Abstract
Objective
To evaluate the hypothesis that implementation of a preoperative standardized feeding protocol increases human milk use in infants with complex congenital heart disease (CHD).
Study design
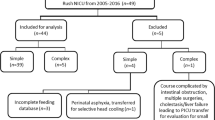
Single-center, quasi-experimental study of infants with complex CHD. A cohort of 546 infants pre protocol was compared to 55 patients post protocol. Feeding regimen and peri-operative outcomes information were collected.
Result
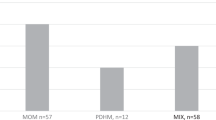
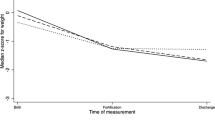
Human milk use increased significantly (58.4% versus 100%, p < 0.01) and there was no formula use post protocol (18.7% versus 0%, p < 0.01). Preoperative necrotizing enterocolitis occurred in 18/546 (3.3%) infants pre protocol versus 1/55 (1.8%) post protocol, p = 1.00. Days to full feeds and length of hospital stay in both cohorts were not significantly different.
Conclusion
Successful implementation of a preoperative standardized feeding protocol can increase human milk and decrease formula use in infants with complex CHD without significant adverse outcomes. A larger study is needed to evaluate the association of human milk use with peri-operative outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Hair AB, Peluso AM, Hawthorne KM, Perez J, Smith DP, Khan JY, et al. Beyond necrotizing enterocolitis prevention: improving outcomes with an exclusive human milk-based diet. Breastfeed Med. 2016;11:70–4.
Cortez J, Makker K, Kraemer DF, Neu J, Sharma R, Hudak ML. Maternal milk feedings reduce sepsis, necrotizing enterocolitis and improve outcomes of premature infants. J Perinatol. 2018;38:71–4.
Meier PP. Human milk and clinical outcomes in preterm infants. Nestle Nutr Inst Workshop Ser. 2019;90:163–74. https://doi.org/10.1159/000490304.
Ballard O, Morrow AL. Human milk composition: nutrients and bioactive factors. Pediatr Clin North Am. 2013;60:49–74.
Lin PW, Stoll BJ. Necrotising enterocolitis. Lancet. 2006;368:1271–83.
Seigel JK, Smith PB, Ashley PL, Cotten CM, Herbert CC, King BA, et al. Early administration of oropharyngeal colostrum to extremely low birth weight infants. Breastfeed Med. 2013;8:491–5.
Gephart SM, Weller M. Colostrum as oral immune therapy to promote neonatal health. Adv Neonatal Care. 2014;14:44–51.
Lee J, Kim HS, Jung YH, Choi KY, Shin SH, Kim EK, et al. Oropharyngeal colostrum administration in extremely premature infants: an RCT. Pediatrics. 2015;135:357–66.
Sohn K, Kalanetra KM, Mills DA, Underwood MA. Buccal administration of human colostrum: impact on the oral microbiota of premature infants. J Perinatol. 2016;36:106–11.
Luce W, Schwartz R, Beauseau W, Giannone P, Hashiguchi B, Cheatham JP, et al. Gastrointestinal morbidity for the hybrid approach to hypoplastic left heart syndrome [abstract]. Cardiol Young. 2009;19:147–8.
Scahill CJ, Graham EM, Atz AM, Bradley SM, Kavarana MN, Zyblewski SC. Preoperative feeding neonates with cardiac disease. World J Pediatr Congenit Heart Surg. 2017;8:62–8.
Mukherjee D, Zhang Y, Chang DC, Vricella LA, Brenner JI, Abdullah F. Outcomes analysis of necrotizing enterocolitis within 11 958 neonates undergoing cardiac surgical procedures. Arch Surg. 2010;145:389–92.
Howley LW, Kaufman J, Wymore E, Thureen P, Magouirk JK, McNair B, et al. Enteral feeding in neonates with prostaglandin-dependent congenital cardiac disease: international survey on current trends and variations in practice. Cardiol Young. 2012;22:121–7.
