Abstract
Hepatocellular carcinoma (HCC) is the third leading cause of cancer-related death worldwide, and systemic chemotherapy is the major treatment strategy for late-stage HCC patients. Poor prognosis following chemotherapy is the general outcome owing to recurrent resistance. Recent studies have suggested that in addition to cytotoxic effects on tumor cells, chemotherapy can induce an alternative cascade that supports tumor growth and metastasis. In the present investigation, we showed that thyroid hormone (TH), a potent hormone-mediating cellular differentiation and metabolism, acts as an antiapoptosis factor upon challenge of thyroid hormone receptor (TR)-expressing HCC cells with cancer therapy drugs, including cisplatin, doxorubicin and tumor necrosis factor-related apoptosis-inducing ligand (TRAIL). TH/TR signaling promoted chemotherapy resistance through negatively regulating the pro-apoptotic protein, Bim, resulting in doxorubicin-induced metastasis of chemotherapy-resistant HCC cells. Ectopic expression of Bim in hepatoma cells challenged with chemotherapeutic drugs abolished TH/TR-triggered apoptosis resistance and metastasis. Furthermore, Bim expression was directly transactivated by Forkhead box protein O1 (FoxO1), which was negatively regulated by TH/TR. TH/TR suppressed FoxO1 activity through both transcriptional downregulation and nuclear exclusion of FoxO1 triggered by Akt-mediated phosphorylation. Ectopic expression of the constitutively active FoxO1 mutant, FoxO1-AAA, but not FoxO1-wt, diminished the suppressive effect of TH/TR on Bim. Our findings collectively suggest that expression of Bim is mediated by FoxO1 and indirectly downregulated by TH/TR, leading to chemotherapy resistance and doxorubicin-promoted metastasis of hepatoma cells.
Similar content being viewed by others
Main
Hormones are molecules produced by glands in the body that enter the bloodstream and influence the behavior of another group of cells located distally. Aberrant hormone levels are implicated in the formation of several cancers. For instance, excessive estrogen or progesterone is reported to promote cellular growth of breast and prostate tumors, with antiestrogen and progesterone currently used as the main treatment strategies for these cancer types.1, 2 Thyroid hormones (TH), mainly 3,3′-5-tri-iodo-L-thyronine (T3), are potent mediators of multiple physiological activities, including cellular differentiation, metabolic rate, digestive functions and lipid metabolism.3, 4 The actions of T3 are executed via binding to thyroid hormone receptor (TR) located in the nucleus. TRs are ligand-dependent transcription factors encoded by two genes, TRα and TRβ. Upon binding of T3, TRs release associated co-repressors and recruit transcriptional co-activators to initiate target gene transcription.5 Liver is one of the major target organs of T3, and body TH levels are closely correlated with multiple liver-associated diseases, such as hepatocellular carcinoma (HCC).6, 7, 8, 9
In the diethylnitrosamine (DEN)-induced HCC animal model,10, 11 T3 has been identified as a potent inhibitor of HCC development, although significant associated mitogenic effects on hepatocytes are reported. Conversely, in chemotherapy-resistant populations of advanced HCC cells, TH/TR has been shown to promote tumor cell metastasis via upregulation of several extracellular matrix (ECM) proteases, such as matrix metalloproteinase (MMP)-2, -7 and -9.12
The observed effects of TH/TR on HCC development signify hormone-mediated targeting of pathways leading to apoptosis to achieve stage-specific outcomes. The conserved intrinsic mitochondrial apoptosis pathway is controlled by interplay between subgroups of the Bcl-2 family,13 specifically, pro-apoptotic multi-domain, antiapoptotic and pro-apoptotic Bcl-2-homology domain 3 only (BH3-only) proteins. The members of the BH3-only subfamily of proteins share only the short BH3 domain with members of the Bcl-2 family. The expression patterns and activities of BH3-only proteins are strictly regulated through complex cellular signals at both the transcriptional and posttranscriptional levels. These proteins have significant roles in initiating various physiological apoptotic events, including developmentally programmed cell death and stress-associated apoptosis.13, 14
Bcl-2-interacting mediator of cell death (Bim) is one of the BH3-only proteins that exhibits potent ability to bind all anti-apoptotic Bcl-2 proteins with high affinity to trigger cell death.15 In addition to its intrinsic toxicity, alternative splicing generates a variety of Bim isoforms with different cellular toxicities and modes of regulation.16, 17, 18 Among these, Bim-EL, Bim-L and Bim-S, differing in proapoptotic activity, have been most extensively studied. In view of the finding that suppression of Bim promotes metastasis and chemoresistance of tumor cells, considerable research attention has focused on its utility as an inducer of cell death and thus a potential target for tumor therapy.19, 20, 21
Expression of Bim is mainly controlled by transcription factors of the class O (FoxO) of the Forkhead box-containing protein family.22, 23 FoxO transcription factors, including FoxO1 (FKHR), FoxO3 (FKHRL1), FoxO4 (AFX) and FoxO6, bind DNA through a conserved forkhead box. They are additionally recruited to target sites through protein–protein interactions with other transcription factors, such as nuclear receptors,24 and are critical for various cellular physiological functions, including cell cycle regulation and apoptosis.25, 26, 27 Transactivational activity of these proteins on target genes is highly dependent on their subcellular localization. For instance, in cells where the PI3k-Akt pathway is activated, FoxO1 is phosphorylated at residues T24, S256 and S319 and later shuttled out of nucleus, resulting in loss of binding to target regulatory elements.28 Mutation of these three residues to alanine creates a constitutively active mutant (FoxO1-AAA), which cannot be phosphorylated by PI3k-Akt pathway and therefore remains in the nucleus.
In the current study, we showed that expression of Bim is mediated by FoxO1 and indirectly downregulated by TH/TR. T3/TR suppresses FoxO1 through transcriptional regulation and Akt-mediated nuclear exclusion and degradation. These events subsequently lead to chemotherapy resistance and doxorubicin-promoted metastasis of TR-expressing hepatoma cells.
