Abstract
Chronic kidney disease (CKD), characterized by senile inflammation, is a risk factor for cardiovascular disease. Conduit artery function and small artery structure relate to cardiovascular disease. We examined the correlations, determinants and interrelationships of arterial indices in association with CKD in a cross-sectional study of 139 patients (60% male; mean age 44 years) with CKD (stages 3–5, 39%) who underwent a renal biopsy. Conduit artery function and small artery sclerosis were assessed by brachial artery flow-mediated dilatation (FMD) and semiquantitative evaluation of small artery intimal thickening (SA-IT), respectively. The estimated glomerular filtration rate correlated with FMD (r=0.31, P=0.0002) and inversely correlated with SA-IT (r=−0.54, P<0.0001). Multiple regression analysis showed that FMD was inversely correlated with SA-IT and vice versa. In addition, high-sensitivity C-reactive protein (hs-CRP) was significantly correlated with SA-IT, but not FMD. Multiple logistic analysis revealed that higher hs-CRP concomitant with decreased FMD was further associated with the risk of severe SA-IT compared with their individual effects. These findings suggest that both conduit artery and small artery disease develop with mutual interaction in parallel with decreased kidney function. Coexistence of inflammation and conduit artery dysfunction may be closely related to renal small artery sclerosis in patients with CKD.
Similar content being viewed by others
Introduction
The risk of cardiovascular disease (CVD) and end-stage renal disease increases with progression of chronic kidney disease (CKD).1, 2, 3 Endothelial dysfunction is an early step in the progression to atherosclerosis that precedes structural vessel changes.4 Accumulating evidence has demonstrated that endothelial dysfunction in large conduit arteries (that is, brachial) can predict CVD in the general population5 as well as among elderly individuals6 and patients with hypertension7 and established atherosclerosis.8, 9 Moreover, endothelial dysfunction has been implicated as a major pathophysiological mechanism responsible for the CKD-associated risk of CVD.10, 11 Although brachial artery flow-mediated dilatation (FMD) is frequently used as a tool for the assessment of endothelial function, it reportedly reflects both endothelial-dependent and endothelial-independent vascular function in patients with cardiovascular risk burdens.12 In CKD patients whose conditions are often complicated by various cardiovascular risk factors, decreased FMD is reportedly associated with carotid intima–media thickness13 and an increased risk of CVD.11
In the past decade, many studies have shown that small artery disease also has a predictive value for CVD. Structural changes in the vascular wall of small arteries in the retina and abdominal subcutaneous fat can predict future CVD in patients with hypertension.14, 15, 16, 17 In addition, previous studies suggested a link between conduit artery disease and small artery disease in patients with hypertension.18, 19 However, it is not clear whether large conduit artery function and small artery structural changes in target organs develop in parallel with CKD progression and whether they mutually correlate with independent risk factors for arteriosclerosis. Moreover, a link between inflammation and both indices of vascular disease is unknown, although inflammation is suggested to be involved in the mechanism of CKD-associated CVD.11
In the present study, we conducted a retrospective cross-sectional review to examine whether large conduit artery dysfunction assessed by FMD and renal small artery sclerosis advanced in parallel with a decrease in the estimated glomerular filtration rate (eGFR) and identify their determinants in CKD patients who had undergone a renal biopsy. We further examined the interrelationship among indices of large and small vascular disease.
Methods
Study participants
A total of 172 consecutive patients with CKD who underwent renal biopsy at University of the Ryukyus Hospital between 1 June 2010 and 31 March 2013 were considered for this study. We routinely examined FMD as a vascular function from 1 June 2010. Both conduit artery function and small artery structural change are proposed to be confounded by primary diseases such as systemic vasculitis and amyloidosis and some drugs such as calcineurin inhibitors. Therefore, we excluded 33 patients because of treatment with steroids (n=16) and/or calcineurin inhibitors (n=6), vasculitis (n=2), amyloidosis (n=3), purpura nephritis (n=1), a transplanted kidney (n=1) and the absence of a small artery specimen (n=1). Data from the remaining 139 patients (84 men and 55 women) were analyzed in this study. The study protocol was approved by the ethics review board of University of the Ryukyus. All patients gave informed consent to participate in the study.
