Abstract
A meta-analysis was performed to evaluate the efficacy of local anesthesia in alleviating pain during prostate biopsy. We searched relevant articles in PubMed and Embase. The included studies should be randomized controlled trials (RCT) using local anesthesia to alleviate pain during biopsy, which was recorded by a pain scale. Analgesic efficacy of different local anesthesia techniques were analyzed, including intrarectal local anesthesia (IRLA), periprostatic nerve block (PNB), pelvic plexus block (PPB) and intraprostatic local anesthesia (IPLA). We included 46 RCTs. PNB significantly reduced pain score compared with placebo (−1.27 [95% confidence interval [95% CI] −1.72, −0.82]) or no injection (−1.01 [95% CI −1.2, −0.82]). IRLA with prilocaine-lidocaine cream could also reduced pain (−0.45 [95% CI −0.76, −0.15]), while the IRLA with lidocaine gel was not effective (−0.1 [95% CI −0.24, 0.04]). PNB lateral to the neurovascular bundle had better analgesic effect than at prostate apex (P = 0.02). Combination use of PPB and IRLA considerably alleviated pain of patients compared with the combination of PNB and IRLA (−1.32 [95% CI −1.59, −1.06]). In conclusion, local anesthesia could alleviate patients’ pain during the prostate biopsy. PNB was not so effective as PPB.
Similar content being viewed by others
Introduction
Most prostate cancers were diagnosed by transrectal ultrasound (TRUS)-guided prostate biopsy. Although it was an efficient diagnostic method, about 65% to 90% of men felt pain or discomfort during TRUS-guided prostate biopsy1. In this condition, some doctors proposed that anesthetic might be a good choice to reduce pains. However, there was a dispute about anesthetic use. Previous study demonstrated that few urologists use any form of local anesthesia for TRUS biopsy2. Though some trials showed that use of local anesthetics made no differences3,4, many clinical studies proved apparent analgesic effect of local anesthesia compared with controls5,6,7. However, there has not been an exact answer about whether to use anesthetic or not up to now.
On the other hand, there were four major kinds of local anesthesia: IRLA, PNB, PPB and IPLA for prostate biopsy at the moment. Various studies have been conducted to investigate and compare the efficacy of different anesthesia methods but did not get a conclusion.
We performed this meta-analysis of RCTs about the use of anesthetic during TRUS-guided prostate biopsy to explore the analgesic efficacy of local anesthetic compared with no anesthesia or placebo, and to figure out which kind of local anesthesia was optimal.
Results
Search results and characteristics of included studies
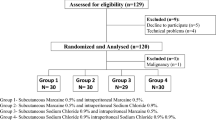
Our search strategy identified 347 studies in the initial database search (Fig. 1). After screening 46 RCTs1,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49 met our study criteria and were included in our meta-analysis.
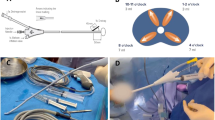
The characteristics of the included studies were listed in Table 1. In these studies, 42 used PNB, 19 used IRLA, 4 used IPLA, and 2 used PPB. In some studies, a local anesthesia method might be used alone or in combination with another one. PNB was used in most of the studies, but different studies chose different injection sites. We defined the different sites as base, apex and both of them. Base meant the area of neurovascular bundle at the base of the prostate, while apex was the area around the prostatic apex. Most studies used visual analogue scale (VAS) or numerical analogue scale (NAS) as the pain scale to evaluate the pain degree of patients.
Quality of the included studies
The risk of bias of included studies was presented with a risk of bias graph (Fig. 2), which showed that the quality of them was moderate. Quality of each study was shown in Supplementary Material (S1).
