve replacement on the same patient as in Supplementary Video 1. Global left-ventricular longitudinal strain improved to 14%. Note the more dynamic contraction compared with the heart before aortic valve surgery. See Supplementary Figure 2 for details on data analysis. (MOV 299 kb)
Supplementary Video 3
Parasternal short axis view from the apical level of the left ventricle. Apical rotation of the heart is visualized by transthoracic echocardiography. Note the counterclockwise rotation throughout systole. (MOV 203 kb)
Supplementary Video 4
Rotational motion of the heart apex. Two-dimensional speckle tracking software was applied to Supplementary Video 3 for quantification of deformation parameters. Segments of the myocardial wall are highlighted by dotted lines. The color-coded image demonstrates systolic counterclockwise rotation (blue) and clockwise diastolic rotation (red). See also Supplementary Figure 3a. (MOV 299 kb)
Supplementary Video 5
Parasternal short axis view of left ventricle at the level of the mitral valve as seen by transthoracic echocardiography. Note the clockwise rotation of the left ventricle during systole. (MOV 171 kb)
Supplementary Video 6
Rotational motion of the heart at the level of the mitral valve. Two-dimensional speckle tracking software was applied to Supplementary Video 5. Segments of the myocardial wall are highlighted by dotted lines. The color-coded image demonstrates diastolic counterclockwise rotation (blue) and systolic clockwise rotation (red). See also Supplementary Figure 3b. (MOV 414 kb)
Rights and permissions
About this article
Cite this article
Ozkan, A., Kapadia, S., Tuzcu, M. et al. Assessment of left ventricular function in aortic stenosis. Nat Rev Cardiol 8, 494–501 (2011). https://doi.org/10.1038/nrcardio.2011.80
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2011.80
This article is cited by
-
Mechanical Stimuli for Left Ventricular Growth During Pressure Overload
Experimental Mechanics (2021)
-
Left atrial dysfunction as a determinant of pulmonary hypertension in patients with severe aortic stenosis and preserved left ventricular ejection fraction
The International Journal of Cardiovascular Imaging (2017)
-
Sleep-disordered breathing and severe aortic stenosis
Somnologie (2017)
-
Cardiovascular magnetic resonance evaluation of symptomatic severe aortic stenosis: association of circumferential myocardial strain and mortality
Journal of Cardiovascular Magnetic Resonance (2016)
-
Calcific aortic stenosis
Nature Reviews Disease Primers (2016)