Abstract
Background/Objective:
Rapid postnatal weight gain is a potentially modifiable risk factor for obesity and metabolic syndrome. To identify markers of rapid infancy weight gain and childhood obesity, we analyzed the metabolome in cord blood from infants differing in their postnatal weight trajectories.
Methods:
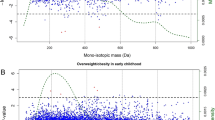
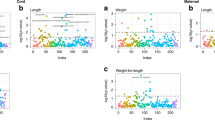
We performed a nested case–control study within Project Viva, a longitudinal cohort of mothers and children. We selected cases (n=26) based on top quartile of change in weight-for-age 0–6 months and body mass index (BMI) >85th percentile in mid-childhood (median 7.7 years). Controls (n=26) were age and sex matched, had normal postnatal weight gain (2nd or 3rd quartile of change in weight-for-age 0–6 months) and normal mid-childhood weight (BMI 25th–75th percentile). Cord blood metabolites were measured using untargeted liquid chromatography–mass spectrometry; individual metabolites and pathways differing between cases and controls were compared in categorical analyses. We adjusted metabolites for maternal age, maternal BMI and breastfeeding duration (linear regression), and assessed whether metabolites improved the ability to predict case–control status (logistic regression).
Results:
Of 415 detected metabolites, 16 were altered in cases versus controls (t-test, nominal P<0.05). Three metabolites were related to tryptophan: serotonin, tryptophan betaine and tryptophyl leucine (46%, 48% and 26% lower in cases, respectively, P<0.05). Mean levels of two methyl donors, dimethylglycine and N-acetylmethionine, were also lower in cases (18% and 16%, respectively, P=0.01). Moreover, the glutamine:glutamate ratio was reduced by 33% (P<0.05) in cases. Levels of serotonin, tryptophyl leucine and N-acetylmethionine remained significantly different after adjustment for maternal BMI, age and breastfeeding. Adding metabolite levels to logistic regression models including only clinical covariates improved the ability to predict case versus control status.
Conclusions:
Several cord blood metabolites are associated with rapid postnatal weight gain. Whether these patterns are causally linked to childhood obesity is not clear from this cross-sectional analysis, but will require further study.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Barker DJ, Osmond C, Forsen TJ, Kajantie E, Eriksson JG . Trajectories of growth among children who have coronary events as adults. N Engl J Med 2005; 353: 1802–1809.
Leunissen RW, Kerkhof GF, Stijnen T, Hokken-Koelega A . Timing and tempo of first-year rapid growth in relation to cardiovascular and metabolic risk profile in early adulthood. JAMA 2009; 301: 2234–2242.
Taveras EM, Rifas-Shiman SL, Belfort MB, Kleinman KP, Oken E, Gillman MW . Weight status in the first 6 months of life and obesity at 3 years of age. Pediatrics 2009; 123: 1177–1183.
Isganaitis E, Jimenez-Chillaron J, Woo M, Chow A, Decoste J, Vokes M et al. Accelerated postnatal growth increases lipogenic gene expression and adipocyte size in low-birth weight mice. Diabetes 2009; 58: 1192–1200.
Jimenez-Chillaron JC, Hernandez-Valencia M, Lightner A, Faucette RR, Reamer C, Przybyla R et al. Reductions in caloric intake and early postnatal growth prevent glucose intolerance and obesity associated with low birthweight. Diabetologia 2006; 49: 1974–1984.
Michaliszyn SF, Sjaarda LA, Mihalik SJ, Lee S, Bacha F, Chace DH et al. Metabolomic profiling of amino acids and beta-cell function relative to insulin sensitivity in youth. J Clin Endocrinol Metab 2012; 97: E2119–E2124.
Wang TJ, Larson MG, Vasan RS, Cheng S, Rhee EP, McCabe E et al. Metabolite profiles and the risk of developing diabetes. Nat Med 2011; 17: 448–453.
Ivorra C, Garcia-Vicent C, Chaves FJ, Monleon D, Morales JM, Lurbe E . Metabolomic profiling in blood from umbilical cords of low birth weight newborns. J Transl Med 2012; 10: 142.