Meta-analyses
14 eligible studies showed that use of PNB significantly reduced pain compared with placebo injection (−1.27 [95% CI −1.72, −0.82], P < 0.00001; Fig. 3a), while 21 studies indicated that PNB could reduced pain compared with no injection (−1.01 [95% CI −1.2, −0.82], P < 0.00001; Fig. 3b). However, both comparisons had significant heterogeneity. We performed a sensitivity analysis by eliminating the included studies one by one. After deleting the study of Pareek et al.33 in the former comparison, I2 reduced from 92% to 59% and there were no apparent changes to the effect estimates. So this study might be the main source of heterogeneity and the reason might be that it used different pain scale. However, the sensitivity analysis could not find a study that was responsible for the heterogeneity in the later comparison. Thereby we performed a meta-regression analysis to investigate the effect of some variables (year of the study, mean age of patients, prostate biopsy numbers and dose of the anesthetics) on the heterogeneity. The result showed that the mean age of patients was apparently related to the outcomes (Table 2), so it might be a main source of heterogeneity.
10 studies showed that use of local anesthesia with lidocaine gel made no noteworthy differences in reducing pain compared with control (−0.1 [95% CI −0.24, 0.04], P = 0.15; Fig. 4a). But 3 eligible studies indicated that use of local prilocaine-lidocaine cream significantly reduced pain compared with control (−0.45 [95% CI −0.76, −0.15], P = 0.003; Fig. 4b).
The subgroup analysis of three different types of PNB showed that there were some differences between different injection sites. Compared with the PNB at prostatic apex, the PNB using the neurovascular bundles at the base of the prostate showed more effective anesthesia results (P = 0.02; Fig. 5a). However, no apparent difference was found between PNB with both sites and PNB at the neurovascular bundles of prostatic base (P = 0.58; Fig. 5b).
There were also some differences among different anesthetic techniques. The use of PNB was more efficient in reducing pain score than intrarectal anesthetic gel (−0.9 [95% CI −1.42, −0.38], P = 0.0007; Fig. 6).The I2 was 93% in this analysis. However, after the sensitivity analysis and meta-regression analysis we did not find any study or any parameter that might be the main source of heterogeneity.
In addition, combined use of PNB and IPLA had better analgesia effect than PNB alone (−0.84 [95% CI −1.11, −0.57], P < 0.00001; Fig.7a). Compared with combination use of PNB and IRLA, combination use of PNB and IRLA could significantly reduce pain score (−1.32 [95% CI −1.59, −1.06], P < 0.00001; Fig. 7b).
Discussion
In this meta-analysis, local anesthesia significantly alleviated pain during (TRUS)-guided prostate biopsy, except IRLA with lidocaine gel.
Although a similar meta-analysis containing 25 studies had been performed before by Tiong HY et al.50, some new studies were conducted after that and it was necessary to update it. Moreover, this meta-analysis only compared PNB with control or IRLA, while we performed more comparisons with more local anesthesia techniques and added a subgroup analysis.
PNB was the most used local anesthesia method. The first randomized, prospective study was published by Nash et al.31, showing the benefit of periprostatic local anesthesia. Our meta-analysis results suggested that PNB significantly reduced pain compared with placebo and no anesthesia, which was consistent with results from previous meta-analysis50.
Generally speaking, there were three different techniques of PNB: PNB lateral to the neurovascular bundle at the base of the prostate, PNB at the apex of the prostate and PNB with both regions. Our meta-analysis showed that all of the three different techniques significantly reduced pain during TRUS-guided prostate biopsy. We then performed a subgroup analysis to compare the effect of these three techniques. The results showed that anesthetic injection lateral to the neurovascular bundle was more effective than the injection at prostatic apex. But the combined injection in two sites was not superior to the single use of injection lateral to the neurovascular bundle.
The pain caused by prostate biopsy came mainly from the prostate capsule or stroma, because these areas had a rich innervation1. During the PNB, anesthetic infiltrated into the nerves around the prostate and blocked the nerve conduction. Hence it could decrease pain of patients. Fibers derived from the pelvic plexus traveled with vessels, forming the neurovascular bundle, and entered into the prostate at the base of the prostate just lateral to the junction between the prostate and seminal vesicle. Thereby the infiltration of local anesthesia in this region had better analgesic effect.