Natarajan G, Reddy Anne S, Aggarwal S. Enteral feeding of neonates with congenital heart disease. Neonatology. 2010;98:330–6.
McElhinney DB, Hedrick HL, Bush DM, Pereira GR, Stafford PW, Gaynor JW, et al. Necrotizing enterocolitis in neonates with congenital heart disease: risk factors and outcomes. Pediatrics. 2000;106:1080–7.
Willis L, Thureen P, Kaufman J, Wymore E, Skillman H, da Cruz E. Enteral feeding in prostaglandin-dependent neonates: is it a safe practice? J Pediatr. 2008;153:867–9.
Toms R, Jackson KW, Dabal RJ, Reebals CH, Alten JA. Preoperative trophic feeds in neonates with hypoplastic left heart syndrome. Congenit Heart Dis. 2015;10:36–42.
Day TG, Dionisio D, Zannino D, Brizard C, Cheung MMH. Enteral feeding in duct-dependent congenital heart disease. J Neonatal Perinat Med. 2019;12:9–12.
Cognata A, Kataria-Hale J, Griffiths P, Maskatia S, Rios D, O’Donnell A, et al. Human milk use in the preoperative period is associated with a lower risk for necrotizing enterocolitis in neonates with complex congenital heart disease. J Pediatr. 2019;215:11–6.
Petrillo-Albarano T, Pettignano R, Asfaw M, Easley K. Use of a feeding protocol to improve nutritional support through early, aggressive, enteral nutrition in the pediatric intensive care unit. Pediatr Crit Care Med. 2006;7:340–4.
Barr J, Hecht M, Flavin KE, Khorana A, Gould MK. Outcomes in critically ill patients before and after the implementation of an evidence-based nutritional management protocol. Chest. 2004;125:1446–57.
del Castillo SL, McMulley ME, Khemani RG, Jeffries HE, Thomas DW, Peregrine J, et al. Reducing the incidence of necrotizing enterocolitis in neonates with hypoplastic left heart syndrome with the introduction of an enteral feed protocol. Pediatr Crit Care Med. 2010;11:373–7.
Gephart SM, Hanson CK. Preventing necrotizing enterocolitis with standardized feeding protocols: not only possible, but imperative. Adv Neonatal Care. 2013;13:48–54.
Patole SK, de Klerk N. Impact of standardised feeding regiments on incidence of neonatal necrotising enterocolitis: a systematic review and meta-analysis of observational studies. Arch Dis Child Fetal Neonatal Ed. 2005;90:F147–51.
Rodriguez NA, Groer MW, Zeller JM, Engstrom JL, Fogg L, Du H, et al. A randomized controlled trial of the oropharyngeal administration of mother’s colostrum to extremely low birth weight infants in the first days of life. Neonatal Intensive Care. 2011;24:31–5.
Glass KM, Greecher CP, Doheny KK. Oropharyngeal administration of colostrum increases salivary secretory IgA levels in very low-birth-weight infants. Am J Perinatol. 2017;34:1389–95.
Moreno-Fernandez J, Sanchez-Martinez B, Serrano-Lopez L, Martin-Alvarez E, Diaz Castro J, Pena-Caballero M, et al. Enhancement of immune response mediated by oropharyngeal colostrum administration in preterm neonates. Pediatr Allergy Immunol. 2019;30:234–41.
Aijia M, Yang J, Li Y, Zhang X, Kang Y Oropharyngeal colostrum therapy reduces the incidence of ventilator-associated pneumonia in very low birth weight infants: a systematic review and meta-analysis. Pediatr Res. 2020. https://doi.org/10.1038/s41390-020-0854-1.
Kantorowska A, Wei JC, Cohen RS, Lawrence RA, Gould JB, Lee HC. Impact of donor milk availability on breast milk use and necrotizing enterocolitis rates. Pediatrics. 2016;137:e20153123.
