Abstract
This study aimed to explore pre-hospital delay and its associated factors in first-ever stroke registered in communities from three cities in China. The rates of delay greater than or equal to 2 hours were calculated and factors associated with delays were determined by non-conditional binary logistic regression, after adjusting for different explanatory factors. Among the 403 cases of stroke with an accurate documented time of prehospital delay, the median time (interquartile range) was 4.00 (1.50–14.00) hours. Among the 544 cases of stroke with an estimated time range of prehospital delay, 24.8% of patients were transferred to the emergency department or hospital within 2 hours, only 16.9% of patients with stroke were aware that the initial symptom represented a stroke, only 18.8% used the emergency medical service and one-third of the stroke cases were not identified by ambulance doctors. In the multivariate analyses, 8 variables or sub-variables were identified. In conclusion, prehospital delay of stroke was common in communities. Thus, intervention measures in communities should focus on education about the early identification of stroke and appropriate emergency medical service (EMS) use, as well as the development of organized stroke care.
Similar content being viewed by others
Introduction
The incidence of stroke in China is higher than in other parts of the world and there is an increasing trend for ischemic stroke1,2. In a WHO’s Monitoring of Trends and Determinants of Cardiovascular Disease (WHO MONICA) project, the age-standardised stroke-attack rate (for first and recurrent events) in Beijing from 1985 to 1990 was 247 per 100 000 per year for men and 175 per 100 000 per year for women, sixth and second highest among the 17 MONICA populations in 10 countries, respectively2. The incidence of overall stroke and ICH among individuals ≥55 years of age from 1991 to 2000 was substantially higher in Beijing and Changsha than in Western populations from published literature1. The estimated rates of thrombolytic use for ischemic stroke are very low, ranging from only 1% to 3% in previous hospital-based studies2,3. Implementation of effective interventions to treat acute strokes within the time window, including the use of thrombolytics in acute ischemic stroke and the management of blood pressure and blood glucose during the acute period of cerebral apoplexy, has a significant impact on stroke recovery. With regard to prehospital delay in stroke, most studies are hospital-based and focus on ischemic stroke4. However, almost all hospital-based studies suggest that the “FAST” criteria (which include three assessment items of facial droop, arm weakness or paralysis and speech difficulty, as well as an attached message of time to promote urgency) should be implemented in communities; however, the factors identified as influencing prehospital delay of stroke were different, even contrary, across different studies. Thus, it might be inappropriate to use the evidence from hospital-based studies to conduct a “FAST” campaign on stroke in all communities.
To better direct the “FAST” compaign in communities, we aimed to explore pre-hospital delay and its associated factors in patients experiencing a first-ever stroke by examining the results from a stroke surveillance registry in communities from three cities in China.
Methods
Subjects
In this study, we used surveillance data of first-ever stroke in 2008 from a Chinese population of approximately 300000 residing in surburban Shanghai (SH), Changsha (CS) and Chengdu (CD). Shanghai, Changsha and Chengdu are three cities located in the eastern, central southern and western southern regions of China, respectively.
As the study initiator, the Beijing Neurosugical Institute presided over the project. The three centers that served as executors, the Shanghai Institute of Cerebral Vascular Disease Prevention and Cure, the Xiangya Hospital of Central South University in Changsha and the West China Hospital of Sichuan University in Chengdu, were responsible for field work and data collection. Personnel from the three collabrating centers were trained by the Beijing Neurosurgical Institute before the beginning of the project.
First, three communities, each with approximately 100 000 residents, were defined in 2008 by the three aforementioned cooperation centers. Demographic information on the age and gender distributions of each community was obtained from local police stations and/or local neighborhood committees (NCs). Temporary residents and individuals who registered in the local police stations but did not actually reside in the communities were excluded.