Histological diagnoses based on renal biopsy specimens
On the basis of renal biopsy findings, the following diagnoses were made for the 139 study participants: immunoglobulin A nephropathy (n=84), membranous nephropathy (n=11), minor glomerular abnormalities (n=4), focal segmental glomerular sclerosis (n=1), membranoproliferative glomerulonephritis (n=2), nonimmunoglobulin A mesangial proliferative glomerulonephritis (n=7), benign nephrosclerosis (n=12), lupus nephritis (n=1), diabetic nephropathy (n=6), tubulointerstitial nephritis (n=2) and other miscellaneous diseases (n=9).
Semiquantitative assessment of renal small arteries
We studied renal small arteries, including the large interlobular artery, with more than three layers of smooth muscle cells and a lumen diameter of ∼200–300 μm and the arcuate arteries of the kidney. The wall/lumen ratio of the small artery, which is often used as an index of small vessel disease,14, 15, 20 is difficult to apply to renal biopsy specimens because it is not commonly available in the tangential view. Intrarenal arteriosclerosis with intimal thickening is often complicated in patients with hypertension21 and in elderly patients.22 Intimal thickening has been shown to be an early morphological change preceding atherosclerosis in humans.23, 24 Therefore, we examined the degree of intimal thickening compared with the thickness of the adjacent medial wall. Specifically, we semiquantitatively assessed intimal thickening in the small arteries of each specimen using the following grading system: grade 0 (G0), no thickening; grade 1 (G1), intimal thickening of less than half the adjusted medial thickness; grade 2 (G2), intimal thickening of more than half and/or less than the adjusted medial thickness; and grade 3 (G3), intimal thickening of more than the adjusted medial thickness. On the basis of this grading system, we calculated the mean grade of intimal thickening in the small renal arteries (small artery intimal thickening (SA-IT) index) in each patient according to the following formula: arteriolar wall thickening index=(n0 × 0+n1 × 1+n2 × 2+n3 × 3)/N.
The representative microphotographs of each graded SA-IT are shown in Figure 1. All histologic analyses were performed by one physician (KK) who was blinded to patient information.
Representative microphotographs of small artery intimal thickening (grades 0–3). Masson’s trichrome staining (magnification: grades 0, 2 and 3, × 400; grade 1, × 200). Small artery intimal thickening was semiquantitatively assessed as follows: grade 0 (G0), no thickening; grade 1 (G1), mild thickening; grade 2 (G2), moderate thickening without definite narrowing of the lumen; and grade 3 (G3), severe thickening with definite narrowing of the lumen. A full color version of this figure is available at Hypertension Research online.
Assessment of brachial artery vascular function
We routinely examined FMD as a vascular function from 1 June 2010. Subjects underwent noninvasive assessment of FMD to evaluate endothelial function using a standardized procedure.21, 25 We measured FMD in the morning before renal biopsy. All patients were requested to fast for at least 10 h, abstain from smoking and the consumption of alcohol and caffeine and withhold all medications. They were asked to rest in a quiet, dark, air-conditioned, temperature-controlled room (23–26 °C) for at least 15 min in a supine position before the examination. Ultrasound equipment and a high-resolution linear array transducer coupled to computer-assisted analysis software provided one longitudinal and two short-axis images using 10 MHz H-type probe (UNEXEF18G, UNEX, Nagoya, Japan). It was used to scan the brachial artery in B-mode 5 to 10 cm above the right elbow. When the clearest B-mode image of the intima–media complex was obtained, the transducer was held at the same point throughout the scan by a stereotactic probe holder. FMD was measured by the A-mode waves as a signal of the intima–media complex that was synchronized with the electrocardiographic R-waves and tracked automatically. After measuring baseline brachial artery diameter, we compressed the brachial artery (at least 50 mm Hg above systolic blood pressure) for 5 min using a blood pressure cuff placed around the forearm. After compression, maximum brachial artery diameter was measured after cuff release for 3 min.
The reproducibility of the FMD measurements using this system and the correlation coefficient between the data of two visits was reported to be 0.86, with a coefficient of variance of 11.2%.26 We also assessed FMD measurement in 7 control subjects who were all healthy volunteers (28–38 years old, 57% male). We examined the first FMD and second FMD in 1 day with 2 h interval using this system. Pearson’s correlation coefficient of the FMD between first FMD and second FMD was 0.93 (P<0.005), and the coefficient of variation was 17.4%. The mean value of the FMD in the control subjects was 7.1%, similar to those of general population aged 20–40 years.27
FMD was expressed as follows: (maximum brachial artery diameter after cuff release−baseline brachial artery diameter)/baseline brachial artery diameter × 100. This dilating rate is referred to as the percentage FMD (%), an evaluation index for the vascular function of the brachial artery. All FMD examinations were performed by one experienced physician (TM).