La TD, Seppanen-Laakso T, Larsson HE, Hyotylainen T, Ivarsson SA, Lernmark A et al. Decreased cord-blood phospholipids in young age-at-onset type 1 diabetes. Diabetes 2013; 62: 3951–3956.
Oken E, Baccarelli AA, Gold DR, Kleinman KP, Litonjua AA, De MD et al. Cohort profile: Project Viva. Int J Epidemiol 2014; 44: 37–48.
Shin SY, Fauman EB, Petersen AK, Krumsiek J, Santos R, Huang J et al. An atlas of genetic influences on human blood metabolites. Nat Genet 2014; 46: 543–550.
Gall WE, Beebe K, Lawton KA, Adam KP, Mitchell MW, Nakhle PJ et al. alpha-hydroxybutyrate is an early biomarker of insulin resistance and glucose intolerance in a nondiabetic population. PLoS One 2010; 5: e10883.
Storey JD, Tibshirani R . Statistical significance for genomewide studies. Proc Natl Acad Sci USA 2003; 100: 9440–9445.
Xia J, Psychogios N, Young N, Wishart DS . MetaboAnalyst: a web server for metabolomic data analysis and interpretation. Nucleic Acids Res 2009; 37: W652–W660.
Cheng S, Rhee EP, Larson MG, Lewis GD, McCabe EL, Shen D et al. Metabolite profiling identifies pathways associated with metabolic risk in humans. Cirulation 2012; 125: 2222–2231.
Lewis GD, Wei R, Liu E, Yang E, Shi X, Martinovic M et al. Metabolite profiling of blood from individuals undergoing planned myocardial infarction reveals early markers of myocardial injury. J Clin Invest 2008; 118: 3503–3512.
Mihalik SJ, Michaliszyn SF, de las HJ, Bacha F, Lee S, Chace DH et al. Metabolomic profiling of fatty acid and amino acid metabolism in youth with obesity and type 2 diabetes: evidence for enhanced mitochondrial oxidation. Diabetes Care 2012; 35: 605–611.
McCormack SE, Shaham O, McCarthy MA, Deik AA, Wang TJ, Gerszten RE et al. Circulating branched-chain amino acid concentrations are associated with obesity and future insulin resistance in children and adolescents. Pediatr Obes 2012; 8: 52–61.
Tea I, Le GG, Kuster A, Guignard N, Alexandre-Gouabau MC, Darmaun D et al. 1H-NMR-based metabolic profiling of maternal and umbilical cord blood indicates altered materno-foetal nutrient exchange in preterm infants. PLoS One 2012; 7: e29947.
Walsh BH, Broadhurst DI, Mandal R, Wishart DS, Boylan GB, Kenny LC et al. The metabolomic profile of umbilical cord blood in neonatal hypoxic ischaemic encephalopathy. PLoS One 2012; 7: e50520.
Servillo L, Giovane A, Balestrieri ML, Ferrari G, Cautela D, Castaldo D . Occurrence of pipecolic acid and pipecolic acid betaine (homostachydrine) in Citrus genus plants. J Agric Food Chem 2012; 60: 315–321.
Guertin KA, Moore SC, Sampson JN, Huang WY, Xiao Q, Stolzenberg-Solomon RZ et al. Metabolomics in nutritional epidemiology: identifying metabolites associated with diet and quantifying their potential to uncover diet-disease relations in populations. Am J Clin Nutr 2014; 100: 208–217.
Deguchi T, Kouno Y, Terasaki T, Takadate A, Otagiri M . Differential contributions of rOat1 (Slc22a6) and rOat3 (Slc22a8) to the in vivo renal uptake of uremic toxins in rats. Pharm Res 2005; 22: 619–627.
Prentice KJ, Luu L, Allister EM, Liu Y, Jun LS, Sloop KW et al. The furan fatty acid metabolite CMPF is elevated in diabetes and induces beta cell dysfunction. Cell Metab 2014; 19: 653–666.
