Abstract
Objective:
To determine if the choice of enteral feeds after gastroschisis repair relates to the time to achieve full feeds and time to discharge.
Study Design:
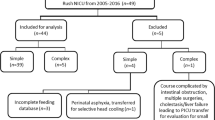
A retrospective study of infants with gastroschisis from 2000 to 2010 examined demographics, days at closure, days at initiation of feeds, days to full feeds, time to discharge and length of stay.
Result:
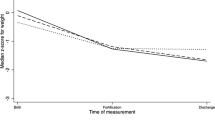
Ninety infants were identified, 22 received (human milk) HM exclusively, 15 were fed >50% HM, 16 were fed <50% HM and 26 were fed only cow milk-based formulas. Infants fed exclusively HM had significantly shorter times to full enteral feedings (median 5 days versus 7 days, P=0.03). The time from initiation of feedings to hospital discharge, which accounts for initiation age, significantly favored the exclusively HM-fed infants (median 7 days versus 10 days, P=0.01).
Conclusion:
Exclusive HM feeding after gastroschisis repair decreases time to achieve full enteral feeds and time to discharge.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Holland AJA, Walker K, Badawi N . Gastroschisis: an update. Pediatr Surg Int 2010; 26: 871–878.
Collins SR, Griffin MR, Arbogast PG, Walsh WF, Rush MR, Carter BS et al. The rising prevalence of gastroschisis and omphalocele in Tennessee. J Pediatr Surg 2007; 42: 1221–1224.
Vu LT, Nobuhara KK, Laurent C, Shaw GM . Increasing prevalence of gastroschisis: population-based study in California. J Pediatr 2008; 152: 807–811.
Laughon M, Meyer R, Bose C, Wall A, Otero E, Heerens A et al. Rising birth prevalence of gastroschisis. J Perinatol 2003; 23: 291–293.
Alvarez SM, Burd RS . Increasing prevalence of gastroschisis repairs in the United States: 1996-2003. J Pediatr Surg 2007; 42: 943–946.
Christensen RD, Henry E, Wiedmeier SE, Burnett J, Lambert DK . Identifying patients, on the first day of life, at high-risk of developing parenteral nutrition-associated liver disease. J Perinatol 2007; 27: 284–290.
Walter-Nicolet E, Rousseau V, Kieffer F, Fusaro F, Bourdaud N, Oucherif S et al. Neonatal outcome of gastroschisis is mainly influenced by nutritional management. J Pediatr Gastr Nutr 2009; 48: 612–617.
Sharp M, Bulsara M, Gollow I, Pemberton P . Gastroschisis: early enteral feeds may improve outcomes. J Paediatr Child Health 2000; 36: 472–476.
Jayanthi S, Seymour P, Puntis JWL, Stringer MD . Necrotizing enterocolitis after gastroschisis repair: a preventable complication? J Pediatr Surg 1998; 33: 705–707.
Williams CA, Hauser KW, Correia JA, Frias JL . Ascertainment of gastroschisis using the ICD-9-CM surgical procedure code. Birth Defects Res A Clin Mol Teratol 2005; 73: 646–648.
Molik KA, Gingalewski CA, West KW, Rescorla FJ, Scherer LR, Engum SA et al. Gastroschisis: a plea for risk categorization. J Pediatr Surg 2001; 36: 51–55.
Arnold MA, Chang DC, Nabaweesi R, Colombani PM, Bathurst MA, Mon KS et al. Risk stratification of 4344 patients with gastroschisis into simple and complex categories. J Pediatr Surg 2007; 42: 1520–1525.
Lao OB, Larison C, Garrison MM, Waldhausen JHT, Goldin AB . Outcomes in neonates with gastroschisis in U.S. children’s hospitals. Am J Perinatol 2010; 27: 97–102.
Samanta S, Farrer K, Breathnach A, Heath PT . Risk factors for late onset gram-negative infections: a case-control study. Arch Dis Child Fetal Neonatal Ed 2011; 96: F15–F18.
Langer JC, Longaker MT, Crombleholme TM, Bond SJ, Finkbeiner WE, Rudolph CA et al. Etiology of intestinal damage in gastroschisis. I: Effects of amniotic fluid exposure and bowel constriction in a fetal lamb model. J Pediatr Surg 1989; 24: 992–997.
Shulman RJ, Schanler RJ, Lau C, Heitkemper M, Ou CN, Smith EO . Early feeding, antenatal glucocorticoids, and human milk decrease intestinal permeability in preterm infants. Pediatr Res 1998; 44: 519–523.
Shulman RJ, Schanler RJ, Lau C, Heitkemper M, Ou CN, Smith EO . Early feeding, feeding tolerance, and lactase activity in preterm infants. J Pediatr 1998; 133: 645–649.
Sisk PM, Lovelady CA, Gruber KJ, Dillard RG, O’Shea TM . Human milk consumption and full enteral feeding among infants who weigh≤1250 grams. Pediatrics 2008; 121: e1528–e1533.
Taylor SN, Basile LA, Ebeling M, Wagner CL . Intestinal permeability in preterm infants by feeding type: mother's milk versus formula. Breastfeed Med 2009; 4: 11–15.
Oldham KT, Coran AG, Drongowski RA, Baker PJ, Wesley JR, Polley TZ . The development of necrotizing enterocolitis following repair of gastroschisis: a surprisingly high incidence. J Pediatr Surg 1988; 23: 945–949.
Marchbank T, Weaver G, Nilsen-Hamilton M, Playford RJ . Pancreatic secretory trypsin inhibitor is a major motogenic and protective factor in human breast milk. Am J Physiol Gastrointest Liver Physiol 2009; 296: 697–703.
Rautava S, Nanthakumar NN, Dubert-Ferrandon A, Lu L, Rautava J, Walker WA . TGF-beta2 induces maturation of immature human intestinal epithelial cells and inhibits inflammatory cytokine responses induced via the NF-kappaB pathway. J Pediatr Gastroenterol Nutr 2012; 54: 630–638.
Sydorak RM, Nijagal A, Sbragia L, Hirose S, Tsao RH, Phibbs RH et al. Gastroschisis: small hole, big cost. J Pediatr Surg 2002; 37: 1669–1672.
Acknowledgements
We would like to acknowledge the support and encouragement of this study by the late chairman of the Department of Pediatrics, Donald W Lewis, MD.
Disclaimer
There was no external funding or source of support for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kohler, J., Perkins, A. & Bass, W. Human milk versus formula after gastroschisis repair: effects on time to full feeds and time to discharge. J Perinatol 33, 627–630 (2013). https://doi.org/10.1038/jp.2013.27
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2013.27
Keywords
This article is cited by
-
How much does a liter of donor human milk cost? Cost analysis of operating a human milk bank in Italy
International Breastfeeding Journal (2022)
-
Prevalence and patterns of gestational parent’s own milk feeds among infants with major congenital surgical anomalies in the NICU
Journal of Perinatology (2021)
-
Mother’s own milk dose is associated with decreased time from initiation of feedings to discharge and length of stay in infants with gastroschisis
Journal of Perinatology (2020)
-
The experience of breastfeeding infants affected by congenital diaphragmatic hernia or esophageal atresia
Italian Journal of Pediatrics (2018)
-
Winging it: maternal perspectives and experiences of breastfeeding newborns with complex congenital surgical anomalies
Journal of Perinatology (2018)