Abstract
Several cross-sectional studies have demonstrated the relevance of DNA methylation of the glucocorticoid receptor exon 1F region (GR-1F) for trauma-related psychopathology. We conducted a longitudinal study to examine GR-1F methylation changes over time in relation to trauma exposure and the development of post-deployment psychopathology. GR-1F methylation (52 loci) was quantified using pyrosequencing in whole blood of 92 military men 1 month before and 6 months after a 4-month deployment period to Afghanistan. GR-1F methylation overall (mean methylation and the number of methylated loci) and functional methylation (methylation at loci associated with GR exon 1F expression) measures were examined. We first investigated the effect of exposure to potentially traumatic events during deployment on these measures. Subsequently, changes in GR-1F methylation were related to changes in mental health problems (total Symptom Checklist-90 score) and posttraumatic stress disorder (PTSD) symptoms (Self-Report Inventory for PTSD). Trauma exposure during deployment was associated with an increase in all methylation measures, but development of mental health problems 6 months after deployment was only significantly associated with an increased functional methylation. Emergence of post-deployment PTSD symptoms was not related to increased functional methylation over time. Pre-deployment methylation levels did not predict post-deployment psychopathology. To our knowledge, this is the first study to prospectively demonstrate trauma-related increases in GR-1F methylation, and it shows that only increases at specific functionally relevant sites predispose for post-deployment psychopathology.
Similar content being viewed by others
Introduction
Exposure to traumatic stress is a major risk factor for a wide range of psychiatric disorders, including posttraumatic stress disorder (PTSD) and major depressive disorder (MDD).1 The hypothalamus–pituitary–adrenal (HPA) axis is crucial for an adequate response to a stressful environment. The glucocorticoid receptor (GR) determines negative feedback on the HPA axis, and impaired GR functionality has been proposed as a potential pathophysiological mechanism underlying both PTSD and MDD.2
Over a decade ago, Weaver et al.3 demonstrated that DNA cytosine methylation of the GR exon 17 promoter in the hippocampus of rats remains elevated after early life stress and leads to decreased GR expression and increased adult HPA axis activity. This methylation effect was particularly pronounced at a nerve growth factor-inducible protein A (NGFI-A) transcription factor binding site. McGowan et al.4 translated these findings to humans, showing elevated methylation in the GR exon 1F region (GR-1F) in the hippocampus of suicide victims with a childhood abuse history compared with nonabused suicide victims and controls. Following these seminal reports, the number of studies examining GR-1F methylation in relation to traumatic stress and stress-related psychiatric disorders has steadily increased (for reviews see refs 5, 6, 7). Of note, all of these studies examined peripheral tissues to assess GR-1F methylation and significant findings were not limited to NGFI-A-binding sites. In humans, both pre- and postnatal stress have consistently been linked to increased GR-1F methylation in most,5 but not all studies.8 In addition, decreased GR-1F methylation has been found in patients with MDD,9 whereas both increased10 and decreased11 GR-1F methylation were reported in patients with PTSD compared with the controls. These studies all employed a cross-sectional design, which precludes conclusions about causality. As a result, it is still unknown whether GR-1F methylation changes as psychopathology emerges and/or whether it represents a pre-existing vulnerability factor predicting the development of psychopathology.
We therefore quantified GR-1F methylation levels in peripheral blood cells of Dutch military personnel before and after deployment to Afghanistan. In line with the accumulating evidence (for an overview see Daskalakis et al.5), we hypothesized that trauma exposure during deployment would increase GR-1F methylation. In addition, we wanted to explore the direction of GR-1F methylation change in relation to emerging psychopathology symptoms after deployment, as previous evidence is equivocal.5 As reported in a previous study,11 we expected methylation changes associated with changes in GR exon 1F expression to be most informative of change in psychopathology symptoms. Furthermore, we investigated the predictive value of pre-deployment GR-1F methylation for the development of post-deployment psychopathology symptoms. Finally, we explored the association between GR-1F methylation and six functional haplotypes of the GR gene (NR3C1), which were previously associated with GR sensitivity and might be relevant for the development of psychopathology.12
Materials and methods
Participants and assessments
The present study was part of a large longitudinal cohort of Dutch military personnel that were deployed to Afghanistan (n=1032), as part of the International Security Assistance Force, between 2005 and 2008 (for details on procedures see refs 13, 14). Among their duties were searching and clearing of buildings, combat patrols, transport across enemy territory and demining operations. The individuals were exposed to potentially traumatic events such as armed combat, combat casualties and enemy fire. Individuals were assessed (questionnaires were administered and blood samples were drawn) 1 month before, and 1 and 6 months after a 4-month period of deployment. This study examined methylation measures prior to and 6 months after deployment, as psychopathology levels were highest 6 months after deployment.13 To maximize power,15 three subgroups of approximately equal size were selected from this cohort (N=92) based on exposure to potentially traumatic events during deployment (high or low) and post-deployment psychopathology (high or low, only in group with high trauma exposure).16 The study was approved by the Institutional Review Board of the University Medical Center Utrecht (UMCU) and both oral and written informed consent was obtained from all participants.
