Abstract
Circulating insulin-like growth factor I (IGF-I) enters the brain and promotes clearance of amyloid peptides known to accumulate in Alzheimer's disease (AD) brains. Both patients and mouse models of AD show decreased level of circulating IGF-I enter the brain as evidenced by a lower ratio of cerebrospinal fluid/plasma IGF-I. Importantly, in presymptomatic AD mice this reduction is already manifested as a decreased brain input of serum IGF-I in response to environmental enrichment. To explore a potential diagnostic use of this early loss of IGF-I input, we monitored electrocorticogram (ECG) responses to systemic IGF-I in mice. Whereas control mice showed enhanced ECG activity after IGF-I, presymptomatic AD mice showed blunted ECG responses. Because nonhuman primates showed identically enhanced electroencephalogram (EEG) activity in response to systemic IGF-I, loss of the EEG signature of serum IGF-I may be exploited as a disease biomarker in AD patients.
Similar content being viewed by others
Introduction
Alzheimer's disease (AD) is a major public health concern worldwide. Decades of fruitless search for effective therapies has led to the suggestion that treatment is started too late in the course of the disease to be able to modify it. This is because available diagnostic tools, mostly relying on clinical scales in common practice, can only detect the disease when pathology is already very advanced. Hence, early diagnosis seems essential to establish earlier treatments.1 Two major types of efforts are ongoing in this direction. One is to develop new diagnostic tools based on advanced imaging protocols through functional magnetic resonance imaging or positron-emission tomography.2 The other is based on biochemical markers using proteomic/genomic analyses.3 Although the federal drug administration in the USA has recently approved the use of a positron-emission tomography amyloid marker for clinical use, general application of these costly techniques are not envisaged for the near future. More importantly, the recent guidelines of the US National Institute on Aging and the US Alzheimer’s Association provide a conceptual framework for defining the stages of preclinical AD in which staging requires a combination of biomarkers. In this regard, although proteomic/genomic signatures in AD patients have already been described,3, 4, 5 none have yet reached common practice. Therefore, there is an unmet need to better define the multidimensional risk in preclinical AD and develop accurate prediction models in order to decide those who should or should not receive the treatment.6
The continued failure to develop effective drugs based on the ‘amyloid cascade’ hypothesis (the most favored one) has led to revisit old ideas of the cause of AD and even to coin new hypotheses. A currently favored one holds that AD is a metabolic disease specifically affecting the brain. In this regard, deterioration of insulin signaling,7 and possibly also of the related hormone IGF-I,8 has been argued to have a role in brain metabolic impairments in AD. Although there are already abundant data supporting a role of insulin in AD, the evidence for a role of IGF-I in AD is gradually accumulating. For instance, IGF-I promotes brain amyloid (Aβ) clearance,9,10 whereas reduced entrance of serum IGF-I into the brain results in increased levels of Aβ in the brain.11 Because serum IGF-I enters the brain in an activity-dependent fashion12 and brain activity is dysregulated in AD brains,13 serum-to-brain traffic of IGF-I is probably disturbed in AD. Accordingly, we suggested that impaired serum IGF-I input to the brain due to a resistance state may herald AD pathology.14 Indeed, new evidence indicates that in postmortem AD brains there is a profound resistance to IGF-I,15 a finding recently replicated in AD mice.16 This is in agreement with a recently reported reduction of the cerebrospinal fluid (CSF)/plasma IGF-I ratio in AD patients.17 Hence, we now tested this hypothesis by introducing the notion that this impairment could be detected through clinically amenable tools such as the electroencephalogram (EEG). The latter assumption is based on the observation that systemic insulin produces rapid changes in EEG patterns in humans18 and that serum IGF-I modulates neuronal excitability.19 Our aim is to translate knowledge of the role of IGF-I in AD into an early diagnostic system.