Murrin C, Shrivastava A, Kelleher CC . Maternal macronutrient intake during pregnancy and 5 years postpartum and associations with child weight status aged five. Eur J Clin Nutr 2013; 67: 670–679.
Heisler LK, Jobst EE, Sutton GM, Zhou L, Borok E, Thornton-Jones Z et al. Serotonin reciprocally regulates melanocortin neurons to modulate food intake. Neuron 2006; 51: 239–249.
Ozawa M, Honda K, Nakai I, Kishida A, Ohsaki A . Hypaphorine an indole alkaloid from Erythrina velutina, induced sleep on normal mice. Bioorg Med Chem Lett 2008; 18: 3992–3994.
Keller BO, Wu BT, Li SS, Monga V, Innis SM . Hypaphorine is present in human milk in association with consumption of legumes. J Agric Food Chem 2013; 61: 7654–7660.
Crane JD, Palanivel R, Mottillo EP, Bujak AL, Wang H, Ford RJ et al. Inhibiting peripheral serotonin synthesis reduces obesity and metabolic dysfunction by promoting brown adipose tissue thermogenesis. Nat Med 2014; 21: 166–172.
Ohara-Imaizumi M, Kim H, Yoshida M, Fujiwara T, Aoyagi K, Toyofuku Y et al. Serotonin regulates glucose-stimulated insulin secretion from pancreatic beta cells during pregnancy. Proc Natl Acad Sci USA 2013; 110: 19420–19425.
Zhu X, Song J, Mar MH, Edwards LJ, Zeisel SH . Phosphatidylethanolamine N-methyltransferase (PEMT) knockout mice have hepatic steatosis and abnormal hepatic choline metabolite concentrations despite ingesting a recommended dietary intake of choline. Biochem J 2003; 370: 987–993.
Alexandre-Gouabau MC, Courant F, Moyon T, Kuster A, Le GG, Tea I et al. Maternal and cord blood LC-HRMS metabolomics reveal alterations in energy and polyamine metabolism, and oxidative stress in very-low birth weight infants. J Proteome Res 2013; 12: 2764–2778.
Askanazi J, Carpentier YA, Michelsen CB, Elwyn DH, Furst P, Kantrowitz LR et al. Muscle and plasma amino acids following injury. Influence of intercurrent infection. Ann Surg 1980; 192: 78–85.
Qi L, Qi Q, Prudente S, Mendonca C, Andreozzi F, di PN et al. Association between a genetic variant related to glutamic acid metabolism and coronary heart disease in individuals with type 2 diabetes. JAMA 2013; 310: 821–828.
Acknowledgements
We gratefully acknowledge the support of the Joslin Bioinformatics Core, funded by Diabetes Research Center grant DK036836. Grant support was provided by K99/R00 (HD064793), the Pediatric Endocrine Society, the Canadian Institutes of Health Research and the Graetz Foundation (to EI); by K24 HD069408 (to EO) and by the American Diabetes Association and the Graetz Foundation (to M-EP).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
WG formerly had a professional relationship with Metabolon, Inc., where he was employed as Program Manager for Diagnostic Development, and where the metabolomic analyses reported in this article were performed. All other authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Rights and permissions
About this article
Cite this article
Isganaitis, E., Rifas-Shiman, S., Oken, E. et al. Associations of cord blood metabolites with early childhood obesity risk. Int J Obes 39, 1041–1048 (2015). https://doi.org/10.1038/ijo.2015.39
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2015.39
This article is cited by
-
Early ascending growth is associated with maternal lipoprotein profile during mid and late pregnancy and in cord blood
International Journal of Obesity (2023)
-
Cord blood metabolic signatures predictive of childhood overweight and rapid growth
International Journal of Obesity (2021)
-
Developmental Programming of Body Composition: Update on Evidence and Mechanisms
Current Diabetes Reports (2019)
-
Integrating -Omics Approaches into Human Population-Based Studies of Prenatal and Early-Life Exposures
Current Environmental Health Reports (2018)
-
Chemical Similarity Enrichment Analysis (ChemRICH) as alternative to biochemical pathway mapping for metabolomic datasets
Scientific Reports (2017)