Abstract
Objectives:
To analyse the relationship between body mass index (BMI) in middle-age and disability status in old-age using data from the Melbourne Collaborative Cohort Study (MCCS).
Methods:
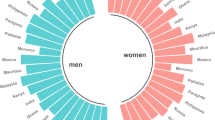
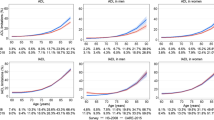
A total of 41 514 participants enroled in the MCCS between 1990–1994. Height and weight were measured at baseline and disability, defined as limitations to self-care activities of daily living (ADLs) and self-care plus mobility activities, was identified at follow-up (2003–2007). In all, 6300 participants were <65 years at baseline, ⩾70 years at follow-up and not missing BMI at baseline or ADLs at follow-up. The association between BMI in six categories (BMI 18.5–22.5; 22.5–25; 25–27.5; 27.5–30; 30–35; 35+) and disability status was analysed using logistic regression. Models were stratified by sex, and sequentially adjusted for age, education, country of birth, then smoking, alcohol, fruit and vegetable intake, and physical activity.
Results:
Adjusted odds ratios for composite self-care ADL and mobility limitations compared with BMI 18.5–22.5 kg m−2 were 1.73 (95%CI 1.14–2.64) for BMI 30–35 kg m−2 and 3.46 (1.78–6.73) for BMI 35+ kg m−2 in males. In females, adjusted odds ratios were 1.29 (1.00–1.68) for BMI 22.5–25 kg m−2, 1.74 (1.35–2.24) for BMI 25–27.5 kg m−2, 2.58 (1.98–3.36) for BMI 27.5–30 kg m−2, 2.74 (2.10–3.58) for BMI 30–35 kg m−2 and 4.21 (3.12–5.88) for BMI 35+ kg m−2.
Conclusion:
A graded relationship was observed between BMI and disability in males and females, across the continuum of BMI. These results highlight the importance of a healthy body weight at middle age in order to reduce the risk of disability in old age.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
World Health OrganisationHealth topics: Disabilities, 2010.
de Bruin A, Picavet HS, Nosikov A . Health Interview Surveys: towards international harmonization of methods and instruments. WHO Reg Publ Eur Ser 1996; 58: i–161.
Vincent HK, Vincent KR, Lamb KM . Obesity and mobility disability in the older adult. Obes Rev 2010; 11: 568–579.
Backholer K, Wong E, Freak-Poli R, Walls HL, Peeters A . Increasing body weight and risk of limitations in activities of daily living: a systematic review and meta-analysis. Obes Rev 2012; 13: 456–468.
Rejeski WJ, Marsh AP, Chmelo E, Rejeski JJ . Obesity, intentional weight loss and physical disability in older adults. Obes Rev 2010; 11: 671–685.
Prentice AM, Jebb SA . Beyond body mass index. Obes Rev. 2001; 2: 141–147.
Stevens J . Impact of age on associations between weight and mortality. Nutr Rev 2000; 58: 129–137.
Vasconcelos Fde A, Cordeiro BA, Rech CR, Petroski EL . Sensitivity and specificity of the body mass index for the diagnosis of overweight/obesity in elderly. Cad Saude Publica 2010; 26: 1519–1527.
Anstey KJ, Cherbuin N, Budge M, Young J . Body mass index in midlife and late-life as a risk factor for dementia: a meta-analysis of prospective studies. Obes Rev 2011; 12: e426–e437.
Ebrahim S, Wannamethee SG, Whincup P, Walker M, Shaper AG . Locomotor disability in a cohort of British men: the impact of lifestyle and disease. Int J Epidemiol 2000; 29: 478–486.
Stenholm S, Sainio P, Rantanen T, Koskinen S, Jula A, Heliovaara M et al. High body mass index and physical impairments as predictors of walking limitation 22 years later in adult Finns. J Gerontol A Biol Sci Med Sci 2007; 62: 859–865.
Launer LJ, Harris T, Rumpel C, Madans J . Body mass index, weight change, and risk of mobility disability in middle-aged and older women. The epidemiologic follow-up study of NHANES I. JAMA 1994; 271: 1093–1098.
Houston DK, Stevens J, Cai J . Abdominal fat distribution and functional limitations and disability in a biracial cohort: the Atherosclerosis Risk in Communities Study. Int J Obes (Lond) 2005; 29: 1457–1463.