Materials and methods
Animals
Adult (3–5 months old) male and female mice were used to minimize animal use. Control C57BL6/J wild-type (WT) mice were used. APPswe and PS1Δ9 mice of C57BL6/J background were a kind gift from P. Mouton (National Institutes of Health). Although no gender differences were observed in any of the parameters measured under our experimental conditions, the proportion of females for each experimental group was kept within 30–60%. Nine adult macaques purchased from R.C. Hartelust BV (Tilburg, The Netherlands) and aged 14 years and weighing ∼8 kg were used. Saline and IGF-I injections were given on separate days. Monkeys were housed at the monkey facility of the Faculty of Medicine at UAM (register number EX 021-U). Animal procedures followed European guidelines (86/609/EEC and 2003/65/EC, European Council Directives) and approval of local Bioethics Committees was obtained.
Human samples
We obtained CSF and plasma from 35 subjects with Alzheimer dementia and 10 age-matched healthy controls. Experimental procedures were approved by the corresponding Ethics Committees. Patients underwent an extensive neuropsychological evaluation20 including Mini-Mental State Examination scores of 16–26. All participants gave written consent for the study. Plasma and CSF were obtained from each subject following established procedures. Samples were processed and stored at −80 °C until analysis.
Environmental enrichment
Animals were under inverted circadian cycle conditions for 1 week before enrichment (dark: 0500–1700; light: 1700–0500). Then, they were split into two groups: control animals, that remained under standard housing conditions (370–530 cm2 cage, 2–5 mice per cage and no objects) and enriched animals, placed for 2 h in a large cage (1815 cm2), 10 animals per cage and with different objects (cardboard tunnels, shelters of different materials, a plastic net, toys, chewable and nesting material). Thereafter, animals were anesthetized with pentobarbital and killed by transcardiac perfusion.
Immunoassays
Western blot and immune precipitation were performed as described.21 Mouse CSF and serum IGF-I were determined using species-specific commercially available enzyme-linked immunosorbent assays (R&D Systems, Minneapolis, MN, USA), as described.22 CSF samples were directly collected from the cisterna magna of pentobarbital anesthetized animals placed in a stereotaxic device before transcardiac perfusion.
Cell cultures and in vitro assays
Endothelial cell cultures were performed as described12 with minor modifications.
Electrocorticogram (ECG) and EEG recordings
The following number of animals were used in these studies: WT saline (n=9): 3±0 months; WT-IGF-I (n=14): 3±0; APP/PS1 (n=7): 3.52±0.44; APP (n=7): 3.75±0.53. Mice were anesthetized with isoflurane (2–3% for induction) mixed with O2 (0.5–1 l min−1) and placed in a stereotaxic device. The skin was cut along midline and a craniotomy made (0.5 mm diameter) on the primary somatosensory area (S1). A tungsten macroelectrode of 0.5 MΩ was placed without disrupting the meninges to register the cortical electrical activity (EEG). After surgery the isoflurane concentration was reduced to 0.5–1.5%, depending on individual requirements, to obtain absence of reflexes and a stable slow wave ECG. EEG baseline was registered during 20 min (control period) and then saline or 25 μg IGF-I (in 100 μl saline) was injected intraperitoneally. EEG was recorded during 60 min after the injection. The cortical electrical activity was filtered between 0.3 and 30 Hz and amplified by a P15 Grass amplifier (Warwick, RI, USA). Signals were stored in a PC through an analogic–digital converter card (1401, Cambridge Electronic Design, Cambridge, UK) for off-line analysis with Spike 2 software (Cambridge Electronic Design) at a sampling frequency of 100 Hz.
For primate studies, monkeys were starved overnight before the experiment to avoid potential hypoglycemia due to intravenous IGF-I administration. Animals were sedated with an intramuscular injection of ketamine (5–10 mg kg−1) and anesthetized with isoflurane (2–4% for induction and 1–1.5% for maintenance) mixed with O2 (2 l min−1 for induction and 1.5 l min−1 for maintenance). EEG recording began 30 min later to assure ketamine clearing and to get a stable slow wave EEG. Blood glucose levels were monitored and clamped at a euglycemic level (Macaca fascicularis: 50–70 mg dl−1; Macaca mulatta: 40–60 mg dl−1) with a 3.3% gluco-saline solution infused systemically through the saphenous vein. EEG recordings were performed from three surface electrodes placed in Fpz, Cz y Oz according to the International 10–20 System. A conductive electrode gel was placed between the skin and the electrode to improve signal recording. The experimental protocol was the same as in mice except that both saline and IGF-I (100 μg kg−1 diluted to 1 mg ml−1 in saline solution) were administered as an intravenous bolus in the saphenous vein. Signal recordings were performed as described above.