Stroke surveillance
The stroke report network, case ascertainment and quality control were described in detail in a previous study1. Briefly, at the beginning of the stroke registry in these communities, community-based stroke surveillance networks were established in all research communities to identify incident stroke cases. Doctors in local centers of community health services (CHS) or hospitals that provide basic and comprehensive medical and public health services to local residents in China were recruited as our grassroots network and trained annually by the 3 collaborating centers in this project. These doctors established close ties with the directors of local NCs and building gate volunteers who were trained to identify and report stroke cases. During the study period, the qualified doctors or general practioners (GPs) in local CHS centers or hospitals collected all the possible stroke cases during their daily health services through directors of NCs or building gate volunteers. Personnel from the 3 collaborating centers would then assess the diagnoses for all of the reported cases of stroke and death and they were responsible for the quality of the stroke surveillance.
Detailed clinical information on each case, including age and sex, clinical signs and symptoms, past medical history, medications, computerized tomography (CT) or magnetic resonance imaging (MRI) results and prehospital clinical status, was obtained through interviews with the patients, families, relatives or witnesses and/or retrieval from medical records in hospitals using a structured questionnaire (Supplementary Appendix 1 online). The prehospital clinical status information included date (year: month: day) and 24-hour time (hour: minute) of stroke onset and hospital arrival, stroke identification, seeking medical service behavior after symptom onset, transport means, first-visit arrival hospital and hospital grade, the first witness who noticed the symptoms or signs, other symptom onset details including nighttime or daytime onset, changes in symptoms from onset to hospital arrival and whether the symptoms occurred on a workday or weekend (including national legal holiday). If the date and 24-hour time of stroke onset or hospital arrival could not be obtained in some cases, the estimated time range from onset to the hospital was approximated to one of 7 time bands (including <2 hours, 2 to 6 hours, 6 to12 hours, 12 to 24 hours, 1 to 3 days, 3–7 days and >7 days) to the greatest extent possible.
Patients who did not go to the hospital or died at home were also identified as parts of the medical workers’ routines, supplemented by our annual door-to-door inquiries of the NCs directors and building gate volunteers for each building. Stroke patients who died at home were identified by eyewitnesses (patients’ relatives) and the monthly review of death certificates. In China, all deaths are legally required to be reported by patients’ relatives to the local medical workers for a death certificate used in cremation and household registration cancellation.
Stroke Diagnosis and Classification
The diagnosis and classification of stroke were performed according to a slightly revised version of that used in the Atherosclerosis Risk in Communities (ARIC) Study1. Briefly, the minimum criteria for a definite or probable stroke diagnosis included evidence of sudden or rapid onset of neurological symptoms lasting for >24 hours or leading to death in the absence of evidence for a nonstroke cause. Stroke subtypes were defined according to published criteria and then grouped into 3 major types: ischemic stroke (IS, including thrombotic brain infarction, cardioembolic stroke and symptomatic lacunar infarcts), intracerebral hemorrhage (ICH), or subarachnoid hemorrhage (SAH). Patients who fit 2 different diagnostic categories, did not go to the hospital or died at home were assigned as undetermined stroke (US).
Definitions of studied factors
The medical histories were defined as follows: hypertension (reported systolic blood pressure ≥140 mm Hg, reported diastolic blood pressure ≥90 mm Hg, patient’s self-report of hypertension or use of antihypertensive drugs), transient ischemic attack (TIA, a temporary disturbance in brain function resulting from a temporary blockage of the brain’s blood supply that resolves within 24 hours), cardiac diseases (history of myocardial infarction, coronary artery disease, congestive heart failure, arrhythmia, or valvular heart disease), diabetes mellitus (fasting blood glucose level ≥7.8 mmol/L, patient’s self-report of diabetes, or use of antidiabetic drugs) and hyperlipidemia (reported fasting total cholesterol ≥5.72 mmol/L, reported low-density lipoprotein (LDL) ≥3.64 mmol/L, reported high-density lipoprotein (HDL) ≤0.91 mmol/L, reported triglyceride ≥1.70 mmol/L, patient’s self-report of hyperlipidemia, or use of antihyperlipidemic drugs).
The onset time was defined as the moment that a patient or witness initially noticed symptoms. When indeterminate, we defined onset time as the last time that the patient was observed without symptoms. The time of admission was defined as the time when the patients presented to the first-visit ED or hospital including primary, secondary or tertiary hospitals. Prehospital delay or time to presentation was defined as the time from symptom onset to the earliest documented time in the first visit to the emergency department or hospital.