Peeters A, Bonneux L, Nusselder WJ, De Laet C, Barendregt JJ . Adult obesity and the burden of disability throughout life. Obes Res 2004; 12: 1145–1151.
Giles GG, English DR . The Melbourne Collaborative Cohort Study. IARC Sci Publ: Melbourne, 2002; 156: 69–70.
World Health OrganisationObesity. Preventing and managing the global epidemic. Geneva: World Health Organisation, 1998, 3–5 June 1997.
Hodge A, Patterson AJ, Brown WJ, Ireland P, Giles G . The Anti Cancer Council of Victoria FFQ: relative validity of nutrient intakes compared with weighed food records in young to middle-aged women in a study of iron supplementation. Aust NZ J Public Health 2000; 24: 576–583.
National Health and Medical Research Council. Food for HealthDietary Guidelines for All Australians. National Health and Medical Research Council: Canberra, Australia, 2003.
National Health and Medical Research CouncilAustralian Alcohol Guidelines: Health Risks and Benefits. National Health and Medical Research Council: Canberra, Australia, 2011.
MacInnis RJ, English DR, Hopper JL, Haydon AM, Gertig DM, Giles GG . Body size and composition and colon cancer risk in men. Cancer Epidemiol Biomarkers Prev 2004; 13: 553–559.
Busetto L, Romanato G, Zambon S, Calo E, Zanoni S, Corti MC et al. The effects of weight changes after middle age on the rate of disability in an elderly population sample. J Am Geriatr Soc 2009; 57: 1015–1021.
Alley DE, Chang VW . The changing relationship of obesity and disability, 1988-2004. JAMA 2007; 298: 2020–2027.
Sun Q, Townsend MK, Okereke OI, Franco OH, Hu FB, Grodstein F . Adiposity and weight change in mid-life in relation to healthy survival after age 70 in women: prospective cohort study. BMJ 2009; 339: b3796.
Chen H, Bermudez OI, Tucker KL . Waist circumference and weight change are associated with disability among elderly Hispanics. J Gerontol A Biol Sci Med Sci 2002; 57: M19–M25.
Larrieu S, Peres K, Letenneur L, Berr C, Dartigues JF, Ritchie K et al. Relationship between body mass index and different domains of disability in older persons: the 3C study. Int J Obes Relat Metab Disord 2004; 28: 1555–1560.
Wu CH, Yao WJ, Lu FH, Yang YC, Wu JS, Chang CJ . Sex differences of body fat distribution and cardiovascular dysmetabolic factors in old age. Age Ageing 2001; 30: 331–336.
Leveille SG, Penninx BW, Melzer D, Izmirlian G, Guralnik JM . Sex differences in the prevalence of mobility disability in old age: the dynamics of incidence, recovery, and mortality. J Gerontol B Psychol Sci Soc Sci 2000; 55: S41–S50.
Wray LA, Blaum CS . Explaining the role of sex on disability: a population-based study. Gerontologist 2001; 41: 499–510.
Majer IM, Nusselder WJ, Mackenbach JP, Kunst AE . Life expectancy and life expectancy with disability of normal weight, overweight, and obese smokers and nonsmokers in Europe. Obesity (Silver Spring) 2011; 19: 1451–1459.
Acknowledgements
AP was supported by the VicHealth fellowship, EW was supported by the Monash University Australian Postgraduate Award and CS was supported by the National Health and Medical Research (Grant No. 465130). AH supported by NHMRC No. 520316. We thank the Melbourne Collaborative Cohort Study investigators and participants, and Damien Jolley for assistance with graph presentation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Backholer, K., Pasupathi, K., Wong, E. et al. The relationship between body mass index prior to old age and disability in old age. Int J Obes 36, 1180–1186 (2012). https://doi.org/10.1038/ijo.2012.99
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2012.99
Keywords
This article is cited by
-
Diet and physical activity as possible mediators of the association between educational attainment and body mass index gain among Australian adults
International Journal of Public Health (2018)
-
Association between adiposity and disability in the Lc65+ cohort
The Journal of nutrition, health and aging (2017)
-
Midlife job profiles and disabilities in later life: a 28-year follow-up of municipal employees in Finland
International Archives of Occupational and Environmental Health (2016)
-
The mediating role of dietary factors and leisure time physical activity on socioeconomic inequalities in body mass index among Australian adults
BMC Public Health (2013)
-
Obesity in the elderly: an emerging health issue
International Journal of Obesity (2012)