ECG and EEG segments of 5 min were analyzed by Spike 2 software, using the fast Fourier transform algorithm to obtain the power spectra. The mean power density was calculated for four different frequency bands that constitute the global EEG: δ-band (0.3–4 Hz), θ-band (4–8 Hz), α-band (8–12 Hz) and β-band (12–30 Hz). Every 5 min the percentage of contribution of each band to the global wavelength of the EEG (band power × 100/total band powers) was calculated and normalized against the baseline (calculated as the mean value of the 20 min before the injection of saline or IGF-I). Results were plotted in the figures as fold increase value for each band every 5 min. For each animal, we calculated the area under the curve (AUC) of the 60 min after injection using the trapezoidal rule. Mean values of AUC of the β-wave (AUC) of each group were plotted against the corresponding value of phosphoIGF-IR/IGF-IR (IGF-I receptor) after environmental enrichment. For that, WT saline was matched with WT control and IGF-I-injected animals were matched with enriched animals.
Statistical analysis
Statistical analysis was performed using GraphPad Prism 5 software (San Diego, CA, USA). All results are shown as mean±s.e.m. For single comparisons, we used Student’s t-test and for multiple comparisons, one or two-way analysis of variance plus Bonferroni’s multiple comparison test as post-hoc test. Probability values <0.05 were considered significant.
Results
Impaired serum IGF-I input to the brain in AD
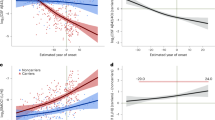
We first corroborated that the CSF/plasma ratio of IGF-I is reduced in AD patients as compared with age-matched controls (Figure 1a and Supplementary Table 1). In agreement with recently published interpretations of this observation,17 we considered that this reduction reflects impaired entrance of IGF-I from serum to CSF in AD patients. A similarly reduced CSF/serum IGF-I ratio was found in APP/PS1 and APP mice, two well-established models of familial AD (Figure 1b, Table 1 and Supplementary Table 2). Therefore we considered that APP/PS1 mice may constitute a valid model to investigate early loss of serum IGF-I input to the brain associated to AD pathology. We explored in detail this possibility.
Evidence of reduced serum insulin-like growth factor I (IGF-I) input in Alzheimer's disease (AD). (a) The cerebrospinal fluid (CSF)/serum IGF-I ratio is significantly reduced in Alzheimer patients (n=35); **P<0.01 vs age-matched controls (n=10). (b) The CSF/serum IGF-I ratio is also decreased in young APP (n=6) and APP/PS1 AD-like mice (n=17). WT: age-matched wild-type controls (n=10). Serum IGF-I and CSF were collected from the same individuals to calculate ratios (F=8.538, *P<0.05 and ***P<0.001 vs WT). (c) Phosphorylation of the hippocampal IGF-I receptor in response to environmental enrichment is reduced in AD mice. Both single (APP) and double-mutant (APP/PS1) mice showed reduced IGF-I receptor activity as compared with controls (n=72). After immunoprecipitation with anti-IGF-IR (IGF-I receptor), membranes were blotted with anti-pTyr antibody (4G10, upper blot), stripped and re-blotted with anti-IGF-IR (lower blot) to normalize for total load. Number of animals is indicated on the bars. White bars are animals housed under standard conditions and filled bars are enriched animals (F=15.64, *P<0.05 and ***P<0.001 vs WT). (d) Soluble amyloid (Aβ) reduces in a dose-dependent manner the amount of biotin-labeled IGF-I accumulated by cultured brain endothelial cells (n=3–4; F=10.95, *P<0.05 and ***P<0.001).