Laboratory procedures and definition of comorbid conditions
Fasting blood samples were used to measure the serum levels of total cholesterol, high-density lipoprotein and low-density lipoprotein (LDL) cholesterol, triglycerides, uric acid, creatinine, high-sensitivity C-reactive protein (hs-CRP), hemoglobin A1c (HbA1c) and glucose. Urinary protein was measured in first spot morning urine samples. Blood and urine samples were collected on the day before FMD measurement. Diabetes mellitus was determined by fasting and postprandial glucose and HbA1c levels in addition to a medical history of diabetes. Dyslipidemia was defined as hyper LDL cholesterolemia and/or hypertriglyceridemia and/or hypo high-density lipoprotein cholesterolemia and/or the use of medications for dyslipidemia. Hyperuricemia was defined as uric acid ⩾7 mg dl−1 among men and uric acid ⩾6 mg dl−1 among women and/or the use of medications for hyperuricemia. Ever smokers were defined as current or ex-smokers. The eGFR was calculated using a new equation for Japanese individuals: eGFR (ml min−1 per 1.73 m2)=194 × serum creatinine1.094 × age0.287 ( × 0.739 if female).28 We estimated eGFR in 7 patients aged <18 years using the Schwartz formula.29
Patient characteristics
Lifestyle information (that is, smoking habits), anthropometric parameters and medication information, including the use of antihypertensive drugs, statins, antidiabetic drugs and antiuricemic drugs, were obtained from medical records.
Statistical analyses
Continuous measures, categorical measures and ordered categorical measures were analyzed using analysis of variance, χ2 tests and Kruskal–Wallis tests, respectively. Multivariate regression analysis was performed to identify independent predictors of either FMD or SA-IT. Some medications, including antihypertensive drugs, statins and antiuricemic drugs; uric acid; and inflammation can potentially affect the indices of vascular damage. Accordingly, we computed models of increasing complexity adjusted for basal status (age, sex, eGFR and medication for risk factors), traditional risk factors (mean blood pressure at FMD measurement, HbA1c, low-density lipoprotein (LDL) cholesterol and ever smoking status) and potential nontraditional risk factors (uric acid and hs-CRP). Because of log-normality distribution of plasma hs-CRP, logarithmic-transformed hs-CRP (Log (hs-CRP)) was used in the analysis. Diabetes mellitus is thought to have an effect on both vascular indices. Therefore, to minimize the confounding effect of diabetes mellitus on the association between FMD and SA-IT, we also conducted multiple regression analysis for subjects without diabetes mellitus. We found that both FMD and hs-CRP were significantly correlated with SA-IT. Therefore, we further examined the interaction of FMD and hs-CRP with SA-IT. The data are expressed as means and s.d., medians and interquartile ranges or numbers and percentages. Statistical analyses were conducted using JMP 10 software (SAS Institute, Cary, NC, USA). The P-values of <0.05 were considered statistically significant.
Results
Clinical characteristics
The mean age of all patients at baseline was 44 years, and 60% were male (Table 1). The mean eGFR was 73±31 ml min−1 per 1.73 m2, whereas the prevalence of CKD stages 3–5 was 39% (n=54). Approximately 50% patients had hypertension, and 84% were being treated with renin–angiotensin system inhibitors. The prevalence of diabetes mellitus was only 9%. Age, prevalence of hypertension and hyperuricemia and the use of some drugs for cardiovascular risk factors, such as renin–angiotensin system inhibitors, increased with advancing CKD stage. There was a significant trend toward lower FMD and higher SA-IT with an advance in CKD stage.
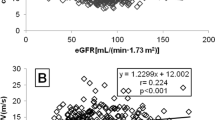
Crude correlation of FMD and SA-IT with eGFR
The eGFR was positively correlated with FMD (r=0.31, P=0.0002) and negatively correlated with the SA-IT index (r=−0.54, P<0.0001; Figures 2a and b).
