Abstract
The OlmeSartan Calcium Antagonists Randomized (OSCAR) study is a multicenter, prospective, randomized, open-label, blinded, end point study of elderly hypertensive Japanese patients that compared the efficacy of a high-dose angiotensin II receptor blocker (ARB) treatment to an ARB plus calcium channel blocker (CCB) combination. In this pre-specified subgroup analysis, we compared the response to such therapy according to sex. A total of 1164 patients (515 (44%) men and 649 (56%) women) were included, and each gender was split into two nearly equal treatment groups. The primary end point was a composite of cardiovascular events and non-cardiovascular death. The baseline characteristics between the two treatment groups in each sex were similar, except for some variables. Male patients had lower systolic and higher diastolic blood pressure than female patients (156.8/85.7 vs. 158.5/84.2 mm Hg). At the end of the study, the mean systolic pressure was higher in the ARB group (134.4 mm Hg) than in the ARB plus CCB group (131.5 mm Hg; P=0.03) for men but not for women (135.4 vs. 133.4 mm Hg; P=0.12). For men, the primary outcome events tended to be higher in the ARB group than in the ARB plus CCB group (hazard ratio (HR)=1.66; P=0.055) but not for women (HR=0.97; P=0.92). This difference in men was due to cardiovascular events (HR=1.86; P=0.03). The interaction between sex and treatment group was not significant (P=0.17). These findings suggest that, in addition to blood pressure control, appropriate patient risk assessment is important for the treatment of hypertension, especially in male patients, as opposed to possible sex differences in treatment effects.
Similar content being viewed by others
Introduction
Essential hypertension is a common comorbid condition and risk factor for cardiovascular events; in addition to lifestyle modification, drug therapy is the main treatment strategy. Although there are indications for specific classes of antihypertensive drugs for particular patients, such as diuretics for hypertensive African Americans,1 there is no uniform agreement on the type of drug(s) that should be used when physicians choose an antihypertensive drug for newly diagnosed patients without specific indications for those drugs.
Recently, many evidence-based clinical practice guidelines from various clinical fields have been published to improve the quality of patient care. For the care of hypertension patients, ‘The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure’ (the JNC-7) was published to provide evidence-based recommendations for patients with specific situations and backgrounds. However, in this guideline, there is no mention of the selection of antihypertensive drugs based on sex, with the exception of pregnancy-related situations.2 In comparison, a relatively recent, large and well-designed randomized controlled trial described possible sex differences in the efficacy of antihypertensive drugs.3 However, only a few cardiovascular trials have provided sex-specific data, and sex differences remain poorly understood. Therefore, this deficiency limits our ability to optimize medical care for both sexes.4, 5
On the basis of the above background, we performed a pre-specified analysis of the OlmeSartan Calcium Antagonists Randomized (OSCAR) study to examine the effect of sex on drug efficacy in patients with hypertension, specifically among Japanese patients at high risk for cardiovascular disease.6
Methods
Study design and participants
The rationale and design for the OSCAR study have been reported elsewhere.6 To summarize, OSCAR was a PROBE (prospective, randomized, open-label, blinded end point) method undertaken at Japanese ambulatory settings.
All enrolled patients had a systolic blood pressure (BP) ⩾140 mm Hg or diastolic pressure ⩾90 mm Hg, in addition to having type 2 diabetes and/or cardiovascular disease (cerebrovascular disease, cardiac disease, vascular disease or renal dysfunction). Before enrollment, all patients provided written informed consent. The study protocol was approved by the institutional review boards of the trial centers and the study was conducted with strict adherence to the Declaration of Helsinki.
The baseline characteristics of the randomized patients have been described in the report of the OSCAR study’s main findings.7
Procedures
In the run-in period, all eligible patients received olmesartan (an angiotensin II receptor blocker (ARB)) monotherapy at a dose of 20 mg per day (a standard dose). If the target BP (<140/90 mm Hg) was not achieved and the treatment was well tolerated, the patients were randomized to receive either (1) a doubled dose (40 mg per day) of olmesartan (high-dose ARB monotherapy) or (2) a calcium channel blocker (CCB) (amlodipine or azelnipidine) combined with 20 mg per day olmesartan (ARB plus CCB combination therapy). If further additional antihypertensive treatment was required to achieve the target BP, other antihypertensive drugs could be added, excluding angiotensin-converting enzyme inhibitors, ARBs and CCBs. The follow-up period was 3 years.