Mental health problems were assessed with the validated Dutch version of the Symptom Checklist-90 (SCL-90), which includes the total score of eight symptom dimensions: agoraphobia, anxiety, depression, somatization, cognitive performance deficits, mistrust and interpersonal sensitivity, hostility and sleep difficulties.17 PTSD symptoms were measured using the Self-Report Inventory for PTSD (SRIP).18 Changes in SCL-90 and SRIP scores were significantly correlated (ρ=0.52). A 19-item self-report deployment experiences checklist was used to assess traumatic stress exposure during deployment, such as direct combat stressors.13 For childhood trauma, the Early Trauma Inventory-Self Report was used, which includes emotional, physical and sexual abuse.19 For prediction of the development of psychopathology after deployment, individuals were divided into groups with low or high symptom levels based on previously defined cutoff scores of 124 for total SCL-90 and 38 for the SRIP.14, 17, 20 This SCL-90 cutoff score delineates individuals in the general population exceeding average symptoms.21 The SRIP cutoff score14 is in the range with the best sensitivity and specificity for PTSD classification according to the DSM-IV (in a general population).22
Biological measures
Methylation was quantified in 52 CpGs in and adjacent to the 1F region (see Figure 1, numbering in accordance with Daskalakis et al.5). The NGFI-A-binding sites in this region (CpG numbers: 17, 18, 21–26, 35–37, 42, 43) have been suggested to be relevant for GR-1F transcription and HPA axis activity.3
The glucocorticoid receptor exon 1F region (GR-1F) in NR3C1. (a) All 52 5′-C–phosphate–G-3′ sites (CpGs) where methylation was measured in the present study are numbered (red: CpGs where change in methylation was associated with GR exon 1F expression change). Lowercase letters mark the promoter region, uppercase letters the GR-1F exon. Black-lined boxes represent canonical (solid) and non-canonical (dashed) NGFI-A binding sites, after McGowan et al.4 (b) NR3C1 (Chromosome 5: 142 657 496–142 815 077) from the 5′ (left) to 3′ (right) untranslated region. Boxes on the horizontal black line represent exons (gray: non-coding, green: coding sequence). The light gray box indicates a CpG island in the proximal promoter region (from 1D to 1H). (c) Six common and functional haplotypes constituted by six SNPs (rs10052957, rs10482605, rs6189, rs6195, rs41423247 and rs6198) and their frequencies in the present study. Red letters represent the minor alleles. For a scaled representation of exons 2 through 9 in relation to the first exons, see Sinclair et al.23
Whole-blood EDTA samples were collected 1 month before and 6 months after deployment. Standard salting procedures were used to extract DNA. Subsequently, DNA concentration and integrity were determined using riboGreen (Thermo Fisher Scientific, Waltham, MA, USA) and BioAnalyser (Agilent Technologies, Santa Clara, CA, USA), respectively.
GR-1F methylation data were available for 92 individuals. For methylation analysis (EpigenDx, Hopkinton, MA, USA24, 25, 26), DNA was denatured using 3 n NaOH followed by 30- min incubation at 42 °C. Bisulfite salt solution was added to the DNA and incubated for 14 h at 50 °C. Bisulfite-treated DNA was purified using Zymogen DNA columns and eluted in 20 μl T1E0.2 (pH 8) and 1 μl was used for each PCR. PCR was performed using 5 ng of genomic DNA and 0.2 μm of each primer. The final PCR product was purified using Sepharose beads (GE Healthcare Life Sciences, Pittsburgh, PA, USA) and the Pyrosequencing Vacuum Prep Tool (Qiagen, Valencia, CA, USA) as recommended by the manufacturer. Purified PCR product was sequenced using 0.2 μm pyrosequencing primer on the Pyrosequencing PSQ96 HS System (Qiagen) following the manufacturer’s instructions. The percentage of methylation at each locus was determined by looking at the CpG site as an artificial C/T SNP using QCpG software (Qiagen), where C% equals %methylation as calculated by the equation below:

All samples resulted in good pyrosequencing signals and good quality data (for assays, sensitivity, coefficients of variance, numbers of CpG sites and chromosomal regions targeted by the primers, see Supplementary Table S1 in the online data supplement). As GR-1F methylation levels are generally low,27, 28 two measures of overall GR-1F methylation were examined: mean methylation across all CpGs and the number of methylated loci (the number of CpGs with >0% methylation). In addition, to optimally investigate the functional dynamics of methylation, we focused on those CpGs where we observed that longitudinal changes in methylation were significantly related to change in GR exon 1F mRNA expression (for the latter see below), defined as functional methylation. In exploratory analyses, we examined DNA methylation at NGFI-A-binding sites.