As previously shown,12 transient exposure of mice to enriched environment (EE) increased phosphorylation of the IGF-IR in the hippocampus (Figure 1c), a brain area actively engaged by this multisensory stimulation (Supplementary Figure 1). Other brain areas such as the cerebellum showed similar increases (Supplementary Figure 2A), albeit slightly smaller. As previously found, this increased phosphorylation of the IGF-IR resulted from increased uptake of serum IGF-I by the brain in response to neuronal activation, rather than from local release of brain IGF-I.12 Accordingly, liver-deficient IGF-I mice,23 which have very low serum IGF-I levels (Table 1), did not show increased IGF-IR phosphorylation in response to EE (Supplementary Figure 2B). Taking advantage of the stimulatory effect of enrichment on hippocampal IGF-IR phosphorylation, we tested whether in AD mice this stimulation leads to similar effects. First, we exposed APP/PS1 mice with Aβ pathology (Supplementary Figure 3) to EE. Contrary to what we observed in WT mice, 4-month-old APP/PS1 mice did not show increased hippocampal IGF-IR phosphorylation in response to EE (Figure 1c). Then we used another model of AD mice with no signs of pathology (Supplementary Figure 3). In this case, 3–5-month-old APP mice, that take a much longer time to develop AD-like amyloidosis than the double-mutant APP/PS1, showed significantly attenuated phosphorylation of the hippocampal IGF-IR after EE (Figure 1c). We measured serum IGF-I in APP/PS1 and APP mice to rule out that this deficit was not due to low serum levels and found them to be similar to that in control mice (Table 1). Also, basal levels of hippocampal IGF-IR in AD mice were similar to that in control mice (Supplementary Figure 4), whereas, as already documented in human AD brains,15 AD mice show increased Ser616 phosphorylation of insulin receptor substrate 1 (Supplementary Figure 4B), a recognized index of insulin/IGF-I resistance.24 Collectively these data suggest that AD mice show early disturbances in serum IGF-I input to the brain due to a resistant state.
To reach the brain, blood-borne IGF-I is internalized by brain endothelial cells and through transcytosis reaches the brain parenchyma.12 Thus, we determined whether uptake of IGF-I by endothelial cells is affected by Aβ, which has an important role in AD pathogenesis. We found that Aβ1–40 dose-dependently decreased IGF-I internalization by brain endothelial cells (Figure 1d). Because internalization of serum IGF-I by brain endothelia requires interaction of the IGF-IR with LRP-1,12 a multicargo membrane transporter possibly associated with risk of AD,25 we examined whether levels of this receptor differ among experimental groups, however, no differences were observed (Supplementary Figure 4C).
Loss of serum IGF-I input as an early biomarker of AD
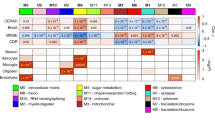
We next explored the potential use of this early loss of neurotrophic input in AD mice as a biomarker of disease onset. To this end, we compared the ECG signature of systemically injected IGF-I (1 μg g−1; intraperitoneal) in AD mice vs control mice. As shown in Figure 2, IGF-I elicited a small decrease in δ-band together with a robust increase in θ-, α- and β-bands (P<0.001 by two-way analysis of variance for all bands) in anesthetized WT mice, whereas in age-matched anesthetized APP mice the response was markedly attenuated. Confirming the greater loss of serum IGF-I input observed in double-mutant APP/PS1 mice (Figure 1), their ECG response to IGF-I was fully blunted (Figure 2). Analysis of ECG stimulation over baseline after a latency of 20 min (the time it takes for IGF-I to consistently alter ECG activity) up to 60 min after IGF-I administration showed significant differences in all the bands in WT mice, whereas both APP and APP/PS1 mice showed no significant changes (Figure 3). Nevertheless, although not significantly different from baseline values, APP mice show an attenuated response to IGF-I. To rule out a nonspecific loss of IGF-I activity in humanized mouse models of neurodegenerative diseases, we examined the ECG signature of IGF-I in transgenic mice bearing a human Friedreich's ataxia transgene26 and found a response similar to WT mice (Supplementary Figure 5). Hippocampal IGF-IR phosphorylation after enrichment could predict ECG signatures after IGF-I injection as higher phosphorylation rates (measured as pIGF-IR/IGF-IR ratio) were directly related to higher ECG activity (Supplementary Figure 6). This suggests that the ECG signature reliably reflects brain sensitivity to systemic IGF-I. Finally, to ascertain the suitability of this method for human studies, we tested whether this ECG pattern in response to IGF-I is seen in EEG recordings in nonhuman primates because of their closer phylogenic proximity to humans, and because EEG is amenable for clinical screening. Figure 4 shows increased EEG activity in the frontal cortex of euglycemic macaque monkeys after an intravenous bolus of IGF-I (100 μg kg−1) reminiscent of that seen in the ECG recordings of WT mice.