Emergency medical services (EMS) and organized stroke care in three cities
In China, larger cities generally use the 120 and/or 999 EMS scheduling systems. Ambulances are based at hospitals in Changsha and Chengdu or at independent facilities in Shanghai. Physicians accompany ambulances in many of the larger services on runs to severely ill patients, whereas ambulance drivers receive little or no formal training. Although there is communication between the EMS systems and hospitals in these larger cities, there is also some competition and conflict over “turf” in providing services5. Although the development of EMS in China has made great progress, the development of the “life green channel” for stroke is just beginning and requires further development.
Although delivering organized stroke services plays key role in the provision of effective therapies and in improving the overall outcome of stroke, organized stroke care is still far from implemented in large parts of China and organization of prehospital care has received less attention than organized inpatient (stroke unit) care. In 2001, the first comprehensive stroke unit in China was established in Beijing. Until 2015, guidelines for the construction of a stroke center in China were first issued and the 455 hospitals’ list of the Chinese Stroke Center Alliance (CSCA) members was announced by the Chinese Stroke Association, the Center of Medical Quality Control of the National Health and Family Planning Commission and the CSCA. However, most hospitals in this stroke registry were not listed among the CSCA members.
Ethics statement
This study was approved by the Ethics Committee of the Beijing Tiantan Hospital affiliated with the Capital Medical University, shared by the Beijing Neurosurgical Institute and oral informed consent was obtained from all participants through patients’ self or caregivers. The study was performed in accordance with the Declaration of Helsinki.
Statistical analysis
Percents were given for categorical variables and means (±SD, median) were given for continuous variables. The prehospital delay time was presented as both a mean and a median according to a previous study’s suggestion4. Significant differences among groups were determined using the χ2 test, Fisher’s exact test, Mann-Whitney’s U-test and analysis of variance (ANOVA).
The prehospital delay rates of greater than or equal to 2 hours were analyzed in the different subgroups and factors associated with delays were determined using non-conditional binary logistic regression after adjusting for different explanatory factors. The explanatory risk factors included age group (<55/≥55/≥65/≥75); sex (men/women); city (Shanghai/Changsha/Chengdu); subtype of stroke (SAH/ICH/IS/US); history (yes/no/unknown) of hypertension, TIA, cardiac disease, diabetes mellitus and hyperlipidemia; symptoms/signs (yes/no/unknown) of vomiting, headache, coma, hemiplegia, diplopia, aphasia, hemianopsia, dysesthesia, vertigo (disorders of gaits) and dysarthria (difficulty in swallowing, enunciation); the prehospital clinical status of stroke identification (yes/no/unknown); seeking medical service behavior after symptom onset (directly go to hospital by self/call 120 or 999/call for GP’s help/unknown); transport means (ambulance/private car or taxi/bicycle or tricycle or other vehicle); arrival hospital and hospital grade (tertiary hospital/secondary hospital/primary hospital or CHS center); first witness who noticed symptoms or signs (patients’ self/family/field witness/GPs or unknown); onset details including nighttime or daytime onset (nighttime/daytime/unknown); changes in symptoms from onset to hospital presentation (worsened/completely improved/partially improved/unchanged/unknown); and workday or weekend (workdays/holidays). In the multivariate analysis, the estimated time range of prehospital delay was used. Given collinearity and problems with multivariable results from small numbers in some categories in the multivariate analysis, the multivariable analysis was done using forward stepwise regression with likelihood ratio to obtain a more parsimonious and reliable model. A sensitivity analysis for the multivariable analysis was also done to validate the results using patients with an accurate time of prehospital delay. All statistical calculations were performed using SPSS 13.0 software (SPSS Inc. Chicago, IL, USA). P < 0.05 was considered statistically significant.
Role of the funding source
The funder had no role in the study design, data collection, analysis, interpretation, or the writing of the report. The project investigators were responsible for the decision to submit the report for publication.