Study outcomes and end points
The primary end point of the main OSCAR study was the time to the first event. The primary end point events were a composite of fatal and non-fatal cardiovascular events, including the following: cerebrovascular disease (cerebral infarction, cerebral hemorrhage, subarachnoid hemorrhage, unspecified stroke and transient ischemic attack); coronary artery disease (sudden death, myocardial infarction, angina pectoris and asymptomatic cardiac ischemia); heart failure; other arteriosclerotic disease (aortic aneurysm, aortic dissection and atherosclerotic disease); diabetic complications (diabetic neuropathy, retinopathy and nephropathy); deterioration of renal function (doubling of serum creatinine, end-stage renal disease as defined by initiation of hemodialysis of renal transplantation); and non-cardiovascular death. The secondary end points were the incidence of each cardiovascular event, change in BP during the follow-up period and serious adverse events other than the primary end points. The end point committee adjudicated all cases of cardiovascular events and deaths without knowledge of the treatment assignment.
Statistical analysis
The subgroup analysis according to sex was pre-specified and described elsewhere, and the rationale of sample size and power calculation for the original study was also previously described.6 Analyses were performed in compliance with the intention-to-treat principle.
Descriptive statistics were summarized with the means and s.d. for continuous variables and frequencies and percentages for categorical variables, and two-sample t-tests were used to compare two continuous variables. χ2 or Fisher’s exact tests were used to evaluate categorical variables, as appropriate. For the primary end points for each sex group, we examined differences between the treatment groups using the log-rank test stratified by age and risk factors. The hazard ratio (HR) and 95% confidence interval (95% CI) were calculated for each treatment group with a stratified Cox proportional hazard model. Time-to-first event curves were estimated by the Kaplan–Meier method. A repeated measures of analysis of variance was used to compare BP during the follow-up period between the groups, and the least square method was used to estimate the mean difference in BP between the treatment groups. In addition, to determine the relationship between prognostic factors and the incidence of primary outcome event, a multivariate Cox proportional hazard analysis was performed for different population models (overall, male and female patients) after adjusting for the following covariates: age, treatment group, baseline cardiovascular disease, baseline diabetes and systolic BP as time-dependent covariates. Moreover, to estimate the heterogeneity of HR for sex, the interaction between the treatment group and sex group was assessed using the interaction terms in a stratified Cox proportional hazard model.
For all the analyses, the overall significant level was determined as 5%, and two-sided tests were used.
Results
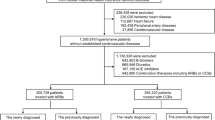
Study patients
The study involved 1164 patients, including 515 (44%) men and 649 (56%) women. Of the male patients, 254 (49%) were assigned to the high-dose ARB group and 261 (51%) were assigned to the ARB plus CCB group. Of the female patients, 324 (50%) were assigned to the high-dose ARB group and 325 (50%) to the ARB plus CCB group. All patients were followed for a median period of 3 years, with a total of 3115.2 patient-years of observation.
Baseline characteristics
Several differences in clinical background were detected between the male and female patients (Table 1). The male patients were younger than the female patients (72.7±5.3 vs. 74.3±5.4; P<0.0001). With regard to comorbid conditions, the male patients were more likely to have both diabetes (58.3 vs. 50.5%; P<0.01) and arteriosclerotic peripheral arterial occlusive disease (3.3 vs. 1.2%; P=0.02) compared with the female patients, but similar rates of history of cardiovascular disease (69.5 vs. 70.0%; P=0.87) existed in the sex groups. Hyperlipidemia was significantly more common in women who used lipid-lowering agents more frequently than the male patients. However, the two treatment groups were similar at baseline within each sex group, although body mass index, diastolic BP and casual plasma glucose were statistically significantly different between the two male groups (Table 1).
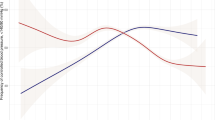
BP during follow-up
At enrollment, systolic BP was lower in men (156.8±12.1 mm Hg) than in women (158.5±11.8 mm Hg; P=0.02), whereas diastolic pressure was higher in men (85.7±10.2 mm Hg) than in women (84.2±9.7; P=0.01) (Figure 1). Significant and clinically relevant reductions in BP relative to the baseline values were noted in both treatment groups and the pattern of BP reduction was similar in men and women. For the male patients, the systolic and diastolic BPs tended to be higher throughout the observation period in the high-dose ARB group than in the ARB plus CCB group, but the differences were not statistically significant at all follow-up points. The mean differences in systolic and diastolic BPs were 2.6 mm Hg (P<0.01) and 2.0 mm Hg (P<0.01), respectively, in the male high-dose ARB and ARB plus CCB groups.