GR exon 1F expression data were available for 75 individuals, as RNA quality was not sufficient in 17 individuals. Pre- and post-deployment RNA from peripheral blood mononuclear cells (PBMCs) was isolated with TRIzol reagent (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s instructions. RNA concentrations were determined using a NanoDrop ND-1000 spectrophotometer (NanoDrop Technologies, Wilmington, DE, USA). One μg of total RNA was converted into first-strand cDNA with oligo(dT) primers using RevertAid First Strand cDNA Synthesis Kit (Thermo Fisher Scientific, Waltham, MA, USA) as described by the manufacturer. qPCR assays were carried out in duplicate in a 7900HT Fast Real-Time PCR System (Applied Biosystems, Foster City, CA, USA) with specific primers (see Supplementary Table S3 in the online data supplement) and SensiMix SYBR Hi-ROX (Bioline Reagents, London, UK). For normalization of mRNA expression, RefFinder (OMICtools, Sotteville-Les-Rouen, France) was used to find the most stable reference gene among PPIB, YWHAZ, RPL13a and RPL37a. The relative abundance of mRNAs was standardized with RPL13a mRNA as the invariant control.
In line with the finding that lower GR-1F methylation is associated with dampening of the cortisol response through higher GR-mediated negative feedback,3 we hypothesized GR-1F methylation to be negatively associated to GR sensitivity. Data on GR-binding capacity of PBMCs were available for 47 individuals, as these were acquired several years earlier from a largely overlapping cohort.20 As previously described,20 GR-binding capacity was quantified using a modification of the whole-cell single point-binding assay described by Yehuda et al.29 Using this protocol, specific binding at 100 nm 3H-dexamethasone gave a reliable Bmax, which was determined with a classical binding assay with 3-200 nm 3H-dexamethasone in the absence or presence of an excess of unlabeled dexamethasone (r2=0.92).20 In short, Ficoll-Paque (Pharmacia and Upjohn, Uppsala, Sweden) was used to isolate PBMCs from heparinized whole blood, and 107 cells were frozen in RPMI-1640 (Gibco, Grand Island, NY, USA) in addition of 10% fetal calf serum (FCS) (Gibco) and 20% DMSO. Samples of every single individual were analyzed simultaneously. Cells were thawed, and subsequently washed twice in RPMI-1640 and incubated for 30 min at 37 °C. Again, cells were washed twice, after which they were resuspended in assay buffer (RPMI- 1640 with 10% FCS) and incubated in duplicate with 100 nm 3H-dexamethasone (Amersham, Buckinghamshire, UK) in the absence or presence of excess unlabeled dexamethasone (Sigma-Aldrich, Steinheim, Germany). After 60 min incubation at 37 °C, cells were washed twice in ice cold assay buffer followed by density centrifugation over Ficoll hypaque, separating cell-bound label from free label. Liquid scintillation analysis was used to analyze cell-bound radioactivity. In two simultaneously processed samples the number of cells was counted.
To examine the effect of genetic variation in the GR gene (NR3C1) on GR-1F methylation, six SNPs linked to glucocorticoid sensitivity (rs10052957, rs10482605, rs6189, rs6195, rs41423247 and rs6198)12 were selected. SNPs were genotyped on the Illumina Human OmniExpress-24 Beadchip array, and genetic data were subjected to quality control (see Supplementary Table S4 in the online data supplement for quality control information). SNPs rs10482605, rs6189 and rs41423247 were imputed using the Haplotype Reference consortium release 1.1. R2 values and average call rates were >0.99 for all three SNPs, whereas allele frequencies did not deviate from Hardy–Weinberg equilibrium (all P-values >0.05). Haplotypes were constructed using SNPHAP,30 yielding the following NR3C1 haplotypes: CTGACA (40%), CTGAGA (22%), TTGAGA (15%), TCGACG (13%), CTGGCA (4%) and TCAACG (4%)). NR3C1 haplotypes and individual SNPs from 85 individuals were available.
Statistical analyses
Longitudinal changes in GR-1F methylation around deployment were analyzed by applying mixed models for repeated measures (MMRM) using the nlme package31 in R. The relation of changes in GR methylation with trauma exposure was investigated in a model without adjustment for symptom outcomes whereas the relation with symptom outcomes was investigated in a model with adjustment for trauma exposure during deployment (methylation~methylationpre+trauma during deployment × time+change in mental health problems × time, random factor: subject ID). We only used continuous measures. PTSD symptom scores were log-transformed to improve the distribution.6 In secondary analyses, NR3C1 haplotypes/SNPs or childhood trauma was added to the model. To investigate the influence of GR-1F methylation on GR-1F expression and GR-binding, the latter two measures were used as dependent variables (for example, expression~expressionpre+trauma during deployment × time+change in methylation × time, random factor: subject ID).
Linear regression models were used to examine the cross-sectional relations between pre-deployment GR-1F methylation and childhood trauma or NR3C1 haplotypes/SNPs. Pre- and post-deployment psychopathology symptoms were compared using paired two-tailed t-tests. Methylation values of one individual were >8 s.ds above the mean methylation and were excluded from further analyses (resulting in n=91). Random effects and residuals of the main MMRM were plotted and evaluated for heteroscedasticity and did not show further aberrations.
Considering the relatedness and relatively low number of tests, the significance threshold was set at P<0.05 in primary analyses. However, as 12 NR3C1 haplotypes/SNPs were investigated without prior hypotheses, the significance threshold in these analyses was set at P<0.0042 (0.05/12).
