Abstract
The aim of this study was to identify factors predicting large post-void residual (PVR) (defined as ≥200 mL), an important unsolved problem, after an intravesical injection of onabotulinumtoxinA in patients with overactive bladder syndrome. The data showed that 133 of 290 patients had a large PVR after treatment. Multivariate analysis found that the baseline 3-day daytime frequency episodes and voiding efficiency were independent predictors for postoperative large PVR. A receiver operating characteristic (ROC) curve analysis showed the following optimum cut-off values: (1) 3-day daytime frequency episodes = 25, which has a ROC area of 0.72; and (2) voiding efficiency = 89%, which has a ROC area being 0.66. The predicted logit transformation of probability of large PVR, logit(p), for a given 3-day daytime frequency episodes (a) and voiding efficiency (b%) can be denoted by logit(p) = −5.18 + 0.07 × a + 0.04 × b, with a cutoff value of logit(p) = 0.34 and a ROC area of 0.79. The median value of the persistent large PVR interval was 5 months. In conclusion, low 3-day daytime frequency episodes (<25) and low voiding efficiency (<89%) are associated with large PVR. Besides, logit(p) <0.34 can be used to predict large PVR for its higher ROC area.
Similar content being viewed by others
Introduction
Overactive bladder syndrome (OAB) is characterized by urgency with or without urge incontinence and is usually associated with frequency and nocturia1. Antimuscarinic agents are the first-line treatment, with a success rate greater than 70%2. Both the presence of urothelial dysfunction and abnormalities of sensory receptor expression or transmitter release in the suburothelial nerves may contribute to OAB, which is refractory to antimuscarinics3. Thus, intravesical treatment to inhibit abnormal receptor expression or transmitter release in the suburothelial space has therapeutic effects in OAB patients4.
The intravesical injection of onabotulinum toxin type A has emerged as the treatment of choice in cases with OAB refractory to antimuscarinic therapy. The intravesical injection of onabotulinum toxin type A has both motor and sensory effects5. Despite the acceptable therapeutic effects obtained following the intravesical injection of onabotulinum toxin type A in OAB cases, the resulting detrusor contractility impairment and large post-void residual (PVR) remains an important unsolved problem for patients6,7,8,9.
Previous reports have demonstrated that large PVR develops significantly more often in men and in patients >61 years old. Large PVR is also observed in patients with a baseline maximum flow rate (Qmax) ≤15 ml/sec, PVR ≥ 100 ml, and voiding efficiency <90% after the intravesical injection of onabotulinum toxin type A10. Additionally, Liao et al. reported an increased risk of large PVR in frail elderly patients11. Wang et al. reported that diabetic patients had a significantly greater incidence of large PVR after treatment12. Furthermore, Kuo et al. found that the incidence of post-treatment large PVR was associated with medical comorbidities13. The study by Osborn et al. reported that the preoperative PVR and bladder capacity were associated with postoperative urine retention in a multivariate logistic regression14. However, age and diabetes were not associated with postoperative urine retention14. These conflicting results led us to identify the independent factors that can predict large PVR after intravesical onabotulinum toxin type A injection for patients with OAB. In addition, the secondary objective was to estimate the recovery time after the presence of postoperative large PVR and identify factors responsible for recovery.
Results
There were 290 patients who underwent intravesical onabotulinum toxin type A injection for OAB, and 133 patients (45.9%, male, n = 65 vs. female, n = 68, P = 0.50) who experienced large PVR (i.e., >200 mL) during the 6-month follow-up period.
Univariate analysis revealed the following baseline characteristics that were predictors for post-treatment large PVR: age, daytime frequency episodes, PVR, voiding efficiency and cystometric bladder capacity (Table 1). However, only daytime frequency episodes and voiding efficiency were independent predictors for post-treatment large PVR by backward stepwise multivariate logistic regression analysis (Table 1).
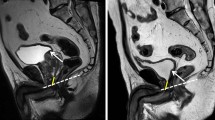
The following optimum cut-off values were determined using ROC analysis: (1) baseline 3-day daytime frequency episodes = 25, which has an area under the ROC curve of 0.72 (95% confidence interval [CI] = 0.60 to 0.84; sensitivity = 73.0%, specificity = 65.6%, Fig. 1A); and (2) baseline voiding efficiency = 89%, which has an area under the ROC curve of 0.66 (95% CI = 0.60 to 0.72; sensitivity = 70.1%, specificity = 56.1%, Fig. 1B).