Results
Stroke registration
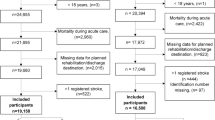
Altogether, 666 cases of first-ever stroke (3 SAH; 47 ICH; 175 IS; 2 US in SH, 4 SAH; 98 ICH; 109 IS; 7 US in CS and 8 SAH; 43 ICH; 160 IS; 10 US in CD) were registered from a population of 341,207 individuals (100,622 people in SH, 110,411 people in CS and 130,174 people in CD). Among the 666 cases, 122 cases were excluded because of missing information on prehospital clinical status including prehospital delay. Therefore, 544 cases of the 666 cases had an estimated time range of prehospital delay and 403 cases (218 cases in SH, 93 cases in CS and 92 cases in CD) of the 544 cases also had an accurate time of prehospital delay. Among the 544 cases, 220 cases (3 SAH; 46 ICH; 170 IS; 1 US) were registered from 12 hospitals (5 tertiary hospitals, 3 secondary hospitals and 4 primary hospitals) in SH, 178 cases (3 SAH; 81 ICH; 87 IS; 7 US) from 9 hospitals (5 tertiary hospitals, 2 secondary hospitals and 2 primary hospitals) in CS and 146 cases (6 SAH; 28 ICH; 109 IS; 3 US) from 9 hospitals (2 tertiary hospitals, 5 secondary hospitals and 2 primary hospitals) in CD. No significant differences were noted between all of the stroke cases and cases with an accurate time or estimated time range of prehospital delay regarding the variables of age, sex and stroke subtype (Table 1). In other words, the cases with an accurate time or estimated time range of prehospital delay represented all stroke cases.
Characteristics and clinical status of pre-hospital transfers among patients with stroke registered in the three cities
Table 2 shows that characteristics and clinical status of pre-hospital transfers among patients with stroke registered in the 3 Chinese communities. Among the 544 cases of stroke, only 16.9% of patients with stroke were aware that the initial symptom was a stroke (by the patient/bystander) and 18.8% used the EMS (one third of the strokes were not identified by the ambulance doctors). In the first-visit to the emergency department or hospital, 4.2% of patients arrived at CHS centers or local hospitals, 71.5% of patients were transferred to a secondary hospital and 24.3% of patients were transferred to a tertiary hospital. Among the 403 cases of stroke, the median (interquartile range) value was 4.00 (1.50–14.00) hours. In the communities studied, 24.8% of patients from the 544 cases were transferred to the emergency department or hospital within 2 hours, while 49.1% of the patients from the 399 cases were transferred within 3 hours.
Associated factors for prehospital delay
In univariate analyses, 17 variables or sub-variables were associated with prehospital delay ≥2 hours, whereas 8 variables or sub-variables were identified in the multivariate analyses. The proportions of prehospital delay ≥2 hours in patients with stroke in CS and CD were higher, respectively 3.6 times and 2.2 times, than in SH, after adjusting for other variables in the multivariate analyses. The proportion of prehospital delay ≥2 hours in patients with stroke whose symptoms/signs were discovered by a cohabitant or non-cohabitant witness was lower, respectively 1/2 and 1/4, compared to the cases identified by the patient. The proportion of prehospital delay ≥2 hours in patients who had symptoms of coma was lower than that in those who did not. The proportion of prehospital delay ≥2 hours in patients with a stroke that occurred at nighttime was higher in comparison to those with daytime stroke; the proportion of prehospital delay ≥2 hours in patients who were unaware of their stroke symptoms was higher than that in patients who were aware; and the proportion of prehospital delay ≥2 hours in those whose symptoms were partially improved was higher than that in patients whose symptoms were unchanged (Table 3). In the sensitivity analysis, more consistent results from patients with an accurate time of prehospital delay and with an estimated time range of prehospital delay were found except “coma” variable (data not shown).