IRLA was a convenient local anesthesia technique and brought only a little discomfort to patients. But our results showed that IRLA with lidocaine gel could not reduce the pain during the prostate biopsy significantly. Even so, we could not deny the efficacy of IRLA. Our analysis indicated that IRLA with prilocaine-lidocaine cream could alleviate patients’ discomfort during the biopsy. This suggested that combined local anesthesia cream might have better analgesic effect than a single one. We compared the efficacy between PNB and IRLA with lidocaine gel and found that the former was more efficient in decreasing pain. It was a pity that there was not enough studies to compare PNB and IRLA with prilocaine-lidocaine cream.
Our meta-analysis also assessed two other block ways: IPLA and PPB. Mutaguchi et al. showed intraprostatic anesthesia was a new local anesthesia technique to anesthetize the prostate which blocked all sensory nerves from the posterior and anterior sides51. Due to the limited number of relevant studies, we were not able to compare the effect of PNB and IPLA alone. However, our meta-analysis suggested that the combination of IPLA and PNB had better analgesic effect than PNB alone. However, a drawback of the IPLA was that it could cause pain when penetrating the prostate capsule.
The pelvic plexus was an autonomic plexus including sympathetic and parasympathetic nerves. The midpoint of pelvic plexus located just lateral to the tip of the seminal vesicle and it was punched through by abundant branches of inferior vesicle vessels. Because the fibers innervating the prostate were derived mainly from pelvic plexus, local anesthesia in this location might be useful. In PPB, anesthesia was injected bilaterally into the pelvic plexus, therefore blocking all the nerve fibers and thus having a theoretical advantage over PNB21. Our meta-analysis showed that combination use of PPB and IRLA significantly reduced pain when compared with combination use of PNB and IRLA. Restricted by the number of studies, we were not able to compare the effect of PNB and PPB directly.
There were some limitations in our meta-analysis. First of all, significant heterogeneity among studies existed in some comparisons, which might reduce the reliability of our results. Even though we performed both sensitivity analysis and meta-regression analysis to investigate the source of heterogeneity, not all the heterogeneity source could be found. Hence we used the random effect model in our analysis. In addition, there was not enough number of studies in some comparisons. More studies were expected to reinforce our results.
In summary, it was the first meta-analysis about the role of PPB and intraprostatic anesthesia in reducing pain during TRUS-guided prostate biopsy to our knowledge. Our meta-analysis suggested that local anesthesia such as PNB, PPB, IPLA and local prilocaine-lidocaine cream was effective in alleviating pain for TRUS-guided prostate biopsy. Besides, PNB lateral to the neurovascular bundle at the base of prostate had better analgesic efficacy than PNB at the prostatic apex. It was also revealed that PPB might be more effective than PNB. Hence, PPB was potential to be a standard of care for patients undergoing TRUS-guided prostate biopsy.
Methods
Study search
We searched Pubmed and Embase for all papers, including conference abstracts, in any language published before May 1, 2016. Our search strategy was: (prostate biopsy) and ((local anesthesia) or analgesic) and (pain or discomfort) and (randomized or randomization). Reviews and nonhuman studies were not included. In addition, if two studies were conducted by the same authors and parts of their patients were also the same, only the latest one with more patients was included. The search was conducted by two authors separately.
Inclusion criterion
The studies that met the following criteria were included: (1) RCTs; (2) patients underwent TRUS-guided prostate biopsy with local anesthetic; (3) local anesthetic was compared with placebo or no anesthetic group, or different kinds of local anesthesia methods were compared; (4) pain during the biopsy should be recorded by a pain scale.
Data Extraction
All available RCTs that had data about pain during TRUS-guided prostate biopsy were selected for analysis. The major characteristics of included articles were extracted: the first author, the year of publication, study design, the number of patients and groups, the utilized local anesthesia methods and their location and the pain scale.