By multivariate logistic regression analysis, baseline 3-day daytime frequency episodes (coefficient = 0.07, P = 0.005) and baseline voiding efficiency (coefficient = 0.04, P = 0.03) were determined to be the significant independent factors to predict the probability of the presence of large PVR with a constant of −5.18 (95% confidence interval [CI] = −8.66 to −1.69, P = 0.004). Thus, the predicted logit(p) for a given baseline 3-day daytime frequency episodes (a) and baseline voiding efficiency (b%) can be denoted by logit(p) = −5.18 + 0.07 × a + 0.04 × b. The mean and standard deviation of logit(p) was 0.14 and 1.31, respectively. Based on the ROC analysis, the optimum cut-off values of logit(p) = 0.34 were determined with the area under the ROC curve being 0.79 (95% confidence interval [CI] = 0.68 to 0.90; sensitivity = 67.6%, specificity = 84.4%, Fig. 1C).
The median value of the persistent large PVR interval was 5 months (95% CI = 2.5 to 5.5 months, Fig. 2). The baseline variables including age, gender, comorbidities, overactive bladder symptoms score (OABSS), bladder diary and video-urodynamic variables were not significant factors associated with predicting the persistent large PVR interval.
If we defined large PVR as >150 mL11, instead of >200 mL, 163 patients (56.2%) had PVR > 150 mL during the 6-month follow-up period. The baseline 3-day daytime frequency episodes and baseline voiding efficiency were the only significant independent predictors for post-treatment PVR > 150 mL, with similar odds ratios of 0.93 (95% CI = 0.89 to 0.98) and 0.93 (95% CI = 0.88 to 0.97), respectively. The ROC areas were 0.71 and 0.66, respectively. The median persistent PVR > 150 mL interval is 5.5 months (95% CI = 3 to 5.5 months, Fig. 3A). The data show that the male patients had a shorter persistent PVR > 150 mL interval than the female patients (median: male, 3 months, 95% CI = 2.5 to 5.5 months vs. female, 5.5 months, 95% CI = 5 to - months, log-rank test, P = 0.04, Fig. 3B).
Discussion
We successfully identified low voiding efficiency (<89%) as an independent factor for predicting post-treatment large PVR. However, variables such as age, comorbidities (including diabetes mellitus), baseline Qmax, PVR, Pdet.Qmax or bladder contractility index were not predictive factors. Previous studies have shown that age, comorbidities, baseline Qmax, PVR, Pdet.Qmax and bladder contractility index are associated with large PVR after intravesical onabotulinum toxin type A injection10,11,12,13,14. Comorbidities such as diabetes mellitus and Pdet.Qmax were not statistically significant in our univariate analysis (Table 1). Although age, baseline Qmax, PVR and bladder contractility index were statistically significant in our univariate analysis (Table 1), these variables failed to remain significant in multivariate analysis (Table 1). The finding of low voiding efficiency as a predictor is similar to the data reported by Jiang et al.10 and Hsiao et al.15.
Osborn et al. reported that preoperative PVR and bladder capacity were associated with postoperative urine retention in a multivariate logistic regression14. It is notable that if we excluded voiding efficiency as a variable in our multivariate backward stepwise logistic regression model, then baseline PVR becomes an independent predictor (odds ratio = 1.01, P = 0.04). This finding would be consistent with the data reported by Osborn et al.14. However, cystometric bladder capacity remains insignificant as a predictor. PVR and bladder capacity are components of voiding efficiency. Thus, voiding efficiency should be a better predictor than PVR and bladder capacity14.
We also identified a novel predictor (daytime frequency episodes) of post-treatment large PVR (Table 1). Low daytime frequency episodes (<25 episodes during 3 days) can also predict a high incidence of large PVR (Table 1, Fig. 1A). We excluded patients with detrusor underactivity for intravesical onabotulinum toxin type A injection; thus our OAB patients in this study should have intact bladder contractility16. From our finding (Table 1, Fig. 1A), the bladder contractility of OAB patients with high daytime frequency episodes would be less affected by onabotulinum toxin type A injection.