Discussion
In this investigation, half of the patients with a stroke were transferred to an emergency department or hospital within 3 hours; the median (interquartile range) delay was 4.00 (1.50–14.00) hours. Both the proportion and the median delay were better than 25% and 15.0 (2.8–51.0) hours in a previous report3. The present study was distinctly different from this previous hospital-based study, which involved 62 hospitals across a variety of economic and geographic regions in China during 2006; it mainly focused on prehospital delay in first visits to the emergency department or hospital in a community-based surveillance registry of patients experiencing a first-ever stroke in 3 large cities. The median prehospital delay in this study ranged between 3 and 4 hours, which was the median delay of symptom onset to ED arrival reported in previous studies published since the year 20004.
The factors associated with prehospital delay are numerous and include socio-demographic characteristics, clinical factors, contextural/social factors, cognitive factors and behavioral factors. For each factor, different associations were found across different studies. Although older age was found to be associated with prehospital delay in previous studies6,7,8,9,10,11,12, no association between older age and prehospital delay was found in our study, similar to other studies13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31. Contrary association with prehospital delay for stroke patients between sexes was found in some studies16,19,23,25, but no association was also found in our study, similar to most studies6,7,8,9,10,13,14,15,17,18,20,21,22,24,26,27,28,29. Regarding regional differences, the differences in the proportions of prehospital delay ≥2 hours between CS, CD and SH were probably due to different EMS deliveries.
No difference in prehospital delay between haemorrhagic and ischemic stroke was found in our multivariate analysis, consistent with most other studies6,7,8,14,16,18,19,24,29,30. Interestingly, the proportion of patients with hemorrhagic stroke in the present study was relatively higher in the CS region, as noted in a previous stroke registry32. Further, the proportion of hemorrhagic stroke patients with a prehospital delay ≥2 hours was higher than that for ischemic stroke patients in CS, in contrast to the findings in SH and CD.
No association between co-morbidities and prehospital delay for stroke was found, which is in agreement with the results from most prior studies8,9,10,14,16,17,18,19,21,23,26,28,30,31. Regarding symptoms and/or signs, only patients with coma were found to be less likely to have a prehospital delay compared to patients without. Similar to this study, stroke patients with coma were often transferred to the emergency department or hospital earlier in previous studies11,15,26,28,33.
In the present study, patients whose stroke symptoms were first noticed by cohabitants and non-cohabitant witnesses arrived at the hospital earlier, than patients who first noticed the stroke symptoms themselves. These findings could be potentially explained by different coping patterns: the patients themselves may have had a passive coping pattern after recognizing the symptoms of stroke, whereas witnesses often took a more active approach.
Previous studies have shown that patients whose symptoms improved between the symptom onset and hospital arrival were less likely to experience a prehospital delay34, whereas patients whose symptoms worsened were more likely to experience a prehospital delay11,28,35. However, the present study showed that only patients with partially improved symptoms, had an increased likelihood of prehospital delay when compared to patients with unchanged symptoms.
In the present study, patients with a nighttime onset of symptoms were more likely to have a prehospital delay compared to patients with a daytime onset. In other studies, patients whose symptoms presented during the day arrived at the emergency department or hospital earlier36, consistent with this study and patients with nighttime-onset stroke were more likely to have a prehospital delay for stroke evaluation13,20. Although nighttime onset was not found to be associated with prehospital delay in most previous studies10,17,18,19,24, similar to daytime onset7,8,17,18,22,25,30, one study even suggested that nocturnal onset independently contributed to early arrival26.
One study found that a Sunday onset was associated with prehospital delay of stroke within 1 hour29. However, no difference in prehospital delay was found between patients who developed symptoms on workdays versus weekends in the present study.
Although no influence of stroke awareness on prehospital delay was found in many previous studies7,10,19,23,24,29,34,37, other studies did find that when patients or bystanders were aware that the initial symptom was a stroke, the patient often arrived at the emergency department or hospital earlier than patients who were unaware26,27,38. The awareness rate of stroke warning symptoms ranged from 58.2% to 80.2% in stroke-free populations from these three cities in a previous study39. However, in the present study, only 16.9% of patients were aware that they were having a stroke. The proportion of prehospital delay ≥2 hours in stroke patients without awareness was higher than that in stroke patients with awareness. These findings suggest that the reported knowledge of early stroke symptoms in people who have not experienced a stroke is not equivalent to the patients’/bystanders’ ability to recognize the initial symptoms of a stroke when it is occurring. In addition, not all patients who were aware that their initial symptom was a stroke reported to EMS to achieve rapid transfer, although the proportion of patients who were aware of their stroke symptom and contacted EMS was higher than that in patients who were unaware.