Results
T3 regulates Bim mRNA and protein levels in TR-overexpressing hepatoma cells
To explore the tumor-killing mechanism of TRs in HCC, the expression patterns of apoptosis-related genes in TR-overexpressing hepatoma cells following T3 treatment were examined via microarray. Among the range of apoptosis-related genes investigated, Bim was significantly downregulated upon T3 stimulation. To confirm this finding, ectopic expression of TRα and TRβ with adenovirus in J7 and Hep3B hepatoma cell lines was performed (Figure 1a). The levels of Bim mRNA were suppressed in a time-, dose- and TR-dependent manner in various TR-overexpressing J7 cells following T3 treatment (Figure 1b). The effect of T3 on Bim protein expression was additionally assessed in isogenic cell lines derived from J7 or Hep3B. After incubation with 0 or 10 nM T3, levels of the three isoforms (EL, L and S) of Bim protein were dramatically suppressed in TR-overexpressing but not control cells (Figures 1c and d). Our results clearly indicate that T3 inhibits Bim expression at both the mRNA and protein level in a TR-dependent manner in hepatoma cells.
Effect of T3 on Bim mRNA and protein expression in hepatoma cell lines. (a) Detection of TR protein in TR-overexpressing or control J7 and Hep3B cell lines. (b) RNA from TR-overexpressing or control cell lines maintained in T3-depleted ([T3]=0 nM) or supplemented medium ([T3]=1 or 10 nM) for 24 or 48 h was prepared prior to qRT-PCR analysis of Bim mRNA. Values (means±S.E.M.) are shown as fold induction relative to 0 nM T3. All assays were repeated at least three times. **P<0.01; *P<0.05 (c and d) Levels of the three isoforms of Bim (Bim-EL, Bim-L and Bim-S) in total lysates of isogenic J7 and Hep3B cell lines maintained in the absence or presence of T3 (1 or 10 nM) for 24 or 48 h were determined via western blotting. ACTIN signals served as the loading control
T3/TR-dependent suppression of the Bim promoter is exerted via FoxO1
To determine whether T3/TR-mediated Bim downregulation occurs through transcriptional repression or other means, the human Bim promoter region encompassing nucleotides from upstream position −1995 to +338 (promoter region 1, P1) was cloned into pGL3-basic-TK vector, and regulation by TR was determined via measuring luciferase activity. Various deletion mutants from this region were additionally generated to pinpoint the crucial elements responsible for T3-induced Bim repression (promoter regions 15, P1–P5). Using these reporter constructs, the effects of transrepression of TR/T3 on the Bim 5′-flanking regions were determined.
Following the reporter activity assay, luciferase activities of the reporters driven by fragments −1995 to +338, −1000 to +338 and -440 to +338 (P1–P3) were dramatically suppressed in the presence of T3 in J7-TR cells. Interestingly, the suppressive effect of T3 on both −190 to +338 (P4) and −1950 to +243 (P5) regions was partially relieved. Previous studies have identified two putative FoxO1-binding elements, F-box1 (positions −216 to −223) and F-box 2 (positions +276 to +283), within this region that have critical roles in Bim activation.22, 23 We propose that these two F-boxes mediate the suppressive effect of T3 on the Bim promoter, in view of the finding that deletion of either one reduces the inhibitory effect of T3 (Figure 2b, P4 and P5). Site-directed mutagenesis of either F-box 1 (Figures 2a and b, P6) or F-box 2 (Figures 2a and b, P7) in the P1 promoter partially rescued T3-suppressed luciferase activity. Furthermore, mutation of both elements (P8) led to blockade of the inhibitory effect of T3 (Figure 2a). These data clearly suggest that F-box 1 and F-box 2 are the major cis-elements mediating the repressive effect of T3 on the Bim promoter.
T3/TR-dependent suppression of the Bim promoter via FoxO1. (a) The Bim 5′-flanking region (−1950 to +338; P1), Bim 5′-deletion and FoxO1 consensus-binding site mutants (P1–P8) were cloned into pGL3-basic-TK vector to generate luciferase reporter plasmids. The promoter region in these mutants is shown (left). After co-transfection with β-galactosidase (a transfection efficiency control), J7-TR cells were harvested and luciferase activity was measured following treatment with T3 (0 or 10 nM) for 48 h. Luciferase activity was normalized to that of β-galactosidase (**P<0.01; *P<0.05). (b) The structure of the human Bim 5′-flanking region (positions −1950 to +338; P1) containing two putative FoxO1 consensus-binding sites. (c) Luciferase activities of the Bim promoter were analyzed in J7 cells after ectopic expression of control or FoxO1-wt via adenoviral transfection. Luciferase activity was normalized to that of β-galactosidase. Data represent means±S.E.M. of values derived from three independent experiments (**P<0.01; *P<0.05). (d) Following ectopic expression of control, FoxO1-wt or FoxO1-AAA via adenoviral (Ad-control, -FoxO1-wt or -FoxO1-AAA) infection in J7-TR cells, the effects of T3 on Bim promoter (positions −1950 to +338; P1) activity were examined as for panel (a)
To further establish whether T3-mediated transcriptional repression of Bim is FoxO1 dependent, we assessed the effect of FoxO1 on Bim promoter activity in J7 or J7-TR cells in the absence and presence of T3. Bim promoter-driven reporter assays showed that FoxO1 overexpression enhances Bim promoter activity in J7 cells (Figure 2c). Additionally, ectopic overexpression of wild-type FoxO1 (FoxO1-wt) in J7-TR cells partially eliminated the effect of T3 on the Bim promoter (Figure 2c). Overexpression of FoxO1-AAA, a constitutively active form of FoxO1 (in which the three Akt phosphorylation sites are mutated to alanine) fully blocked the suppressive effect of T3 on the Bim promoter (Figure 2d). Our findings collectively demonstrate an important role of FoxO1 in T3-mediated regulation of Bim promoter activity and further suggest that T3 suppresses Bim promoter activity by interfering with FoxO1-mediated activation of the Bim promoter via regulating Akt-mediated phosphorylation of FoxO1.
