Abstract
The human ubiquitin protein ligase E3C (UBE3C) regulates airway inflammatory responses and is hypothesized to be associated with the presence of nasal polyps in asthma-related diseases. A total of 24 UBE3C single-nucleotide polymorphisms (SNPs) were genotyped in a 467 Korean asthma cohort that was stratified into more homogenous phenotypes of 114 aspirin-exacerbated respiratory disease subgroup and 353 aspirin-tolerant asthma (ATA) subjects. Association analysis revealed that 16 UBE3C SNPs were significantly associated with presence of nasal polyps in the overall asthma group (P=0.0008 and Pcorr=0.01; odds ratio (OR)=0.60). The strength of association from 10 polymorphisms was increased in the ATA subgroup (P=0.0002 and Pcorr=0.003; OR=0.49). In addition, UBE3C_ht1 was found to be consistently associated with nasal polyps in the overall asthmatics group (P=0.006) and the ATA phenotype (P=0.002; Pcorr=0.02) via a codominant mechanism. Our findings provide evidence that variations in UBE3C are potent genetic markers of nasal polyps development in Korean asthmatics and may contribute novel insights into the clinical relevance and potential involvement of UBE3C in respiratory deficiencies.
Similar content being viewed by others
Introduction
Nasal polyps are benign growth, which develop from chronic inflammation of the lateral wall of the nose and sinuses.1, 2 Prevalence estimates of nasal polyps have been reported to be around 7–15% in aspirin-tolerant asthma (ATA)3 and 31–60% in aspirin-exacerbated respiratory disease (AERD),4 a condition that is characterized by bronchial obstruction, nasal polyposis and aspirin hypersensitivity.
The homologous to the E6-AP carboxyl terminus-type ubiquitin protein ligase E3C (UBE3C) gene is crucial in the development and differentiation of lymphocytes, activation of T-cell tolerance, antigen presentation and immune invasion.5 In the protein proteolytic pathway, UBE3C assembles polyubiquitin chain by binding to E2 ubiquitin-conjugating enzyme and transferring activated ubiquitin moieties to Lys48 of the previously conjugated ubiquitin molecule.6 The ubiquitin-proteasome pathway facilitates activation of nuclear transcription factor κB,7, 8 an important regulator of a large number of cellular processes, including inflammatory responses in airways.9, 10, 11 Furthermore, evidence of association between UBE3C polymorphisms and AERD have been revealed previously.12
This case–control analysis was carried out to investigate the association of UBE3C gene variations with presence of nasal polyps in Korean asthma patients.
Materials and methods
Study patients
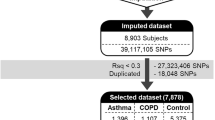
A total of 467 asthma patients were recruited from Korean hospitals affiliated with the Asthma Genome Research Center. Evaluation of asthma and tests measuring total immunoglobulin E, atopy and reaction to inhalant allergens were carried out as described previously.13, 14 Nasal polyposis was diagnosed based on the presence of endoscopically visible polyps arising from the middle nasal meatus.
The patients were stratified further into 114 AERD (composed of 66 polyp-positive cases and 48 polyp-negative controls) and 353 ATA subgroups (composed of 92 polyp-positive cases and 261 polyp-negative controls) based on the individual reaction to aspirin challenge that was performed according to previous methods.13 Aspirin-induced FEV1 decline (polyp-positive=12.22 vs polyp-negative=6.78) and positive history of aspirin intolerance (polyp-positive=41.77 vs polyp-negative=15.53) were significantly different between cases and controls (P<0.0001; Table 1). The protocols were approved by the institutional review board of the each hospital, and the study subjects provided written informed consent.
Genotyping of single-nucleotide polymorphisms and statistical analysis
Selection of single-nucleotide polymorphisms (SNPs), genotyping and statistical analyses were performed according to previous methods.13 Differences in the frequency distribution of UBE3C variations were analyzed using logistic models controlling for age, sex, smoking status and atopy, including AERD status in the analysis of the overall asthma patients.
Results and Discussion
Twenty-four UBE3C SNPs were successfully genotyped and showed a tight LD block in 467 asthma patients, similar to previous results.12 Three major haplotypes with frequencies over 0.05 were then included in the association analyses.
Logistic analysis in the overall asthmatics revealed that 21 SNPs achieved significance (P=0.0008–0.009; odds ratio (OR)=0.60–0.67; Table 2). The association signals of 16 SNPs remained robust (Pcorr=0.01–0.05; Table 1) even after multiple testing corrections. Among the tested haplotypes, UBE3C_ht1 and UBE3C_ht2 were found to be nominally associated with nasal polyps development in asthmatics (P=0.006 and 0.009, respectively, Pcorr>0.05; Table 2).
To further characterize the association signals, more homogeneous asthma phenotypes composed of AERD and ATA subgroups were analyzed. Results of logistic analysis between the presence of nasal polyps in ATA patients and UBE3C polymorphisms revealed significant association signals for 10 SNPs even after multiple testing corrections (P=0.0002–0.01; Pcorr=0.003–0.009; OR=0.49–0.54; Table 3). Although UBE3C_ht1 and UBE3C_ht2 were initially associated with nasal polyposis in ATA patients (P=0.002 and 0.006, respectively, Table 3), only UBE3C_ht1 maintained significance under the strict criteria after multiple testing corrections (Pcorr=0.02; Table 3). Furthermore, although several variants in UBE3C were previously identified to be risk factors of AERD,12 only nominal evidence of association were observed between UBE3C polymorphisms and nasal polyposis among AERD patients in the current study (P=0.04–0.05; Pcorr>0.05; Table 3), suggesting that the tested genetic variants may not affect polyp development in aspirin-hypersensitive asthmatics. The inconsistencies between the findings can be attributed to differences in the mechanisms underlying deficiencies of the upper and lower airways. In addition, although nasal polyps often co-occur with AERD, estimates of the prevalence of nasal polyposis are around 4% in the general population, suggesting that unidentified by-pathway and/or complex modulations might be involved in the generation of nasal polyps in AERD patients.