The mean and standard deviations of pain scores were extracted to perform the analysis. These data were recorded by different pain scales, such as VAS, NAS and others. We extracted the pain scores which were taken immediately at the end of the biopsy for evaluation. If a research used both placebo injection and no analgesic, both groups were used as controls and the patients’ number in the anesthesia group was divided equally into two parts. Similarly, if more than one local anesthesia groups was used in one study, the number of patients of the control group was divided equally by the number of anesthesia groups. All the data were extracted independently by different study authors and any discrepancy was resolved by consensus.
Quality assessment
Quality assessment of the included studies was performed by The Cochrane Collaboration’s tool for assessing risk of bias, including assessments of random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting and other bias.
Statistical analysis
All meta-analyses were performed using RevMan 5.2 (The Nordic Cochrane Centre, the Cochrane Collaboration, 2012, Copenhagen, Denmark). Continuous outcomes were presented as standardized mean difference (SMD) with 95% confidence interval (CI). Statistical heterogeneity was assessed with the I2 statistic, in whichI2 > 50% was considered to be of high heterogeneity. When significant heterogeneity was present, data were analyzed using the random effect model and a sensitivity analysis or meta-regression analysis was performed to find the source of heterogeneity. The meta-regression analysis was performed by using Stata 12.0. Differences were considered statistically significant when P < 0.05.
Firstly, we compared the outcomes of PNB groups with placebo groups and no anesthesia groups separately. Secondly, we analyzed the anesthesia efficacy of different IRLA methods, including the simple IRLA with lidocaine gel and IRLA with lidocaine-prilocaine cream. And then, we performed subgroup analysis to compare the efficacy of PNB methods with different injection positions. At last we compared the outcomes of different kinds of local anesthesia methods.
Additional Information
How to cite this article: Li, M. et al. Local anesthesia for transrectal ultrasound-guided biopsy of the prostate: A meta-analysis. Sci. Rep. 7, 40421; doi: 10.1038/srep40421 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Alavi, A. S., Soloway, M. S., Vaidya, A., Lynne, C. M. & Gheiler, E. L. Local anesthesia for ultrasound guided prostate biopsy: a prospective randomized trial comparing 2 methods. J Urol. 166, 1343–1345 (2001).
Amling, C. L., Spencer, C. R. & Roberts, J. L. Practice patterns in transrectal ultrasound guided prostate biopsy: results of a questionnaire survey of practicing urologists. J Urol. 171 (suppl), 1809 (2004).
Bozlu, M. et al. Periprostatic lidocaine infiltration and/or synthetic opioid (meperidine or tramadol) administration have no analgesic benefit during prostate biopsy: a prospective randomized double-blind placebo-controlled study comparing different methods. Urol Int. 72, 308–311 (2004).
Walsh, K., O’Brien, T., Salemmi, A. & Popert, R. A randomised trial of periprostatic local anaesthetic for transrectal biopsy. Prostate Cancer Prostatic Dis. 6, 242–244 (2003).
Akdere, H., Burgazli, K. M., Aktoz, T., Acikgoz, A. & Gozen, A. S. The importance of anatomical region of local anesthesia for prostate biopsy; a randomized clinical trial. Eur Rev Med Pharmacol Sci. 17, 2890–2895 (2013).
Obek, C. et al. Comparison of 3 different methods of anesthesia before transrectal prostate biopsy: a prospective randomized trial. J Urol. 172, 502–505 (2004).
Ozden, E., Yaman, O., Göğüs, C., Ozgencil, E. & Soygür, T. The optimum doses of and injection locations for periprostatic nerve blockade for transrectal ultrasound guided biopsy of the prostate: a prospective, randomized, placebo controlled study. J Urol. 70, 2319–2322 (2003).
Adamakis, I. et al. & Giannopoulos, A. Pain during transrectal ultrasonography guided prostate biopsy: a randomized prospective trial comparing periprostatic infiltration with lidocaine with the intrarectal instillation of lidocaine-prilocain cream. World J Urol. 22, 281–284 (2004).