For prediction, receiver operation curves (ROC) were constructed to predict a high level of post-deployment mental health problems or PTSD symptoms with pre-deployment GR-1F methylation. Individuals with a high level of pre-deployment mental health problems (n=8) or PTSD symptoms (n=0) were excluded in the respective analyses. Areas under the curve (AUCs) and corresponding P-values were determined using the verification package in R.32 Sensitivity, specificity, positive and negative predictive values were calculated using the Epi package.33
Potential confounding was investigated by analyzing the correlations of age, body-mass index (BMI), military rank, education, previous number of deployments and white blood cell counts (including values of neutrophils, lymphocytes, monocytes, eosinophils and basophils) with methylation before and after deployment. Moreover, we analyzed the interaction of these covariates with time in our main models to investigate whether they affected the relation between our variables of interest (trauma, and change in psychopathology, GR exon 1F expression and GR-binding) and change in GR-1F methylation.
To investigate the possible influence of alcohol use, medication and smoking, we excluded all individuals that changed medication between baseline and follow-up (n=18, for types of medication see Supplementary Table S3 in the online data supplement), as well as individuals with a changed alcohol use (n =1) or smoking status (n=6) in sensitivity analyses.
Results
Sample characteristics, including information on age, childhood trauma, number of previous deployments, number of deployment-related trauma events, BMI, education, rank, mental health problems and PTSD symptoms are listed in Table 1.
Mean methylation per locus ranged from 0 to 2.60% (see Supplementary Table S2 in the online data supplement). Methylation changes per locus were highly correlated, especially for CpGs 31 to 52 (see Supplementary Figure S1 in the online data supplement).
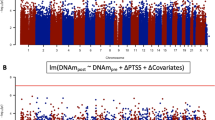
Change in GR-1F methylation was associated with change in GR exon 1F expression at a nominal significance level at the following 17 CpGs: 1, 9, 11, 12, 23, 24, 28, 34, 39, 40, 45–51 (all P-values <0.05, see Figure 1, as well as Supplementary Table S2 and Supplementary Figure S2 in the online data supplement). The mean methylation at these sites constituted our measure of functional methylation. Changes in our three main methylation measures (mean methylation, number of methylated sites and functional methylation) over time were significantly correlated with a minimal ρ of 0.89. Increases in all three methylation measures were associated with decreases in GR exon 1F expression (mean methylation: β=−0.54, P=0.011; number of methylated loci: β=−0.039, P=0.001; functional methylation: β=−0.526, P<0.001, see Table 2 and Figures 2a and b) and GR-binding (mean methylation: β=−463, P=0.014; number of methylated loci: β=−29.9, P=0.010; functional methylation: β=−317, P=0.016). In exploratory analyses, methylation change at NGFI-A binding sites was not associated with a change in GR exon 1F expression (β=−0.22, P=0.36) or GR-binding (β=−413, P=0.06) and was therefore not further analyzed.
Change in mental health problems in relation to (a) the number of methylated loci (n=88, β=0.089, P=0.050) and (b) functional methylation (n=88, β=0.010, P=0.005), and change in GR exon 1F expression in relation to (c) the number of methylated loci (n=75, β=−0.039, P=0.001) and (d) functional methylation (n=75, β=−0.53, P<0.001). Standardized change indicates that methylation levels after deployment were adjusted for pre-deployment values.
GR-1F methylation and exposure to potentially traumatic events
Trauma exposure during deployment was significantly associated with an increase in all three methylation measures (mean methylation: β=0.040, P=0.003; number of methylated loci: β=0.75, P=0.002; functional methylation: β=0.56, P=0.002, see Table 2) and with an increase in methylation at 23 individual CpGs: 2, 4, 8, 9, 17, 19, 20, 22, 28, 31, 32, 34, 35, 39, 40, 45–52 (see Supplementary Table S2 in the online data supplement).
No significant associations were observed between childhood trauma and our main methylation measures (change in methylation over time: all P-values >0.54; pre-deployment methylation: all P-values >0.40).
GR-1F methylation and the development of psychopathology
Although the development of mental health problems was only at trend level significance associated with an increase in the number of methylated loci (β=0.089, P=0.050) (Figure 2c) and not with mean methylation (β=0.004, P=0.10), it was significantly associated with an increase in functional methylation (β=0.010, P=0.005) (Table 2 and Figure 2d). Significant associations between change in mental health problems and methylation change existed at 14 CpGs (22, 31–35, 39–41, 44, 47, 48, 51, 52).
The development of PTSD symptoms was not associated with change in any methylation measure (all P-values >0.12, see Table 2). At a nominal significance level, change in PTSD symptoms was associated with methylation change at 9 individual CpGs (10, 20, 25, 31, 35–37, 44, 51, see Supplementary Table S2 in the online data supplement).
GR-1F methylation and genetic variation in NR3C1
None of the NR3C1 haplotypes or individual SNPs was significantly associated with either pre-deployment or prospective changes in GR-1F methylation measures after correcting for multiple testing (data not shown). Nevertheless, rs10052957 showed an association with prospective methylation changes at a nominal significance level (TC carriers with CC as reference; mean methylation: β=−0.25, P=0.046; number of methylated loci: β=−4.21, P=0.045; functional methylation: β=−0.38, P=0.022).