Previous studies reported that the following characteristics were associated with large PVR after treatment: male patients, >61 years old, baseline Qmax ≤15 mL/sec, PVR ≥ 100 mL, voiding efficiency <90%, comorbidities, and diabetes10,11,12,13. However, only comorbidities were identified by multivariate logistic regression analysis13, the other studies did not perform multivariate analysis10,11,12. Thus, our predictors for post-treatment large PVR should be more valuable and reliable.
In a previous study13, comorbidities (including diabetes mellitus, chronic kidney disease, chronic obstructive pulmonary disease and congestive heart failure in previous study) predicted large PVR (odds ratio = 2.2, P = 0.01)13. However, all comorbidities are not a predictor in the current study (odds ratio = 1.20, P = 0.45, Table 1). If we use 4 comorbidities (including variables of diabetes mellitus, chronic kidney disease, chronic obstructive pulmonary disease and congestive heart failure as previous study13), instead of all cormorbidities (Table 1), the variable remains insignificant as a predictor of large PVR (odds ratio = 1.23, P = 0.38). Thus, the impact of comorbidities on the post-treatment PVR requires further clarification.
We also found that the median bladder recovery time for patients experiencing large PVR is 5 months (Fig. 2), despite the intravesical onabotulinum toxin type A injection may remain therapeutically effective in patients for up to 1 year13. Besides, from the finding of Fig. 3B, male patients had a faster recovery from large PVR than female patients. These data should be valuable for patient consultations.
A limitation of this study is the retrospective design. However, the large sample size and multivariate backward stepwise logistic regression analysis performed in this study should make our analysis reliable and valuable. In addition, because the ROC areas of daytime frequency episodes and voiding efficiency were low, the proposed cut-off values might be less useful. However, logit(p) had a higher ROC area, thus the proposed cut-off value (0.34) of logit(p) can provide a valuable reference for physicians to select appropriate OAB patients for intravesical onabotulinum toxin type A injection.
In conclusion, low 3-day daytime frequency episodes (<25) and low voiding efficiency (<89%) are associated with large PVR. Besides, logit(p) <0.34 can be used to predict large PVR for its higher ROC area. The median recovery time for large PVR was 5 months. Our findings can be used as an initial guide for intravesical onabotulinum toxin type A injection in patients with refractory OAB.
Methods
This study was a retrospective investigation of 290 OAB patients who were treated with intravesical injection of 100 U of onabotulinum toxin type A (Allergan, Irvine, CA, USA) from 2005 to 2014. All patients received their first onabotulinum toxin type A injection.
The indications of intravesical onabotulinum toxin type A injection were OAB patients who were refractory to antimuscarinic treatment. The duration of previous antimuscarinic treatment was at least 3 months. All patients had been treated with at least two different antimuscarinic agents and were still bothered by severe urgency or urgency incontinence of at least one episode per day. All patients were free of urinary tract infections, intrinsic sphincter deficiency, and neurogenic bladder at the time of study enrolment.
The Research Ethics Committee of Hualien Tzu Chi Hospital approved the study. The corresponding author confirmed that all methods were performed in accordance with relevant guidelines and regulations. This study is a post hoc analysis of a previous study10. All patients were informed about the possible adverse events after onabotulinum toxin type A injection, and written informed consent was obtained from all patients before treatment. All patients received intravesical suburethelial injections totalling 100 U of onabotulinum toxin type A in the bladder body and excluding the trigone.
The video-urodynamic study was routinely performed for the diagnosis of detrusor over activity, bladder outlet obstruction, and intrinsic sphincter deficiency using Life-Tech urodynamics equipment (Stafford, Texas, USA). Women with bladder outlet obstruction and detrusor underactivity were also excluded from this study. A bladder outlet obstruction was defined as the radiologic evidence of bladder outlet narrowing, a voiding detrusor pressure greater than 35 cmH2O and a Qmax less than 15 mL/s or a voiding detrusor pressure greater than 40 cmH2O17. If patients did not have a voiding detrusor contractility of more than 10 cmH2O and needed to void by abdominal straining or were unable to void, then detrusor underactivity was diagnosed18. The urodynamic parameters of the first sensation of filling, full sensation, cystometric bladder capacity, bladder compliance, Qmax, PVR, voiding detrusor pressure at Qmax (Pdet.Qmax), bladder contractility index (defined as Pdet.Qmax +5 × Qmax)19, and voiding efficiency (defined as voided volume/ bladder capacity ×100%)19 were measured and recorded in detail.