Crude correlation between potential risk factors for FMD and SA-IT
Age and all classic risk factors, uric acid and the SA-IT index showed an inverse correlation with FMD, whereas eGFR showed a positive correlation. Similarly, age, all classic risk factors except for LDL cholesterol, Log (hs-CRP) and uric acid showed a positive correlation with the SA-IT index, whereas eGFR and FMD showed an inverse correlation.
Correlation between FMD and renal small artery disease
FMD was inversely correlated with the SA-IT index (r=−0.39, P<0.0001; Figure 2c).
Multiple regression analysis for determinants of FMD
In the multivariate analysis with forced entry of age, sex, eGFR, medications for traditional risk factors and traditional risk factors, male sex and LDL cholesterol were significant determinants of FMD (Table 2). After the addition of uric acid and Log (hs-CRP) to model 1, the significance of male sex and LDL cholesterol was attenuated and became marginal. Finally, addition of the SA-IT index to model 2 demonstrated that male sex and medication use were positively correlated with FMD, whereas the SA-IT index was negatively correlated.
Multiple regression analysis for determinants of SA-IT
In the multivariate analysis with force entry of age, sex, eGFR, medications for traditional risk factors and traditional risk factors, age and male sex were significant determinants of the SA-IT index (Table 3). After the addition of Log (hs-CRP) and uric acid (model 2), Log (hs-CRP), age and male sex were significant determinants. Finally, the addition of FMD to model 2 demonstrated that all significant factors in model 2 remained significant.
Therefore, there was a mutual interrelation between FMD and the SA-IT index, independent of various risk factors for CVD. This interaction remained significant even after additional adjustment for baseline brachial artery diameter (data was not shown). Moreover, even after the exclusion of 13 patients with diabetes, the mutual interrelation remained significant as follows: SA-IT for FMD (β=−0.12, P=0.04) and FMD for SA-IT (β=−0.27, P=0.04).
Combination effects of FMD and hs-CRP on SA-IT
Because multiple regression analysis revealed that both FMD and Log (hs-CRP) were significant determinants of SA-IT, we further examined their combined effects on SA-IT and found a significant interaction between these factors for SA-IT (P=0.02 for interaction; Figure 3). Moreover, multiple logistic analysis revealed that the coexistence of a decreased FMD, defined as FMD lower than the mean value, and higher hs-CRP, defined as >3 mg l−1 of hs-CRP, was significantly associated with severe SA-IT, defined as the highest SA-IT index tertile independent of age, sex, medication use, traditional risk factors for CVD and hyperuricemia.
Age, sex, medication use, traditional risk factors for cardiovascular disease (CVD) and hyperuricemia were included in the analysis. Adjusted odds ratios (ORs) for risk of higher-grade small artery intimal thickening (SA-IT) defined as the highest SA-IT index tertile according to higher (⩾3 mg l−1) high-sensitivity C-reactive protein (hs-CRP) and lower (<5.9%) flow-mediated vasodilation (FMD). *vs. subgroup hs-CRP<3 mg l−1/FMD⩾5.9% as a reference, P=0.018. CI, confidence interval.
Discussion
Decreased renal function is an independent risk factor for CVD among CKD patients.10, 11 The present study showed that large conduit artery dysfunction and small renal artery sclerosis progress in parallel with a decrease in kidney function. Although neither eGFR nor traditional risk factors correlated with both indices of vascular disease, hs-CRP correlated with SA-IT in multiple models. Moreover, interrelations between FMD and SA-IT existed independent of traditional risk factors.
Renal small vessel disease reportedly exists even in healthy kidney donors, and its prevalence increases with age.22 In addition, renal function itself is suggested to be associated with endothelial dysfunction in large conduit arteries11, 13 and with small vessel disease in the retina20 and kidney30 among CKD patients. Similarly, we found a significant crude correlation among age, eGFR and both FMD (inverse relationship) and SA-IT. However, multiple regression analysis revealed that the contribution of either age or eGFR to both indices of large and small vessel disease was not clear, suggesting possible contribution by other factors.
