Abstract
Particulate matter (PM) and its constituents are recognized risk factors for the development of respiratory symptoms and illness in children. Most measurements of exposure have relied upon stationary indoor monitors (SIMs), overlooking the role of resuspended PM. To improve exposure characterization to resuspended aerosol PM, a recently developed methodology has been employed. The goal of this study was to characterize the resuspendable fraction of house dust and early childhood exposures to PM and its constituents in the child’s home and compare conventional SIM and the Pre-toddler Inhalable Particulate Environmental Robotic (PIPER), an innovative mobile sampler. The study seeks to demonstrate that PIPER provides a more relevant estimate of exposure from inhalable particulate matter through improved correlation with respiratory symptoms in young children. Seventy-five households with children between 3 and 59 months of age were recruited from clinics in central New Jersey. Demographic information, and responses to a health questionnaire based upon that used by the International Study of Allergies and Asthma in Childhood (ISAAC), and household data were collected. Household exposures to inhalable PM (PM100) and endotoxin were determined with simultaneous SIM and mobile (PIPER) sampling. Univariate and multivariate analyses were carried out. History of wheeze (“recent” (<1 year) and “ever”), cough, asthma and eczema was evaluated. Multivariate analysis models included PM100 and endotoxin levels by tertiles of exposure. Risk of asthma for the highest tertile of PM100, as measured by PIPER (odds ratio=4.2; 95% confidence interval 0.7–24.0), was compared with measurements by SIM (odds ratio=0.7; 95% confidence interval 0.2–2.6). Measurements of PM and its constituents with PIPER are more strongly associated with asthma, eczema and wheeze compared with measurements using SIMs. Application of this methodology may provide useful insights into early childhood exposures related to the etiology of childhood illnesses associated with inhalation exposures.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Klepeis NE, Nelson WC, Ott WR, Robinson JP, Tsang AM, Switzer P et al. The National Human Activity Pattern Survey (NHAPS): a resource for assessing exposure to environmental pollutants. J Expo Anal Environ Epidemiol 2001; 11: 231–252.
Arrandale VH, Brauer M, Brook JR, Brunekreef B, Gold DR, London SJ et al. Exposure assessment in cohort studies of childhood asthma. Environ Health Perspect 2011; 119: 591–597.
Wood RA, Bloomberg GR, Kattan M, Conroy K, Sandel MT, Dresen A et al. Relationships among environmental exposures, cord blood cytokine responses, allergy and wheeze at 1 year of age in an inner-city birth cohort (Urban Environment and Childhood Asthma study). J Allergy Clin Immunol 2011; 127: 913–919.
Patel MM, Quinn JW, Jung KH, Hoepner L, Diaz D, Perzanowski M et al. Traffic density and stationary sources of air pollution associated with wheeze, asthma, and immunoglobulin E from birth to age 5 years among New York City children. Environ Res 2011; 111: 1222–1229.
Perzanowski MS, Miller RL, Thorne PS, Barr RG, Divjan A, Sheares BJ et al. Endotoxin in inner-city homes: associations with wheeze and eczema in early childhood. J Allergy Clin Immunol 2006; 117: 1082–1089.
Gehring U, Strikwold M, Schram-Bijkerk D, Weinmayr G, Genuneit J, Nagel G et al. Asthma and allergic symptoms in relation to house dust endotoxin: phase two of the International Study on Asthma and Allergies in Childhood (ISAAC II). Clin Exp Allergy 2008; 38: 1911–1920.
McCormack MC, Breysse PN, Matsui EC, Hansel NN, Williams D, Curtin-Brosnan J et al. In-home particle concentrations and childhood asthma morbidity. Environ Health Perspect 2009; 117: 294–298.
Raja S, Xu Y, Ferro AR, Jaques PA, Hopke PK . Resuspension of indoor aeroallergens and relationship to lung inflammation in asthmatic children. Environ Int 2010; 36: 8–14.
Wallace LA, Wheeler AJ, Kearney J, Van Ryswyk K, You H, Kulka RH et al. Validation of continuous particle monitors for personal, indoor, and outdoor exposures. J Expo Sci Environ Epidemiol 2011; 21: 49–64.
Wallace LA, Mitchell H, O'Connor GT, Neas L, Lippmann M, Kattan M et al. Particle concentrations in inner-city homes of children with asthma: the effect of smoking, cooking, and outdoor pollution. Environ Health Perspect 2003; 111: 1265–1272.