Electrocorticogram (ECG) signature of systemic insulin-like growth factor I (IGF-I) in control animals is strongly attenuated in Alzheimer’s disease (AD) mice. Intraperitoneal administration of IGF-I in anesthetized animals induces a pronounced increase of α-, β- and θ-band frequencies in the ECG of wild-type (WT) mice (n= 14) as compared with WT injected with saline (n=9), whereas no changes are seen in APP/PS1 mice (n=7) and in presymptomatic APP mice (n=7).
Loss of electrocorticogram (ECG) signature in Alzheimer’s disease (AD) mice. Insulin-like growth factor I (IGF-I) induces significant increases in α, β and θ ECG frequency bands and a decrease in δ-wave in control animals. In contrast, both double- and single-mutant AD mice showed no changes. Average changes in ECG bands from 20 to 60 min after IGF-I injection were compared with average baseline levels (paired t-test: **P<0.01, ***P<0.001 vs baseline).
Changes elicited by systemic insulin-like growth factor I (IGF-I) in the electroencephalogram (EEG) activity of anesthetized macaque monkeys. Increased α, β and θ EEG frequency bands are elicited in macaques (n=9) after systemic injection of IGF-I. Note that the response is identical to that seen in wild-type mice but slightly faster because IGF-I was administered intravenously.
Discussion
Early disruption of the entrance of serum IGF-I into the brain of AD mice supports a pathogenic significance of this disturbance in AD.14 In this regard we reported that reduced IGF-I signaling at the blood–CSF barrier in choroid plexus epithelium elicited AD-like pathology in healthy young rats, including cognitive loss, amylodosis and tauopathy.11 Others reported increases in various indicators of IGF-I resistance in the brain of AD patients15,27,28 and more recently, in APP/PS1 mice.16 Changes in systemic IGF components have also been proposed as biomarkers of AD.17,29 Indeed, we confirmed the existence of reduced traffic of serum-to-CSF IGF-I in AD patients,17 a reduction replicated in AD mice. This reinforces the notion that these animal models provide useful information about the human condition. The fact that the EEG signature of systemic IGF-I in healthy animals is shared by relatively distant species (mice and monkeys) opens the possibility to find a similar EEG signature in healthy humans. Nevertheless, human studies are needed to determine the potential use of EEG recordings after IGF-I challenge as an early screening system to define a population at risk of AD.
As recently confirmed in AD mice,16 Aβ interferes with insulin and IGF-I signaling.30 Accordingly, we observed that Aβ interferes with IGF-I uptake by brain endothelium, a process that requires the interaction of IGF-I with its receptor.12 This interference may explain the loss of serum IGF-I input not only in the very rare familial cases of AD with high levels of Aβs caused by mutations in presenilins and APP, but also in sporadic forms of AD (SAD). Recent evidence shows that Aβ also accumulates in induced pluripotent stem cells derived from SAD patients and elicits cell stress.31 Further, other processes related or not with Aβ load that may elicit endothelial cell dysfunction may intervene in SAD. These may include an inadequate diet (known to elicit stress of endoplasmic reticulum32), oxidative stress associated with aging, or life-style factors known to reduce serum IGF-I traffic to the brain such as sedentary life, peripheral infections or imbalanced diets.33,34 We suggest that in SAD, these multiple factors negatively impinge on serum-to-brain IGF-I traffic.