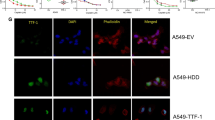
T3/TR represses FoxO1 expression through genomic and non-genomic effects
Although a crucial role of FoxO1 in T3-mediated transcriptional repression of Bim has been demonstrated, the issue of whether the FoxO1 transcription factor is regulated by T3/TR is yet to be clarified. RNA levels of FoxO1 were dramatically repressed in J7 cells after incubation with T3 in a time-, dose- and TR-dependent manner (Figure 3a). Similarly, the protein levels of FoxO1 were repressed by T3 in TR-expressing J7 and Hep3B cell lines (Figures 3b and c). Notably, T3 effect on the repression of FoxO1 and Bim proteins was observed in Huh7, a hepatoma cell line expressing endogenous TR proteins. (Supplementary Figures S1A and B). Regulation of Bim expression by FoxO1 was examined by GFP-FoxO1 overexpression transiently. Dramatic enhancement of all isoforms of Bim protein was observed (Figure 3d). To further ascertain whether the suppressive effect of T3 on Bim protein occurs through FoxO1 downregulation, FoxO1-wt or FoxO1-AAA was overexpressed in J7-TR cells following T3 treatment. Interestingly, FoxO1-wt had only a minor effect in restoring the Bim protein level in the presence of T3. However, overexpression of FoxO1-AAA, diminished the T3-suppressive effect on Bim protein expression (Figure 3e). These data were consistent with the results of the reporter assays (Figure 2a) and suggest that T3 not only suppresses FoxO1 expression at the transcriptional level but also influences its activities via Akt-mediated nuclear exclusion or degradation. As T3/TR can trigger rapid, non-transcriptional effects through cross-coupling with the phosphatidylinositol 3-kinase (PI3K)-Akt pathway,29 we explored whether T3 influences FoxO1 activity in hepatoma cells through a non-genomic mechanism. The level of activated phospho-Akt was dynamically enhanced (Figure 3f), in parallel with downregulation of Bim and the nuclear exclusion of endogenous FoxO1 or exogenous GFP-FoxO1 after T3 treatment (Supplementary Figure S2 and Figures 3g and h). The results indicate that T3/TR represses FoxO1 through both genomic and non-genomic effects, leading to decreased Bim expression.
T3/TR represses Bim protein expression via downregulation of FoxO1. (a) RNA from TR-overexpressing or control J7 cells in the absence or presence of T3 for 24 or 48 h was prepared prior to qRT-PCR analysis of FoxO1 mRNA expression. Values (means±S.E.M.) are shown as fold induction, compared with 0 nM T3. All assays were repeated at least three times (**P<0.01). (b and c) FoxO1 protein levels in total lysates of isogenic J7 and Hep3B cell lines maintained in the absence or presence of T3 (1 or 10 nM) for 24 or 48 h, determined using western blotting. ACTIN signals served as the loading control. (d) After transfection of GFP-FoxO1 for 48 h in J7 cells, the expression levels of FoxO1 and three isoforms of Bim were examined using western blotting. (e) Following ectopic expression of control, FoxO1-wt or FoxO1-AAA via adenoviral infection in J7-TR cells, the effects of T3 on Bim protein expression were examined using western blotting. (f) Following T3 (10 nM) stimulation for the indicated times, lysates of J7-TR cells were extracted for examining phosphor-AKT expression with western blotting. AKT1 and ACTIN were used as internal controls. (g and h) After T3 (10 nM) treatment for the indicated times, cytoplasmic and nuclear fractions of J7-TR or GFP-FoxO1-overexpressing J7-TR cells were extracted for detecting endogenous FoxO1 or exogenous GFP-FoxO1 protein expression
Bim acts synergistically with cisplatin, doxorubicin and tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) to kill hepatoma cells
The expression levels of Bim proteins in several hepatoma cells with various invasion/metastatic capabilities at distinct differentiation stages were compared. Bim proteins were highly enriched in Hep3B and Mahlavu but present at lower levels in HepG2 and SK-Hep1 cells (Figure 4a). To ascertain whether higher levels of Bim sensitize hepatoma cells to chemotherapeutic drugs or tumor-killing cytokines, Bim-S was overexpressed via adenoviral transduction in HepG2 and Sk-Hep1 cell lines displaying low Bim expression, followed by challenge with the anticancer drugs cisplatin, doxorubicin or recombinant (r)-TRAIL (Figure 4b). Cell viability results with both cell types indicated enhanced cisplatin, doxorubicin and r-TRAIL-induced cell death in Bim-s-overexpressing cells (Figure 4c). Moreover, although all the tested drugs triggered apoptotic events, as evident from increased activation of Caspase-3 and the number of cells in the sub-G1 populations, their effects were significantly enhanced upon Bim overexpression in HepG2 and Sk-Hep1 cells (Figures 4d and e). To further determine the influence of Bim on anticancer drug-mediated apoptosis of hepatoma cells, expression in J7, the hepatoma cell line containing physiologically high levels of Bim, was reduced using the shRNA-mediated knockdown approach (Figure 4f). As expected, the extent of cisplatin, doxorubicin or r-TRAIL-induced apoptosis (indicated by cell viability and active caspase 3 levels) was dramatically reduced in Bim-depleted J7 cells (Figures 4g–i). These results suggest that Bim acts as a synergistic factor to induce apoptosis in hepatoma cells challenged with chemotherapeutic drugs or tumor-killing cytokines, such as TRAIL.