A three-day voiding diary20, uroflowmetry for Qmax, voided volume and PVR was performed at each visit. PVR was measured by transabdominal ultrasound at each visit to the outpatient clinic. The bladder capacity was derived from the sum of the voided volume and PVR.
The urgency severity scale (USS) was measured using a modified version of the validated Indevus Urgency Severity Scale. The USS rates urgency severity as 0, 1, 2, or 3 and is defined as none, mild, moderate, and severe urgency, respectively21. We defined urgency incontinence as an urgency incontinence score of 4. The overactive bladder symptom score (OABSS)22 was also measured at each visit. OAB-wet was diagnosed by the presence of at least one episode of urgency incontinence in the 3-day voiding diary. The remaining patients were considered OAB-dry.
The therapeutic efficacy was graded using the Global Response Assessment (GRA) and categorized as −3, −2, −1, 0, 1, 2, and 3, indicating markedly worse, moderately worse, mildly worse, no change, mildly improved, moderately improved, and markedly improved bladder symptoms, respectively. The patients were closely monitored by personal interview and reported their subjective perception of the bladder condition at 2 weeks, 1, 3, and 6 months after the onabotulinum toxin type A injection. These results were combined with the improvement of OAB symptoms and any adverse effects after onabotulinum toxin type A treatment. A GRA score ≥2 at 3 months after onabotulinum toxin type A injection was defined as a successful treatment23.
STATA software (Version 11.0; Stata Corp, College Station, TX, USA) was used for statistical analyses. The variables in the univariate regression analysis included age, gender, OAB-wet or OAB-dry, comorbidities, OABSS, USS scores, 3-day voiding diary and urodynamic variables. Multivariate backward stepwise logistic regression analysis was performed using the variables with P < 0.25 from univariate analysis24. A P value of less than 0.05 was considered statistically significant. Receiver operating characteristic (ROC) curve analysis was performed to identify the optimum cut-off value for predicting post-treatment large PVR (defined as ≥200 mL). The optimal cut-off value was determined by the point on the ROC curve closest to the upper left-hand corner. In addition, multivariate logistic regression analysis including all significant factors was performed to predict the probability of large PVR (=p) and obtain logit transformation logit(p)25,26. With all patients’ values derived from the equation of logit(p), ROC curve analysis was performed to identify optimum cutoff value.
The persistent large PVR interval was measured from the date of first documented large PVR during the follow-up visits to the date of documented absence of large PVR and afterwards or last follow-up. The survival curve of the persistent large PVR interval was estimated using the Kaplan-Meier method. The P values of between-group differences were calculated from the log-rank test27. A Cox proportional-hazards model was used to assess the factors affecting the persistent large PVR interval.
Additional Information
How to cite this article: Hsiao, S.-M. et al. Urodynamic prognostic factors for large post-void residual urine volume after intravesical injection of onabotulinumtoxinA for overactive bladder. Sci. Rep. 7, 43753; doi: 10.1038/srep43753 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Abrams, P. et al. The standardisation of terminology of lower urinary tract function: Report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 21, 167–178 (2002).
Chapple, C. R. Muscarinic receptor antagonist in the treatment of overactive bladder. Urology 55, 33–50 (2000).
Yiangou, Y. et al. Capsaicin receptor VR1 and ATP-gated ion channel P2X3 in human urinary bladder. BJU Int 87, 774–779 (2001).
Apostolidis, A. et al. Decreased sensory receptors P2X3 and TRPV1 in suburothelial nerve fibers following intradetrusor injections of Botulinum toxin for human detrusor overactivity. J Urol 174, 977–982 (2005).
Kuo, H. C. Reduction of urgency severity is associated with long-term therapeutic effect after intravesical onabotulinumtoxin A injection for idiopathic detrusor overactivity. Neurourol Urodyn 30, 1497–1502 (2011).
Kuo, H. C. Urodynamic evidence of effectiveness of botulinum A toxin injection in treatment of detrusor overactivity refractory to anticholinergic agents. Urology 63, 868–872 (2004).
Sahai, A., Khan, M. S. & Dasgupta, P. Efficacy of botulinum toxin-A for treating idiopathic detrusor overactivity: Results from a single center, randomized, double-blind, placebo controlled trial. J Urol 177, 2231–2236 (2007).