Our findings open the possibility to diagnose AD earlier than that possible by the present methods. We believe this method could be implemented in humans for the following reasons: (i) there is extensive safety data for IGF-I; it is already approved for chronic use in children with Laron's dwarfism (see: http://www.drugs.com/pro/increlex.html) and our method is based on a single injection of IGF-I; (ii) EEG recordings are of routine use in clinical practice as easy, cheap and noninvasive explorations; and (iii) validation of the method could be carried out along the AD continuum in SAD and also in familial AD cases. An abnormal EEG response to IGF-I might therefore prove useful to better define a subpopulation of patients in preclinical AD as a biomarker that adds to the multidimensional risk assessment in these subjects or as a surrogate response to treatment. Perhaps more importantly, such a biomarker might be useful to develop preventive schemes including physical exercise, adequate diet or even early treatment with IGF-I or its mimetics35, 36, 37, 38 in a population in which such long-term interventions might have special interest and rationale.
References
Sinha G . European scientists push spinal taps for Alzheimer diagnosis. Nat Med 2006; 12: 156.
Perrin RJ, Fagan AM, Holtzman DM . Multimodal techniques for diagnosis and prognosis of Alzheimer's disease. Nature 2009; 461: 916–922.
Ray S, Britschgi M, Herbert C, Takeda-Uchimura Y, Boxer A, Blennow K et al. Classification and prediction of clinical Alzheimer's diagnosis based on plasma signaling proteins. Nat Med 2007; 13: 1359–1362.
Fjell AM, Walhovd KB, Fennema-Notestine C, McEvoy LK, Hagler DJ, Holland D et al. CSF biomarkers in prediction of cerebral and clinical change in mild cognitive impairment and Alzheimer's disease. J Neurosci 2010; 30: 2088–2101.
Villemagne VL, Perez KA, Pike KE, Kok WM, Rowe CC, White AR et al. Blood-borne amyloid-{beta} dimer correlates with clinical markers of Alzheimer's disease. J Neurosci 2010; 30: 6315–6322.
Sperling R, Johnson K . Biomarkers of Alzheimer disease: current and future applications to diagnostic criteria. Continuum (Minneap Minn) 2013; 19: 325–338.
Blum-Degen D, Frolich L, Hoyer S, Riederer P . Altered regulation of brain glucose metabolism as a cause of neurodegenerative disorders? J Neural Transm Suppl 1995; 46: 139–147.
Carro E, Trejo JL, Gomez-Isla T, LeRoith D, Torres-Aleman I . Serum insulin-like growth factor I regulates brain amyloid-beta levels. Nat Med 2002; 8: 1390–1397.
Carro E, Torres-Aleman I . Serum insulin-like growth factor I in brain function. Keio J Med 2006; 55: 59–63.
Saenger S, Goeldner C, Frey JR, Ozmen L, Ostrowitzki S, Spooren W et al. PEGylation enhances the therapeutic potential for insulin-like growth factor I in central nervous system disorders. Growth Hormone & IGF Research 2011; 21: 292–303.
Carro E, Trejo JL, Spuch C, Bohl D, Heard JM, Torres-Aleman I . Blockade of the insulin-like growth factor I receptor in the choroid plexus originates Alzheimer's-like neuropathology in rodents: new cues into the human disease? Neurobiol Aging 2006; 27: 1618–1631.
Nishijima T, Piriz J, Duflot S, Fernandez AM, Gaitan G, Gomez-Pinedo U et al. Neuronal activity drives localized blood-brain-barrier transport of serum insulin-like growth factor-I into the CNS. Neuron 2010; 67: 834–846.
Jones DT, Machulda MM, Vemuri P, McDade EM, Zeng G, Senjem ML et al. Age-related changes in the default mode network are more advanced in Alzheimer disease. Neurology 2011; 77: 1524–1531.
Carro E, Torres-Aleman I . The role of insulin and insulin-like growth factor I in the molecular and cellular mechanisms underlying the pathology of Alzheimer's disease. Eur J Pharmacol 2004; 490: 127–133.