Bim acts synergistically with cisplatin, doxorubicin and TRAIL to kill hepatoma cells. Detection of Bim proteins in (a) parental HCC cell lines and (b) Ad-Bim-infected HepG2 or SK-hep1 cells. (c) Ad-control or Ad-Bim infected cells were treated with cisplatin (2.5 μg/ml), doxorubicin (2.5 μM) or r-TRAIL (10 ng/ml) for 48 h. After stimulation, cell viability was measured using the MTT assay, and data are presented as relative absorbance values (%) of vehicle-treated cells. (d and e) Control and Bim-overexpressing cells were treated with the indicated reagents for 24 h, the extent of caspase-3 activation determined via western blotting (d), and the proportions of apoptotic cells in samples subjected to various treatments assessed using propidium iodide (PI) staining and flow cytometry (e). Values are presented as means±S.E.M. of data from experiments performed in triplicate. Differences between data were evaluated using Student’s t-test (**P<0.01; *P<0.05). (f) Immunoblot analysis of the expression patterns of Bim proteins in J7 cells infected with lentivirus expressing luciferase (Sh-Luc) or Bim-targeting shRNA. (g) Control (Sh-Luc) or Bim-depleted (Sh-Bim) cells were treated with cisplatin (2.5 μg/ml), doxorubicin (2.5 μM) or r-TRAIL (10 ng/ml) for 48 h, and cell viabilities were determined via the MTT assay. The extent of caspase-3 activation and proportion of apoptotic cells were determined via (h) western blotting and (i) flow cytometry, respectively, and cell viability was measured using the MTT assay. (h) After treatment with the indicated reagents for 24 h, caspase-3 activation in control or Bim-depleted cells was determined via western blotting analysis. (i) PI staining and flow cytometry were performed to assess the proportion of the sub-G1 phase in samples subjected to various treatments
T3-mediated Bim downregulation protects hepatoma cells against cisplatin, doxorubicin and TRAIL-induced apoptosis
To further clarify the influence of T3/TR on activities of anticancer drugs, TR-overexpressing J7 cells and Huh7 cells were stimulated with several chemotherapeutic drugs and r-TRAIL. The apoptotic events following addition of cisplatin, doxorubicin and r-TRAIL were significantly reduced in T3-pretreated J7-TR and Huh7 cells (Figures 5a–c and Supplementary Figure S3). We were interested in clarifying whether T3 influences the sensitivity of hepatoma cells to these drugs via downregulation of Bim. To this end, Bim-S was ectopically expressed in J7-TR and Huh7 cells with or without T3 treatment (Figure 5d and Supplementary Figure S4A). Interestingly, although T3 pretreatment protected J7-TR and Huh7 cells control cells from apoptosis induced by chemotherapeutic agents, the antiapoptotic effect of T3 was abolished in Bim-overexpressing cells (Figures 5e–g and Supplementary Figures 4B–D). The protective effect of T3/TR against drug-induced cell death was further studied in vivo using subcutaneous xenografts of control (J7-Neo) and TR-overexpressing J7 cells (J7-TR) in euthyroid nude mice. Concordant with in vitro results, TR overexpression conferred not only tumor growth advantage but also resistance to cisplatin and doxorubicin in J7 hepatoma cells (Figure 5h). Based on these collective findings, we propose that T3/TR inhibits the apoptotic effects of chemotherapeutic drugs in hepatoma cells through suppressing expression of the apoptosis regulator FoxO1 and its downstream target Bim.
T3/TR-induced cisplatin, doxorubicin and TRAIL resistance is mediated via Bim downregulation. (a) J7-TR cells were treated with the indicated reagents for 24 h after T3 (0 or 10 nM) stimulation for 48 h, and cell viability was measured using the MTT assay. Data are presented as relative absorbance values (%) of vehicle-treated cells. The extent of caspase-3 activation and proportion of apoptotic cells were determined via (b) western blotting and (c) flow cytometry, respectively. (d) Bim-S was ectopically overexpressed in J7-TR cells via adenovirus infection in the presence or absence of T3 for 48 h, and Bim proteins were determined via western blotting. Cells were subsequently stimulated with the indicated agents for 24 h. (e) Cell viabilities were determined with the MTT assay. (f and g) Caspase-3 activation was determined via western blotting and the percentage of apoptotic cells was assessed with PI-stained flow cytometry. (h) J7-Neo and J7-TR cells were subcutaneously injected into the flanks of nude mice. At 24 days after tumor inoculation, mice were treated with vehicle, cisplatin or doxorubicin. Tumor volumes were measured once every 3 days, and tumor growth curves are shown. Differences between data were evaluated using Student’s t-test (**P<0.01; *P<0.05)
Bim suppresses TH/TR-enhanced doxorubicin resistance and metastasis
Several lines of evidence suggest that chemotherapeutic drugs alternatively have the potential to accelerate tumor progression of apoptosis-resistant cells.30 To further explore this issue, a transwell assay was employed to determine the metastatic capabilities of T3-treated J7-TR cells in the presence of cisplatin or doxorubicin. cisplatin treatment dramatically inhibited cellular migration and invasion, regardless of T3 (Figures 6a and b). Interestingly, doxorubicin suppressed cellular migration but enhanced the invasive potential of J7-TR cells. Additionally, T3 treatment further accelerated doxorubicin-mediated cellular invasion (Figure 6b). The results imply that T3 stimulates apoptosis resistance of J7-TR cells and, subsequently, doxorubicin-enhanced invasion. To ascertain whether Bim has the ability to eliminate the effects of T3 and doxorubicin on cellular invasion, ectopic expression of Bim in J7-TR and Huh7 cells was achieved, followed by transwell invasion analysis. Notably, Bim expression led to dramatic suppression of the invasive ability of J7-TR and Huh7 cells, even in the presence of doxorubicin and T3 (Figure 6c and Supplementary Figure S5). To further ascertain whether these T3/TR-associated effects are replicated in vivo, the orthotopic mouse model was employed. Tumor growth and metastasis were monitored with in vivo imaging system (IVIS) weekly after liver implantation of Luc-GFP-expressing J7-Neo or J7-TR tumors. Concordant with the in vitro results, TR overexpression not only caused tumor resistance to doxorubicin but also increased the metastatic potential of J7 hepatoma cells in vivo (Figure 6d). Taken together, these observations confirm that T3/TR inhibits the apoptotic effects of doxorubicin through Bim downregulation, subsequently promoting tumor progression.