Addla, S. K., Adeyoju, A. A., Wemyss-Holden, G. D. & Neilson, D. Local anaesthetic for transrectal ultrasound-guided prostate biopsy: a prospective, randomized, double blind, placebo-controlled study. Eur Urol. 43, 441–443 (2003).
Bingqian, L., Peihuan, L., Yudong, W., Jinxing, W. & Zhiyong, W. Intraprostatic local anesthesia with periprostatic nerve block for transrectal ultrasound guided prostate biopsy. J Urol. 182, 479–483 (2009).
Buckley, M. R. et al. Tolerance of local anesthetic for transrectal ultrasound-guided prostate biopsy: our experience and a literature review. Can Assoc Radiol J. 57, 169–174 (2006).
Cam, K., Sener, M., Kayikci, A., Akman, Y. & Erol, A. Combined periprostatic and intraprostatic local anesthesia for prostate biopsy: a double-blind, placebo controlled, randomized trial. J Urol. 180, 141–144 discussion 144-145 (2008).
Cantiello, F. et al. Pelvic plexus block is more effective than periprostatic nerve block for pain control during office transrectal ultrasound guided prostate biopsy: a single center, prospective, randomized, double arm study. J Urol. 188, 417–421 (2012).
Cevik, I., Ozveri, H., Dillioglugil, O. & Akdaş, A. Lack of effect of intrarectal lidocaine for pain control during transrectal prostate biopsy: a randomized prospective study. Eur Urol. 42, 217–220 (2002).
Chang, S. S., Alberts, G., Wells, N., Smith, J. A. Jr. & Cookson, M. S. Intrarectal lidocaine during transrectal prostate biopsy: results of a prospective double-blind randomized trial. J Urol. 166, 2178–2180 (2001).
Galosi, A. B., Minardi, D., Dell’atti, L., Yehia, M. & Muzzonigro, G. Tolerability of prostate transrectal biopsies using gel and local anesthetics: results of a randomized clinical trial. J Endourol. 19, 738–743 (2005).
Hiros, M., Selimovic, M., Spahovic, H., Sadovic, S. & Spuzic-Celic, E. Transrectal ultrasound-guided prostate biopsy, periprostatic local anesthesia and pain tolerance. Bosn J Basic Med Sci. 10, 68–72 (2010).
Inal, G. et al. Effect of periprostatic nerve blockade before transrectal ultrasound-guided prostate biopsy on patient comfort: a randomized placebo controlled study. Int J Urol. 11, 148–151 (2004).
Ingber, M. S., Ibrahim, I., Turzewski, C., Hollander, J. B. & Diokno, A. C. Does periprostatic block reduce pain during transrectal prostate biopsy? A randomized, placebo-controlled, double-blinded study. Int Urol Nephrol. 42, 23–27 (2010).
Izol, V., Soyupak, B., Seydaoglu, G., Aridogan, I. A. & Tansug, Z. Three different techniques for administering analgesia during transrectal ultrasound-guided prostate biopsy: a comparative study. Int Braz J Urol. 38, 122–128 (2012).
Jindal, T. et al. Transrectal Ultrasound Guided Pelvic Plexus Block to reduce pain during prostate biopsy: a randomized controlled trial. BJU Int. Jul. 21 (2014).
Kandirali, E. et al. Is only perianal anesthesia with lidocaine-prilocaine cream sufficient to decrease the pain during transrectal ultrasound-guided prostate biopsy? A prospective randomized study. Urol Int. 82, 262–265 (2009).
Kaver, I., Mabjeesh, N. J. & Matzkin, H. Randomized prospective study of periprostatic local anesthesia during transrectal ultrasound-guided prostate biopsy. Urology. 59, 405–8 (2002).
von Knobloch, R. et al. Bilateral fine-needle administered local anaesthetic nerve block for pain control during TRUS-guided multi-core prostate biopsy: a prospective randomised trial. Eur Urol. 41, 508–514, discussion 514 (2002).