Confounder and sensitivity analyses
Confounding by age, BMI, military rank, education, previous number of deployments and white blood cell counts (including values of neutrophils, lymphocytes, monocytes, eosinophils and basophils) was highly unlikely as these measures were not correlated with methylation before or after deployment (P-values >0.05). In addition, cell-type composition was similar before and after deployment.16 Furthermore, including the interactions of these covariates with time did not affect the associations between change in GR-1F methylation with trauma exposure during deployment, change in mental health problems or PTSD symptoms, change in GR-1F expression or change in GR-binding.
No individuals used antidepressants at any time point (see Supplementary Table S5 in the online data supplement). Exclusion of individuals with changed medication, smoking status or alcohol use status after deployment (total n=23) strengthened most associations of GR-1F methylation in the longitudinal analyses (as indicated by the βs) except for the associations with GR-binding, which did not remain significant (see Supplementary Table S6 in the online data supplement).
Prediction of post-deployment psychopathology by pre-deployment GR-1F methylation
Pre-deployment methylation did not significantly predict a high level of post-deployment mental health problems (mean methylation: AUC=0.51, P=0.47; number of methylated loci: AUC=0.54, P=0.32; functional methylation: AUC=0.51, P=0.47) or PTSD symptoms (mean methylation: AUC=0.58, P=0.11; number of methylated loci: AUC=0.56, P=0.18; functional methylation: AUC=0.56, P=0.17).
Discussion
We examined longitudinal changes in whole-blood GR-1F methylation from 1 month prior to until 6 months after a 4-month period of military deployment in relation to deployment-related trauma and the development of mental health problems and PTSD symptoms. We found that deployment-related trauma was associated with an increase in all GR-1F methylation measures. However, only an increase in GR-1F methylation at loci associated with GR exon 1F expression (functional methylation) was significantly related to the development of post-deployment mental health problems. In contrast, the emergence of PTSD symptoms was not associated with an increase in functional methylation over time. Pre-deployment GR-1F methylation did not predict a high level of psychopathology symptoms after deployment. Moreover, six functional NR3C1 haplotypes and the six SNPs constituting these haplotypes were not associated with changes in GR-1F methylation.
We believe this study provides the first longitudinal evidence in humans that methylation differences between trauma- and non-trauma-exposed individuals previously reported in the majority of cross-sectional studies (see for review Daskalakis et al.5) reflect a response to traumatic stress exposure. An increase in GR-1F methylation at functionally relevant sites could result in impaired negative feedback on the HPA axis,34 leading to increased vulnerability to psychopathology. The here reported association between functional GR-1F methylation increase and emerging mental health problems fits this hypothesis. In contrast, we did not find any associations between childhood trauma and GR-1F methylation, whereas most, but not all,8 previous studies found a positive association (see for review Daskalakis et al.5). Of note, the fact that elevated GR-1F methylation levels could constitute a vulnerability factor for the development of psychopathology was not supported by our prediction models and has not been investigated in prior studies. Moreover, the only two previous longitudinal studies on GR-1F methylation do not indicate that psychotherapeutic interventions influence this hypothesized pathophysiological mechanism. Perroud et al.35 reported no change in mean GR-1F methylation in 61 patients with borderline personality disorder after intensive dialectical behavior therapy. Yehuda et al.28 showed that pre-treatment GR-1F methylation levels (sum and number of methylated loci) significantly differed between responders (n=8) and non-responders (n=8) receiving psychotherapy for PTSD, but did not find a significant methylation change over time.
In contrast to our study, it was previously observed that individuals with a high level of post-deployment PTSD symptoms had increased GR sensitivity36 and GR-binding14, 37 prior to deployment (whereas depressive symptom development was associated with decreased GR sensitivity36). Moreover, Yehuda et al.11 found lower GR-1F methylation and evidence for increased GR sensitivity in PTSD patients compared with trauma-exposed controls. These opposing directionalities of effects cannot be ascribed to a difference in pathophysiology between PTSD symptoms and mental health problems (measured with the SCL-90), as Yehuda et al.11 found negative associations of GR-1F methylation with both outcomes, whereas we found positive associations (not significant for PTSD symptoms). Of note, both increased and decreased functionality of the GR have been linked to psychopathology, and Raison and Miller2 previously suggested that these mechanisms are specific to PTSD and MDD, respectively. However, two recent studies contradict this hypothesis, showing decreased GR-1F methylation in MDD9 and increased GR-1F methylation in PTSD.10 Moreover, PTSD and MDD often co-occur which complicates the interpretation of findings. This is illustrated by the significant correlation (ρ=0.50) between change in depressive symptoms (subscale SCL-90) and change in PTSD symptoms in the present study.