Abt E, Suh HH, Allen G, Koutrakis P . Characterization of indoor particle sources: a study conducted in the metropolitan Boston area. Environ Health Perspect 2000; 108: 35–44.
Zeldin DC, Eggleston P, Chapman M, Piedimonte G, Renz H, Peden D . How exposures to biologics influence the induction and incidence of asthma. Environ Health Perspect 2006; 114: 620–626.
McHugh BM, MacGinnitie AJ . Indoor allergen sensitization and the risk of asthma and eczema in children in Pittsburgh. Allergy Asthma Proc 2011; 32: 372–376.
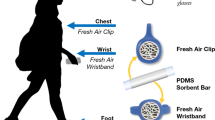
Shalat SL, Lioy PJ, Schmeelck K, Mainelis G . Improving estimation of indoor exposure to inhalable particles for children in the first year of life. J Air Waste Manag Assoc 2007; 57: 934–939.
Shalat SL, Stambler AA, Wang Z, Mainelis G, Emoekpere OH, Hernandez M et al. Development and in-home testing of the pretoddler inhalable particulate environmental robotic (PIPER Mk IV) sampler. Environ Sci Technol 2011; 45: 2945–2950.
Ferro AR, Kopperud RJ, Hildemann LM . Elevated personal exposure to particulate matter from human activities in a residence. J Expo Anal Environ Epidemiol 2004; 14 (Suppl 1): S34–S40.
Wang Z, Shalat SL, Black K, Lioy PJ, Stambler AA, Emoekpere OH et al. Use of a robotic sampling platform to assess young children's exposure to indoor bioaerosols. Indoor Air 2012; 22: 159–169.
Castro-Rodriguez JA . The asthma predictive index: a very useful tool for predicting asthma in young children. J Allergy Clin Immunol 2010; 126: 212–216.
Lawson JA, Dosman JA, Rennie DC, Beach J, Newman SC, Senthilselvan A . The association between endotoxin and lung function among children and adolescents living in rural area. Can Respir J 2011; 18: e89–84.
Rennie DC, Lawson JA, Kirychuk SP, Paterson C, Willson PJ, Senthilselvan A et al. Assessment of endotoxin levels in the home and current asthma and wheeze in school-age children. Indoor Air 2008; 18: 447–453.
Rosenbaum PF, Crawford JA, Anagnost SE, Wang CJK, Hunt A, Anbar RD et al. Indoor airborne fungi and wheeze in the first year of life among a cohort of infants at risk for asthma. J Expo Sci Environ Epidemiol 2010; 20: 503–515.
Mendy A, Gasana J, Viera ER, Forno E, Patel J, Kadam P et al. Endotoxin exposure and childhood wheeze and asthma: a meta-analysis of observational studies. J Asthma 2011; 48: 685–693.
Celedon JC, Milton DK, Ramsey CD, Litonjua AA, Ryan L, Platts-Mills TA et al. Exposure to dust mite allergen and endotoxin in early life and asthma and atopy in childhood. J Allergy Clin Immunol 2007; 120: 144–149.
Sordillo JE, Hoffman EB, Celedon JC, Litonjua AA, Milton DK, Gold DR . Multiple microbial exposures in the home may protect against asthma or allergy in childhood. Clin Exp Allergy 2010; 40: 902–910.
Sordillo JE, Sharma S, Poon A, Lasky-Su J, Belanger K, Milton DK et al. Effects of endotoxin exposure on childhood asthma risk are modified by a genetic polymorphism in ACAA1. BMC Med Genet 2011; 12: 158.
Fuiano N, Incorvaia C, Prodam F, Procaccini DA, Bona G . Relationship between the atopy patch test and clinical expression of the disease in children with atopic eczema/dermatitis syndrome and respiratory symptoms. Ann Allergy Asthma Immunol 2008; 101: 174–178.
Horick N, Weller E, Milton DK, Gold DR, Li R, Spiegelman D . Home endotoxin exposure and wheeze in infants: correction for bias due to exposure measurement error. Environ Health Perspect 2006; 114: 135–140.
Center for Disease Control and Prevention, National Center for Health Statistics, http://cdc.gov/growthcharts. CDC, Atlanata, GA, 2000.
Cavagna GA, Franzetti P, Fuchimoto T . The mechanics of walking in children. J Physiol 1983; 343: 323–339.