Similarly, for the female patients, both the systolic and diastolic BPs were higher in the high-dose ARB group than in the ARB plus CCB group, and the mean difference in systolic BP in the two treatment groups was 2.8 mm Hg (P<0.01) and 1.4 mm Hg (P=0.01), respectively.
At the end of the study period, the mean systolic pressure was 134.4 mm Hg in the male high-dose ARB treatment group and 131.5 mm Hg in the male ARB plus CCB treatment group (P=0.03). For the female patients, the respective values in both groups were 135.4 mm Hg and 133.4 mm Hg (P=0.12).
The percentage of patients who achieved the target BP of <140/90 mm Hg was significantly lower in the high-dose ARB treatment group than in the ARB plus CCB group for men (61.4 vs. 73.6%; P<0.01) but not for women (62.3 vs. 68.0%; P=0.15).
Primary and secondary outcomes
Among the male patients, the overall rate of primary composite outcome events, including cardiovascular events and all-cause deaths, was better in the ARB plus CCB group than in the high-dose ARB group, although the difference was not statistically significant (HR=1.66, 95% CI=0.99–2.79; P=0.055). Among the female patients, there were no differences in the two parameters between the two treatment groups (HR=0.97, 95% CI=0.55–1.72; P=0.92) (Figure 2). With regard to fatal and non-fatal cardiovascular events, the rate of composite cardiac events (excluding non-cardiovascular deaths) was significantly lower in the ARB plus CCB group than in the high-dose ARB group in men (HR=1.86, 95% CI=1.05–3.30; P=0.03) but not in women (HR=1.02, 95% CI=0.53–1.97; P=0.95). However, for each outcome event, there were no statistically significant differences between the two treatment groups in both sexes, except that cerebrovascular disease and heart failure showed borderline significance in the male patients (Table 2). The interaction between sex and treatment group for the primary composite end points was not statistically significant (P=0.17).
Clinical background and primary outcome events
After adjusting for important prognostic factors such as age, comorbid conditions (previous cardiovascular diseases and/or diabetes) and systolic BP as time-dependent covariates, the rate of primary outcome events was lower in the ARB plus CCB group than in the high-dose ARB group only for men, although only borderline significance was found (HR=1.64, 95% CI=0.97–2.76; P=0.06). The rate of secondary outcome events was significantly lower in the ARB plus CCB group than in the high-dose ARB group (HR=1.81, 95% CI=1.02–3.22; P=0.04) (Table 3).
Adverse events
There were no differences in serious adverse events between the two treatment groups (high-dose ARB and ARB plus CCB) in both men (31 (12.2%), 33 (12.6%); P=0.90) and women (25 (7.7%), 23 (7.1%); P=0.78), respectively. Moreover, the incidence of cancer was also not different in men (5 (2.0%) vs. 12 (4.8%); P=0.14) and women (5 (1.6%) vs. 9 (2.8%); P=0.42).
Discussion
The main finding of the present study was that the treatment of male elderly hypertensive Japanese at high-risk for cardiovascular diseases with ARB plus CCB might result in a better outcome, as defined by cardiovascular events, compared with the treatment with high-dose ARB, albeit no statistical significance was found. No such benefit was found in women.
Our findings are similar and add more information to those reported in previous studies. Although various antihypertensive drugs have similar effects with regard to the lowering of BP, several studies have examined the differences in their efficacies with regard to cardiovascular outcome in patients with different backgrounds. For example, a previous meta-analysis study showed that the relative benefits of hypertension treatment were similar in men and women.8 In that study, the benefit of treatment with antihypertensives was primarily observed for stroke in women and both coronary events and stroke in men. Because the risk levels in untreated patients are different, the absolute benefit as a risk reduction from the therapy would not be the same in men and women.8
Wing et al.9 showed that treatment with ACE inhibitors correlates with a better outcome than treatment with diuretics, whereas another study concluded that the response to specific treatment agents appeared to differ between men and women.10 The ACCOMPLISH trial, which is one of the best clinical trials of combination therapy for hypertension, revealed potential positive effects beyond BP reduction; however, the drugs used in that trial were different from those used in the present study.3 Intriguingly, there was no mention of drug selection for female hypertensive patients in the JNC-7 report published before the ACCOMPLISH trial, and drug treatment of hypertension in women had been assumed to be similar to that in men.2
Our study in male patients showed that treatment with ARB plus CCB resulted in a significantly higher proportion of patients who could achieve their target BP compared with the high-dose ARB group. However, no such benefit was found in female patients. Although the cause for these differences in the response to therapy according to sex are not certain, the proportion of patients who achieved their target BP should have influenced the outcome for both sex groups. Furthermore, the reduction in fatal and non-fatal cardiovascular events was larger in the ARB plus CCB group than in the high-dose ARB group for male patients (P=0.03), but no such benefit was noted in female patients. This finding in male patients was mainly from the differences of cerebrovascular disease (P=0.06) and heart failure (P=0.07), although both findings were not statistically significant. When considered with evidence from previous studies, these findings suggest that high-dose ARB therapy is not as effective as ARB plus CCB therapy in preventing cardiovascular events in male patients, mainly due to differences in BP reduction and/or differences in baseline cardiovascular risk factors and comorbid conditions that could have influenced the clinical outcome. However, as based on a multivariate analysis adjusted for baseline comorbid conditions and sequence of BP, our results for the superiority of ARB plus CCB therapy to high-dose ARB therapy in male patients were consistent with regard to fatal and non-fatal cardiovascular events (P=0.04).