FMD and associated factors
Several risk factors related to atherosclerosis were crudely correlated with conduit artery function assessed by FMD; however, these associations were not clear in multiple regression analysis. Therefore, the present study may not have enough power to elucidate the contributions of each risk factor or FMD may not be determined solely by individual risk factors. In contrast, SA-IT correlated with FMD independent of these risk factors. The degree of SA-IT may reflect the burden of measurable and unmeasurable CVD risk factors in CKD patients. Because FMD was reportedly improved after renal transplantation in hemodialysis patients,31, 32 uremia-related risk factors may play a significant role in the progression of large conduit artery dysfunction among CKD patients. A previous study of CKD patients demonstrated that hs-CRP increased in a linear manner with an advance in CKD stage and that it was significantly associated with FMD independent of traditional risk factors.11 However, an independent association between hs-CRP and FMD was not confirmed in the present study. The greater proportion of patients with stage 4–5 CKD in the previous study compared with that in the present study may account for the differences in results. Alternatively, a higher prevalence of patients treated with renin–angiotensin inhibitors may have affected the results because these drugs reportedly improve FMD.33
Renal SA-IT and associated factors
Retinal artery caliber changes closely parallel microvascular structural changes elsewhere in the body, including the kidneys.34 An Australian cohort study demonstrated that a small artery in the retina was narrowed with a decrease in eGFR; therefore, the authors implied that concurrent small vessel disease in the kidney may contribute to the progression of CKD.20 Consistent with those observations, small artery sclerotic changes in the kidneys became more severe with a decline in kidney function in the present study. In addition, senile small artery disease may progress systemically with the progression of CKD. Previous studies demonstrated that hs-CRP was significantly associated with coronary artery atherosclerotic plaque and carotid artery intimal thickening. However, few clinical studies have reported the contribution of inflammation to small artery sclerosis in target organs such as the kidneys. The present study suggests that inflammation may be partially responsible for the development of small artery sclerosis. Moreover, the present study suggests that inflammation concomitant with vascular dysfunction may play a crucial role in small artery sclerosis.
Interrelationship between FMD and renal small artery sclerosis
Besides hs-CRP, FMD was found to be a significant factor for small artery sclerotic change along with conventional risk factors such as hypertension. Although we cannot conclude causality from the present study, these interrelationship may be involved in some underlying mechanisms. A previous report clearly showed that FMD closely correlated with the endothelial function of resistant small arteries of subcutaneous tissue.35 Moreover, accumulation of asymmetric dimethylarginine, an endogenous nitric oxide inhibitor, was reportedly related to endothelial dysfunction in small vessels in patients with advanced CKD.36, 37 These observations suggest that local endothelial dysfunction may be related to renal SA-IT in CKD patients. Alternatively, conduit artery arterial wall stiffness, which can be reflected by decreased FMD, may contribute to small vessel disease as previously proposed.19 Alternatively, renal small artery sclerosis may affect remote peripheral artery function because atherosclerotic renal artery stenosis has been suggested to cause peripheral conduit artery dysfunction.38
The association of decreased kidney function with large conduit artery dysfunction and renal small artery sclerosis may have some clinical implications. Previous studies increasingly suggest that small artery disease is involved in the progression of CVD and kidney dysfunction.16, 34 The present study suggests that inflammation may be responsible for small artery disease. Inflammation was consistently reported to be associated with an increased risk of CVD11 and CKD.39 The direct assessment of small artery disease in target organs is difficult in clinical settings. The results of the present study suggest that FMD may be a potent indicator of small artery sclerosis. In particular, decreased FMD accompanying elevated hs-CRP may be linked to the presence of renal small artery sclerosis among CKD patients. In addition, cross-talk between large vessel disease and small vessel disease is proposed to create a malignant circle and consequently play a crucial role in the progression of CVD.19
There are some limitations to the present study. First, measurement of FMD is highly dependent on technique in the conventional system40 that often fails to detect peak diameter of brachial artery, resulting in underestimation of FMD. However, we used newly developed and semiautomated computerized ultrasonography (UNEXEF18G, UNEX) along with the protocol used in the FMD study conducted in Japan (FMDJ study), the ongoing multicenter study assessing clinical usefulness of FMD.21 In this procedure, continuous edge-tracking system automatically detects and tracks the edges of the brachial artery at the same point throughout the study. In addition to technical issues, FMD at one point could vary because of several factors, including physiological variations and therapeutic effects. Therefore, FMD at one point does not always represent the steady state; however, the variability of FMD generally weakens the correlation of FMD with small artery sclerotic change. Second, we cannot conclude a cause–result relationship in the observed associations such as the correlation of FMD with renal small artery sclerosis. Third, we could not exclude the effects of sampling bias on the accuracy of the assessment of structural changes in the renal small arteries. However, the SA-IT index showed a linear correlation with age and classical risk factors. Moreover, if it had a profound impact on the results, such bias would tend to diminish the significance of specific associations. Fourth, the study sample included a small number of patients with hypertensive nephrosclerosis and diabetic nephropathy, and renal biopsies are generally not indicated in these patients. Therefore, it is not clear whether the observed association between FMD and small artery sclerosis in the kidney can be extended to all CKD etiologies.