Bim suppresses TH/TR-enhanced doxorubicin resistance and metastasis. (a) In the presence of cisplatin (2.5 μg/ml) and doxorubicin (2.5 μM), the migratory and (b) invasive properties of J7-TR cells treated with or without T3 were assessed using the transwell assay. Images of traversing cells are shown in the left panels and the quantitative results in the right panels. To assess the influence of Bim on chemotherapeutic drugs-mediated invasion of J7-TR cells, (c) invasive properties of control or Bim-overexpressing J7-TR cells were stimulated with cisplatin or doxorubicin in the absence or presence of T3 and subsequently assessed using the transwell assay. Images of traversing cells are shown in the upper panels and the quantitative results in the lower panels. Differences between data were evaluated using Student’s t-test (**P<0.01; *P<0.05). (d) Tumors dissected from mice were subjected to subcutaneous injection with Luc-GFP-expressing J7-Neo and J7-TR cells were introduced orthotopically into the livers of nude mice and monitored weekly with IVIS. After 4 weeks, mice were treated with vehicle or doxorubicin (10 mg/kg, once a week). Relative intensity of luminescence from IVIS is shown in the upper panel, and representative IVIS images 13 weeks after tumor inoculation are shown in the lower panels
Discussion
HCC is the fifth most common cancer and the third most common cause of cancer-related mortality worldwide. More than 748 000 newly diagnosed cases and about 700 000 deaths occur annually.7, 31 Because of the advanced stage of this disease at the time of diagnosis, <30–40% of HCC cases are eligible for curative treatments, including surgery, liver transplantation or percutaneous ablation.32 Eventually, the majority of HCC patients require chemotherapy. To date, doxorubicin has been widely used as a chemotherapeutic drug for advanced HCC but displays low efficacy with a ~15–20% response rate.32 Other chemotherapeutic agents, such as cisplatin, Etoposide, 5-Fluorouracil and their combinations, demonstrate even lower efficacy.33 Because of the poor response to the currently available chemotherapeutic agents, continuous efforts have been made to establish new molecular targets or signaling pathways for developing more effective drugs.
Circulating TH and its cognate receptors have pivotal roles in controlling cellular development and metabolic homeostasis in vertebrates. Additionally, it is increasingly apparent that TH/TRs have important roles in HCC development, with several documented roles in tumorigenesis. For instance, expression levels of TRs and their target genes are decreased in early preneoplastic lesions and hepatocellular HCC in rats, and local hypothyroid status may favor the onset and progression of preneoplastic lesions to HCC.34 A recent epidemiological study also suggested that long-term hypothyroidism is positively correlated with HCC incidence, independent of other risk factors.35 However, the proposed tumor-suppressor role of TRs remains a subject of controversy. For example, an animal model of colorectal tumorigenesis revealed that TRα1 positively regulates several molecules downstream of the Wnt signal, consequently facilitating the expression of β-catenin/Tcf4 target genes and enhancing cell growth. Intriguingly, in a strain of Wnt-activated Apc+/1638N mice, TRα overexpression in the intestinal epithelium did not induce cancer formation but rather accelerated tumorigenesis.36 Recently, another group reported that TRs act as potent suppressors of tumor metastasis in breast cancer cell lines.37 The investigators further showed that mice with double knockout of TRα and TRβ are vulnerable to epithelial tumors and that TR deficiency suppresses the number of benign tumors but enhances malignant tumor formation during carcinogenesis. Thus TH/TR appears to perform dual roles, mitogenic and tumor suppressive, in various tissues, although the mechanisms by which these two functions are coupled remain to be elucidated.
Adult liver is a quiescent organ that exhibits an extremely low mitosis frequency (<1/20 000 hepatocytes). However, several lines of evidence suggest that liver damage caused by partial hepatectomy or other means (including chemical-, nutrition-, vascular- or viral-mediated liver injury) strongly enhances the hepatocyte turnover rate to regenerate damaged parts. These stimulated hepatocytes have higher potential to generate tumor precursor cells that later develop into preneoplastic lesions or HCC.38, 39, 40 Previous studies using the DEN-induced HCC animal model have suggested that T3 serves as a hepatomitogenic factor to stimulate liver cell growth but without associated cell death, consequently leading to decreased preneoplastic hepatic lesions.10, 11 However, in advanced HCC cells, the TH may exert a pro-survival function, causing chemotherapeutic drug resistance. The mitogenic effect of TH may promote malignant hepatic tumor progression or chemoresistance but requires further investigation. In the current study, we confirmed the protective role of T3/TR in hepatoma cells following challenge with several chemotherapeutic agents. Our data suggest that this function is attributable to downregulation of FoxO1 through both transcriptional repression and Akt-mediated nuclear exclusion, subsequently leading to transcriptional repression of Bim.
The FoxO transcription factors are important regulators of cell cycle arrest and apoptosis acting downstream of PTEN.41 These proteins act as important tumor suppressors as they induce cell cycle arrest at the G1–S checkpoint through activation of p27Kip1 or the G2–M checkpoint via activation of GAD45 to stimulate the DNA repair pathway.41, 42, 43 Furthermore, under sustained stress conditions, FoxOs induce expression of the pro-apoptosis gene, Bim, to trigger programmed death of overstressed/damaged cells.22, 23 The ability of FoxO proteins to induce cell arrest and death at multiple steps has attracted considerable research efforts to assess their roles in carcinogenesis or as targets in cancer therapy. A number of lines of evidence have shown that Bim is the major mediator of the cell death effect of various anticancer drugs, including cisplatin and doxorubicin, and its degradation/downregulation is responsible for resistance to these drugs. Therefore, induction of Bim by FoxO may have a key role in maintaining the Bim level in cancer cells and dictating their response to drugs. The current discovery that T3/TR can mitigate the FoxO/Bim cascade in HCC cells suggests that the TR expression level has a significant effect on patient responses to therapeutic drugs. Thus manipulating the T3/TR level in patients may become an important issue in cancer therapy.
Acquisition of anchorage independence is a crucial step for tumor metastasis. Cell life is dependent on anchorage, and cells undergo apoptosis after loss of attachment to ECM or adherence with their neighboring cells. Thus apoptosis induced by cell detachment, designated anoikis, is a critical barrier against tumor metastasis. Bim has a key role in anoikis in several cancer types, including breast cancer, lung cancer, osteosarcoma and melanoma.44, 45, 46 In these cancer types, abrogation of Bim-mediated cell death is required for metastasis. Our data indicate that doxorubicin has the potential to induce hepatoma cell invasion. Notably, T3-induced Bim repression not only caused chemotherapeutic drug resistance but also enhanced doxorubicin-induced metastasis of hepatoma cells. Conversely, ectopic expression of Bim in hepatoma cells strongly increased sensitivity to chemotherapeutic drugs and suppressed doxorubicin-induced metastasis, consequently abolishing TH/TR-enhanced apoptosis resistance and metastasis following drug treatment. The clinical relevance of the TH/TR-suppressed FoxO/Bim cascade needs to be further investigated to establish whether patients with abnormal levels (high or low) of TR show different degrees of metastasis.
