Abstract
Emerging evidence demonstrates that the blockade of intracellular Ca2+ signals may protect pancreatic acinar cells against Ca2+ overload, intracellular protease activation, and necrosis. The activation of cannabinoid receptor subtype 2 (CB2R) prevents acinar cell pathogenesis in animal models of acute pancreatitis. However, whether CB2Rs modulate intracellular Ca2+ signals in pancreatic acinar cells is largely unknown. We evaluated the roles of CB2R agonist, GW405833 (GW) in agonist-induced Ca2+ oscillations in pancreatic acinar cells using multiple experimental approaches with acute dissociated pancreatic acinar cells prepared from wild type, CB1R-knockout (KO), and CB2R-KO mice. Immunohistochemical labeling revealed that CB2R protein was expressed in mouse pancreatic acinar cells. Electrophysiological experiments showed that activation of CB2Rs by GW reduced acetylcholine (ACh)-, but not cholecystokinin (CCK)-induced Ca2+ oscillations in a concentration-dependent manner; this inhibition was prevented by a selective CB2R antagonist, AM630, or was absent in CB2R-KO but not CB1R-KO mice. In addition, GW eliminated L-arginine-induced enhancement of Ca2+ oscillations, pancreatic amylase, and pulmonary myeloperoxidase. Collectively, we provide novel evidence that activation of CB2Rs eliminates ACh-induced Ca2+ oscillations and L-arginine-induced enhancement of Ca2+ signaling in mouse pancreatic acinar cells, which suggests a potential cellular mechanism of CB2R-mediated protection in acute pancreatitis.
Similar content being viewed by others
Introduction
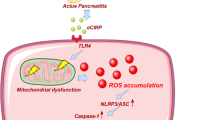
Acute pancreatitis is an inflammatory disease, which has several causes and symptoms and requires immediate medical attention1,2. In clinical practice, there are still no efficient drugs that specifically treat acute pancreatitis1. Emerging evidence demonstrates that a primary event initiating the process of acute pancreatitis is the excessive release of Ca2+ from intracellular stores3. These studies provide a promising therapeutic strategy—the blockade of Ca2+ release-activated Ca2+ currents in pancreatic acinar cells may provide significant protection against Ca2+ overload, intracellular protease activation, and necrosis, which are the major triggers of acute pancreatitis.
The cannabinoid receptor type 2 (CB2R) is a G protein-coupled receptor that, in humans, is encoded by the CNR2 gene4. CB2Rs are predominantly expressed in the periphery, especially in immune cells, suggesting that CB2R mediates the effects of cannabinoids mainly in the immune system. For example, activation of CB2Rs inhibits adenylyl cyclase via Gi/Goα subunits and causes a reduction in the intracellular level of cyclic adenosine monophosphate (cAMP)5,6, which has been implicated in a variety of modulatory functions including immune suppression, induction of apoptosis, and induction of cell migration7. Thus, CB2R agonists may be useful candidates for treating inflammatory diseases and pain8. Consistent with these findings, increased CB2R expression has been observed in spinal cord, dorsal root ganglion, and activated microglia in a rodent model of neuropathic pain, as well as in human hepatocellular carcinoma tumor samples9. In addition, emerging data demonstrate that CB2R mRNA and protein are expressed in pancreatic acinar cells, and activation of these CB2Rs prevents acinar cell pathogenesis in an animal model of pancreatitis10. However, whether the activation of CB2R modulates intracellular Ca2+ signals in pancreatic acinar cells is largely unknown. Specifically, it is unknown whether an agent that induces pancreatitis (e.g., L-arginine) enhances Ca2+ oscillations and whether application of a CB2R agonist eliminates L-arginine-induced enhancement of Ca2+ oscillations in pancreatic acinar cells.
In this study, we address these important questions using patch-clamp and confocal Ca2+ imaging approaches combined with immunohistochemistry using wild-type (WT), CB1R-knockout (KO), and CB2R-KO mice.
Methods
All experimental protocols were approved by and performed in accordance with guidelines set by the animal care and use and ethical committees at the Barrow Neurological Institute, Xiangya Hospital (Hunan, Changsha, China), and Shantou University Medical College (Shantou, Guangdong, China).
Animals
Mice used for this study were adult (4–6 month old), male, CD1 mice (Charles River Laboratories International, Inc., Wilmington, MA, USA). In addition, WT, CB1RKO11, and CB2RKO mice12 with C57BL/6J genetic backgrounds were initially provided by Dr. Zheng-Xiong Xi at the National Institute on Drug Abuse (NIDA; Bethesda, MD, USA), and were then bred in animal facilities at the Barrow Neurological Institute, which are accredited by the Association for Assessment and Accreditation of Laboratory Animal Care. Genotyping was performed at the NIDA Intramural Research Program before experiments were begun. All animals used in the experiments were matched for age (8–14 weeks) and weight (25–35 grams).
Mouse Pancreatic Acinar Cell Preparation
Acute isolated pancreatic cells were prepared as previously described13,14,15. In brief, pancreatic glands were taken from isoflurane-anesthetized mice, and fragments of the tissue were minced and digested using collagenase (200 U/mL, 25–30 min, 37 °C; Wako Pure Chemicals, Osaka, Japan) in the presence of 1-mM Ca2+. After collagenase digestion, the cell suspension was gently pipetted to obtain further separation of the cells, and then washed with physiological saline. A 100-μL volume of cell suspension was then poured into extracellular solution in a 2-mL experimental bath. The isolated cells usually adhered to the bottom within 15–20 min and were used for recording within 3 h after preparation. All experiments were performed at room temperature (22 ± 1 °C).
Whole-Cell Patch-Clamp Recording and Perforated-Patch Recording
Conventional whole-cell patch-clamp recording was used to record the Ca2+-activated Cl− currents for monitoring intracellular Ca2+ signal oscillations, as reported previously13,14. The recording pipettes, made from borosilicate glass capillaries, had a resistance of 3–5 MΩ when filled with pipette solution. After a GΩ seal was established between the cell membrane and the pipette, a whole-cell configuration was achieved by brief negative suction. Transmembrane currents were recorded with a patch-clamp amplifier (Axopatch 200B; Molecular Devices, Sunnyvale, CA, USA) at a holding potential (VH) of −30 mV. For perforated-patch recording, amphotericin B (200 μg/mL) was dissolved into the pipette solution. In these studies, we did not compensate for series resistance.
Drug Application
A stream of standard extracellular solution was continuously perfused over the cell during recording. A computer-controlled U-tube system was used for drug application16. For intracellular drug application, the drug was added into pipette solution, and establishment of a whole-cell configuration allowed the drug to diffuse into the recorded cell.
Amylase Estimation
Serum amylase activity was measured using the AMS assay kit (Nanjing Jiancheng Corp., Nanjing, China) and a microplate reader, following the manufacturer’s recommendations.