In the present study, only 18.8% of patients used the emergency medical aid service and one-third of the stroke cases were not identified by ambulance doctors. According to the present investigation, the distance from the site of symptom onset to the hospital was obviously not the cause of prehospital delay for stroke, as 92.5% of patients with first-ever stroke were transferred to the emergency department or hospitals within 2 hours and no association was found between prehospital delay of stroke and means of prehospital transfer. In fact, one-quarter of patients arrived at the emergency department or hospital within 2 hours but did not receive standard treatment. Therefore, it would be beneficial to improve EMS for stroke in China to address the conflicts of interest between the hospital and the EMS system, improve the acute care of the “life green channel” for stroke in the hospital and achieve more rapid interactions between prehospital transfer in the EMS system and the “life green channel” for stroke in the hospital through implementation of organized stroke care.
The results of the univariate analysis of this study, but not the multivariate analysis, found that the use of EMS services reduced prehospital delay when compared to patients who arrived at the hospital by themselves and these finding are consistent with most previous studies6,8,12,16,19,20,21,22,23,25,27,28,29,30,36,38,40. These contradictory analyses may be due to a limited study sample; it is also possible that validity may be difficult to maintain a significant difference in OR values, or that the development of private car or taxi services in these larger cities may invalidate the results. In contrast, prehospital delay of arrival at the emergency department or hospital by non-EMS transfer was longer, as documented in previous studies11,35.
Another study showed that prehospital delay of arrival at a teaching hospital was longer, as these cases constituted non-first-referral at a teaching hospital20. However, the proportion of prehospital delay ≥2 hours at secondary hospitals was lower than that at tertiary hospitals in our univaritate analysis, although no difference in prehospital delay was found in the multivariate analysis. The present study evaluated information from a first-ever stroke registry regarding prehospital delay for patients’ first visits to the hospital, thus, our findings did not pertain to non-first-referral patients. Further analysis showed that the proportion of transfer time on the road of first visits to a secondary hospital within 2 hours was significantly higher than that to a tertiary hospital. Differences in the prehospital delay between different grade hospitals were likely due to resource allocation of different grade hospitals in communities, which led to differences in arrival times to different- grade hospitals.
In the present study, only 4.2% of patients arrived at local CHS centers or hospitals and 4 patients with stroke waited for their GPs at home in SH. Thus, GP contact was not a risk factor for prehospital delay in this target populations, which was different from the findings in other studies7,24,34. Obviously, it is necessary to improve the knowledge of stroke warning symptoms and the awareness of EMS use in populations through health education. Indeed, the proportion of patients who arrived at local hospitals or CHS centers was not high in our investigation and our findings further showed that patients lacked an awareness of the rapid transfer following stroke to qualified hospitals for acute stroke care. In brief, the continuity of optimal stroke care calls for the development of organized stroke care, covering organization of prehospital care, hospital treatment and follow-up care (rehabilitation and recurrence prevention) from available health resources and services in China.
The strength of this study was its use of a community-based stroke registry that collected information on first visits to an emergency department or hospital without organized stroke care. In particular, these findings are more suitable for education regarding the “FAST” compaign in communities in the developing countries where organized stroke care is nonexistent. However, it was difficult to completely register stroke information on presentation to the emergency or hospitals in communities. Nonetheless, no differences in age, sex, or major subtypes of stroke were found, which implied that the patient sample used in this analysis could be representative of all strokes registered in communities.
In summary, prehospital delay for stroke was common in communities and was attributed to a lack of awareness of the symptoms of stroke, not calling for emergency medical services and the lack of effective interactions between prehospital transfer and the “life green channel” for stroke in hospitals. Thus, intervention measures in communities should focus on education regarding the early identification of stroke, the importance of calling for EMS and the development of organized stroke care.