Talbot K, Wang HY, Kazi H, Han LY, Bakshi KP, Stucky et al. Demonstrated brain insulin resistance in Alzheimer's disease patients is associated with IGF-1 resistance, IRS-1 dysregulation, and cognitive decline. J Clin Invest 2012; 122: 1316–1338.
Zhang B, Tang XC, Zhang HY . Alternations of central insulin-like growth factor-1 sensitivity in APP/PS1 transgenic mice and neuronal models. J Neurosci Res 2013; 91: 717–725.
Johansson P, Aberg D, Johansson JO, Mattsson N, Hansson O, Ahrén B et al. Serum but not cerebrospinal fluid levels of insulin-like growth factor-I (IGF-I) and IGF-binding protein-3 (IGFBP-3) are increased in Alzheimer's disease. Psychoneuroendocrinology 2013; 38: 1729–1737.
Tschritter O, Preissl H, Hennige AM, Stumvoll M, Porubska K, Frost R et al. The cerebrocortical response to hyperinsulinemia is reduced in overweight humans: a magnetoencephalographic study. PNAS 2006; 103: 12103–12108.
Nunez A, Carro E, Torres-Aleman I . Insulin-like growth factor I modifies electrophysiological properties of rat brain stem neurons. J Neurophysiol 2003; 89: 3008–3017.
Sala I, Belen Sanchez-Saudinos M, Molina-Porcel L, Lázaro E, Gich I, Clarimón J et al. Homocysteine and cognitive impairment. Relation with diagnosis and neuropsychological performance. Dement Geriatr Cogn Disord 2008; 26: 506–512.
Fernandez AM, Jimenez S, Mecha M, Dávila D, Guaza C, Vitorica J et al. Regulation of the phosphatase calcineurin by insulin-like growth factor I unveils a key role of astrocytes in Alzheimer's pathology. Mol Psychiatry 2012; 17: 705–718.
Trejo JL, Piriz J, Llorens-Martin MV, Fernandez AM, Bolós M, LeRoith D et al. Central actions of liver-derived insulin-like growth factor I underlying its pro-cognitive effects. Mol Psychiatry 2007; 12: 1118–1128.
Yakar S, Liu JL, Stannard B, Butler A, Accili D, Sauer B et al. Normal growth and development in the absence of hepatic insulin-like growth factor I. Proc Natl Acad Sci USA 1999; 96: 7324–7329.
Aguirre V, Werner ED, Giraud J, Lee YH, Shoelson SE, White MF . Phosphorylation of Ser307 in insulin receptor substrate-1 blocks interactions with the insulin receptor and inhibits insulin action. J Biol Chem 2002; 277: 1531–1537.
Wavrant-DeVrieze F, Perez-tur J, Lambert JC, Frigard B, Pasquier F, Delacourte et al. Association between the low density lipoprotein receptor-related protein (LRP) and Alzheimer's disease. Neurosci Lett 1997; 227: 68–70.
Al-Mahdawi S, Pinto RM, Varshney D, Lawrence L, Lowrie MB, Hughes S et al. GAA repeat expansion mutation mouse models of Friedreich ataxia exhibit oxidative stress leading to progressive neuronal and cardiac pathology. Genomics 2006; 88: 580–590.
Moloney AM, Griffin RJ, Timmons S, O'Connor R, Ravid R, O'Neill C . Defects in IGF-1 receptor, insulin receptor and IRS-1/2 in Alzheimer's disease indicate possible resistance to IGF-1 and insulin signalling. Neurobiol Aging 2010; 31: 224–243.
Steen E, Terry BM, Rivera EJ, Cannon JL, Neely TR, Tavares R et al. Impaired insulin and insulin-like growth factor expression and signaling mechanisms in Alzheimer's disease--is this type 3 diabetes? J Alzheimers Dis 2005; 7: 63–80.