Myeloperoxidase Estimation
To measure myeloperoxidase (MPO) activity, lung tissues were immediately homogenized on ice in 10 volumes of normal saline. MPO activity was measured using the MPO assay kit (Nanjing Jiancheng Corp., Nanjing, China) and a microplate reader, following the manufacturer’s recommendations.
CB2R Immunoblot Assay
WT, CB1R-KO, and CB2R- KO mice (3 mice for each group) were anesthetized and quickly perfused with saline to flash all blood cells. Both whole striatum and spleen tissue were dissected out, snap frozen, and kept on dry ice. All the tissues were homogenized in cell lysis buffer (Cell Signaling Technology, Inc., Danvers, MA, USA) using a sonicator and centrifuge at 15,000 rpm for 15 min at 4 °C to get supernatant. The protein concentration for each sample was quantified with a Bio-Rad Protein Assay (Bio-Rad Laboratories, Hercules, CA, USA). A total of 20-μg protein (spleen) or 40-μg protein (striatum) were loaded and separated by SDS-PAGE in a 4–15% gradient gel for the detection of endogenous calnexin (Enzo Life Sciences, SPA865) and CB2R (NIDA-5633) by using Invitrogen blotting and transferring modules (Grand Island, NY, USA). Membranes were blocked for 2 h at room temperature with Licor Odyssey blocking buffer (LI-COR Biosciences, Lincoln, NE, USA) after washing 3 times with phosphate-buffered saline containing 0.1% Tween-20. Membranes were first incubated with either anti-CB2 (1:500 NIDA-5633 Ab) or anti-calnexin (1:1,000) antibody overnight at 4 °C. After washing 3 times, the membranes were incubated with goat anti-rabbit IgG (IRDye 680CW) (1:2,500) for 1.5 h at room temperature. Then the membranes were washed 3 times and then scanned in a Licor Odyssey Sa Imaging System (LI-COR Biosciences).
Immunohistochemistry
Sections were first blocked in 5% bovine serum albumin (BSA) and 0.5% Triton X-100 in phosphate buffer (PB) for 2 h at room temperature. Then, sections were incubated with 1:500 NIDA-5633 mCB2R antibody (Genemed Synthesis Inc, San Antonio, TX, USA) at 4 °C overnight. After washing 3 times with 0.1 M PB, sections were incubated with Alexa Fluor 488 goat anti-rabbit secondary antibody (Invitrogen, Carlsbad, CA, USA) in 5% BSA and 0.5% Triton X-100 PB for 2 h at room temperature. Sections were then washed, mounted, and cover slipped. Images were taken with a fluorescence microscope (Nikon Eclipse 80i) equipped with a digital camera (Nikon Instruments Inc., Melville, NY, USA).
Confocal Ca2+ Imaging
Dissociated pancreatic acinar cells were first incubated with fluo-4-AM (15 μM) (Molecular Probes, Eugene, OR, USA) for 15 min, followed by a 10-min rest allowing for de-esterification of the indicator. Confocal imaging was performed using an Olympus FluoView FV1000 microscope (Olympus Corporation, Center Valley, PA, USA) equipped with an argon laser (488 nm) and a UPLSAPO 40×, 0.95 NA objective. X-Y imaging was performed at a rate of 1.644 s per frame, 400 frames total, with a resolution of 512 × 512. Fluorescent fluo-4 signal was measured using ImageJ v.1.47 (available from the U.S. National Institutes of Health, Bethesda, MD, USA; http://imagej.nih.gov/ij/).
Solution and Chemicals
Standard extracellular solution contained (in mM): 140 NaCl, 1.0 CaCl2, 4.7 KCl, 1.13 MgCl2, 10 glucose, and 10 HEPES, adjusted to pH 7.2 with NaOH. Pipette solution contained (in mM) 140 KCl, 1.13 MgCl2, 5 Na2ATP, 0.24 EGTA, 10 glucose and 10 HEPES, pH 7.2. Drugs used in this study were GW405833 (Supplemental Fig. 1), JWH133, ACEA, and AM630, cholecystokinin (CCK), which were purchased from Tocris Bioscience (Minneapolis, MN, USA). Acetylcholine (ACh), amphotericin B, and L-arginine were purchased from Sigma-Aldrich (St. Louis, MO, USA).
CB2R antibodies, NIDA-5633 mCB2-Ab (customer-designed, raised in rabbit) that recognize the C-terminal (326-340 aa) of mCB2Rs, were produced by Genemed Synthesis Inc. (San Antonio, TX, USA).
Statistics
For patch-clamp experiments, the Ca2+-activated Cl− current responses were presented as the current charge (current area/Cm/min), and then the drug-induced changes were compared to the baseline level of charge (induced by ACh). When data were obtained from the same recorded cell and the changes of ACh response were compared before, during, and after testing drug exposure, a paired Student t test was used. To compare the effect of the tested drug between 2 groups of animals (e.g., saline group and L-arginine group), the unpaired Student t test was used. To analyze multiple effects, one-way analysis of variance (ANOVA) with Tukey’s post hoc tests were used.
Results
CB2Rs Are Expressed on Mouse Pancreatic Acinar Cells
Under the acutely dissociated acinar cell protocol, the isolated cells exhibited a typical kidney shape with secretion granules in the central area of the cells (Supplemental Fig. 2), suggesting the purity of the acinar cells as previously reported13,15,17. Figure 1A shows the results of the immunoblot assays, illustrating that a CB2-positive band was detected (at ~40 kD) in both the spleen and striatal tissues of WT and CB1-KO (CB1−/−), while the densities of this band in CB2-KO mice (CB2−/−) were substantially reduced in CB2-rich spleen tissues and almost undetectable in striatal tissues. Figure 1B shows CB2R immunostaining with the CB2R antibody (NIDA-5633), illustrating that the high densities of CB2R immunostaining were detected in the majority of spleen cells of WT mice. In contrast, a very low density of CB2-like staining was detected in a minority of spleen cells in CB2R KO mice, suggesting that the NIDA-5633 antibody used is highly mouse CB2R-specific. We then used this antibody to detect CB2R expression in single isolated acinar cells. Figure 1C demonstrates the photographs taken in bright field (Ca), mouse CB2R antibody (mCB2-ir, Cb), DAPI (Cc), and merged mCB2-ir and DAPI (Cd). We found high densities of CB2R immunolabeling in pancreatic acinar cells (Fig. 1Cb,d). These results suggest that CB2R protein is expressed in dissociated mouse pancreatic acinar cells.
(A) Western blot assay shows that a high-density CB2-immunoreactive band is detected in both spleen and striatal tissues in WT and CB1-KO mice, but is undetectable in striatal tissues or substantially reduced in CB2-rich spleen tissues in CB2-KO mice. (B) Immunohistochemical assays show high densities of CB2-immunostaining in spleen slices of WT mice, which are undetectable or substantially diminished in CB2-KO mice. (C) Immunocytochemical assays use mouse CB2R antibody (NIDA-5633). The bright field photograph (Ca) shows freshly dissociated pancreatic acinar cells. CB2-immunostaining (mCB2-ir) in single dissociated pancreatic acinar cells illustrates the high densities of CB2R proteins (Cb). DAPI staining demonstrates cell nucleus (Cc). The “Merged” image shows superimposed mCB2-ir and DAPI images (Cd).