Additional Information
How to cite this article: Jiang, B. et al. Pre-hospital delay and its associated factors in first-ever stroke registered in communities from three cities in China. Sci. Rep. 6, 29795; doi: 10.1038/srep29795 (2016).
References
Jiang, B. et al. Incidence and trends of stroke and its subtypes in China. Results from three large cities. Stroke 37, 63–68 (2006).
Liu, M. et al. Stroke in China: epidemiology, prevention and management strategies. Lancet Neurol 6, 456–64 (2007).
Jin, H. et al. Factors Associated With Prehospital Delays in the Presentation of Acute Stroke in Urban China. Stroke 43, 362–370 (2012).
Evenson, K. R., Foraker, R., Morris, D. L. & Rosamond, W. D. A comprehensive review of prehospital and in-hospital delay times in acute stroke care. Int J Stroke 4, 187–199 (2009).
Ali, R. Emergency medicine in China: Redefining a specialty. J Emerg Med 21, 197–207 (2001).
Lacy, C. R., Suh, D. C., Bueno, M. & Kostis, J. B. Delay in presentation and evaluation for acute stroke: Stroke time registry for outcomes knowledge and epidemiology (S.T.R.O.K.E.). Stroke 32, 63–69 (2001).
Srivastava, A. K. & Pradsd, K. A study of factors delaying hospital arrival of patients with acute stroke. Neurol India 49, 272–276 (2001).
Rossnagel, K. et al. Out-of-hospital delays in patients with acute stroke. Ann Emerg Med 44, 476–483 (2004).
Nowacki, P. et al. Patients’ and bystanders’ awareness of stroke and prehospital delay after stroke onset: Perspectives for thrombolysis in West Pomerania Province, Poland. Eur Neurol 58, 159–165 (2007).
Chang, K. C., Tseng, M. C. & Tan, T. Y. Prehospital delay after acute stroke in Kaohsiung, Taiwan. Stroke 35, 700–704 (2004).
Kim, H. J., Ahn, J. H., Kim, S. H. & Hong, E. S. Factors associated with prehospital delay for acute stroke in Ulsan, Korea. J Emerg Med 41, 59–63 (2011).
Faiz, K. W., Sundseth, A., Thommessen, B. & Rønning, O. M. Prehospital delay in acute stroke and TIA. Emerg Med J 30, 669–74 (2013).
Harper, G. D., Haigh, R. A., Potter, J. F. & Castleden, C. M. Facters delaying hospital admission after stroke in Leicestershire. Stroke 23, 835–838 (1992).
Jorgensen, H. S., Nakayama, H., Reith, J., Raaschou, H. O. & Olsen, T. S. Factors delaying hospital admission in acute stroke: The Copenhagen Stroke Study. Neurology 47, 383–387 (1996).
Azzimondi, G. et al. Variables associated with hospital arrival time after stroke: Effect of delay on the clinical efficiency of early treatment. Stroke 28, 537–542 (1997).
Menon, S. C., Pandey, D. K. & Morgenstern, L. B. Critical factors determining access to acute stroke care. Neurology 51, 427–432 (1998).
Smith, M. A. et al. Delayed hospital arrival for acute stroke: The Minnesota stroke survey. Ann Intern Med 129, 190–196 (1998).
Casetta, I. et al. Temporal trend and factors associated with delayed hospital admission of stroke patients. Neuroepidemiology 18, 255–264 (1999).
Derex, L., Adeleine, P., Nighoghossian, N., Honnorat, J. & Trouillas, P. Factors influencing early admission in a French stroke unit. Stroke 33, 153–159 (2002).
Harraf, F. et al. A multicentre observational study of presentation and early assessment of acute stroke. BMJ 325(7354), 17, 10.1136/bmj.325.7354.17 (2002).
Turan, T. N. et al. Clinical characteristics of patients with early hospital arrival after stroke symptom onset. J Stroke Cerebrovasc Dis 14, 272–277 (2005).
Agyeman, O. et al. Time to admission in acute ischemic stroke and transient ischemic attack. Stroke 37, 963–966 (2006).