Kravchick, S. et al. Comparison of different local anesthesia techniques during TRUS-guided biopsies: a prospective pilot study. Urology. 65, 109–113 (2005).
Lee, H. Y. et al. Effect of intraprostatic local anesthesia during transrectal ultrasound guided prostate biopsy: comparison of 3 methods in a randomized, double-blind, placebo controlled trial. J Urol. 178(2), 469–472, discussion 472 (2007).
Leibovici, D. et al. Local anesthesia for prostate biopsy by periprostatic lidocaine injection: a double-blind placebo controlled study. J Urol. 167, 563–565 (2002).
Mallick, S. et al. Which anaesthesia should be recommended for prostate biopsy? West Indian Med J. 54, 135–138 (2005).
Manikandan, R., Srirangam, S. J., Brown, S. C., O’Reilly, P. H. & Collins, G. N. Nitrous oxide vs periprostatic nerve block with 1% lidocaine during transrectal ultrasound guided biopsy of the prostate: a prospective, randomized, controlled trial. J Urol. 170, 1881–1883, discussion 1883 (2003).
Nambirajan, T. et al. Efficacy and safety periprostatic local anaesthetic injection in transrectal biopsy of the prostrate: a prospective randomised study. Surgeon. 2, 221–224 (2004).
Nash, P. A., Bruce, J. E., Indudhara, R. & Shinohara, K. Transrectal ultrasound guided prostatic nerve blockade eases systematic needle biopsy of the prostate. J Urol. 155, 607–609 (1996).
Obi, A. O., Okafor, V. U. & Nnodi, P. I. Prospective randomized trial of spinal saddle block versus periprostatic lignocaine for anesthesia during transrectal prostate biopsy. Urology. 77, 280–285 (2011).
Pareek, G., Armenakas, N. A. & Fracchia, J. A. Periprostatic nerve blockade for transrectal ultrasound guided biopsy of the prostate: a randomized, double-blind, placebo controlled study. J Urol. 166, 894–897 (2001).
Raber, M. et al. Topical prilocaine-lidocaine cream combined with peripheral nerve block improves pain control in prostatic biopsy: results from a prospective randomized trial. Eur Urol. 53(5), 967–973 (2008).
Rabets, J. C., Jones, J. S., Patel, A. R. & Zippe, C. D. Bupivacaine provides rapid, effective periprostatic anaesthesia for transrectal prostate biopsy. BJU Int. 93, 1216–1217 (2004).
Rodriguez, A., Kyriakou, G., Leray, E., Lobel, B. & Guillé, F. Prospective study comparing two methods of anaesthesia for prostate biopsies: apex periprostatic nerve block versus intrarectal lidocaine gel: review of the literature. Eur Urol. 44, 195–200 (2003).
Schostak, M. et al. Optimizing local anesthesia during 10-core biopsy of the prostate. Urology. 60, 253–257 (2002).
Seçkiner, I., Sen, H., Erturhan, S. & Yağcı, F. A prospective, randomized controlled study comparing lidocaine and tramadol in periprostatic nerve blockage for transrectal ultrasound-guided prostate biopsy. Urology. 78, 257–260 (2011).
Seymour, H., Perry, M. J., Lee-Elliot, C., Dundas, D. & Patel, U. Pain after transrectal ultrasonography-guided prostate biopsy: the advantages of periprostatic local anaesthesia. BJU Int. 88, 540–544 (2001).
Singh, S. K., Kumar, A., Griwan, M. S. & Sen, J. Comparative Evaluation of Periprostatic Nerve Block with and without Intraprostatic Nerve Block in Transrectal Ultrasound-Guided Prostatic Needle Biopsy. Korean J Urol. 53, 547–551 (2012).