Effects of GW405833 on ACh-Induced Ca2+ Oscillations
In acutely dissociated pancreatic acinar cells, low nanomolar concentrations of ACh induced intracellular Ca2+ signal oscillations, which can be detected using patch-clamp recording and Ca2+ imaging as previously reported13,14,18,19,20. Our initial series of experiments was designed to test the effects of the CB2R agonist, GW405833 (GW), on ACh-induced Ca2+ oscillations. Figure 2A demonstrates an experimental protocol, in which the ACh (e.g., 10 nM) is continuously perfused to the recorded cell through a bath (U-tube) to get Ca2+ oscillation response (as a baseline). Then, the GW is added to the bath perfusion in the presence of ACh. Finally, the GW is washed out with the same concentration of ACh. With this protocol, the ACh is continuously perfused throughout the recording period, and we can compare the change of ACh-induced Ca2+ oscillations before GW perfusion (baseline), during GW perfusion, and after GW washout in the same recorded cell. For statistical analysis of the effects of GW on ACh-induced Ca2+ oscillations, we measured baseline oscillations as the charge (current area/Cm/min)18 and compared the changes of Ca2+ oscillations during GW perfusion and after washout of GW to the baseline. Our data showed that in the continuous presence of 10 nM ACh, 10 μM GW reduced Ca2+ oscillations, and this inhibitory effect was reversed after washout (Fig. 2B). A similar inhibitory effect by GW (100 μM) was also observed on 100 nM ACh-induced Ca2+ oscillations using confocal Ca2+ imaging (Fig. 2C). Statistical analysis of the Ca2+ oscillation signal from 8 cells tested showed that GW significantly reduced ACh-induced Ca2+ oscillations from baseline level of −4.69 ± 0.32 to −1.68 ± 0.32 nC/min (the level after GW exposure, n = 8, paired t test p < 0.001, Fig. 2D). Ca2+ imaging experiments also showed a similar inhibition of Ca2+ oscillations by GW (n = 66, paired t test p < 0.001, Fig. 2E). After washout of GW, Ca2+ oscillations were partially recovered in both patch recording and Ca2+ imaging. These results suggest that activation of CB2R by GW inhibits ACh-induced intracellular Ca2+ signals in freshly isolated pancreatic acinar cells.
(A) Experimental protocol shows continuous exposure to ACh (baseline), addition of GW on top of ACh, and washout of GW (with ACh). A typical trace of ACh-induced Ca2+ oscillations measured using patch-clamp whole-cell recording in voltage-clamp mode (measuring Ca2+-dependent Cl− current). In the continuous presence of ACh (10 nM), addition of GW (10 μM) reversibly reduced Ca2+ oscillations. (B) A typical trace of ACh-induced Ca2+ oscillations measured using confocal Ca2+ imaging; GW (100 μM) inhibited ACh (100 nM)-induced Ca2+ oscillations. Statistical analysis shows that GW significantly reduces ACh-induced Ca2+ oscillations in both patch-clamp recording (C) and Ca2+ imaging experiments (D). (D) The net charge of ACh-induced baseline Ca2+ oscillations (prior to GW application) is compared to the charge during GW application (+GW) and during washout of GW (Washout). Numbers in parentheses indicate the number of cells tested. Columns indicate the mean of current charge ± SEM (left) and the mean DF/DO ± SEM (right) as compared to the baseline level. ***Indicates p < 0.001 for the value compared to baseline level. Statistic comparison between the levels of baseline and washout of GW showed significance (p < 0.05) in patch-clamp data (Fig. 2D left panel) and in Ca2+ imaging data (p < 0.01, Fig. 2D right panel).
GW Inhibits ACh-Induced Ca2+Oscillations in a Concentration-Dependent Manner
To profile the pharmacological effect of GW on ACh-induced Ca2+ oscillations, we examined the effects of different concentrations of GW on 10 nM ACh-induced Ca2+ oscillations. Figure 3A–C show that GW inhibited Ca2+ oscillations in a concentration-dependent manner. In 1 μm GW group, Ca2+ oscillation levels were slightly reduced from baseline −4.59 ± 1.11 to −4.46 ± 1.25 nC/min (p > 0.05, n = 8). In 10 μm GW group, Ca2+ oscillation levels were reduced from baseline −4.69 ± 0.32 to −1.68 ± 0.32 nC/min (p < 0.0001, n = 8). In 100 μm GW group, Ca2+ oscillation levels were reduced from baseline −5.77 ± 1.75 to −0.50 ± 0.15 nC/min (p < 0.05, n = 5). Further comparisons determined that Ca2+ oscillation levels differed significantly between the following groups: GW 1 μM vs. 10 μM (p < 0.05), GW 1 μM vs. 100 μM (p < 0.05), and GW 10 μM vs. 100 μM (p < 0.01), which confirms that GW inhibition occurs in a concentration-dependent manner.
Typical traces show the effect of different concentrations of GW: (A) 1 μM, (B) 10 μM, (C) 100 μM. (D) Bar graph summarizes the concentration-dependent effect of GW on ACh-induced Ca2+ oscillations. The number of cells tested is stated for each condition in parentheses. Columns show the mean of charge ± SEM. *Indicates p < 0.05, ***Indicates p < 0.001 for the values between baseline level of ACh response indicated as open columns at left and the level after GW exposure (solid columns). No asterisk mark means (GW 1 μM group) p > 0.05.
GW Inhibits ACh-Induced Ca2+ Oscillations by a Selective Action on CB2Rs
To address the question of whether GW inhibition of ACh-induced Ca2+ oscillations is mediated through CB2Rs, we designed three sets of experiments. 1) We tested the effect of a selective CB2R antagonist (AM630) on GW inhibition of Ca2+ oscillations. 2) We examined GW inhibitory effects on pancreatic acinar cells prepared from CB1-KO and CB2-KO mice. 3) We evaluated the effects of a selective CB1R agonist (ACEA) on ACh-induced Ca2+ oscillations. The results of these experiments demonstrated that GW inhibition of ACh-induced Ca2+ oscillations was presented in WT (Fig. 4A) and CB1R-KO mice (Fig. 4B), but was absent in CB2R-KO mice (Fig. 4C). Figure 4D summarizes pooled data demonstrating the effect of GW on 30 nM ACh-induced Ca2+ oscillations in WT (p < 0.01, n = 5), CB1R-KO (p < 0.001, n = 6), and CB2R-KO (p > 0.05, n = 8) mice. Furthermore, co-application of AM630 (0.1 μM) and GW (10 μM) abolished the inhibitory effect of GW on 10 nM ACh-induced Ca2+ oscillations (baseline vs. AM630 + GW p > 0.05, n = 10), while AM630 alone had no affect (baseline vs. AM630, p > 0.05, n = 10, Fig. 4E). Finally, we found that CB1R agonist, ACEA (10 μM) also reduced ACh-induced Ca2+ oscillations but this effect was likely mediated through ethanol that was used to dissolve ACEA (Supplemental Fig. 3). Together, these results suggest that GW inhibits ACh-induced intracellular Ca2+ signaling through the action of CB2Rs.