In conclusion, large conduit artery dysfunction and renal small artery sclerosis progress in parallel with CKD progression. An interrelationship was found to exist between these indices independent of age, sex and various risk factors among the CKD patients evaluated. Inflammation, particularly when accompanied by vascular dysfunction, was significantly associated with renal small artery sclerosis.
References
Levey AS, de Jong PE, Coresh J, El Nahas M, Astor BC, Matsushita K, Gansevoort RT, Kasiske BL, Eckardt KU . The definition, classification, and prognosis of chronic kidney disease: a KDIGO Controversies Conference report. Kidney Int 2011; 80: 17–28.
Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, de Jong PE, Coresh J, Gansevoort RT . Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet 2010; 375: 2073–2081.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY . Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. New Engl J Med 2004; 351: 1296–1305.
Ross R . Atherosclerosis—an inflammatory disease. New Engl J Med 1999; 340: 115–126.
Yeboah J, Folsom AR, Burke GL, Johnson C, Polak JF, Post W, Lima JA, Crouse JR, Herrington DM . Predictive value of brachial flow-mediated dilation for incident cardiovascular events in a population-based study: the multi-ethnic study of atherosclerosis. Circulation 2009; 120: 502–509.
Yeboah J, Crouse JR, Hsu FC, Burke GL, Herrington DM . Brachial flow-mediated dilation predicts incident cardiovascular events in older adults: the Cardiovascular Health Study. Circulation 2007; 115: 2390–2397.
Muiesan ML, Salvetti M, Paini A, Monteduro C, Galbassini G, Poisa P, Porteri E, Agabiti-Rosei C, Paderno V, Belotti E, Rizzoni D, Castellano M, Agabiti-Rosei E . Prognostic role of flow-mediated dilatation of the brachial artery in hypertensive patients. J Hypertens 2008; 26: 1612–1618.
Chan SY, Mancini GB, Kuramoto L, Schulzer M, Frohlich J, Ignaszewski A . The prognostic importance of endothelial dysfunction and carotid atheroma burden in patients with coronary artery disease. J Am Coll Cardiol 2003; 42: 1037–1043.
Brevetti G, Silvestro A, Schiano V, Chiariello M . Endothelial dysfunction and cardiovascular risk prediction in peripheral arterial disease: additive value of flow-mediated dilation to ankle-brachial pressure index. Circulation 2003; 108: 2093–2098.
Stam F, van Guldener C, Becker A, Dekker JM, Heine RJ, Bouter LM, Stehouwer CD . Endothelial dysfunction contributes to renal function-associated cardiovascular mortality in a population with mild renal insufficiency: the Hoorn study. J Am Soc Nephrol 2006; 17: 537–545.
Yilmaz MI, Stenvinkel P, Sonmez A, Saglam M, Yaman H, Kilic S, Eyileten T, Caglar K, Oguz Y, Vural A, Çakar M, Altun B, Yenicesu M, Carrero JJ . Vascular health, systemic inflammation and progressive reduction in kidney function; clinical determinants and impact on cardiovascular outcomes. Nephrol Dial Transplant 2011; 26: 3537–3543.
Maruhashi T, Soga J, Fujimura N, Idei N, Mikami S, Iwamoto Y, Kajikawa M, Matsumoto T, Hidaka T, Kihara Y, Chayama K, Noma K, Nakashima A, Goto C, Higashi Y . Nitroglycerine-induced vasodilation for assessment of vascular function: a comparison with flow-mediated vasodilation. Arterioscler Thromb Vasc Biol 2013; 33: 1401–1408.