Toledo JB, Da X, Bhatt P, Wolk DA, Arnold SE, Shaw LM et al. Relationship between plasma analytes and SPARE-AD defined brain atrophy patterns in ADNI. PLoS ONE 2013; 8: e55531.
Zhao WQ, De Felice FG, Fernandez S, Chen H, Lambert MP, Quon MJ et al. Amyloid beta oligomers induce impairment of neuronal insulin receptors. FASEB J 2007; 22: 246–260.
Kondo T, Asai M, Tsukita K, Kutoku Y, Ohsawa Y, Sunada Y et al. Modeling Alzheimers disease with iPSCs reveals stress phenotypes associated with intracellular a¦ and differential drug responsiveness. Cell Stem Cell 2013; 12: 487–496, Ref Type: Abstract.
Ozcan U, Cao Q, Yilmaz E, Lee AH, Iwakoshi NN, Ozdelen E et al. Endoplasmic reticulum stress links obesity, insulin action, and type 2 diabetes. Science 2004; 306: 457–461.
Fernandez AM, Torres-Aleman I . The many faces of insulin-like peptide signalling in the brain. Nat Rev Neurosci 2012; 13: 225–239.
Dietrich MO, Muller A, Bolos M, Carro E, Perry ML, Portela LV et al. Western style diet impairs entrance of blood-borne insulin-like growth factor-1 into the brain. Neuromolecular Med 2007; 9: 324–330.
Dodart JC, Mathis C, Bales KR, Paul SM, Ungerer A . Early regional cerebral glucose hypometabolism in transgenic mice overexpressing the V717F beta-amyloid precursor protein. Neurosci Lett 1999; 277: 49–52.
Carro E, Trejo JL, Gerber A, Loetscher H, Torrado J, Metzger F et al. Therapeutic actions of insulin-like growth factor I on APP/PS2 mice with severe brain amyloidosis. Neurobiol Aging 2006; 27: 1250–1257.
Baker LD, Barsness SM, Borson S, Merriam GR, Friedman SD, Craft S et al. Effects of growth hormone-releasing hormone on cognitive function in adults with mild cognitive impairment and healthy older adults: results of a controlled trial . Arch Neurol 2012; 69: 1420–1429.
Baker LD, Bayer-Carter JL, Skinner J, Montine TJ, Cholerton BA, Callaghan M et al. High-intensity physical activity modulates diet effects on cerebrospinal amyloid-beta levels in normal aging and mild cognitive impairment. J Alzheimers Dis 2012; 28: 137–146.
Acknowledgements
This work has been supported by grants from the Spanish Ministry of Economy (Explora Program and SAF2010/17036 to IT-A and BFU2012/36107 to AN). Ángel Trueba-Sáiz holds an FPU fellowship of the Spanish Ministry of Education (ref. FPU AP2009-0372). We thank L Guinea, M Garcia and M Dominguez for their excellent help.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
AT-S, CC, AN and IT-A have filled a patent application describing this method as a diagnostic tool for AD. The remaining authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Trueba-Sáiz, A., Cavada, C., Fernandez, A. et al. Loss of serum IGF-I input to the brain as an early biomarker of disease onset in Alzheimer mice. Transl Psychiatry 3, e330 (2013). https://doi.org/10.1038/tp.2013.102
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tp.2013.102
Keywords
This article is cited by
-
Insulin-like growth factor I sensitization rejuvenates sleep patterns in old mice
GeroScience (2022)
-
Age-related decline in circulating IGF-1 associates with impaired neurovascular coupling responses in older adults
GeroScience (2022)
-
Endothelial deficiency of insulin-like growth factor-1 receptor (IGF1R) impairs neurovascular coupling responses in mice, mimicking aspects of the brain aging phenotype
GeroScience (2021)
-
IGF1R signaling regulates astrocyte-mediated neurovascular coupling in mice: implications for brain aging
GeroScience (2021)
-
Adenovirus-Mediated Transduction of Insulin-Like Growth Factor 1 Protects Hippocampal Neurons from the Toxicity of Aβ Oligomers and Prevents Memory Loss in an Alzheimer Mouse Model
Molecular Neurobiology (2020)