(A) A typical trace shows the effect of GW on ACh (30 nM)-induced Ca2+ oscillations in WT mice cells. (B) GW fails to inhibit ACh-induced Ca2+ oscillations in acinar cells prepared from CB1R-KO mice. (C) GW inhibits ACh-induced Ca2+ oscillations in acinar cells prepared from CB2R-KO mice. (D) Columns show the mean of charge ± SEM, summarizing the effect of GW on ACh-induced Ca2+ oscillations in WT, CB1R-KO and CB2R-KO mice cells. The number of cells tested is stated for each condition in parentheses. **Indicates p < 0.01 compared to the baseline level of ACh response (open columns) to the level after GW exposure (solid columns). (E) Bar graph demonstrates that the CB2R antagonist (AM630) alone does not significantly affect ACh-induced Ca2+ oscillation response (baseline vs. AM630: p > 0.05) but abolishes GW-induced inhibition (baseline vs. Am630 + GW: p > 0.05).
GW Inhibits ACh-Induced Ca2+ Oscillations through Membrane CB2Rs
Our data clearly demonstrated that GW inhibited ACh-induced intracellular Ca2+ oscillations. However, it remained unclear whether GW inhibition was mediated through extracellular or intracellular CB2Rs. GW could act on extracellular membrane CB2Rs and/or modulate muscarinic receptors, or GW could affect intracellular CB2Rs, and then modulate signal molecules such as G-protein and/or inositol 1,4,5-trisphosphate (IP3) receptors21. To distinguish among these possibilities, we designed two experiments, in which, either the CB2R agonist (GW) or antagonist (AM630) was applied internally or in which, IP3 was applied internally. When GW (100 μM) was added into the recording electrode and a perforated whole-cell recording (amphotericin B) was performed, bath-application of 10 nM ACh induced Ca2+ oscillations. When the recording mode was switched from perforated to conventional whole-cell recording by a brief suction, GW was infused into the recorded cell, and no detectable inhibitory effect on ACh-induced Ca2+ oscillations was present (Fig. 5A,D). Using the same experimental protocol, we applied AM630 (1 μM) intracellularly and found that internal AM630 failed to prevent bath-applied GW-induced inhibition in the ACh-induced Ca2+ oscillations (Fig. 5B,D). In the presence of intracellularly applied IP3 (30 μM), which causes IP3-induced Ca2+ oscillations, GW produced little inhibitory effect on the IP3-induced Ca2+ oscillations (Fig. 5C,D). These data suggest that GW inhibition of ACh-induced Ca2+ oscillations is not mediated through intracellular IP3 receptors. Together, these results suggest that GW inhibition of intracellular Ca2+ oscillations is mediated through CB2Rs on the surface of the cytoplasmic membrane.
(A) A typical trace shows ACh-induced Ca2+ oscillations between perforated and conventional whole-cell recordings, in which the pipette solution contained 100 μM GW. Infusion of GW into the recorded cell does not reduce ACh-induced Ca2+ oscillations (Aa). Ab: Summary of pooled data, demonstrating no significant difference between ACh responses with and without intracellular GW (p > 0.05, n = 6). (B) Internal infusion of AM630 fails to prevent bath-applied GW inhibition of ACh-induced Ca2+ oscillations. **Indicates p < 0.01. (C) Intracellular applied IP3-induced Ca2+ oscillations are not sensitive to bath-applied GW (Ca). (Cb) Bar graph summarizes the effect of GW on IP3-induced Ca2+ oscillations and showing no significance before and after GW exposure (p > 0.05, n = 7). The number of cells tested is stated for each condition in parentheses.
Effects of GW on CCK-Induced Ca2+ Oscillations
Data presented thus far demonstrate that GW inhibited ACh-induced Ca2+ oscillations through cell membrane CB2Rs, perhaps through CB2Rs and muscarinic receptor cross talk. To test this possibility, we applied CCK to induce Ca2+ oscillations, which occurs through different receptor signaling pathway than muscarinic receptor, and examined the effects of GW on the CCK-induced Ca2+ oscillations. As shown in Fig. 6, bath application of 10 pM CCK induced Ca2+ oscillation responses, which were not affected by bath application of GW (100 μM, Fig. 6A). In the same recorded cell, bath application of GW (100 μM) dramatically inhibited 10 nM ACh-induced Ca2+ oscillations (Fig. 6B). Figure 6C summarizes pooled data from 4 cells tested, and no significant effect of GW on CCK-induced Ca2+ oscillations was found (p > 0.05, n = 4, Ca), but GW inhibited ACh-induced Ca2+ oscillations in the same recorded cell (p < 0.01, n = 4, Cb).
(A) Representative typical trace of CCK (10 pM)-induced Ca2+ oscillations, which are not affected by 100 μM GW. (B) In the same recorded cell, ACh (10 nM)-induced Ca2+ oscillations are completed eliminated by GW. (C) Bar graph summarizes the effect of 100 μM GW on CCK (Ca)- and ACh (Cb)-induced Ca2+ oscillations. No asterisk mark (CCK vs CCK + GW 100 μM) means p > 0.05 (n = 4). **Indicates p < 0.01 compared between ACh 10 nM and ACh + GW 100 μM, n = 4.
L-arginine Potentiates ACh-Induced Ca2+ Oscillations
L-arginine is used to induce acute pancreatitis in rodents22. In dissociated pancreatic acinar cells, bath-application of L-arginine for 10 min enhanced ACh-induced Ca2+ oscillations from baseline level of 4.93 ± 0.39 to 10.34 ± 1.83 nC/min (Fig. 7Aa,b), which was not reversible after washout for 10 min (Ca2+ oscillations between L-arginine exposure and washout groups p > 0.05, n = 6, Fig. 7Ac). Statistical analysis revealed that L-arginine significantly enhanced ACh-induced Ca2+ oscillations (p < 0.05) in an irreversible manner (Fig. 7B).
(A) Representative traces of ACh-induced Ca2+ oscillations before (A), during (B), and after (C) bath-application of L-arginine (10 mM, L-Arg). Traces (A–C) were recorded from the same cell. (B) Bar graph summarizes the charge (±SEM) and shows an enhanced effect of L-Arg on ACh-induced Ca2+ oscillations. Six cells were assessed before and after L-Arg application. *Indicates p < 0.05 compared to baseline level. There was no significance between L-Arg application and washout of L-Arg (p > 0.05), suggesting the effects of L-Arg is non-reversible.