Brubaker, L. et al. Refractory idiopathic urge urinary incontinence and botulinum A injection. J Urol 180, 217–222 (2008).
Anger, J. T., Weinberg, A., Suttorp, M. J., Litwin, M. S. & Shekelle, P. G. Outcomes of intravesical botulinum toxin for idiopathic overactive bladder symptoms: a systematic review of the literature. J Urol 183, 2258–2264 (2010).
Jiang, Y. H., Ong, H. L. & Kuo, H. C. Predictive factors of adverse events after intravesical suburothelial onabotulinumtoxina injections for overactive bladder syndrome-A real-life practice of 290 cases in a single center. Neurourol Urodyn 36, 147–147 (2017).
Liao, C. H. & Kuo, H. C. Increased risk of large post-void residual urine and decreased long-term success rate after intravesical onabotulinumtoxinA injection for refractory idiopathic detrusor overactivity. J Urol 189, 1804–1810 (2013).
Wang, C. C., Liao, C. H. & Kuo, H. C. Diabetes mellitus does not affect the efficacy and safety of intravesical onabotulinumtoxinA injection in patients with refractory detrusor overactivity. Neurourol Urodyn 33, 1235–1239 (2014).
Kuo, H. C., Liao, C. H. & Chung, S. D. Adverse events of intravesical botulinum toxin a injections for idiopathic detrusor overactivity: risk factors and influence on treatment outcome. Eur Urol 58, 919–926 (2010).
Osborn, D. J. et al. Urinary retention rates after intravesical onabotulinumtoxinA injection for idiopathic overactive bladder in clinical practice and predictors of this outcome. Neurourol Urodyn 34, 675–678 (2015).
Hsiao, S. M., Lin, H. H. & Kuo, H. C. Factors associated with therapeutic efficacy of intravesical onabotulinumtoxinA injection for overactive bladder syndrome. PLoS One 11, e0147137 (2011).
Chancellor, M. B. The overactive bladder progression to underactive bladder hypothesis. Int Urol Nephrol 46 (Suppl 1), S23–27 (2014).
Kuo, H. C. Videourodynamic characteristics and lower urinary tract symptoms of female bladder outlet obstruction. Urology 66, 1005–1009 (2005).
Kuo, H. C. Clinical symptoms are not reliable in the diagnosis of lower urinary tract dysfunction in women. J Formos Med Assoc 111, 386–391 (2012).
Abrams, P. Bladder outlet obstruction index, bladder contractility index, and bladder voiding efficiency: three simple indices to define bladder voiding function. BJU Int 84, 14–15 (1999).
Hsiao, S. M. et al. Evaluation of bladder diary parameters based on correlation with the volume at strong desire to void in filling cystometry. PLoS One 8, e69946 (2013).
Nixon, A. et al. A validated patient reported measure of urinary urgency severity in overactive bladder for use in clinical trials. J Urol 174, 604–607 (2005).
Homma, Y. et al. Symptom assessment tool for overactive bladder syndrome–overactive bladder symptom score. Urology 68, 318–323 (2006).
Jiang, Y. H., Liu, H. T. & Kuo, H. C. Decrease of urinary nerve growth factor but not brain-derived neurotrophic factor in patients with interstitial cystitis/bladder pain syndrome treated with hyaluronic acid. PLoS One 9, e91609 (2014).
Altman, D. G. Practical statistics for medical research (ed. Altman, D. G. ) 325–364 (Chapman & Hall, 1991).
Rosner, B. Fundamentals of Biostatistics. (ed. Rosner, B. ) 577–676 (Duxbury, 2000).
Rosenbaum, P. R. & Rubin, D. B. The central role of the propensity score in observational studies for causal effects. Biometrika 70, 41–55 (1983).
Kaplan, E. L. & Myer, P. Nonparametric estimation from incomplete observations. J Am Stat Assoc 53, 457–481 (1958).
Author information
Authors and Affiliations
Contributions
H.-C.K designed the study. S.-M.H. analyzed the data. S.-M.H. and H.-H.L. wrote the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Hsiao, SM., Lin, HH. & Kuo, HC. Urodynamic prognostic factors for large post-void residual urine volume after intravesical injection of onabotulinumtoxinA for overactive bladder. Sci Rep 7, 43753 (2017). https://doi.org/10.1038/srep43753
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep43753
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.