Doxorubicin is one of the most commonly used chemotherapeutic drugs. However, several lines of evidence, including data from the current study, support its potential to accelerate malignant tumor progression, with a number of mechanisms proposed to explain this phenomenon. For instance, doxorubicin induces epithelial–mesenchymal transition and cell migration through TGFβ signaling activation in breast cancer.30 MMP-2 and -9, the crucial enzymes that degrade the ECM to facilitate tumor invasion, are activated by doxorubicin.47 Although the current findings suggest that suppression of Bim expression accounts to a large extent for TH/TR-enhanced doxorubicin-mediated metastasis, further studies are essential to ascertain whether metastasis is also enhanced via the above mechanisms. Our observations provide conclusive molecular evidence supporting targeting of the TH and Bim in chemotherapy regimens for HCC.
Materials and Methods
Cell culture
Hepatoma cell lines, including HepG2, Sk-Hep1, Hep3B and isogenic J7, were routinely cultured in Dulbecco’s Modified Eagle’s Medium (DMEM) supplemented with 10% FBS (v/v) at 37 °C in a humidified atmosphere containing 5% (v/v) CO2 and 95% (v/v) air. T3-depleted (T3, 0 nM) serum was prepared by treatment with AG 1-X8 resin (Bio-Rad, Hercules, CA, USA) and added to DMEM at 10% (v/v) to form Td medium. T3 was purchased from Sigma-Aldrich (St. Louis, MO, USA).
Real-time PCR (qRT-PCR)
Total RNA of hepatoma cells was extracted using TRIzol reagent (Life Technologies Inc., Carlsbad, CA, USA), and cDNA strands were synthesized using the Superscript III Kit for RT-PCR (Life Technologies). Real-time quantitative RT-PCR was performed using SYBR Green reaction mix (Applied Biosystems, Carlsbad, CA, USA), and products detected using the ABI PRISM 7500 system (Applied Biosystems, Foster City, CA, USA).
Western blotting
Cell extracts were fractionated via SDS-PAGE on a 12% gel, and the separated proteins were transferred to a polyvinylidene fluoride membrane. Subsequent procedures were performed as described previously.48 Rabbit anti-human antibodies against Bim and active caspase-3 were purchased from Epitomics (Burlingame, CA, USA). The rabbit anti-GFP antibody was obtained from GeneTex (Irvine, CA, USA). Rabbit antibodies against FoxO1 were acquired from Cell Signaling Technology (Boston, MA, USA).
Transient transfection and reporter assays
The 5′-flanking region (positions −1950 to +338) of the Bim gene was amplified and cloned into pGL3-TK vector to generate a P1 reporter plasmid. Sequential 5′or 3′-deletions (P2–P5) and mutants of the FoxO1 consensus-binding element (P6–P8) derived from this reporter were generated. To explore Bim promoter response to T3 or FoxO1 stimulation, J7-TR, J7-FoxO1-WT or J7-FoxO1-AAA cells were transfected with 0.2 μg of Bim promoter-driven reporter constructs and 0.05 μg of SVβ vector expressing β-galactosidase (Clontech, Palo Alto, CA, USA) for 16 h. Cells were subsequently treated with T3 (0 or 10 nM) and incubated for 48 h prior to harvesting. Activities of luciferase and β-galactosidase were subsequently measured.
In vitro invasion assay
The influence of Bim on doxorubicin or T3/TR-mediated invasive activity of TR-overexpressing hepatoma cell lines was assessed using the rapid Transwell in vitro assay. After adjusting cell density to 1 × 105 cells/100 μl of serum-free DMEM, cells were added to each upper chamber coated with Matrigel (Becton-Dickinson, Franklin Lakes, NJ, USA). The lower chamber contained DMEM supplemented with 20% (v/v) FBS. Following incubation for 16 h at 37 °C, cells traversing the filter to the lower chamber were stained with crystal violet and counted. All assays were repeated at least three times. Among-treatment differences were explored using one-way ANOVA (*P<0.05; **P<0.01).
Xenograft mouse model
J7-Neo and J7-TR cells (1 × 106) were subcutaneously injected into the flanks of nude mice (BALB/cAnN.Cg-Foxn1nu/CrlNarl). At 24 days after tumor inoculation, mice were treated with vehicle, cisplatin (10 mg/kg once every 3 days, i.p) or doxorubicin (10 mg/kg once every 3 days, i.p). Tumor volumes were measured twice a week (n=4 for each group), and tumor growth curves are shown.
Orthotopic mouse model
Tissues of subcutaneously grown Luc-GFP-expressing J7-Neo and J7-TR hepatoma cells were sectioned into 1 mm3 pieces. Tumor sections were transplanted into livers of nude mice, as described earlier.49 After 4 weeks, mice were treated with vehicle or doxorubicin (10 mg/kg once per week, i.p). Cellular growth and metastasis of tumors were monitored once a week via IVIS.50 After 13 weeks, mice were killed, and the livers and lungs are collected.
Flow cytometric assay of apoptosis
Parental or derived hepatoma cells were treated with cisplatin, doxorubicin or r-TRAIL after stimulation with T3 (0 or 10 nM) for 24 h. Cells were harvested via trypsinization and fixed in ethanol/PBS (7:3, v/v) for 1 h at −20 °C. Subsequently, cells were washed with PBS and resuspended in PBS containing 40 μg/ml RNase A and 0.5% (v/v) Triton X-100 for 1 h at 37 °C. Finally, cells were pelleted and resuspended in PBS containing propidium iodide (50 μg/ml, Sigma). The extent of genomic DNA fragmentation was quantified via flow cytometric analysis of hypodiploid DNA. Data were collected and analyzed with FACScan (Becton Dickinson, San Jose, CA, USA) running the CellQuest software (Becton Dickinson, San Jose, CA, USA).