GW Prevents L-arginine-Enhanced Ca2+ Oscillations
Next, we sought to determine whether GW could eliminate L-arginine-induced enhancement of Ca2+ oscillations. We showed that either pre-treatment with GW (Fig. 8A), or co-administration of GW (10 μM) and L-arginine (Fig. 8B), abolished L-arginine-induced enhancement of Ca2+ oscillations (Fig. 8C,D), suggesting that selective activation of acinar cell CB2Rs significantly eliminates L-arginine-induced enhancement of intracellular Ca2+ signals in mouse pancreatic acinar cells.
(A) After pretreatment with GW, bath-applied L-Arg (10 mM for 10 min) fails to enhance ACh-induced Ca2+ oscillations. Traces in Fig. 8Aa,b were recorded from the same cell. (B) Without pretreatment, bath-applied L-Arg enhances ACh-induced Ca2+ oscillations, and under this condition, the addition of GW also reduces L-Arg-induced enhancement of Ca2+ oscillations. Traces in Fig. 8Ba,b were recorded from the same cell. (C,D) GW significantly blocks L-Arg-induced enhancement of Ca2+ oscillations either with or without pretreatment of GW. Bar graphs represent averaged charge ± SEM. The number of cells tested is stated for each condition in parentheses. *Indicates p < 0.05, ***Indicates p < 0.001.
GW Improves L-arginine-Induced Pathology
Finally, we tested whether systemic injection of GW can prevent L-arginine-induced elevation of Ca2+ oscillations, and subsequent pathological changes including enhancement of pancreatic amylases (AMS) and pulmonary peritoneal macrophages (MPO) levels, which are two major effects present in early-stage of acute pancreatitis. We injected L-arginine (4.0 g/kg, i.p.) to establish an acute pancreatitis model23,24, and dissociated pancreatic acinar cells 24 hours later, then compared ACh-induced Ca2+ oscillations between saline- and L-arginine-treated groups using Ca2+ imaging. Systemic L-arginine injection enhanced ACh-induced Ca2+ oscillations compared to systemic saline injection, but GW and L-arginine co-injected showed similar level of ACh-induced Ca2+ oscillations (Fig. 9A). Compared to the ACh-induced Ca2+ oscillations in saline-treated mice, the acinar cells prepared from L-arginine–treated mice showed a significant increase in Ca2+ oscillation response (saline vs. L-arginine group, p < 0.01), while co-injection of GW and L-arginine reduced L-arginine’s effect (saline vs. L-arginine + GW group, p > 0.05). These results suggest that the activation of pancreatic acinar cell CB2Rs may prevent early pathogenesis of acute pancreatitis through the inhibition of enhanced intracellular Ca2+ signals. In addition, co-injection of GW (10 mg/kg, i.p.) and L-arginine (4 g/kg, i.p.) also significantly reduced pancreatic L-arginine-induced enhancement of AMS (saline vs. L-arginine, p < 0.05, and saline vs. GW + L-arginine, p > 0.05; Fig. 9C) and pulmonary MPO levels (saline vs. L-arginine, p < 0.05, and saline vs. GW + L-arginine, p > 0.05; Fig. 9D). These results suggest that the activation of pancreatic acinar cell CB2Rs may prevent early pathogenesis of acute pancreatitis through the inhibition of intracellular Ca2+ signals.
(A) Representative comparison of ACh-induced Ca2+ oscillations between the acinar cells prepared from L-Arg (4 g/kg, i.p.) and normal saline (NS) treated mice (after injection for 24 h). These demonstrate an enhancement of ACh-induced Ca2+ oscillations in L-Arg-treated mice compared to NS-treated mice. This enhanced effect is prevented by co-injection of GW and L-Arg (GW + L-Arg). (B) In these studies, we measured Ca2+ responses as ∆F/F0, where F refers to the current Fluo signal intensity, F0 refers to the background Fluo signal intensity, and ∆F/F0 refers to the change of F/F0. Using the same measurement, we compared ACh-induced Ca2+ responses from pancreatic acinar cells collected from three groups of mice: control (saline-treated mice), L-Arg, and L-Arg plus GW. Compared to the ACh-induced Ca2+ oscillations in saline group, there is a significant enhancement of ACh-induced Ca2+ oscillations in L-Arg group (**Indicates p < 0.01), and there is no statistically significant difference between saline and GW + L-Arg groups (#indicates p > 0.05), suggesting a prevention of L-Arg-induced enhanced effect by GW. In addition, GW also prevents L-Arg-induced elevation of pancreatic AMS (C) and pulmonary MPO (D). The number of cells tested is stated for each condition. Bars represent mean ± SEM. In parts C and D, *Indicates p < 0.05 between saline and L-Arg groups, but there is no statistically significant difference between saline and L-Arg + GW group (#indicates p > 0.05).
Discussion
The novel findings of this study are that the activation of membrane CB2Rs by GW reduces ACh-, but not CCK-induced intracellular Ca2+ oscillations, and GW induced reduction of Ca2+ oscillations in a concentration-dependent manner. The CB2R-mediated reduction of ACh-induced Ca2+ oscillations is abolished by pharmacological blockade of CB2Rs (AM630) or is absent in CB2-KO mice, but not in CB1-KO mice. The pancreatitis inducer, L-arginine, significantly enhances ACh-induced intracellular Ca2+ oscillations, and the CB2R agonist, GW, abolishes this L-arginine effect. In addition, this CB2R agonist also improved L-arginine-induced pathological changes. Collectively, our data demonstrate that CB2R agonist GW reduces ACh-enhanced intracellular Ca2+ signals in mouse pancreatic acinar cells, and this may underlie an important cellular mechanism for a CB2R agonist to serve as a new candidate for treating acute pancreatitis.
CB2R Expression in Mouse Pancreatic Acinar Cells
Previously, in rodent pancreatic acinar cells, CB2R protein expression was found using immunohistochemical staining and Western blot10,25. In mouse pancreatic tissue, both CB1R and CB2R mRNA were identified using real-time RT-PCR and immunohistochemical staining10. In the present study, we confirmed that CB2R proteins were expressed in freshly isolated mouse pancreatic acinar cells, which is consistent with previous report10. Our data demonstrate that CB2Rs are expressed in mouse pancreatic acinar cells and they may play an important role in modulating acinar cells function.