Song, S. H., Kim, J. K., Song, K., Ahn, H. & Kim, C. S. Effectiveness of local anaesthesia techniques in patients undergoing transrectal ultrasound-guided prostate biopsy: a prospective randomized study. Int J Urol. 13, 707–710 (2006).
Stirling, B. N., Shockley, K. F., Carothers, G. G. & Maatman, T. J. Comparison of local anesthesia techniques during transrectal ultrasound-guided biopsies. Urology. 60, 89–92 (2002).
Trucchi, A. et al. Local anesthesia reduces pain associated with transrectal prostatic biopsy. A prospective randomized study. Urol Int. 74, 209–213 (2005).
Turgut, A. T., Ergun, E., Koşar, U., Koşar, P. & Ozcan, A. Sedation as an alternative method to lessen patient discomfort due to transrectal ultrasonography-guided prostate biopsy. Eur J Radiol. 57, 148–153 (2006).
Vanni, A. P., Schaal, C. H., Costa, R. P. & Sala, F. C. Is the periprostatic anesthetic blockade advantageous in ultrasound-guided prostate biopsy? Int Braz J Urol. 30, 114–118 (2004).
Walker, A. E., Schelvan, C., Rockall, A. G., Rickards, D. & Kellett, M. J. Does pericapsular lignocaine reduce pain during transrectal ultrasonography-guided biopsy of the prostate? BJU Int. 90, 883–886 (2002).
Wu, C. L., Carter, H. B., Naqibuddin, M. & Fleisher, L. A. Effect of local anesthetics on patient recovery after transrectal biopsy. Urology. 57, 925–929 (2001).
Yurdakul, T., Taspinar, B., Kilic, O., Kilinc, M. & Serarslan, A. Topical and long-acting local anesthetic for prostate biopsy: a prospective randomized placebo-controlled study. Urol Int. 83, 151–154 (2009).
Kuppusamy, S., Faizal, N., Quek, K. F., Razack, A. H. & Dublin, N. The efficacy of periprostatic local anaesthetic infiltration in transrectal ultrasound biopsy of prostate: a prospective randomised control study. World journal of urology. Dec. 28(6), 673–6 (2010).
Tiong, H. Y., Liew, L. C., Samuel, M., Consigliere, D. & Esuvaranathan, K. A meta-analysis of local anesthesia for transrectal ultrasound-guided biopsy of the prostate. Prostate Cancer Prostatic Dis. 10, 127–136 (2007).
Mutaguchi, K. et al. Local anesthesia during 10 core biopsy of the prostate: comparison of 2 methods. J Urol. 173, 742–745 (2005).
Author information
Authors and Affiliations
Contributions
H.L. and J.Y. extracted and analyzed the data. T.W. and J.H.L. conceived and designed the study. S.G.W., H.L., and K.R. participated in the critical revision of the manuscript. M.C.L. and Z.Y.W. drafted the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Li, M., Wang, Z., Li, H. et al. Local anesthesia for transrectal ultrasound-guided biopsy of the prostate: A meta-analysis. Sci Rep 7, 40421 (2017). https://doi.org/10.1038/srep40421
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep40421
This article is cited by
-
Efficacy of additional periprostatic apex nerve block on pain in each of 12 transrectal prostate core biopsies: a retrospective study
BMC Urology (2021)
-
The effect of heated lidocaine gel on pain reduction during transrectal ultrasound-guided prostate biopsy: a randomized-controlled study
International Urology and Nephrology (2021)
-
What is the most effective local anesthesia for transrectal ultrasonography-guided biopsy of the prostate? A systematic review and network meta-analysis of 47 randomized clinical trials
Scientific Reports (2019)
-
A randomized controlled comparison between periprostatic nerve block and pelvic plexus block at the base and apex of 14-core prostate biopsies
World Journal of Urology (2019)
-
Prospective comparison among three intrarectal anesthetic treatments combined with periprostatic nerve block during transrectal ultrasonography-guided prostate biopsy
World Journal of Urology (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.