Nonetheless, our analyses focused on differences in sex groups but the interaction between treatment and sex was not significant,11, 12 similar to previous studies.13, 14 Therefore, the effect of treatment cannot be explained exclusively by sex. Thus, the differences in the clinical outcomes between the treatment groups for each sex are likely due to unadjusted, confounding factors and comorbid conditions, including baseline differences of patient characteristics. Such factors are known to affect the outcome in hypertensive patients, as opposed to unknown biological sex effects of the drug used. On the basis of this point of view, we believe that risk assessment at baseline and the establishment of a treatment strategy based on clinical background and comorbidities are important, especially for male patients, and are also critical for the choice of antihypertensive agents and BP reduction.
Our study has several limitations. First, the results cannot be generalized. As mentioned above, the OSCAR study included elderly high-risk Japanese patients who had diabetes and/or history of cardiovascular diseases at enrollment. In addition to these conditions, other clinical features may have influenced the outcome of antihypertensive treatment. Furthermore, one of the distinctive aspects of the OSCAR study was its characteristic population, both with regard to old age and comorbidities and the inclusion of as much as 56% female patients. In general, women are underrepresented in clinical trials and studies, even in National Institute of Health-supported cardiovascular randomized controlled trials.15 One report that analyzed 56 randomized controlled trials indicated that the median percentage of women in studies that included both sexes was as low as 37%.16 Second, it is important to consider the possible false results due to issues related to power analysis used in our study. The OSCAR study enrolled a rather small number of patients compared with recent clinical trials. For example, the non-significant interaction between treatment and sex observed in the present study might be due to an underpowered sample size.12 However, the obtained results should not represent an overestimation and should be interpreted based on the best available knowledge from former studies. Finally, the OSCAR study employed a PROBE design and only the end points were blinded. Therefore, physician and patient bias could not be eliminated.17 However, as we reported previously, we believe that aggressive treatment for BP control was performed for all patients, as there was a high percentage of patients who achieved target BP control in both the treatment and sex groups.7 To tackle these issues in future, large, well-designed studies and extended meta-analyses are needed.
In conclusion, treatment with ARB plus CCB might result in a better outcome than high-dose ARB treatment in male patients but not in female patients. Our present findings should be interpreted as appropriate patient risk assessment, and BP control is important in any strategy for hypertension treatment, especially in male patients, rather than as possible sex differences in treatment effect. Further studies are necessary to select the best antihypertension treatment that is amenable to the patients’ background in addition to sex differences.
References
Flack JM, Sica DA, Bakris G, Brown AL, Ferdinand KC, Grimm RH Jr, Hall WD, Jones WE, Kountz DS, Lea JP, Nasser S, Nesbitt SD, Saunders E, Scisney-Matlock M, Jamerson KA . Management of high blood pressure in blacks: an update of the international society on hypertension in blacks consensus statement. Hypertension 2010; 56: 780–800.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ . The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 2003; 289: 2560–2572.
Jamerson K, Weber MA, Bakris GL, Dahlof B, Pitt B, Shi V, Hester A, Gupte J, Gatlin M, Velazquez EJ . Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. New Engl J Med 2008; 359: 2417–2428.
Blauwet LA, Hayes SN, McManus D, Redberg RF, Walsh MN . Low rate of sex-specific result reporting in cardiovascular trials. Mayo Clin Proc 2007; 82: 166–170.