The main strength of the current study is its longitudinal design, with GR-1F methylation, expression, GR-binding and psychiatric outcomes assessed before and after military deployment. Evidence from longitudinal studies is paramount as it is much less influenced by genetic predispositions and other confounding factors that may influence both methylation levels and psychopathology than cross-sectional studies. In addition, the present study investigated the entire GR exon 1F region, allowing examination of all CpGs in relation to GR exon 1F expression. This approach highlights that associations between change in GR-1F methylation and expression are site-specific and present at 17 out of 52 CpGs. Thirteen of these 17 CpGs have previously been associated with trauma and/or psychopathology (CpG numbers 1, 9, 23, 28, 34, 40 and 45–51, see this review5). Our findings do not support an important role for NGFI-A binding sites in GR-1F transcription. This is in line with recent evidence suggesting that several other transcription factors are important in the GR exon 1F region.38 Other strengths are the generally healthy cohort at baseline, the absence of antidepressant use at any time point and the sensitivity analyses that exclude a confounding effect of change in any medication, smoking or alcohol use status. Finally, we explored the associations between NR3C1 haplotypes and SNPs with GR-1F methylation and did not find any significant associations with baseline GR-1F methylation, which is in line with a recent study,39 or with methylation change. This finding highlights the fact that GR-1F methylation is just one biological mechanism influencing GR sensitivity, whereas NR3C1 haplotypes may be independently associated with GR functioning and psychopathology.12
A possible limitation is the relevance of peripheral blood methylation to the brain. Several studies suggest that methylation differences across tissues are substantial,40, 41 even though consistent effects of various methylation quantitative trait loci are found across tissues.42 However, the effect of trauma, mediated through stress hormones or cytokines, appears to affect the epigenome in a wide range of cell and tissue types.7 This is in line with findings of Tyrka et al.,34 who demonstrated a cross-sectional relation between trauma-related whole-blood GR-1F methylation with decreased negative feedback of the HPA axis. Also, increased GR-1F methylation in peripheral blood cells has consistently been linked to (early life) adversity.5 The question of generalizability of methylation patterns across tissues also pertains to our measurement of GR exon 1F expression and GR-binding in PBMCs, instead of whole blood.43 Another limitation is our focus on GR-1F, whereas methylation in other parts of NR3C1 may hold additional information about the relation between trauma and GR function.44 In addition, only Dutch Caucasian males were investigated that limits the generalizability. This may be relevant as there is evidence for ethnic and sex-specific differences in cortisol stress responsivity in relation to DNA methylation.45 Furthermore, in addition to baseline GR exon 1F expression data examined here, GR exon 1F expression data following stress may provide additional information of its relation with GR-1F methylation. Finally, we used self-report questionnaires to assess psychiatric outcomes, constituting a possible source of social desirability bias, and our questionnaire for exposure to potentially traumatic events does not take severity and impact into account.
In conclusion, this is the first longitudinal evidence-linking changes in GR-1F methylation to trauma exposure and the development of psychopathology symptoms. Our data indicate that trauma exposure increases GR-1F methylation and that only increases at specific functionally relevant sites may predispose for post-deployment psychopathology. These results suggest an important role for epigenetic regulation of GR functioning after trauma exposure in the development of psychopathology.
References
Kendler KS, Karkowski LM, Prescott CA . Causal relationship between stressful life events and the onset of major depression. Am J Psychiatry 1999; 156: 837–841.
Raison CL, Miller AH . When not enough is too much: The role of insufficient glucocorticoid signaling in the pathophysiology of stress-related disorders. Am J Psychiatry 2003; 160: 1554–1565.
Weaver ICG, Cervoni N, Champagne FA, D’Alessio AC, Sharma S, Seckl JR et al. Epigenetic programming by maternal behavior. Nat Neurosci 2004; 7: 847–854.
McGowan PO, Sasaki A, D’Alessio AC, Dymov S, Labonté B, Szyf M et al. Epigenetic regulation of the glucocorticoid receptor in human brain associates with childhood abuse. Nat Neurosci 2009; 12: 342–348.
Daskalakis NP, Yehuda R . Site-specific methylation changes in the glucocorticoid receptor exon 1F promoter in relation to life adversity: systematic review of contributing factors. Front Neurosci 2014; 8: 369.
Vinkers C, Kalafateli AL, Rutten B, Kas M, Kaminsky Z, Turner J et al. Traumatic stress and human DNA methylation: a critical review. Epigenomics 2015; 7: 593–608.
Turecki G, Meaney M . Effects of the social environment and stress on glucocorticoid receptor gene methylation: a systematic review. Biol Psychiatry 2016; 79: 87–96.
Tyrka AR, Parade SH, Welch ES, Ridout KK, Price LH, Marsit C et al. Methylation of the leukocyte glucocorticoid receptor gene promoter in adults: associations with early adversity and depressive, anxiety and substance-use disorders. Transl Psychiatry 2016; 6: e848.
Na K-S, Chang HS, Won E, Han K-M, Choi S, Tae WS et al. Association between glucocorticoid receptor methylation and hippocampal subfields in major depressive disorder. PLoS ONE 2014; 9: e85425.
Perroud N, Rutembesa E, Paoloni-Giacobino A, Mutabaruka J, Mutesa L, Stenz L et al. The Tutsi genocide and transgenerational transmission of maternal stress: epigenetics and biology of the HPA axis. World J Biol Psychiatry 2014; 15: 334–345.