Recio-Mayoral A, Banerjee D, Streather C, Kaski JC . Endothelial dysfunction, inflammation and atherosclerosis in chronic kidney disease—a cross-sectional study of predialysis, dialysis and kidney-transplantation patients. Atherosclerosis 2011; 216: 446–451.
Rizzoni D, Porteri E, Guelfi D, Muiesan ML, Valentini U, Cimino A, Girelli A, Rodella L, Bianchi R, Sleiman I, Rosei EA . Structural alterations in subcutaneous small arteries of normotensive and hypertensive patients with non-insulin-dependent diabetes mellitus. Circulation 2001; 103: 1238–1244.
Rizzoni D, Porteri E, Boari GE, De Ciuceis C, Sleiman I, Muiesan ML, Castellano M, Miclini M, Agabiti-Rosei E . Prognostic significance of small-artery structure in hypertension. Circulation 2003; 108: 2230–2235.
Anderson TJ, Charbonneau F, Title LM, Buithieu J, Rose MS, Conradson H, Hildebrand K, Fung M, Verma S, Lonn EM . Microvascular function predicts cardiovascular events in primary prevention: long-term results from the Firefighters and Their Endothelium (FATE) study. Circulation 2011; 123: 163–169.
Lind L, Berglund L, Larsson A, Sundström J . Endothelial function in resistance and conduit arteries and 5-year risk of cardiovascular disease. Circulation 2011; 123: 1545–1551.
O'Rourke MF, Safar ME . Relationship between aortic stiffening and microvascular disease in brain and kidney: cause and logic of therapy. Hypertension 2005; 46: 200–204.
Laurent S, Briet M, Boutouyrie P . Large and small artery cross-talk and recent morbidity-mortality trials in hypertension. Hypertension 2009; 54: 388–392.
Ooi QL, Tow FK, Deva R, Alias MA, Kawasaki R, Wong TY, Mohamad N, Colville D, Hutchinson A, Savige J . The microvasculature in chronic kidney disease. Clin J Am Soc Nephrol 2011; 6: 1872–1878.
Tomiyama H, Kohro T, Higashi Y, Takase B, Suzuki T, Ishizu T, Ueda S, Yamazaki T, Furumoto T, Kario K, Inoue T, Koba S, Watanabe K, Takemoto Y, Hano T, Sata M, Ishibashi Y, Node K, Maemura K, Ohya Y, Furukawa T, Ito H, Yamashina A . A multicenter study design to assess the clinical usefulness of semi-automatic measurement of flow-mediated vasodilatation of the brachial artery. Int Heart J 2012; 53: 170–175.
Rule AD, Amer H, Cornell LD, Taler SJ, Cosio FG, Kremers WK, Textor SC, Stegall MD . The association between age and nephrosclerosis on renal biopsy among healthy adults. Ann Intern Med 2010; 152: 561–567.
Nakashima Y, Chen YX, Kinukawa N, Sueishi K . Distributions of diffuse intimal thickening in human arteries: preferential expression in atherosclerosis-prone arteries from an early age. Virchows Arch 2002; 441: 279–288.
Nakashima Y, Wight TN, Sueishi K . Early atherosclerosis in humans: role of diffuse intimal thickening and extracellular matrix proteoglycans. Cardiovasc Res 2008; 79: 14–23.
Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA, Deanfield J, Drexler H, Gerhard-Herman M, Herrington D, Vallance P, Vita J, Vogel R, International Brachial Artery Reactivity Task Force. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol 2002; 39: 257–265.
Tomiyama H, Matsumoto C, Yamada J, Teramoto T, Abe K, Ohta H, Kiso Y, Kawauchi T, Yamashina A . The relationships of cardiovascular disease risk factors to flow-mediated dilatation in Japanese subjects free of cardiovascular disease. Hypertens Res 2008; 31: 2019–2025.
Maruhashi T, Soga J, Fujimura N, Idei N, Mikami S, Iwamoto Y, Kajikawa M, Matsumoto T, Hidaka T, Kihara Y, Chayama K, Noma K, Nakashima A, Goto C, Tomiyama H, Takase B, Yamashina A, Higashi Y . Relationship between flow-mediated vasodilation and cardiovascular risk factors in a large community-based study. Heart 2013; 99: 1837–1842.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A, Collaborators developing the Japanese equation for estimated GFR.. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 2009; 53: 982–992.
Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL . New equations to estimate GFR in children with CKD. J Am Soc Nephrol 2009; 20: 629–637.
MacIsaac RJ, Panagiotopoulos S, McNeil KJ, Smith TJ, Tsalamandris C, Hao H, Matthews PG, Thomas MC, Power DA, Jerums G . Is nonalbuminuric renal insufficiency in type 2 diabetes related to an increase in intrarenal vascular disease? Diabetes Care 2006; 29: 1560–1566.
Yilmaz MI, Saglam M, Caglar K, Cakir E, Ozgurtas T, Sonmez A, Eyileten T, Yenicesu M, Acikel C, Oguz Y, Ozcan O, Bozlar U, Erbil K, Aslan I, Vural A . Endothelial functions improve with decrease in asymmetric dimethylarginine (ADMA) levels after renal transplantation. Transplantation 2005; 80: 1660–1666.
Kocak H, Ceken K, Yavuz A, Yucel S, Gurkan A, Erdogan O, Ersoy F, Yakupoglu G, Demirbas A, Tuncer M . Effect of renal transplantation on endothelial function in haemodialysis patients. Nephrol Dial Transplant 2006; 21: 203–207.
Koh KK, Ahn JY, Han SH, Kim DS, Jin DK, Kim HS, Shin MS, Ahn TH, Choi IS, Shin EK . Pleiotropic effects of angiotensin II receptor blocker in hypertensive patients. J Am Coll Cardiol 2003; 42: 905–910.
Thompson CS, Hakim AM . Living beyond our physiological means: small vessel disease of the brain is an expression of a systemic failure in arteriolar function: a unifying hypothesis. Stroke 2009; 40: e322–e330.
Park JB, Charbonneau F, Schiffrin EL . Correlation of endothelial function in large and small arteries in human essential hypertension. J Hypertens 2001; 19: 415–420.
Morris ST, McMurray JJ, Spiers A, Jardine AG . Impaired endothelial function in isolated human uremic resistance arteries. Kidney Int 2001; 60: 1077–1082.
Luksha N, Luksha L, Carrero JJ, Hammarqvist F, Stenvinkel P, Kublickiene K . Impaired resistance artery function in patients with end-stage renal disease. Clin Sci (Lond) 2011; 120: 525–536.
Koivuviita N, Tertti R, Luotolahti M, Raitakari O, Vahlberg T, Nuutila P, Nuutila P, Knuuti J, Metsärinne K . The effect of revascularization of atherosclerotic renal artery stenosis on coronary flow reserve and peripheral endothelial function. Nephron Clin Pract 2011; 118: c241–c248.
Tonelli M, Sacks F, Pfeffer M, Jhangri GS, Curhan G, Cholesterol and Recurrent Events (CARE) Trial Investigators. Biomarkers of inflammation and progression of chronic kidney disease. Kidney Int 2005; 68: 237–245.
Ter Avest E, Stalenhoef AF, de Graaf J . What is the role of non-invasive measurements of atherosclerosis in individual cardiovascular risk prediction? Clin Sci (Lond) 2007; 112: 507–516.
Acknowledgements
We thank the following doctors who provided invaluable advice and support: K Nagahama, A Miyagi, A Hirano, J Ishikawa, M Nakachi, K Tokashiki, N Tomiyama, S Chinen, M Yamazato and A Ishida. We are also grateful to S Hatoma and M Ohta for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Miyagi, T., Kohagura, K., Ishiki, T. et al. Interrelationship between brachial artery function and renal small artery sclerosis in chronic kidney disease. Hypertens Res 37, 863–869 (2014). https://doi.org/10.1038/hr.2014.60
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2014.60
Keywords
This article is cited by
-
Structural changes in renal arterioles are closely associated with central hemodynamic parameters in patients with renal disease
Hypertension Research (2021)
-
A high normal ankle-brachial index is associated with biopsy-proven severe renal small artery intimal thickening and impaired renal function in chronic kidney disease
Hypertension Research (2020)
-
An exaggerated blood pressure response to exercise is associated with nitric oxide bioavailability and inflammatory markers in normotensive females
Hypertension Research (2016)
-
The relationships between visit-to-visit blood pressure variability and renal and endothelial function in chronic kidney disease
Hypertension Research (2015)