Barr, J., McKinley, S., O’Brien, E. & Herkes, G. Patient recognition of and response to symptoms of TIA or stroke. Neuroepidemiology 26, 168–175 (2006).
Pandian, J. D. et al. Factors delaying admission to a hospital-based stroke unit in India. J Stroke Cerebrovasc Dis 15, 81–87 (2006).
Mandelzweig, L., Goldbourt, U., Boyko, V. & Tanne, D. Perceptual, social and behavioral factors associated with delays in seeking medical care in patients with symptoms of acute stroke. Stroke 37, 1248–1253 (2006).
Iguchi, Y. et al. First Impression at stroke onset plays an important role in early hospital arrival. Intern Med 45, 447–451 (2006).
Ritter, M. A. et al. Discrepancy between theoretical knowledge and real action in acute stroke: Self-assessment as an important predictor of time to admission. Neurol Res 29, 476–479 (2007).
Inatomi, Y., Yonehara, T., Hashimoto, Y., Hirano, T. & Uchino, M. Prehospital delay in the use of intravenours rt-PA for acute ischemic stroke in Japan. J Neurol Sci 270, 127–132 (2008).
Palomeras, E. et al. Emergency perception and other variables associated with extra-hospital delay in stroke patients in the Maresme region (Spain). Eur J Neurol 15, 329–335 (2008).
Maestroni, A. et al. Factors influencing delay in presentation for acute stroke in an emergency department in Milan, Italy. Emerg Med J 25, 340–345 (2008).
Memis, S., Tugrul, E., Evci, E. D. & Ergin, F. Multiple causes for delay in arrival at hospital in acute stroke patients in Aydin, Turkey. BMC Neurol 8, 15, 10.1186/1471-2377-8-15 (2008).
Yang, Q. D. et al. Incidence of Cerebral Hemorrhage in the Changsha Community. Cerebrovasc Dis 17, 303–313 (2004).
Yanagida, T., Fujimoto, S., Inoue, T. & Suzuki, S. Prehospital delay and stroke-related symptoms. Intern Med 54, 171–177 (2015).
Salisbury, H. R., Banks, B. J., Footitt, D. R., Winner, S. J. & Reynolds, D. J. Delay in presentation of patients with acute stroke to hospital in Oxford. QJM 91, 635–640 (1998).
Hong, E. S., Kim, S. H., Kim, W. Y., Ahn, R. & Hong, J. S. Factors associated with prehospital delay in acute stroke. Emerg Med J 28, 790–793 (2011).
Song, D. et al. Factors Associated with Early Hospital Arrival in Patients with Acute Ischemic Stroke. J Stroke 17, 159–167 (2015).
Bohannon, R. W., Silverman, I. E. & Ahlquist, M. Time to emergency department arrival and its determinants in patients with acute ischemic stroke. Conn Med 67, 145–148 (2003).
Kim, Y. S. et al. Stroke awareness decreases prehospital delay after acute ischemic stroke in Korea. BMC Neurol 11, 2, 10.1186/1471-2377-11-2 (2011).
Sun, H. et al. Public Knowledge of Stroke in Chinese urban residents: a community questionnaire study. Neurol Res 33, 536–540 (2011).
Zerwic, J., Hwang, S. Y. & Tucco, L. Interpretation of symptoms and delay in seeking treatment by patients who have had a stroke: exploratory study. Heart Lung 36, 25–34 (2007).
Acknowledgements
This study was funded by the Ministry of Science and Technology and the Ministry of Health of the People’s Republic of China under Grant Nos. 2007BAI24B03 and 2011BAI08B01 of the National Key Technology R&D Program.
Author information
Authors and Affiliations
Contributions
All authors contributed to the field works, data collection and analysis. B.J. and W.W. designed the study and directed its implementation. Y.L., J.H. and L.H. were responsible for local field work. B.J. performed the statistical analysis and manuscript writing. All contributors discussed the findings and approved the final version for publication.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Jiang, B., Ru, X., Sun, H. et al. Pre-hospital delay and its associated factors in first-ever stroke registered in communities from three cities in China. Sci Rep 6, 29795 (2016). https://doi.org/10.1038/srep29795
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep29795
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.