Yehuda R, Flory JD, Bierer LM, Henn-Haase C, Lehrner A, Desarnaud F et al. Lower methylation of glucocorticoid receptor gene promoter 1F in peripheral blood of veterans with posttraumatic stress disorder. Biol Psychiatry 2015; 77: 356–364.
Hardeveld F, Spijker J, Peyrot WJ, de Graaf R, Hendriks SM, Nolen WA et al. Glucocorticoid and mineralocorticoid receptor polymorphisms and recurrence of major depressive disorder. Psychoneuroendocrinology 2015; 55: 154–163.
Reijnen A, Rademaker AR, Vermetten E, Geuze E . Prevalence of mental health symptoms in Dutch military personnel returning from deployment to Afghanistan: a 2-year longitudinal analysis. Eur Psychiatry 2015; 30: 341–346.
Van Zuiden M, Geuze E, Willemen HLDM, Vermetten E, Maas M, Amarouchi K et al. Glucocorticoid receptor pathway components predict posttraumatic stress disorder symptom development: a prospective study. Biol Psychiatry 2012; 71: 309–316.
Boks MPM, Schipper M, Schubart CD, Sommer IE, Kahn RS, Ophoff RA . Investigating gene-environment interaction in complex diseases: Increasing power by selective sampling for environmental exposure. Int J Epidemiol 2007; 36: 1363–1369.
Boks MP, Rutten BPF, Geuze E, Houtepen LC, Vermetten E, Kaminsky Z et al. SKA2 methylation is involved in cortisol stress reactivity and predicts the development of post-traumatic stress disorder (PTSD) after military deployment. Neuropsychopharmacology 2016; 41: 1350–1356.
Arrindell W, Ettema H, Groenman N, Brook F, Janssen I, Slaets J et al. Further Dutch experiences with the symptom checklist-90 revised. Psycholoog 2003; 38: 582.
Hovens JE, Bramsen I, van der Ploeg HM . Self-rating inventory for posttraumatic stress disorder: review of the psychometric properties of a new brief Dutch screening instrument. Percept Mot Skills 2002; 94: 996–1008.
Bremner JD, Bolus R, Mayer EA . Psychometric properties of the early trauma inventory-self report. J Nerv Ment Dis 2007; 195: 211–218.
van Zuiden M, Geuze E, Maas M, Vermetten E, Heijnen CJ, Kavelaars A . Deployment-related severe fatigue with depressive symptoms is associated with increased glucocorticoid binding to peripheral blood mononuclear cells. Brain Behav Immun 2009; 23: 1132–1139.
Arrindell WA, Ettema JHM . SCL-90: Revised Manual for a Multidimensional Indicator of Psychopathology in Herziene Handleiding bij een Multidimensionele Psychopathologie Indicator. Swets & Zeitlinger: Lisse, The Netherlands, 2003.
Van Zelst WH, De Beurs E, Beekman ATF, Deeg DJH, Bramsen I, Van Dyck R . Criterion validity of the self-rating inventory for posttraumatic stress disorder (SRIP) in the community of older adults. J Affect Disord 2003; 76: 229–235.
Sinclair D, Fullerton JM, Webster MJ, Weickert CS . Glucocorticoid receptor 1B and 1C mRNA transcript alterations in schizophrenia and bipolar disorder, and their possible regulation by GR gene variants. PLoS ONE 2012; 7: e31720.
Liu T, Zhang X, So CK, Wang S, Wang P, Yan L et al. Regulation of Cdx2 expression by promoter methylation, and effects of Cdx2 transfection on morphology and gene expression of human esophageal epithelial cells. Carcinogenesis 2007; 28: 488–496.
Brakensiek K, Wingen LU, Länger F, Kreipe H, Lehmann U . Quantitative high-resolution CpG island mapping with pyrosequencing reveals disease-specific methylation patterns of the CDKN2B gene in myelodysplastic syndrome and myeloid leukemia. Clin Chem 2007; 53: 17–23.
England R, Pettersson M . Pyro Q-CpG TM: quantitative analysis of methylation in multiple CpG sites by Pyrosequencing®. Nat Methods 2005; i–ii.
Yehuda R, Daskalakis NP, Lehrner A, Desarnaud F, Bader HN, Makotkine I et al. Influences of maternal and paternal PTSD on epigenetic regulation of the glucocorticoid receptor gene in Holocaust survivor offspring. Am J Psychiatry 2014; 171: 872–880.
Yehuda R, Daskalakis NP, Desarnaud F, Makotkine I, Lehrner AL, Koch E et al. Epigenetic biomarkers as predictors and correlates of symptom improvement following psychotherapy in combat veterans with PTSD. Front Psychiatry 2013; 4: 1–14.
Yehuda R, Boisoneau D, Lowy MT, Giller EL . Dose–response changes in plasma cortisol and lymphocyte glucocorticoid receptors following dexamethasone administration in combat veterans with and without posttraumatic stress disorder. Arch Gen Psychiatry 1995; 52: 583–593.
Clayton D SNPHAP. Version 1.3.1. installed in HIPPUe. 2004. Available at http://www.csc.fi/english/research/sciences/bioscience/programs/snphap/index_html.