CB2R Agonist Reduces ACh-Induced Ca2+ Oscillations in Mouse Pancreatic Acinar Cells
Mouse pancreatic acinar cells have been used as an excellent cell model of agonist-induced Ca2+ oscillations for studying pancreatitis26. We examined whether a selective CB2R agonist, GW, affected ACh-induced Ca2+ oscillations in the isolated pancreatic acinar cells through CB2Rs. Using both patch-clamp recording and confocal Ca2+ imaging techniques, we found that GW significantly reduced ACh-induced Ca2+ oscillations, and this inhibition is GW-concentration dependent. We also tested another selective CB2R agonist, JWH-133, on the ACh-induced Ca2+ oscillations, and found a similar inhibition (Supplemental Fig. 4), but the inhibitory effect of JWH-133 was weaker (a higher concentration of JWH-133 was needed compared with GW to induce the same inhibition). It was reported that GW acts as a potent and selective partial agonist for CB2R with an EC50 of 0.65 nM and selectivity of around 1200× for CB2R over CB1R27,28, while JWH-133 has an EC50 of 3.4 nM and selectivity of around 200× for CB2R over CB1R29. These findings may explain why GW is more potent than JWH-133 for ACh-induced Ca2+ oscillations.
Accumulating evidence demonstrates a complex relationship between the cannabinoid ligand (and receptors) and intracellular Ca2+ signals in different types of cells. For example, on one hand, activation of cannabinoid CB1R or CB2R increased (initiated) intracellular Ca2+ levels in endothelia cells30, submandibular acinar cells31, canine kidney cells32, and bladder cancer cells33. On the other hand, in pancreatic beta cells, the activation of either CB1R34 or CB2R35 reduced glucose-induced intracellular Ca2+ oscillations and insulin release. It has been reported that anandamide reduced intracellular Ca2+ concentration through the suppression of a Na+/Ca2+ exchanger current in rat cardiac myocytes36. To our knowledge, ours is the first report that a selective CB2R agonist reduces intracellular Ca2+ signals in mouse pancreatic acinar cells. Considering that Ca2+ plays an important role in cellular function, especially enzyme secretion in pancreatic acinar cells, our data suggest that CB2R modulates an important aspect of pancreatic acinar cell physiology and pathophysiology.
CB2R Agonist Reduces ACh-Induced Ca2+ Oscillations through Membrane CB2Rs
Cannabinoid ligands exert their pharmacological effects through CB1R or CB2R, but in some cases they also can act on non-cannabinoid targets37. We determined whether GW modulated intracellular Ca2+ signals through a cell membrane or cytosolic CB2Rs. First, we examined the effects of pharmacological manipulations of CB1R and CB2R and found that the CB2R selective antagonist AM630 abolished GW-induced reduction of Ca2+ oscillations, suggesting that GW modulates ACh-induced Ca2+ oscillations through the CB2Rs. Then, we genetically manipulated cannabinoid receptors and compared the effects of GW on Ca2+ oscillations between WT and CB2R-KO mice, and also WT and CB1R-KO mice. We found that in CB2R-KO but not CB1R-KO mice, GW lost its inhibitory effect, further confirming that CB2R is the key target for mediating GW-induced reduction in Ca2+ oscillations.
In a group of cells tested, we found that a CB1R agonist, ACEA (dissolved by ethanol; 10-μM ACEA solution contained 7.3-mM ethanol) reduced ACh-induced Ca2+ oscillations (Supplemental Fig. 3); however, the control experiments using the same concentration of ethanol (7.3 mM) also reduced ACh-induced Ca2+ oscillations, and the inhibitory effect of ACEA was not absent in the acinar cells dissociated from CB1R-KO mice, suggesting a non-specific effect, likely caused by ethanol. In addition, we also tested the effects of DMSO (GW was dissolved by DMSO to 100 mM stock solution), and found that 1 μM DMSO itself did not affect ACh-induced Ca2+ oscillations (Supplemental Fig. 5). Together, our data support the conclusion that GW selectively acts on acinar cell CB2Rs and reduces ACh-induced Ca2+ oscillations.
Finally, we asked where the CB2Rs are located (membrane or cytosolic CB2Rs). To address this question, we designed three experiments. We first examined the effect of bath-applied GW on the Ca2+ oscillations induced by intracellular application of IP3, and found that GW did not affect IP3-induced Ca2+ oscillations, suggesting that the target that mediated GW-induced inhibition in Ca2+ oscillations is located in the signal pathway before IP3 receptors, and not on the IP3 receptor itself. We then intracellularly applied GW through a recording electrode to examine the effect of intracellular administration of GW on bath ACh-induced Ca2+ oscillations, and found that intracellular infusion of GW (even at 100 μM) did not alter ACh-induced Ca2+ oscillations. Finally, we intracellularly applied AM630 through a recording electrode to examine the effect of bath-applied GW on ACh-induced Ca2+ oscillations. Our data showed that intracellular infusion of AM630 did not prevent bath-applied GW-induced reduction of Ca2+ oscillations. Collectively, our data support the conclusion that GW modulates intracellular Ca2+ signaling through the membrane CB2Rs in pancreatic acinar cells.
Possible Mechanisms of GW-Induced Reduction in ACh-Induced Ca2+ Oscillations
The precise mechanism by which GW modulates intracellular Ca2+ signals is unclear. Our data show that membrane CB2Rs are necessary for mediating GW’s effect. GW’s action in ACh-induced Ca2+ oscillations should occur at the G-protein-mediated signal pathway between muscarinic receptor (M3) activation and IP3 production because GW did not affect IP3-induced Ca2+ oscillations. We also demonstrated that GW failed to affect ACh-induced Ca2+ oscillations in pancreatic acinar cells prepared from CB2R-KO mice, suggesting that GW likely did not affect muscarinic receptor function. In addition, we found that bath-applied GW failed to inhibit CCK-induced Ca2+ oscillations even at 100 μM, suggesting that GW selectively modulates muscarinic receptor-mediated G-protein signaling38. Therefore, the possible mechanisms for GW-induced modulation of ACh-induced Ca2+ oscillations may involve cross talk between muscarinic receptor- and CB2R-mediated G-protein signal pathways, such as homologous and/or heterologous desensitization of G-protein coupled receptors (GPCRs)39. For example, in the case of homologous desensitization of GPCRs, the activation of one type of GPCR can rapidly terminate another GPCR signaling through the internalization of receptors after binding, phosphorylation of G-protein coupled receptor kinases, and formation of complexes with β-arresting39,40. In addition, the activation of a GPCR may also result in temporary inhibition of another GPCR signal through a heterologous desensitization, which does not involve receptor internalization, but activation of several signal transduction pathways, particularly protein kinase C (PKC)- and PKA-dependent signaling pathways38,41. It has been reported that intracellular cyclic AMP-generated substances play an important role in regulation of IP3 and Ca2+ responses to ACh in rat submandibular acini. Investigators found that intracellular cAMP increased IP3 formation in response to ACh, while blocking PKA by H89 reduced IP3 formation41. Because it is well known that the activation of CB2Rs significantly reduces intracellular cAMP levels, we thus postulated that GW may activate CB2Rs, reduce cAMP, and in turn reduce intracellular IP3 production, and lead to a reduction of ACh-induced Ca2+ oscillations. Our findings warrant further testing of this hypothesis.