Abbreviations
- BH3-only:
-
Bcl-2-homology domain 3 only
- Bim:
-
Bcl-2-interacting mediator of cell death
- DEN:
-
diethylnitrosamine
- ECM:
-
extracellular matrix
- FoxO:
-
transcription factors of the class O
- HCC:
-
hepatocellular carcinoma
- MMP:
-
matrix metalloproteinase
- PI3K:
-
phosphatidylinositol 3-kinase
- TH:
-
thyroid hormone
- TR:
-
thyroid hormone receptor
- TRAIL:
-
tumor necrosis factor-related apoptosis-inducing ligand
References
Pike MC, Spicer DV, Dahmoush L, Press MF . Estrogens, progestogens, normal breast cell proliferation, and breast cancer risk. Epidemiol Rev 1993; 15: 17–35.
Brawer MK . Hormonal therapy for prostate cancer. Rev Urol 2006; 8 (Suppl 2): S35–S47.
Huang YH, Tsai MM, Lin KH . Thyroid hormone dependent regulation of target genes and their physiological significance. Chang Gung Med J 2008; 31: 325–334.
Pilo A, Iervasi G, Vitek F, Ferdeghini M, Cazzuola F, Bianchi R . Thyroidal and peripheral production of 3,5,3'-triiodothyronine in humans by multicompartmental analysis. Am J Physiol 1990; 258 (Pt 1): E715–E726.
Huang YH, Tsai MM, Lin KH . Thyroid hormone dependent regulation of target genes and their physiological significance. Chang Gung Med J 2008; 31: 325–334.
Chan IH, Privalsky ML . Thyroid hormone receptor mutants implicated in human hepatocellular carcinoma display an altered target gene repertoire. Oncogene 2009; 28: 4162–4174.
El-Serag HB, Rudolph KL . Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology 2007; 132: 2557–2576.
Sorvillo F, Mazziotti G, Carbone A, Morisco F, Cioffi M, Rotondi M et al. Increased serum reverse triiodothyronine levels at diagnosis of hepatocellular carcinoma in patients with compensated HCV-related liver cirrhosis. Clin Endocrinol (Oxf) 2003; 58: 207–212.
Chi HC, Chen CY, Tsai MM, Tsai CY, Lin KH . Molecular functions of thyroid hormones and their clinical significance in liver-related diseases. Biomed Res Int 2013; 2013: 601361.
Ledda-Columbano GM, Perra A, Concas D, Cossu C, Molotzu F, Sartori C et al. Different effects of the liver mitogens triiodo-thyronine and ciprofibrate on the development of rat hepatocellular carcinoma. Toxicol Pathol 2003; 31: 113–120.
Ledda-Columbano GM, Perra A, Piga R, Pibiri M, Loi R, Shinozuka H et al. Cell proliferation induced by 3,3',5-triiodo-L-thyronine is associated with a reduction in the number of preneoplastic hepatic lesions. Carcinogenesis 1999; 20: 2299–2304.
Chi HC, Chen SL, Liao CJ, Liao CH, Tsai MM, Lin YH et al. Thyroid hormone receptors promote metastasis of human hepatoma cells via regulation of TRAIL. Cell Death Differ 2012; 19: 1802–1814.
Youle RJ, Strasser A . The BCL-2 protein family: opposing activities that mediate cell death. Nat Rev Mol Cell Biol 2008; 9: 47–59.
Strasser A . The role of BH3-only proteins in the immune system. Nat Rev Immunol 2005; 5: 189–200.
Chen L, Willis SN, Wei A, Smith BJ, Fletcher JI, Hinds MG et al. Differential targeting of prosurvival Bcl-2 proteins by their BH3-only ligands allows complementary apoptotic function. Mol Cell 2005; 17: 393–403.
U M, Miyashita T, Shikama Y, Tadokoro K, Yamada M . Molecular cloning and characterization of six novel isoforms of human Bim, a member of the proapoptotic Bcl-2 family. FEBS Lett 2001; 509: 135–141.
O'Connor L, Strasser A, O'Reilly LA, Hausmann G, Adams JM, Cory S et al. Bim: a novel member of the Bcl-2 family that promotes apoptosis. EMBO J 1998; 17: 384–395.
Ley R, Ewings KE, Hadfield K, Cook SJ . Regulatory phosphorylation of Bim: sorting out the ERK from the JNK. Cell Death Differ 2005; 12: 1008–1014.
Gillings AS, Balmanno K, Wiggins CM, Johnson M, Cook SJ . Apoptosis and autophagy: BIM as a mediator of tumour cell death in response to oncogene-targeted therapeutics. FEBS J 2009; 276: 6050–6062.
Akiyama T, Dass CR, Choong PF . Bim-targeted cancer therapy: a link between drug action and underlying molecular changes. Mol Cancer Ther 2009; 8: 3173–3180.
Wang J, Zhou JY, Wu GS . Bim protein degradation contributes to cisplatin resistance. J Biol Chem 2011; 286: 22384–22392.
Yang Y, Zhao Y, Liao W, Yang J, Wu L, Zheng Z et al. Acetylation of FoxO1 activates Bim expression to induce apoptosis in response to histone deacetylase inhibitor depsipeptide treatment. Neoplasia 2009; 11: 313–324.
Gilley J, Coffer PJ, Ham J . FOXO transcription factors directly activate bim gene expression and promote apoptosis in sympathetic neurons. J Cell Biol 2003; 162: 613–622.
Zhao HH, Herrera RE, Coronado-Heinsohn E, Yang MC, Ludes-Meyers JH, Seybold-Tilson KJ et al. Forkhead homologue in rhabdomyosarcoma functions as a bifunctional nuclear receptor-interACTINg protein with both coactivator and corepressor functions. J Biol Chem 2001; 276: 27907–27912.
Accili D, Arden KC . FoxOs at the crossroads of cellular metabolism, differentiation, and transformation. Cell 2004; 117: 421–426.
Tran H, Brunet A, Griffith EC, Greenberg ME . The many forks in FOXO's road. Sci STKE 2003; 2003: RE5.
Lam EW, Francis RE, Petkovic M . FOXO transcription factors: key regulators of cell fate. Biochem Soc Trans 2006; 34 (Pt 5): 722–726.
Zhang X, Tang N, Hadden TJ, Rishi AK . Akt, FoxO and regulation of apoptosis. Biochim Biophys Acta 2011; 1813: 1978–1986.
Hiroi Y, Kim HH, Ying H, Furuya F, Huang Z, Simoncini T et al. Rapid nongenomic actions of thyroid hormone. Proc Natl Acad Sci USA 2006; 103: 14104–14109.