Pinheiro J, Bates D, DebRoy S, Sarkar D R Development Core Team. nlme: linear and nonlinear mixed effects models. R Package version 31-122, 2015, pp 1–3. Available at http://CRAN.R-project.org/package=nlme..
NCAR—Research Applications Laboratory. Verification: weather forecast verification utilities. R package version 1.42. 2015. Available at http://CRAN.R-project.org/package=verification.
Carstensen B, Plummer M, Laara EHM Epi: a package for statistical analysis in epidemiology. R Package version 1.1.44. 2013. Available at http://cran.r-project.org/package=Epi.
Tyrka AR, Price LH, Marsit C, Walters OC, Carpenter LL . Childhood adversity and epigenetic modulation of the leukocyte glucocorticoid receptor: Preliminary findings in healthy adults. PLoS ONE 2012; 7: e30148.
Perroud N, Salzmann A, Prada P, Nicastro R, Hoeppli ME, Furrer S et al. Response to psychotherapy in borderline personality disorder and methylation status of the BDNF gene. Transl Psychiatry 2013; 3: e207.
van Zuiden M, Heijnen CJ, Maas M, Amarouchi K, Vermetten E, Geuze E et al. Glucocorticoid sensitivity of leukocytes predicts PTSD, depressive and fatigue symptoms after military deployment: a prospective study. Psychoneuroendocrinology 2012; 37: 1822–1836.
Van Zuiden M, Geuze E, Willemen HLDM, Vermetten E, Maas M, Heijnen CJ et al. Pre-existing high glucocorticoid receptor number predicting development of posttraumatic stress symptoms after military deployment. Am J Psychiatry 2011; 168: 89–96.
Witzmann SR, Turner JD, Meriaux SB, Meijer OC, Muller CP . Epigenetic regulation of the glucocorticoid receptor promoter 17 in adult rats. Epigenetics 2012; 7: 1290–1301.
Li-Tempel T, Larra MF, Sandt E, Mériaux SB, Schote AB, Schächinger H et al. The cardiovascular and hypothalamus-pituitary-adrenal axis response to stress is controlled by glucocorticoid receptor sequence variants and promoter methylation. Clin Epigenet 2016; 8: 12.
Davies MN, Volta M, Pidsley R, Lunnon K, Dixit A, Lovestone S et al. Functional annotation of the human brain methylome identifies tissue-specific epigenetic variation across brain and blood. Genome Biol 2012; 13: R43.
Hannon E, Lunnon K, Schalkwyk L, Mill J . Interindividual methylomic variation across blood, cortex, and cerebellum: Implications for epigenetic studies of neurological and neuropsychiatric phenotypes. Epigenetics 2015; 10: 1024–1032.
Smith AK, Kilaru V, Kocak M, Almli LM, Mercer KB, Ressler KJ et al. Methylation quantitative trait loci (meQTLs) are consistently detected across ancestry, developmental stage, and tissue type. BMC Genomics 2014; 15: 145.
Reinius LE, Acevedo N, Joerink M, Pershagen G, Dahlén SE, Greco D et al. Differential DNA methylation in purified human blood cells: implications for cell lineage and studies on disease susceptibility. PLoS ONE 2012; 7: e41361.
Labonte B, Yerko V, Gross J, Mechawar N, Meaney MJ, Szyf M et al. Differential glucocorticoid receptor exon 1(B), 1(C), and 1(H) expression and methylation in suicide completers with a history of childhood abuse. Biol Psychiatry 2012; 72: 41–48.
Houtepen LC, Vinkers CH, Carrillo-Roa T, Hiemstra M, van Lier PA, Meeus W et al. Genome-wide DNA methylation levels and altered cortisol stress reactivity following childhood trauma in humans. Nat Commun 2016; 7: 10967.
Acknowledgements
This study was funded by a grant from the Dutch Ministry of Defence. Methylation and gene expression analyses were funded by the VENI fellowship from the Netherlands Organisation for Scientific Research (NWO, Grant Number 451.13.001) to CHV. We thank JW Deiman for creating Figure 1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Translational Psychiatry website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Schür, R., Boks, M., Rutten, B. et al. Longitudinal changes in glucocorticoid receptor exon 1F methylation and psychopathology after military deployment. Transl Psychiatry 7, e1181 (2017). https://doi.org/10.1038/tp.2017.150
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tp.2017.150
This article is cited by
-
Epigenetics of traumatic stress: The association of NR3C1 methylation and posttraumatic stress disorder symptom changes in response to narrative exposure therapy
Translational Psychiatry (2023)
-
Decreased mononuclear cell NR3C1 SKA2 and FKPB5 expression levels among adult survivors of suicide bombing terror attacks in childhood are associated with the development of PTSD
Molecular Psychiatry (2023)
-
Glucocorticoid receptor gene (NR3C1) is hypermethylated in adult males with aggressive behaviour
International Journal of Legal Medicine (2021)
-
DNA methylation of FKBP5 in South African women: associations with obesity and insulin resistance
Clinical Epigenetics (2020)
-
DNA Methylation Analysis of the NR3C1 Gene in Patients with Schizophrenia
Journal of Molecular Neuroscience (2020)