Clinical Significance of CB2R-Mediated Reduction of Ca2+ Oscillations in Pancreatic Acinar Cells
Pancreatic acinar cells are functional units of the exocrine pancreas. They synthesize, store, and secrete inactive preforms of digestive enzymes into the lumen of the acinus. The activity of pancreatic acinar cells is crucially modulated by the secretagogues ACh and CCK; both can act on their specific membrane receptors (muscarinic and CCK receptor, respectively) and then induce an elevation in cytoplasmic calcium. If high concentrations of intracellular Ca2+ persist, intracellular signaling is disrupted, cell damage occurs, and acute pancreatitis forms. Emerging evidence suggests that the earliest abnormalities of acute pancreatitis arise by aberrant elevation of intracellular Ca2+ within acinar cells because the sustained intracellular Ca2+ elevation activates intracellular digestive proenzymes resulting in necrosis and inflammation, and pharmacological blockade of store-operated or Ca2+ release-activated Ca2+ channels would prevent sustained elevation of intracellular Ca2+, and consequence protease activation and necrosis3. In the present study, we provide the first evidence that the CB2R agonist, GW, reduces ACh-induced Ca2+ oscillations, abolishes L-arginine–induced enhancement of Ca2+ oscillations and prevents L-arginine–induced elevation of both pancreatic AMS and pulmonary MPO levels. These results suggest that a CB2R agonist may serve as a novel therapeutic strategy to prevent and/or treat acute pancreatitis. This conclusion is consistent with previous report that a CB2R agonist exhibits a protective effect on pathogenesis in an acute pancreatitis animal model10. Our data showing a reduction of intracellular Ca2+ signaling by GW also provide a new target to interpret the role of CB2R agonists in treating acute pancreatitis in addition to CB2R-mediated anti-inflammation.
Additional Information
How to cite this article: Huang, Z. et al. Cannabinoid receptor subtype 2 (CB2R) agonist, GW405833 reduces agonist-induced Ca2+ oscillations in mouse pancreatic acinar cells. Sci. Rep. 6, 29757; doi: 10.1038/srep29757 (2016).
References
Pandol, S. J., Saluja, A. K., Imrie, C. W. & Banks, P. A. Acute pancreatitis: bench to the bedside. Gastroenterology 132, 1127–1151 (2007).
Bakker, O. J. et al. Treatment options for acute pancreatitis. Nature reviews. Gastroenterology & hepatology 11, 462–469 (2014).
Gerasimenko, J. V. et al. Ca2+ release-activated Ca2+ channel blockade as a potential tool in antipancreatitis therapy. Proceedings of the National Academy of Sciences of the United States of America 110, 13186–13191 (2013).
Munro, S., Thomas, K. L. & Abu-Shaar, M. Molecular characterization of a peripheral receptor for cannabinoids. Nature 365, 61–65 (1993).
Kaminski, N. E. Immune regulation by cannabinoid compounds through the inhibition of the cyclic AMP signaling cascade and altered gene expression. Biochemical pharmacology 52, 1133–1140 (1996).
Herring, A. C., Koh, W. S. & Kaminski, N. E. Inhibition of the cyclic AMP signaling cascade and nuclear factor binding to CRE and kappaB elements by cannabinol, a minimally CNS-active cannabinoid. Biochemical pharmacology 55, 1013–1023 (1998).
Basu, S., Ray, A. & Dittel, B. N. Cannabinoid receptor 2 is critical for the homing and retention of marginal zone B lineage cells and for efficient T-independent immune responses. Journal of immunology 187, 5720–5732 (2011).
Cheng, Y. & Hitchcock, S. A. Targeting cannabinoid agonists for inflammatory and neuropathic pain. Expert opinion on investigational drugs 16, 951–965 (2007).
Pertwee, R. G. The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: delta9-tetrahydrocannabinol, cannabidiol and delta9-tetrahydrocannabivarin. British journal of pharmacology 153, 199–215 (2008).
Michler, T. et al. Activation of cannabinoid receptor 2 reduces inflammation in acute experimental pancreatitis via intra-acinar activation of p38 and MK2-dependent mechanisms. American journal of physiology. Gastrointestinal and liver physiology 304, G181–G192 (2013).
Zimmer, A., Zimmer, A. M., Hohmann, A. G., Herkenham, M. & Bonner, T. I. Increased mortality, hypoactivity, and hypoalgesia in cannabinoid CB1 receptor knockout mice. Proceedings of the National Academy of Sciences of the United States of America 96, 5780–5785 (1999).
Buckley, N. E. et al. Immunomodulation by cannabinoids is absent in mice deficient for the cannabinoid CB(2) receptor. European journal of pharmacology 396, 141–149 (2000).
Wu, J. et al. Thimerosal modulates the agonist-specific cytosolic Ca2+ oscillatory patterns in single pancreatic acinar cells of mouse. FEBS Lett 390, 149–152 (1996).
Wu, J. et al. 2-Aminoethoxydiphenyl borate modulates kinetics of intracellular Ca(2+) signals mediated by inositol 1,4,5-trisphosphate-sensitive Ca(2+) stores in single pancreatic acinar cells of mouse. Mol Pharmacol 58, 1368–1374 (2000).
Huang, Z. B. et al. Congo red modulates ACh-induced Ca(2+) oscillations in single pancreatic acinar cells of mice. Acta pharmacologica Sinica 35, 1514–1520 (2014).
Yang, K. et al. Distinctive nicotinic acetylcholine receptor functional phenotypes of rat ventral tegmental area dopaminergic neurons. J Physiol 587, 345–361 (2009).
Wu, J. et al. 2-aminoethoxydiphenyl borate inhibits agonist-induced Ca2+ signals by blocking inositol trisphosphate formation in acutely dissociated mouse pancreatic acinar cells. Pflugers Archiv: European journal of physiology 448, 592–595 (2004).
Wakui, M., Potter, B. V. & Petersen, O. H. Pulsatile intracellular calcium release does not depend on fluctuations in inositol trisphosphate concentration. Nature 339, 317–320 (1989).
Wakui, M., Osipchuk, Y. V. & Petersen, O. H. Receptor-activated cytoplasmic Ca2+ spiking mediated by inositol trisphosphate is due to Ca2(+)-induced Ca2+ release. Cell 63, 1025–1032 (1990).
Osipchuk, Y. V., Wakui, M., Yule, D. I., Gallacher, D. V. & Petersen, O. H. Cytoplasmic Ca2+ oscillations evoked by receptor stimulation, G-protein activation, internal application of inositol trisphosphate or Ca2+: simultaneous microfluorimetry and Ca2+ dependent Cl- current recording in single pancreatic acinar cells. The EMBO journal 9, 697–704 (1990).
den Boon, F. S. et al. Excitability of prefrontal cortical pyramidal neurons is modulated by activation of intracellular type-2 cannabinoid receptors. Proceedings of the National Academy of Sciences of the United States of America 109, 3534–3539 (2012).