Ljungman C, Mortensen L, Kahan T, Manhem K . Treatment of mild to moderate hypertension by gender perspective: a systematic review. J Womens Health (Larchmt) 2009; 18: 1049–1062.
Ogawa H, Kim-Mitsuyama S, Jinnouchi T, Matsui K, Arakawa K . Rationale, design and patient baseline characteristics of olmesartan and calcium antagonists randomized (OSCAR) study: a study comparing the incidence of cardiovascular events between high-dose angiotensin II receptor blocker (ARB) monotherapy and combination therapy of ARB with calcium channel blocker in Japanese elderly high-risk hypertensive patients (ClinicalTrials. Gov no. NCT00134160). Hypertens Res 2009; 32: 575–580.
Ogawa H, Kim-Mitsuyama S, Matsui K, Jinnouchi T, Jinnouchi H, Arakawa K . Angiotensin II receptor blocker-based therapy in Japanese elderly, high-risk, hypertensive patients. Am J Med 2012; 125: 981–990.
Gueyffier F, Boutitie F, Boissel JP, Pocock S, Coope J, Cutler J, Ekbom T, Fagard R, Friedman L, Perry M, Prineas R, Schron E . Effect of antihypertensive drug treatment on cardiovascular outcomes in women and men. A meta-analysis of individual patient data from randomized, controlled trials. The INDANA Investigators. Ann Intern Med 1997; 126: 761–767.
Wing LM, Reid CM, Ryan P, Beilin LJ, Brown MA, Jennings GL, Johnston CI, McNeil JJ, Macdonald GJ, Marley JE, Morgan TO, West MJ . A comparison of outcomes with angiotensin-converting-enzyme inhibitors and diuretics for hypertension in the elderly. New Engl J Med 2003; 348: 583–592.
Safar ME, Smulyan H . Hypertension in women. Am J Hypertens 2004; 17: 82–87.
Wang R, Lagakos SW, Ware JH, Hunter DJ, Drazen JM . Statistics in medicine—reporting of subgroup analyses in clinical trials. New Engl J Med 2007; 357: 2189–2194.
Lagakos SW . The challenge of subgroup analyses-reporting without distorting. New Engl J Med 2006; 354: 1667–1669.
ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs. diuretic: The antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). JAMA 2002; 288: 2981–2997.
Zanchetti A, Julius S, Kjeldsen S, McInnes GT, Hua T, Weber M, Laragh JH, Plat F, Battegay E, Calvo-Vargas C, Cieslinski A, Degaute JP, Holwerda NJ, Kobalava J, Pedersen OL, Rudyatmoko FP, Siamopoulos KC, Storset O . Outcomes in subgroups of hypertensive patients treated with regimens based on valsartan and amlodipine: an analysis of findings from the value trial. J Hypertens 2006; 24: 2163–2168.
Kim ES, Carrigan TP, Menon V . Enrollment of women in national heart, lung, and blood institute-funded cardiovascular randomized controlled trials fails to meet current federal mandates for inclusion. J Am Coll Cardiol 2008; 52: 672–673.
Geller SE, Koch A, Pellettieri B, Carnes M . Inclusion, analysis, and reporting of sex and race/ethnicity in clinical trials: have we made progress? J Womens Health 2011; 20: 315–320.
Kohro T, Yamazaki T . Cardiovascular clinical trials in Japan and controversies regarding prospective randomized open-label blinded end-point design. Hypertens Res 2009; 32: 109–114.
Acknowledgements
This work was supported by a grant from the Japan Heart Foundation. This trial was registered with ClinicalTrails.gov, number NCT00134160.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
SK-M has received consultancy fees/honoraria from AstraZeneca, Astellas, Bayer, Boerhinger Ingelheim, Daiichi-Sankyo, Kyowa Hakko Kirin, Novartis, Pfizer, Takeda, Shionogi and Servier. HO has received grants from the Japan Heart Foundation and has also received consultancy fees/honoraria from Astellas, AstraZeneca, Bayer, Boehringer Ingelheim, Daiichi-Sankyo, Eisai, Kowa, Kyowa Hakko Kirin, MSD, Novartis, Pfizer, Sanofi-Aventis, Schering-Plough and Takeda. The remaining authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Matsui, K., Kim-Mitsuyama, S., Ogawa, H. et al. Sex differences in response to angiotensin II receptor blocker-based therapy in elderly, high-risk, hypertensive Japanese patients: a subanalysis of the OSCAR study. Hypertens Res 37, 526–532 (2014). https://doi.org/10.1038/hr.2014.23
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2014.23