Asher MI, Keil U, Anderson HR, Beasley R, Crane J, Martinez F et al. International Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur Respir J 1995; 8: 483–491.
Chen WY, Tseng HI, Wu MT, Hung HC, Wu HT, Chen HL et al. Synergistic effect of multiple indoor allergen sources on atopic symptoms in primary school children. Environ Res 2003; 93: 1–8.
Perry TT, Wood RA, Matsui EC, Curtin-Brosnan J, Rand C, Eggleston PA . Room-specific characteristics of suburban homes as predictors of indoor allergen concentrations. Ann Allergy Asthma Immunol 2006; 97: 628–635.
Chen CM, Sausenthaler S, Bischof W, Herbarth O, Borte M, Behrendt H et al. Perinatal exposure to endotoxin and the development of eczema during the first 6 years of life. Clin Exp Dermatol 2010; 35: 238–244.
Ozkaynak H, Xue J, Weker R, Butler D, Koutrakis K, Sprengler J The Particle Team (PTEAM) Study: Analysis of the Data. EPA Project Summary, 1997. EPA/600/SR-95/098: 1–12.
Carlsten C, Ferguson A, Dimich-Ward H, Chan H, DyBuncio A, Rousseau R et al. Association between endotoxin and mite allergen exposure with asthma and specific sensiticitization at age 7 in high-risk children. Pediatr Allergy Immunol 2011; 22: 320–326.
Liu AH . Endotoxin exposure in allergy and asthma: reconciling a paradox. J Allergy Clin Immunol 2002; 109: 379–392.
Ryan PH, Bernstein DI, Lockey J, Reponen T, Levin L, Grinshpun S et al. Exposure to traffic-related particles and endotoxin during infancy is associated with wheezing at age 3 years. Am J Respir Crit Care Med 2009; 180: 1068–1075.
Thorne PS, Kulhankova K, Yin M, Cohn R, Arbes SJ, Jr, Zeldin DC . Endotoxin exposure is a risk factor for asthma: the national survey of endotoxin in United States housing. Am J Respir Crit Care Med 2005; 172: 1371–1377.
Cohen Hubal EA, Sheldon LS, Burke JM, McCurdy TR, Berry MR, Rigas ML et al. Children's exposure assessment: a review of factors influencing children's exposure, and the data available to characterize and assess that exposure. Environ Health Perspect 2000; 108: 475–486.
Bouillard L, Michel O, Dramaix M, Devleeschouwer M . Bacterial contamination of indoor air, surfaces, and settled dust, and related dust endotoxin concentrations in health office buildings. Ann Agric Environ Med 2005; 12: 187–192.
Rosati JA, Thornburg J, Rodes C . Resuspension of particulate matter from carpet due to human activity. Aerosol Sci Technol 2008; 42: 472–482.
Jantunen M, Hanninen O, Koistinen K, Hashim JH . Fine PM measurements: personal and indoor air monitoring. Chemosphere 2002; 49: 993–1007.
Schneider T . Dust and fibers as a cause of indoor environment problems. SJWEH Suppl 2008; 4: 10–17.
Acknowledgements
Funding for this research was provided by the National Institute of Environmental Health Science, R01ES014717 and R01ES020415: SL Shalat, Piscataway, NJ, USA, and the Center for Environmental Exposures and Disease, P30ES005022: H Zarbl, Piscataway, NJ, USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ramagopal, M., Wang, Z., Black, K. et al. Improved exposure characterization with robotic (PIPER) sampling and association with children’s respiratory symptoms, asthma and eczema. J Expo Sci Environ Epidemiol 24, 421–427 (2014). https://doi.org/10.1038/jes.2014.27
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jes.2014.27
Keywords
This article is cited by
-
Exploring the utility of robots in exposure studies
Journal of Exposure Science & Environmental Epidemiology (2021)
-
Household airborne endotoxin associated with asthma and allergy in elementary school-age children: a case–control study in Kaohsiung, Taiwan
Environmental Science and Pollution Research (2020)
-
Crawling-induced floor dust resuspension affects the microbiota of the infant breathing zone
Microbiome (2018)
-
Respiratory health effects of exposure to low levels of airborne endotoxin – a systematic review
Environmental Health (2018)
-
Comparison of particulate matter exposure estimates in young children from personal sampling equipment and a robotic sampler
Journal of Exposure Science & Environmental Epidemiology (2017)