Bandyopadhyay A, Wang L, Agyin J, Tang Y, Lin S, Yeh IT et al. doxorubicin in combination with a small TGFbeta inhibitor: a potential novel therapy for metastatic breast cancer in mouse models. PLoS One 2010; 5: e10365.
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D . Global cancer statistics. CA Cancer J Clin 2011; 61: 69–90.
Park KW, Park JW, Choi JI, Kim TH, Kim SH, Park HS et al. Survival analysis of 904 patients with hepatocellular carcinoma in a hepatitis B virus-endemic area. J Gastroenterol Hepatol 2008; 23: 467–473.
Cao H, Phan H, Yang LX . Improved chemotherapy for hepatocellular carcinoma. Anticancer Res 2012; 32: 1379–1386.
Frau C, Loi R, Petrelli A, Perra A, Menegon S, Kowalik MA et al. Local hypothyroidism favors the progression of preneoplastic lesions to hepatocellular carcinoma in rats. Hepatology 2015; 61: 249–259.
Hassan MM, Kaseb A, Li D, Patt YZ, Vauthey JN, Thomas MB et al. Association between hypothyroidism and hepatocellular carcinoma: a case-control study in the United States. Hepatology 2009; 49: 1563–1570.
Kress E, Skah S, Sirakov M, Nadjar J, Gadot N, Scoazec JY et al. Cooperation between the thyroid hormone receptor TRalpha1 and the WNT pathway in the induction of intestinal tumorigenesis. Gastroenterology 2010; 138: 1863–1874.
Martinez-Iglesias O, Garcia-Silva S, Tenbaum SP, Regadera J, Larcher F, Paramio JM et al. Thyroid hormone receptor beta1 acts as a potent suppressor of tumor invasiveness and metastasis. Cancer Res 2009; 69: 501–509.
Preston-Martin S, Pike MC, Ross RK, Jones PA, Henderson BE . Increased cell division as a cause of human cancer. Cancer Res 1990; 50: 7415–7421.
Farber E . Hepatocyte proliferation in stepwise development of experimental liver cell cancer. Dig Dis Sci 1991; 36: 973–978.
Columbano A, Shinozuka H . Liver regeneration versus direct hyperplasia. FASEB J 1996; 10: 1118–1128.
Nakamura N, Ramaswamy S, Vazquez F, Signoretti S, Loda M, Sellers WR . Forkhead transcription factors are critical effectors of cell death and cell cycle arrest downstream of PTEN. Mol Cell Biol 2000; 20: 8969–8982.
Medema RH, Kops GJ, Bos JL, Burgering BM . AFX-like Forkhead transcription factors mediate cell-cycle regulation by Ras and PKB through p27kip1. Nature 2000; 404: 782–787.
Tran H, Brunet A, Grenier JM, Datta SR, Fornace AJ Jr., DiStefano PS et al. DNA repair pathway stimulated by the forkhead transcription factor FOXO3a through the Gadd45 protein. Science 2002; 296: 530–534.
Simpson CD, Anyiwe K, Schimmer AD . Anoikis resistance and tumor metastasis. Cancer Lett 2008; 272: 177–185.
Woods NT, Yamaguchi H, Lee FY, Bhalla KN, Wang HG . Anoikis, initiated by Mcl-1 degradation and Bim induction, is deregulated during oncogenesis. Cancer Res 2007; 67: 10744–10752.
Uehara N, Matsuoka Y, Tsubura A . Mesothelin promotes anchorage-independent growth and prevents anoikis via extracellular signal-regulated kinase signaling pathway in human breast cancer cells. Mol Cancer Res 2008; 6: 186–193.
Spallarossa P, Altieri P, Garibaldi S, Ghigliotti G, Barisione C, Manca V et al. Matrix metalloproteinase-2 and -9 are induced differently by doxorubicin in H9c2 cells: The role of MAP kinases and NAD(P)H oxidase. Cardiovasc Res 2006; 69: 736–745.
Liao CS, Tai PJ, Huang YH, Chen RN, Wu SM, Kuo LW et al. Regulation of AKR1B1 by thyroid hormone and its receptors. Mol Cell Endocrinol 2009; 307: 109–117.
Gao YS, Chen XP, Li KY, Wu ZD . Nude mice model of human hepatocellular carcinoma via orthotopic implantation of histologically intact tissue. World J Gastroenterol 2004; 10: 3107–3111.
Liu SC, Tsang NM, Chiang WC, Chang KP, Hsueh C, Liang Y et al. Leukemia inhibitory factor promotes nasopharyngeal carcinoma progression and radioresistance. J Clin Invest 2013; 123: 5269–5283.
Acknowledgements
This work was supported by grants from Chang Gung Memorial Hospital, Taoyuan, Taiwan (CMRPD1C0271, CMRPD1C0272, CMRPD1C0273) and from the Ministry of Science and Technology of the Republic of China (MOST103-2320-B182-018-MY3).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by G Raschella
Supplementary Information accompanies this paper on Cell Death and Disease website
Supplementary information
Rights and permissions
Cell Death and Disease is an open-access journal published by Nature Publishing Group. This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Chi, HC., Chen, SL., Cheng, YH. et al. Chemotherapy resistance and metastasis-promoting effects of thyroid hormone in hepatocarcinoma cells are mediated by suppression of FoxO1 and Bim pathway. Cell Death Dis 7, e2324 (2016). https://doi.org/10.1038/cddis.2016.227
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cddis.2016.227
This article is cited by
-
Acetylation of FOXO1 activates Bim expression involved in CVB3 induced cardiomyocyte apoptosis
Apoptosis (2023)
-
FOXO1 represses MCL1 transcription to regulate the function of vascular smooth muscle cells in intracranial aneurysm
Experimental Brain Research (2022)
-
DOCK6 promotes chemo- and radioresistance of gastric cancer by modulating WNT/β-catenin signaling and cancer stem cell traits
Oncogene (2020)
-
RCC2 contributes to tumor invasion and chemoresistance to cisplatin in hepatocellular carcinoma
Human Cell (2020)
-
Molecular functions and clinical impact of thyroid hormone-triggered autophagy in liver-related diseases
Journal of Biomedical Science (2019)