Tshamala D, Pelecanos, Davis MW. Factors associated with infants receiving their mother’s own breast milk on discharge from hospital in a unit where pasteurized donor human milk is available. J Paediatr Child Health. 2018;54:1016–22.
Siano E, Lauriti G, Ceccanti S, Zani A. Cardiogenic necrotizing enterocolitis: a clinically distinct entity from classical necrotizing enterocolitis. Eur J Pediatr Surg. 2019;29:14–22.
Carlo WF, Kimball TR, Michelfelder EC, Border WL. Persistent diastolic flow reversal in abdominal aortic Doppler-flow profiles is associated with an increased risk of necrotizing enterocolitis in term infants with congenital heart disease. Pediatrics. 2007;119:330–5.
Becker KC, Hornik CP, Cotten CM, Clark RH, Hill KD, Smith PB, et al. Necrotizing enterocolitis in infants with ductal-dependent congenital heart disease. Am J Perinatol. 2015;32:633–8.
Kataria-Hale J, Osborne SW, Hair A, Hagan J, Pammi M. Preoperative feeds in ductal-dependent cardiac disease: a systematic review and meta-analysis. Hosp Pediatr. 2019;9:998–1006.
Underwood MA. Human milk for the premature infant. Pediatr Clin North Am. 2013;1:189–207.
Wang Y, Hoenig JD, Malin KJ, Qamar S, Petrof EO, Sun J, et al. 16S rRNA gene-based analysis of fecal microbiota from preterm infants with and without necrotizing enterocolitis. ISME J. 2009;3:944–54.
Mai V, Young CM, Ukhanova M, Warng X, Sun Y, Casella G, et al. Fecal microbiota in premature infants prior to necrotizing enterocolitis. PLoS One. 2011;6:e20647.
Ford SL, Lohmann P, Preidis GA, Gordon PS, O’Donnell A, Hagan J, et al. Improved feeding tolerance and growth are linked to increased gut microbial community diversity in very-low-birth-weight infants fed mother’s own milk compared with donor breast milk. Am J Clin Nutr. 2019;109:1088–97.
Meinzen-Derr J, Poindexter B, Wrage L, Morrow AL, Stoll B, Donovan EF. Role of human milk in extremely low birth weight infants’ risk of necrotizing enterocolitis or death. J Perinatol. 2009;29:57–62.
Funding
Evie Whitlock Grant—Texas Children’s Hospital.
Author information
Authors and Affiliations
Contributions
JK-H: conceptualized and designed the study, collected the data, drafted the initial manuscript, and approved the final manuscript as submitted. DJR: contributed to the study design, reviewed and revised the manuscript and approved the final manuscript as submitted. AC: contributed to the study design, collected the data, reviewed and revised the manuscript and approved the final manuscript as submitted. PH: contributed to the study design, collected the data, reviewed and revised the manuscript and approved the final manuscript as submitted. JZ: contributed to the study design, collected the data, reviewed and revised the manuscript and approved the final manuscript as submitted. PS: contributed to the study design, reviewed and revised the manuscript and approved the final manuscript as submitted. KT: contributed to the study design, reviewed and revised the manuscript and approved the final manuscript as submitted. NH: contributed to the study design, reviewed and revised the manuscript and approved the final manuscript as submitted. JH: carried out the statistical analyses, reviewed and revised the manuscript and approved the final manuscript as submitted. AH: mentored the primary author in study design, supervised data collection, and critically reviewed the manuscript and approved the manuscript as submitted. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Kataria-Hale, J., Roddy, D.J., Cognata, A. et al. A preoperative standardized feeding protocol improves human milk use in infants with complex congenital heart disease. J Perinatol 41, 590–597 (2021). https://doi.org/10.1038/s41372-021-00928-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-021-00928-8
This article is cited by
-
Relationship Between Human Milk Feeding Patterns and Growth in the First Year of Life in Infants with Congenital Heart Defects
Pediatric Cardiology (2023)
-
Prevalence and patterns of gestational parent’s own milk feeds among infants with major congenital surgical anomalies in the NICU
Journal of Perinatology (2021)