To determine whether rs10949635G>T in the promoter region could be a putative binding site for regulators, we conducted in silico analysis using the Signal Scan program.15 However, the results failed to identify transcriptional regulators binding to the variant. In silico analysis using the EMBL-EBI splice site prediction was also performed to estimate the function of SNPs in intronic regions of UBE3C. None of the tested intronic SNPs, however, were predicted to be potential branch point sites for alternative splicing. Furthermore, using the microRNA database,16 we failed to detect any microRNA sequences within the UBE3C that could potentially repress gene translation.
The current study is limited by the exclusion of non-asthmatic controls with nasal polyps. Furthermore, after performing power calculations of single associations, we observed a 66.5% average statistical power to detect the effect sizes associated with the significant SNPs in all asthma subjects (Table 2). Although results from power calculations indicate insufficient sample size, a similar trend in the allelic frequencies of the analyzed UBE3C variants was observed in Asian populations including Korean after comparing data from various ethnic groups using information from the International HapMap database (data not shown). In order to address these limitations and validate the findings, further replications using larger sample scales are required.
The current study shows for the first time that UBE3C is an important genetic marker for onset of nasal polyposis in asthma patients. This finding may provide useful insights on the pathogenic mechanisms of nasal polyps development among asthmatics and directing future researches of disease etiology.
References
Bernstein, J. M. & Kansal, R. Superantigen hypothesis for the early development of chronic hyperplastic sinusitis with massive nasal polyposis. Curr. Opin. Otolaryngol. Head Neck Surg. 13, 39–44 (2005).
Kakoi, H. & Hiraide, F. A histological study of formation and growth of nasal polyps. Acta Otolaryngol. 103, 137–144 (1987).
Larsen, K. The clinical relationship of nasal polyps to asthma. Allergy Asthma Proc. 17, 243–249 (1996).
Szczeklik, A., Nizankowska, E. & Duplaga, M. Natural history of aspirin-induced asthma. AIANE Investigators. European Network on Aspirin-Induced Asthma. Eur. Respir. J. 16, 432–436 (2000).
Hershko, A. & Ciechanover, A. The ubiquitin system. Annu. Rev. Biochem. 67, 425–479 (1998).
Ciechanover, A. The ubiquitin-proteasome proteolytic pathway. Cell 79, 13–21 (1994).
Palombella, V. J., Rando, O. J., Goldberg, A. L. & Maniatis, T. The ubiquitin-proteasome pathway is required for processing the NF-kappa B1 precursor protein and the activation of NF-kappa B. Cell 78, 773–785 (1994).
Chen, Z., Hagler, J., Palombella, V. J., Melandri, F., Scherer, D., Ballard, D. et al. Signal-induced site-specific phosphorylation targets I kappa B alpha to the ubiquitin-proteasome pathway. Genes Dev. 9, 1586–1597 (1995).
Picado, C., Bioque, G., Roca-Ferrer, J., Pujols, L., Mullol, J., Benitez, P. et al. Nuclear factor-kappaB activity is down-regulated in nasal polyps from aspirin-sensitive asthmatics. Allergy 58, 122–126 (2003).
Takeno, S., Hirakawa, K., Ueda, T., Furukido, K., Osada, R. & Yajin, K. Nuclear factor-kappa B activation in the nasal polyp epithelium: relationship to local cytokine gene expression. Laryngoscope 112, 53–58 (2002).
Ward, C. L., Omura, S. & Kopito, R. R. Degradation of CFTR by the ubiquitin-proteasome pathway. Cell 83, 121–127 (1995).
Lee, J. S., Kim, J. H., Bae, J. S., Kim, J. Y., Park, T. J., Pasaje, C. F. et al. Association analysis of UBE3C polymorphisms in Korean aspirin-intolerant asthmatic patients. Ann. Allergy Asthma Immunol. 105, 307–312 (2010).
Pasaje, C. F., Bae, J. S., Park, B. L., Jang, A. S., Uh, S. T., Kim, M. K. et al. Association analysis of DTD1 gene variations with aspirin-intolerance in asthmatics. Int. J. Mol. Med. 28, 129–137 (2011).
Crapo, R. O., Casaburi, R., Coates, A. L., Enright, P. L., Hankinson, J. L., Irvin, C. G. et al. Guidelines for methacholine and exercise challenge testing-1999. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. Am. J. Respir. Crit. Care Med. 161, 309–329 (2000).
Prestridge, D. S. SIGNAL SCAN: a computer program that scans DNA sequences for eukaryotic transcriptional elements. Comput. Appl. Biosci. 7, 203–206 (1991).
Ambros, V., Bartel, B., Bartel, D. P., Burge, C. B., Carrington, J. C., Chen, X. et al. A uniform system for microRNA annotation. RNA 9, 277–279 (2003).
Acknowledgements
This work was supported by Grant Number M1-0302-00-0073 from the Korea Science and Engineering Foundation funded by the Korean government (Ministry of Education, Science and Technology; No. 2009-0080157), a Priority Research Centers Program through the NRF funded by the MEST (2009-0093822) and grant from the Korea Health 21 R&D Project (A010249).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Pasaje, C., Kim, JH., Park, BL. et al. UBE3C genetic variations as potent markers of nasal polyps in Korean asthma patients. J Hum Genet 56, 797–800 (2011). https://doi.org/10.1038/jhg.2011.104
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2011.104