Zhang, J. & Rouse, R. L. Histopathology and pathogenesis of caerulein-, duct ligation-, and arginine-induced acute pancreatitis in Sprague-Dawley rats and C57BL6 mice. Histology and histopathology 29, 1135–1152 (2014).
Kui, B. et al. New insights into the methodology of L-arginine-induced acute pancreatitis. PloS one 10, e0117588 (2015).
Yu, L. T. et al. Recombinant Reg3alpha protein protects against experimental acute pancreatitis in mice. Molecular and cellular endocrinology 422, 150–159 (2016).
Linari, G. et al. Involvement of cannabinoid CB1- and CB2-receptors in the modulation of exocrine pancreatic secretion. Pharmacological research: the official journal of the Italian Pharmacological Society 59, 207–214 (2009).
Petersen, O.H. Ca2+ signaling in pancreatic acinar cells: physiology and pathophysiology. Braz J Med Biol Res 42, 9–16 (2009).
Marriott, K. S. & Huffman, J. W. Recent advances in the development of selective ligands for the cannabinoid CB(2) receptor. Current topics in medicinal chemistry 8, 187–204 (2008).
Huffman, J. W. The search for selective ligands for the CB2 receptor. Current pharmaceutical design 6, 1323–1337 (2000).
Huffman, J. W. et al. 3-(1′,1′-Dimethylbutyl)-1-deoxy-delta8-THC and related compounds: synthesis of selective ligands for the CB2 receptor. Bioorganic & medicinal chemistry 7, 2905–2914 (1999).
Zoratti, C., Kipmen-Korgun, D., Osibow, K., Malli, R. & Graier, W. F. Anandamide initiates Ca(2+) signaling via CB2 receptor linked to phospholipase C in calf pulmonary endothelial cells. Br J Pharmacol 140, 1351–1362 (2003).
Kopach, O. et al. Cannabinoid receptors in submandibular acinar cells: functional coupling between saliva fluid and electrolytes secretion and Ca2+ signalling. Journal of cell science 125, 1884–1895 (2012).
Chou, K. J. et al. CP55,940 increases intracellular Ca2+ levels in Madin-Darby canine kidney cells. Life sciences 69, 1541–1548 (2001).
Jan, C. R. et al. Novel effect of CP55,940, a CB1/CB2 cannabinoid receptor agonist, on intracellular free Ca2+ levels in bladder cancer cells. The Chinese journal of physiology 45, 33–39 (2002).
Nakata, M. & Yada, T. Cannabinoids inhibit insulin secretion and cytosolic Ca2+ oscillation in islet beta-cells via CB1 receptors. Regulatory peptides 145, 49–53 (2008).
Juan-Pico, P. et al. Cannabinoid receptors regulate Ca(2+) signals and insulin secretion in pancreatic beta-cell. Cell calcium 39, 155–162 (2006).
Li, Q., Cui, N., Du, Y., Ma, H. & Zhang, Y. Anandamide reduces intracellular Ca2+ concentration through suppression of Na+/Ca2+ exchanger current in rat cardiac myocytes. PloS one 8, e63386 (2013).
Xiong, W. et al. Cannabinoids suppress inflammatory and neuropathic pain by targeting alpha3 glycine receptors. The Journal of experimental medicine 209, 1121–1134 (2012).
Doi, R., Chowdhury, P. & Rayford, P. L. Agonist-regulated alteration of the affinity of pancreatic muscarinic cholinergic receptors. The Journal of biological chemistry 268, 22436–22443 (1993).
Mohle, R. & Drost, A. C. G protein-coupled receptor crosstalk and signaling in hematopoietic stem and progenitor cells. Annals of the New York Academy of Sciences 1266, 63–67 (2012).
Luttrell, L. M. & Lefkowitz, R. J. The role of beta-arrestins in the termination and transduction of G-protein-coupled receptor signals. Journal of cell science 115, 455–465 (2002).
Martinez, J. R. & Zhang, G. H. Cross-talk in signal transduction pathways of rat submandibular acinar cells. European journal of morphology 36 Suppl, 190–193 (1998).
Acknowledgements
Part of this work was supported by a Seed Fund of Shangtou University Medical College and by Guangdong Science and Technology Foundation (HYW). Authors thank the editor in Barrow Neurological Institute Publication Department for her assistance for editing the English.
Author information
Authors and Affiliations
Contributions
All authors reviewed the manuscript. Z.H. reached the literature, designed patch-clamp experiments, performed most patch-clamp experiments, collected patch-clamp data, analyzed patch-clamp data, and prepared Figures 2, 3, 4, 5, 7 and 8. HW designed the acute pancreatitis experiments, collected and analyzed data, prepared Figure 9, and wrote part of the manuscript. M.Z. researched the literature, performed Ca2+ imaging experiments, collected and analyzed data, prepared Figures 2B,D and 9A,B. NS researched the literature, performed acute pancreatitis experiments, collected and analyzed data, and prepared Figure 9. F.S. researched the literature, performed acute pancreatitis experiments, collected and analyzed data, and prepared Figure 9. J.S. researched the literature, designed Ca2+ imaging experiments, analyzed data, prepared Figures 2B,D and 9A,B and wrote part of the manuscript. H.Z. designed and performed immunocytochemical experiments, analyzed data, prepared Figure 1, and wrote part of the manuscript. Z.X. designed molecular and cell biological experiments, analyzed data, prepared Figure 1 and revised the manuscript. Q.L. designed molecular biological experiments, analyzed data, prepared Figure 1 and revised the manuscript. K.X. and D.C. performed patch-clamp experiments and collected data for Figure 6. M.G. researched the literature, performed some patch-clamp experiments, collected patch-clamp data, analyzed patch-clamp data, and participated in the preparation of Figures 2, 3, 4, 5. R.P.H. designed and advised on patch-clamp experiments and revised the manuscript. X.F. participated in the design of all experiments, discussed and analyzed data, wrote part of the manuscript, and revised the manuscript. J.W. researched the literature, designed experiments, analyzed data, finalized all figures, and wrote the main manuscript text.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Huang, Z., Wang, H., Wang, J. et al. Cannabinoid receptor subtype 2 (CB2R) agonist, GW405833 reduces agonist-induced Ca2+ oscillations in mouse pancreatic acinar cells. Sci Rep 6, 29757 (2016). https://doi.org/10.1038/srep29757
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep29757
This article is cited by
-
CB2R agonist GW405833 alleviates acute liver failure in mice via inhibiting HIF-1α-mediated reprogramming of glycometabolism and macrophage proliferation
Acta Pharmacologica Sinica (2023)
-
Protective effects of specific cannabinoid receptor 2 agonist GW405833 on concanavalin A-induced acute liver injury in mice
Acta Pharmacologica Sinica (2019)
-
Heterogeneity of cannabinoid ligand-induced modulations in intracellular Ca2+ signals of mouse pancreatic acinar cells in vitro
Acta Pharmacologica Sinica (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.